Abstract
BACKGROUND AND PURPOSE: Various authors have developed criteria to classify MR imaging findings that suggest the possibility of multiple sclerosis. The purpose of this study was to evaluate and compare the capacity of three sets of MR imaging criteria for predicting the conversion of isolated demyelinating syndromes to clinically definite multiple sclerosis.
METHODS: Seventy patients with clinically isolated neurologic symptoms suggestive of multiple sclerosis were prospectively studied with MR imaging. The MR imaging findings were evaluated by two independent neuroradiologists who were blinded to clinical follow-up data. Based on the clinical outcome at follow-up (presence of a second attack that established clinically definite multiple sclerosis), the sensitivity, specificity, accuracy, positive predictive value, and negative predictive value of the criteria proposed by Paty et al, Fazekas et al, and Barkhof et al were calculated.
RESULTS: Clinically definite multiple sclerosis developed in 22 (31%) patients after a mean follow-up time of 28.3 months. The criteria proposed by Paty et al and those proposed by Fazekas et al showed identical results: sensitivity, 86%; specificity, 54%; accuracy, 64%; positive predictive value, 46%; and negative predictive value, 89%. The criteria proposed by Barkhof et al showed the following: sensitivity, 73%; specificity, 73%; accuracy, 73%; positive predictive value, 55%; and negative predictive value, 85%.
CONCLUSION: The four dichotomized MR imaging parameters proposed by Barkhof et al are more specific and accurate than the criteria proposed by Paty et al or Fazekas et al for predicting conversion to clinically definite multiple sclerosis.
Patients presenting with clinically isolated demyelinating syndromes do not necessarily have multiple sclerosis, although they may be at risk of developing this disease. It could be important for treatment and prognosis to determine the patient's likelihood of developing clinically definite multiple sclerosis after the first episode. The main paraclinical indicators associated with an increased risk of progression to multiple sclerosis are the presence of CSF oligoclonal bands (1) and multifocal white matter abnormalities on MR images (2). These MR imaging abnormalities are indistinguishable from multiple sclerosis in 40% to 80% of patients presenting with isolated syndromes, such as unilateral optic neuritis, internuclear ophthalmoplegia, or partial myelopathy (3–7). Even when such lesions are present, it is still not possible to diagnose definite multiple sclerosis, because the criterion of dissemination in time has not been fulfilled. It has, however, been shown that the presence of white matter abnormalities on MR images at the time of presentation with a clinically isolated syndrome suggestive of central nervous system demyelination is predictive of the long-term risk for subsequent development of multiple sclerosis, type of disease, and extent of disability (8, 9).
Several criteria have been proposed to classify MR imaging findings as being suggestive or not suggestive of multiple sclerosis. In 1988, Paty et al (10) established that images showing either four or more lesions or three lesions, one of which is in a periventricular location, are indicative of multiple sclerosis. These criteria have been evaluated prospectively in cases of patients who presented with isolated syndromes suggestive of multiple sclerosis, and they have shown high sensitivity but relatively low specificity (11). The most widely used diagnostic criteria for this purpose have been established by Fazekas et al (12), who defined abnormal images as those that show three or more lesions with two of the following characteristics: infratentorial location, periventricular location, or size larger than 6 mm. This model showed high sensitivity and specificity when evaluated retrospectively in cases of established multiple sclerosis (13), but it performed less well when prospectively applied to patients presenting with isolated syndromes suggestive of multiple sclerosis (14). Recently, Barkhof et al (15) developed a four-parameter dichotomized MR imaging model based on logistic regression analysis that requires the presence of at least one enhancing lesion (or nine lesions visible on T2-weighted image), one juxtacortical lesion, one infratentorial lesion, and three periventricular lesions. This model predicts conversion to clinically definite multiple sclerosis better than do the criteria proposed by Paty et al or Fazekas et al. The purpose of this study was to compare the effectiveness of the MR imaging criteria established by Barkhof et al, Paty et al, and Fazekas et al for predicting conversion of isolated demyelinating syndromes to clinically definite multiple sclerosis in a cohort of patients followed up prospectively for a minimum of 18 months.
Methods
The patients included in this prospective study were those who presented for the first time with monophasic neurologic symptoms of the type seen in cases of multiple sclerosis who were recruited at the Hospital General Vall d'Hebron in Barcelona or who were referred to us by neurologists and ophthalmologists from the surrounding area. The criteria for inclusion were as follows: 1) clinically isolated syndrome suggestive of central nervous system demyelination, involving the optic nerve, brain stem, or spinal cord, or any two or all three of these areas, and not attributable to other diseases; 2) age of 18 to 50 years; 3) onset of syndrome within 3 months of clinical and MR imaging examinations; and 4) minimum clinical follow-up duration of 18 months.
Seventy patients (46 female and 24 male patients) were enrolled in the study. Ages ranged from 19 to 49 years, with a mean age of 31 years. The mean follow-up duration was 28.3 ± 6.6 months (range, 18–43 months). Clinical history taking, physical examination, and follow-up were performed by one of four neurologists (M.T., J.R., P.D.-V., X.M.) to determine whether the patients spontaneously presented with new symptoms. A diagnosis of clinically definite multiple sclerosis was established when there was a second attack. This new attack was defined as an episode of symptoms, documented at the time of examination, that indicated a neurologic abnormality attributable to acute demyelination in one or more regions of the central nervous system; the symptoms had to last more than 24 hours and had to be separated from the initial attack by at least 4 weeks (16). The patients were seen every 3 months and were instructed to report any new symptoms or worsening of pre-existing symptoms.
Patients with an isolated spinal cord syndrome underwent spinal MR imaging, in addition to MR imaging of the brain, to exclude alternative pathologic abnormalities (data not shown). The CSF of 27 patients was analyzed for the presence of oligoclonal banding.
MR imaging was performed on a 1.0- or 1.5-T imager with a standard head coil and included the following pulse sequences: transverse proton density–and T2-weighted conventional spin-echo (2200/20−90/1 [TR/TE/excitations]) or fast spin-echo (3000/14−85/2) and, in some patients, contrast-enhanced (0.1 mmol/kg; imaging delay, 5 min) T1-weighted spin-echo (600/15/2). This last sequence was obtained for 25 of the 44 patients whose T2-weighted images showed high signal abnormalities. We used a section thickness of 5 mm, a pixel size of approximately 1 × 1 mm, and an interleaved imaging mode with an intersection gap of either 1.5 mm when using conventional spin-echo sequences or 5 mm when using fast spin-echo sequences to obtain, in the latter case, 2 × 13 sections, resulting in 26 contiguous sections covering the whole brain.
Additional sequences, such as sagittal T2-weighted fast spin-echo (3550−5000/90/2) or transverse T2-weighted fast fluid-attenuated inversion recovery (9000/110−150/11, with an inversion time of 2200–2500) were also performed in most patients. Because this was a comparative study of different MR imaging criteria applied to the images obtained in each patient individually, the use of different imagers and T2-weighted sequences should not have influenced the results.
The MR images were assessed independently by two neuroradiologists (A.R. and M.J.M.) who were blinded to clinical follow-up. In cases of discrepancy, a final decision was reached by consensus after a third analysis of the images.
The proton density–and T2-weighted images were scored according to total number of lesions, number of periventricular lesions, presence of juxtacortical lesions, presence of lesions larger than 6 mm, and presence of infratentorial lesions. For the patients for whom a contrast-enhanced T1-weighted sequence was obtained, the presence of at least one enhancing area related to a lesion seen on the T2-weighted images was also scored.
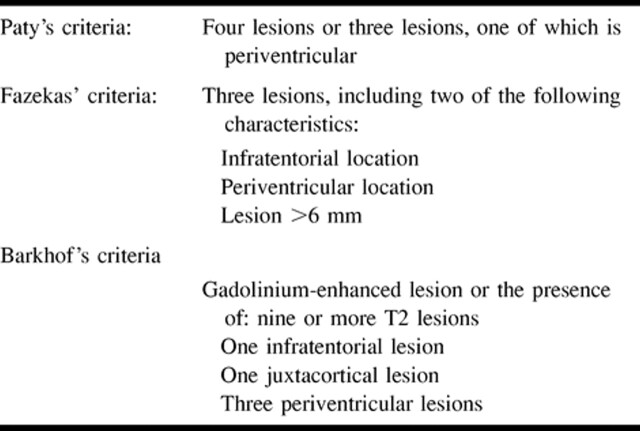
The criteria proposed by Paty et al (10) define imaging findings as definitely abnormal when four or more lesions are present or when at least three lesions, one of which is in a periventricular location, are present. The criteria proposed by Fazekas et al (12) require at least three lesions and two of the following features: 1) size of 6 mm or larger, 2) location abutting the lateral ventricles, or 3) infratentorial location (Table 1). The four-parameter dichotomized MR imaging model proposed by Barkhof et al (15) includes the following: 1) presence of at least one contrast-enhancing lesion (or at least nine lesions on the T2-weighted images of a patient for whom no contrast-enhanced T1-weighted images were obtained), 2) at least three periventricular lesions, 3) at least one juxtacortical lesion, and 4) at least one infratentorial lesion (Table 1).
TABLE 1:
Diagnostic MR Imaging criteria
The value of MR imaging findings with regard to clinical follow-up was expressed as sensitivity (true-positive/[true-positive + false-negative]), specificity (true-negative/[true-negative + false-positive]), and accuracy (true-positive + true-negative/[true-positive + false-negative + true-negative + false-positive]). Positive predictive value was defined as (true-positive/[true-positive + false-positive]) and negative predictive value as (true-negative/[true-negative + false-negative]). True-positive was defined as abnormal MR imaging findings and conversion to clinically definite multiple sclerosis, false-positive as positive MR imaging findings in the absence of conversion to clinically definite multiple sclerosis, false-negative as normal MR imaging findings but conversion to clinically definite multiple sclerosis, and true-negative as normal MR imaging findings and no conversion to clinically definite multiple sclerosis. Logistic regression analysis was conducted to calculate these parameters for the model presented by Barkhof et al. The comparison of ratios was based on the range observed at a 95% confidence interval, considering the absence of overlapping as an indicator of differences.
Results
Of the 70 patients enrolled in the study, 24 presented with optic neuritis, 20 with brain stem symptoms, 19 with spinal cord syndrome, and seven with polyregional symptoms. At clinical follow-up (mean, 28.3 ± 6.6 months; range, 18–43 months), clinically definite multiple sclerosis was diagnosed in 22 of the 70 patients (prevalence, 31%; mean conversion time, 12 months).
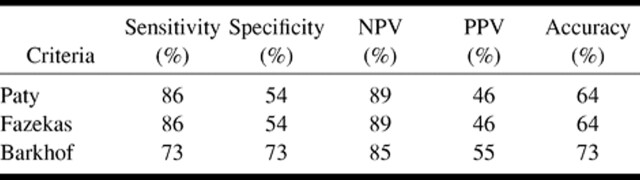
The MR images did not meet the criteria proposed by Paty et al and Fazekas et al in 29 (41%) patients, three (10%) of whom developed clinically definite multiple sclerosis (negative predictive value of 89%). MR imaging initially revealed T2-weighted abnormalities according to the criteria proposed by Paty et al and Fazekas et al in 41 (58%) patients, 19 (46%) of whom developed clinically definite multiple sclerosis. These criteria showed sensitivity of 86% (19 of 22 patients), specificity of 54% (26 of 48 patients), accuracy of 64% (45 of 70 patients), positive predictive value of 46% (19 of 41 patients), and negative predictive value of 89% (26 of 29 patients) (Table 2).
TABLE 2:
Diagnostic performance of different MR Imaging criteria
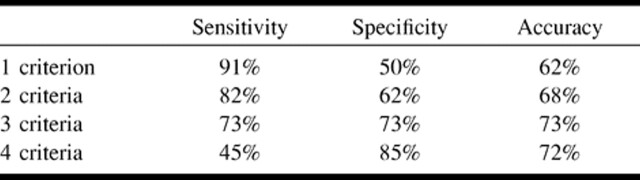
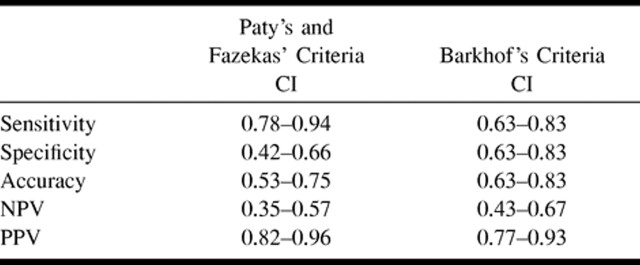
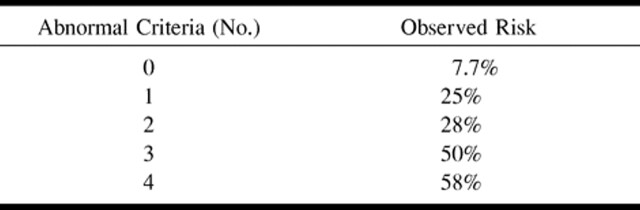
MR imaging was considered normal according to the criteria proposed by Barkhof et al (none of the four requisites fulfilled) in 26 (37%) patients, two (7%) of whom developed clinically definite multiple sclerosis. Based on the results of logistic regression analysis using the four dichotomized parameters proposed by Barkhof et al, we determined that specificity increased and sensitivity decreased when the minimum number of criteria for classifying an image as abnormal was incremented. Accuracy was optimal with a minimum of three parameters (Table 3). With this new cutoff point, we obtained sensitivity of 73% (16 of 22 patients), specificity of 73% (35 of 48 patients), accuracy of 73% (51 of 70 patients), positive predictive value of 55% (16 of 29 patients), and negative predictive value of 85% (35 of 41 patients) (Table 2). Based on the confidence intervals, we determined no differences in terms of sensitivity, accuracy, positive predictive value, and negative predictive value among the three sets of criteria. The confidence intervals of specificity, however, showed practically no overlapping; therefore, in terms of specificity, a difference can be assumed between the criteria proposed by Barkhof et al and those proposed by Paty et al or Fazekas et al (Table 4). The relationship between the number of abnormal parameters in the Barkhof model and the observed risk (percentage of patients with clinically definite multiple sclerosis) is shown in Table 5.
TABLE 3:
Sensitivity, specificity, and accuracy versus the number of Barkhof criteria for optimized cut-off
TABLE 4:
Confidence intervals for the different MR Imaging criteria
TABLE 5:
Relationship between number of abnormal Barkhof criteria and observed risk
CSF analysis for the presence of oligoclonal banding was positive in 66% of the patients (18 of 27 patients). Among patients who fulfilled the criteria proposed by Paty et al and Fazekas et al, the results of analysis of oligoclonal banding were positive in 93% (13 of 14 patients). For patients who did not fulfill the criteria proposed by Paty et al or Fazekas et al, the results of analysis of oligoclonal banding were positive in 38% (5 of 13 patients) (P < .002). The results of analysis of oligoclonal banding were positive in 33% of the patients (4 of 12 patients) who had none of the criteria proposed by Barkhof et al, in 80% of the patients (4 of 5 patients) with one criterion, and in all of the patients (10 of 10 patients) with two, three, or four of the criteria (P < .002).
Discussion
Multiple sclerosis is a central nervous system disorder that results in abnormalities over time and space. In most instances, the first symptoms and signs indicate a lesion in the optic nerve, brain stem, or spinal cord. Not all patients with these symptoms, however, have conditions that progress to clinically definite multiple sclerosis.
A clinical diagnosis of multiple sclerosis is established when the two fundamental criteria of dissociation in space and time are fulfilled. MR imaging is the most sensitive paraclinical test for revealing dissociation in space (10, 11), and several follow-up studies have shown that MR imaging of the brain at the time of presentation with a clinically isolated syndrome is strongly predictive of the risk of developing clinically definite multiple sclerosis. Short-term follow-up studies of 1 to 5 years' duration have shown that patients with normal results of MR imaging of the brain at the time of presentation have a low (5%) risk of progression to clinically definite multiple sclerosis, whereas for those with abnormal MR imaging results, the risk is much higher (7, 17–19). Our study shows similar results. After a mean follow-up duration of 28 months, only one patient with strictly normal MR imaging results and 47% of the patients with abnormal MR imaging results had their conditions progress to clinically definite multiple sclerosis. The number and characteristics of the lesions are also important. Morrissey et al (20) reported conversion to clinically definite multiple sclerosis after 5 years of follow-up in 54% of their patients with one to three lesions and in 85% of their patients with four or more lesions. A long-term study recently reported by O'Riordan et al (9) confirmed progression to clinically definite multiple sclerosis in 83% of their patients who had abnormal results of MR imaging of the brain at the time of presentation and in 11% of their patients who had normal results of MR imaging of the brain. The number of lesions at the time of presentation also seemed to be related to clinical scores and the course of disease at follow-up (9).
The MR images of the present cohort revealed disseminated abnormalities consistent with demyelination in 58% to 63% of subjects, depending on the MR imaging criteria used. These asymptomatic abnormalities could potentially represent a disseminated presentation of a monophasic illness or the onset of multiple sclerosis. Differentiation between these two processes at the time of presentation is important, not only because it provides patients with an accurate prognosis but also because it is fundamental for selecting patients for therapeutic trials aimed at preventing or delaying the development of multiple sclerosis and disability (9, 21), the main issue being selection of patients at high risk for progression over a 2- to 5-year period. Different MR imaging entry criteria are currently being used in phase III treatment trials to determine whether the use of interferon-β in patients with a clinically isolated syndrome delays development of clinically definite multiple sclerosis. These criteria show high sensitivity, although specificity is considerably lower. Using the most commonly applied criteria, such as those proposed by Paty et al and Fazekas et al, we reached a sensitivity of 86% and a specificity of 54%. Conversion of multiple sclerosis at follow-up, however, is usually less than 50%, implying that specificity is more important than sensitivity for initial evaluation of these patients. Barkhof et al (15) proposed a four-parameter dichotomized MR imaging model that increased specificity. The model was obtained by means of logistic regression analysis assessing the relative individual contribution of several MR imaging parameters. Regression analysis was used to decrease redundancy of information and to identify the parameters that best predicted conversion to clinically definite multiple sclerosis. This method showed that enhancing and juxtacortical lesions provided the most important information and that infratentorial and periventricular lesions provided the next most important information. If there are no contrast-enhanced images, the alternative criterion proposed by Barkhof et al was the presence of at least nine lesions on T2-weighted images. These requisites combine number and location of lesions on T2-weighted images and presence of enhancing lesions, thus indicating dissociation not only in space but also in time and fulfilling both clinical requirements needed to establish a definite diagnosis of multiple sclerosis. Based on the MR imaging criteria proposed by Barkhof et al, we found that accuracy was optimal when at least three parameters were fulfilled. Specificity was 73%, a value higher than the values obtained by applying the criteria proposed by Paty et al and Fazekas et al, which are sensitive but less specific.
Almost 50% of the patients for whom oligoclonal banding analysis was conducted could be considered to have had laboratory-supported definite multiple sclerosis according to the criteria proposed by Poser et al (16). A significant correlation was observed between the likelihood of having positive results of oligoclonal banding analysis and fulfillment of the criteria proposed by Paty et al, Fazekas et al, and Barkhof et al. All patients who met at least two of the criteria proposed by Barkhof et al had positive results of their oligoclonal banding analysis and were thus considered to have laboratory-supported definite multiple sclerosis.
The sensitivity of all the MR criteria should improve by using a 3-mm section thickness and a combination of fast spin-echo and fast fluid-attenuated inversion-recovery sequences (22–24), although an increase in specificity has not been shown. This approach results in increased operator time but should be recommended in the initial workup of patients who are presenting for the first time with neurologic syndromes that suggest a demyelinating disease when sensitivity in detection of brain lesions is considered more important than specificity. Moreover, it has been shown that the use of different field strengths does not significantly influence the number of lesions detected (25).
Considering the relatively short follow-up period, it is important to emphasize that lack of conversion may simply indicate a less active course during the observation period rather than lack of conversion to multiple sclerosis. With longer clinical follow-up, the rate of progression to clinically definite multiple sclerosis will probably increase and the sensitivity and specificity of the MR imaging criteria proposed by Barkhof et al will probably improve. The negative predictive value was very high for all of the criteria studied, but it might be even higher if spinal MR imaging is also performed at the time of presentation. O'Riordan et al (26) described asymptomatic spinal cord lesions in 27% of their patients with clinically isolated syndromes, suggesting that MR imaging of the spinal cord could increase the sensitivity and negative predictive value of MR imaging criteria in predicting conversion to clinically definite multiple sclerosis.
Conclusion
In our prospectively selected cohort, the four dichotomized MR imaging parameters proposed by Barkhof et al constituted the most effective model for predicting conversion to clinically definite multiple sclerosis. The variables involved can be easily assessed, and the fact that the number of positive criteria can be related to the likelihood for developing multiple sclerosis is attractive. In future studies, the cutoff for the criteria proposed by Barkhof et al can be adapted according to the individual goal: priority for high sensitivity or priority for high specificity. To balance both end points best, we found that selecting patients with three or four criteria resulted in the highest accuracy.
Acknowledgments
We thank Juli Alonso and Xavi Aymerich for technical assistance and Celine L. Cavallo for preparation of the manuscript.
Footnotes
Address reprint requests to Mar Tintoré, MD, Unit of Clinical Neuroimmunology, Escola d'Enfermeria 5ª planta, Hospital General Universitari Vall d'Hebron, Pg. Vall d'Hebron 119–129, 08035 Barcelona, Spain.
References
- 1.Sandberg-Wollheim M, Bynke H, Cronqvist S, Holtas S, Platz P, Ryder LP. A long-term prospective study of optic neuritis: evaluation of risk factors. Ann Neurol 1990;27:386-393 [DOI] [PubMed] [Google Scholar]
- 2.Ormerod IE, Miller DH, McDonald WI, et al. The role of NMR imaging in the assessment of multiple sclerosis and isolated neurological lesions: a quantitative study. Brain 1987;110:1579-1616 [DOI] [PubMed] [Google Scholar]
- 3.Beck RW, Cleary PA, Anderson MM Jr, et al. A randomized, controlled trial of corticosteroids in the treatment of acute optic neuritis: The Optic Neuritis Study Group. N Engl J Med 1992;27:581-588 [DOI] [PubMed] [Google Scholar]
- 4.Ford B, Tampieri D, Francis G. Long-term follow-up of acute partial transverse myelopathy. Neurology 1992;42:250-252 [DOI] [PubMed] [Google Scholar]
- 5.Miller DH, Ormerod IE, Gibson A, du Boulay EP, Rudge P, McDonald WI. MR brain scanning in patients with vasculitis: differentiation from multiple sclerosis. Neuroradiology 1987;29:226-231 [DOI] [PubMed] [Google Scholar]
- 6.Río J, Nos C, Rovira A, Tintoré M, Codina A, Montalbán X. The development of multiple sclerosis following an isolated episode of optic neuritis: magnetic resonance study. Med Clin (Barc) 1997;109:370-372 [PubMed] [Google Scholar]
- 7.Tintoré M, Rovira A, Río J, Hernández D, Marzo ME, Montalbán X. Optic neuritis brainstem syndromes and myelitis: early conversion to multiple sclerosis. Med Clin (Barc) 1999;112:693-694 [PubMed] [Google Scholar]
- 8.Filippi M, Horsfield MA, Morrissey SP, et al. Quantitative brain MRI lesion load predicts the course of clinically isolated syndromes suggestive of multiple sclerosis. Neurology 1994;44:635-641 [DOI] [PubMed] [Google Scholar]
- 9.O'Riordan JI, Thompson AJ, Kingsley DP, et al. The prognostic value of brain MRI in clinically isolated syndromes of the CNS: a 10-year follow-up. Brain 1998;121:495-503 [DOI] [PubMed] [Google Scholar]
- 10.Paty DW, Oger JJ, Kastrukoff LF, et al. MRI in the diagnosis of MS: a prospective study with comparison of clinical evaluation, evoked potentials, oligoclonal banding, and CT. Neurology 1988;38:180-185 [DOI] [PubMed] [Google Scholar]
- 11.Lee KH, Hashimoto SA, Hooge JP, et al. Magnetic resonance imaging of the head in the diagnosis of multiple sclerosis: a prospective 2-year follow-up with comparison of clinical evaluation, evoked potentials, oligoclonal banding, and CT. Neurology 1991;41:657-660 [DOI] [PubMed] [Google Scholar]
- 12.Fazekas F, Offenbacher H, Fuchs S, et al. Criteria for an increased specificity of MRI interpretation in elderly subjects with suspected multiple sclerosis. Neurology 1988;38:1822-1825 [DOI] [PubMed] [Google Scholar]
- 13.Offenbacher H, Fazekas F, Schmidt R, et al. Assessment of MRI criteria for a diagnosis of MS. Neurology 1993;43:905-909 [DOI] [PubMed] [Google Scholar]
- 14.Tas MW, Barkhol F, van Walderveen MA, Polman CH, Hommes OR, Valk J. The effect of gadolinium on the sensitivity and specificity of MR in the initial diagnosis of multiple sclerosis. AJNR Am J Neuroradiol 1995;16:259-264 [PMC free article] [PubMed] [Google Scholar]
- 15.Barkhof F, Filippi M, Miller DH, et al. Comparison of MRI criteria at first presentation to predict conversion to clinically definite multiple sclerosis. Brain 1997;120:2059-2069 [DOI] [PubMed] [Google Scholar]
- 16.Poser CM, Paty DW, Scheinberg L, et al. New diagnostic criteria for multiple sclerosis: guidelines for research proposals. Ann Neurol 1983;13:227-231 [DOI] [PubMed] [Google Scholar]
- 17.Filippini G, Comi GC, Cosi V, et al. Sensitivities and predictive values of paraclinical tests for diagnosing multiple sclerosis. J Neurol 1994;241:132-137 [DOI] [PubMed] [Google Scholar]
- 18.Miller DH, Ormerod IE, Rudge P, Kendall BE, Moseley IF, McDonald WI. The early risk of multiple sclerosis following isolated acute syndromes of the brainstem and spinal cord. Ann Neurol 1989;26:635-639 [DOI] [PubMed] [Google Scholar]
- 19.Sharief MK, Thompson EJ. The predictive value of intrathecal immunoglobulin synthesis and magnetic resonance imaging in acute isolated syndromes for subsequent development of multiple sclerosis. Ann Neurol 1991;29:147-151 [DOI] [PubMed] [Google Scholar]
- 20.Morrissey SP, Miller DH, Kendall BE, et al. The significance of brain magnetic resonance imaging abnormalities at presentation with clinically isolated syndromes suggestive of multiple sclerosis: a 5-year follow-up study. Brain 1993;116:135-146 [DOI] [PubMed] [Google Scholar]
- 21.Miller DH, Albert PS, Barkhof F, et al. Guidelines for the use of magnetic resonance techniques in monitoring the treatment of multiple sclerosis: US National MS Society Task Force. Ann Neurol 1996;39:6-16 [DOI] [PubMed] [Google Scholar]
- 22.Filippi M, van Waesberghe JH, Horsfield MA, et al. Interscanner variation in brain MRI lesion load measurements in MS: implications for clinical trials. Neurology 1997;49:371-377 [DOI] [PubMed] [Google Scholar]
- 23.Molyneaux PD, Tubridy N, Parker GJM, et al. The effect of section thickness on MR lesion detection and quantification in multiple sclerosis. AJNR Am J Neuroradiol 1998;19:1715-1720 [PMC free article] [PubMed] [Google Scholar]
- 24.Yousry TA, Filippi M, Becker C, Horsfield MA, Voltz R. Comparison of MR pulse sequences in the detection of multiple sclerosis lesions. AJNR Am J Neuroradiol 1997;18:959-963 [PMC free article] [PubMed] [Google Scholar]
- 25.Lee DH, Vellet AD, Eliasziw M, et al. MR imaging field strength: prospective evaluation of the diagnostic accuracy of MR for diagnosis of multiple sclerosis at 0.5 and 1.5 T. Radiology 1995;194:257-262 [DOI] [PubMed] [Google Scholar]
- 26.O'Riordan JI, Losseff NA, Phatouros C, et al. Asymptomatic spinal cord lesions in clinically isolated optic nerve, brain stem, and spinal cord syndromes suggestive of demyelination. J Neurol Neurosurg Psychiatry 1998;64:353-357 [DOI] [PMC free article] [PubMed] [Google Scholar]