Abstract
BACKGROUND AND PURPOSE: Most traumatic brain injuries are classified as mild, yet in many instances cognitive deficits result. The purpose of this study was to investigate possible relationships between quantitative magnetization transfer imaging (MTI) and neurocognitive findings in a cohort of patients with mild head trauma but negative findings on conventional MR images.
METHODS: We examined 13 patients and 10 healthy volunteers with a standard MR protocol including fast spin-echo and gradient-echo imaging, to which was added quantitative MTI. MTI was performed with a modified gradient-echo sequence incorporating pulsed, off-resonance saturation. Both region-of-interest analysis and contour plots were obtained from the MTI data. A subgroup of nine patients was examined with a battery of neuropsychological tests, comprising 25 measures of neurocognitive ability.
RESULTS: The magnetization transfer ratio (MTR) in the splenium of the corpus callosum was lower in the patient group as compared with the control group, but no significant reduction in MTR was found in the pons. Individual regional MTR values were significantly reduced in two cases, and contour plot analysis revealed focal areas of abnormality in the splenium of four patients. All the patients showed impairment on at least three measures of the neuropsychological test battery, and in two cases a significant correlation was found between regional MTR values and neuropsychological performance.
CONCLUSION: Our results suggest that MTI and contour plot analysis may add sensitivity to the MR imaging examination of patients with traumatic brain injury.
Head injury is common in the United States, with severe traumatic brain injury (TBI) accounting for approximately 100 000 deaths per year (1–3). Most TBI is not severe, however, and 75% of TBIs can be classified as mild by a number of competing criteria. The present study was motivated by previous results in animal models of TBI (4, 5) and a desire to understand the relationship between the severity of trauma and its consequences. Discerning this relationship is complicated by the necessity to differentiate between postconcussion symptoms and cognitive weakness (6). The purpose of this study was to investigate relationships between results of quantitative MR imaging, obtained with magnetization transfer (MT) contrast, and neurocognitive findings in a cohort of patients who had experienced mild head trauma but had negative findings on conventional MR imaging studies. For the purposes of this article, conventional MR imaging is defined as a routine clinical brain protocol, including both T1- and T2-weighted spin-echo sequences and a susceptibility-weighted gradient-echo sequence. Our hypothesis was that quantitative magnetization transfer imaging (MTI) analysis would offer increased sensitivity over conventional MR imaging in the detection of TBI in patients at risk for cognitive deficits consequent to mild TBI.
Methods
We examined 13 patients who had experienced a head injury, met the limited criteria for mild TBI, and were subsequently referred for neuropsychological follow-up owing to persistent cognitive deficit(s). We used the definition for mild head trauma developed by the Mild Traumatic Brain Injury Interdisciplinary Special Interest Group of the American Congress of Rehabilitation Medicine (7). The definition includes manifestation of at least one of the following: 1) any period of loss of consciousness; 2) any loss of memory for events immediately before or after the accident; 3) any alteration in mental state at the time of the accident (eg, feeling dazed, disoriented, or confused); and 4) focal neurologic deficit(s) that may or may not be transient, with severity of the injury not exceeding the following: a) loss of consciousness for approximately 30 minutes or less, b) an initial Glasgow Coma Scale score of 13 to 15 after 30 minutes, and c) posttraumatic amnesia for not more than 24 hours.
Mechanisms of injury include the head being struck, the head striking an object, and the brain undergoing an acceleration/deceleration movement, such as in whiplash. The definition excludes stroke, tumors, and other disorders not directly related to trauma. Findings on conventional CT scans and MR images may be normal.
For all patients in this study, conventional MR examinations included fast spin-echo proton density–weighted (2500/16/1) (TR/TE/excitations) and T2-weighted (2500/85/1, echo train length = 4, slice thickness = 5 mm) sequences, as well as a susceptibility-weighted gradient-echo sequence (750/40/2, flip angle = 10°, slice thickness = 5 mm). Sample images are depicted in Figure 1. In 12 of 13 patients, no abnormalities were detected. In one 60-year-old patient, a few subcortical areas of high signal intensity on T2-weighted images were attributed to small-vessel ischemic disease and judged to be unrelated to TBI. Ten healthy volunteers with no history of head injury underwent an identical MR protocol, including MTI. The control and patient groups had a similar age range and distribution, with patients averaging 38 years of age and volunteers 35 years (median age, 35 and 36 years, respectively). Most patients were studied within several months of their injury, but in two cases self-referral and follow-up for cognitive deficit took place years after the injury.
fig 1.
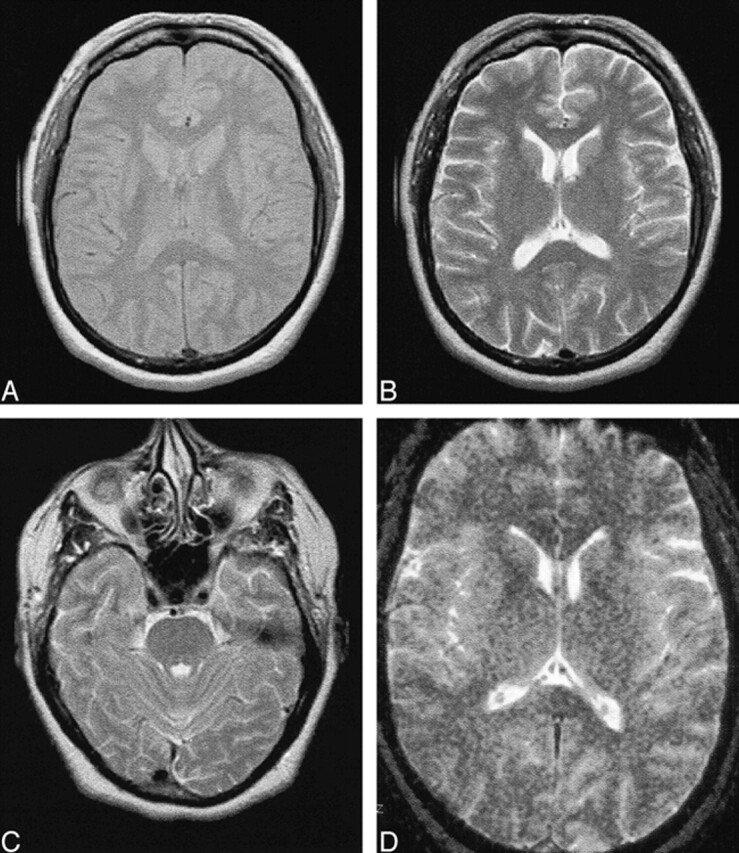
A–D, MR images in a patient with mild head trauma. Proton density–weighted (A) and T2-weighted (B) axial images at the level of the splenium and T2-weighted image at the level of the pons (C) show hyperintensity attributed to partial volume effect from the petrous bone. D is a gradient-echo image
Magnetization Transfer Imaging
A 3D gradient-echo pulse sequence, modified to generate MT contrast, was implemented at 1.5 T. Both saturation and control images were acquired in the axial plane by using a pulsed, off-resonance MT technique with MT saturation applied at 1200 Hz below resonance frequency. Slice thickness was 5 mm and 28 slices were acquired. Timing parameters were chosen to minimize T1 and T2 weighting (106/5/1, flip angle = 12°). Calculation of the magnetization transfer ratio (MTR) (8) was carried out on a pixel-by-pixel basis for generation of contour plots and average region-of-interest (ROI) MTR values. For analysis of the splenium and pons, slices were selected as demonstrated in Figure 1. Adjacent slices were examined to exclude partial volume effects, and four or five ROIs (3 × 3 pixels) were placed on the splenium or pons, respectively, then averaged to yield individual mean values.
MTR contour plots reveal variations and gradations of MTR overlaid on anatomic images, analogous to elevation information on topographic maps. This technique has been described previously in a double-blind study of an animal model of head trauma (4). It is based on a larger body of investigation using MTR, a measure that has been found to be robust and reproducible in a number of centers (10, 13–15). In the present study, the variance of normal white matter in areas pertinent to our investigation was obtained via ROI analysis of the control subjects, and contour lines corresponding to boundaries of 2 SD below normal were overlaid on MT images. Thus, each contour line represented a boundary between regions of MTR greater than and less than the individual threshold. We focused our investigation on two regions, the splenium of the corpus callosum and the pons, regions that were found to be susceptible to injury detectable by MTI in a previous study of more severe trauma (9). Average MTRs were determined over the ROIs, and the regional average MTR values were compared between the patient and control groups. MTR contour maps were constructed on the basis of statistical analysis of the control group, such that regions identified by contours were characterized by values at least 2 SD from normal. Contour maps of the focal areas were evaluated by a neuroradiologist and compared with contour maps from the group of volunteers to identify areas of abnormal MTRs. Examples are shown in Figure 1.
Neuropsychological Testing
A battery of neuropsychological tests was administered to each patient during two separate sessions. Tests expected to be sensitive to mild TBI were chosen for inclusion in the battery. In particular, the cognitive domains tested were attention/concentration, memory/new learning ability, mental flexibility, verbal fluency, confrontational naming, and visuoconstruction. The neuropsychological test battery consisted of the Trail Making Test, Paced Auditory Serial Addition Test, Controlled Oral Word Association, Finger Tapping Test, Wechsler Memory Scales, California Verbal Learning Test, Wechsler Adult Intelligence Tests, Boston Naming Test, and the Rey Osterreith Complex Figure, as well as associated subtests, for a total of 25 measures.
Nine of the 13 patients completed the entire neuropsychological test battery. The other four patients were unable to complete the battery and were excluded from the comparison between neuropsychological testing and MTR values but retained in the other analyses. The scores that fell within more than 1 SD from the mean were summed for each patient, and a total score obtained. Patients were ranked according to scores on both the total number of measures (ie, among the total of 25 measures, patient 1 had the highest number of scores within more than 1 SD below normal) and on each individual measure. These total and individual scores were compared with the average regional MTR values using Spearman's rank correlation coefficient.
Results
The MTR values obtained from the healthy volunteers had an average value of 34.5 ± 1.9 (mean ± SD) in the pons and 34.3 ± 1.6 in the splenium of the corpus callosum, with an average of 34.4 ± 1.7 for all the white matter regions examined. Consistent with previous results, the regional values did not differ from one another, although there was a suggestion of a more diffuse distribution of values in the pons as compared with the splenium. Examination of contour plots revealed a relatively homogeneous distribution of MTR values in the splenium, in contrast to inhomogeneity observed in the pons.
With the average MTR values from the healthy group serving as a standard, ROIs placed in the splenium of the patients yielded demonstrably abnormal MTRs (more than 2 SD below normal) in two of 13 patients, although the grouped average of the splenium MTR values in patients was significantly different from normal by Student's t-test (P < .05). ROI analysis in the pons revealed MTR values to be significantly low (>2 SD below normal) in only one of 13 patients, and the grouped values were not significantly different. An example of an MTI of the splenium is shown in Figure 2.
fig 2.
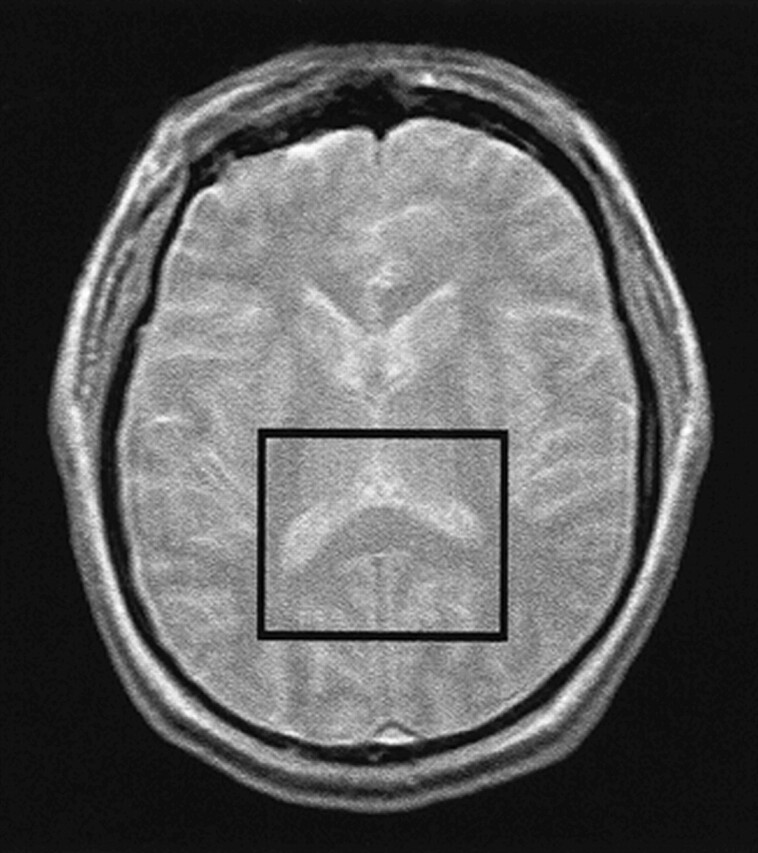
MT image of an axial section at the level of the splenium, with superimposed box to indicate the region of detailed analysis by contour plotting, as exemplified in figure 3
Examination of the contour plots suggested a greater sensitivity in detecting specific areas of lowered MTRs that may have been averaged out by the ROI procedure. Four of the 13 patients had abnormal areas of reduced MTR values (at least2 SD below normal) that were clearly visible in homogeneous regions of the splenium with the contour plots, as exemplified in Figures 2 and 3. This group included all who had below-normal composite regional MTR values. No abnormalities were detected in the control population upon examination of the splenium area with the use of contour plots. The pontine region in both the volunteers and the patients was considered too heterogeneous for evaluation with contour plots.
The results of the 25 measures in the neuropsychological test battery were compared with regional MTR values. Spearman rank correlation coefficients revealed a moderate correlation (r = .59) between one of the California Verbal Learning Test measures (Recognition Hits) and the MTR value for the splenium and between the Wechsler Memory Scale-Visual Span Forward subtest and the MTR value for the pons (r = .58). All nine patients studied with neuropsychological testing were classified as impaired on the basis of results of the test battery, as each had scores between 3 and 15 (average, 9), which were more than 1 SD below the norm. Among all patients, 70% had more than 30% of their measures in the impaired range.
Discussion
To assess the consequences of mild TBI, objective diagnostic and prognostic measures are needed. Neuropsychological testing can provide essential information concerning cognitive status; however, these tests may also be sensitive to factors not directly related to the cognitive sequelae of the injury, such as pain, situational stress, emotional adjustment, age, and education, all potentially interfering with the assessment. Thus, it may not be possible to assess the severity of brain injury solely by the extent of impairment gauged by neuropsychological tests (6). Imaging techniques, such as CT, MR spectroscopy (10), and MR imaging, have been used to assess the extent of TBI through the detection of physiological abnormalities of tissue in various parts of the brain. MR imaging has proved useful in the evaluation of patients with severe head injury in whom CT failed to depict an anatomic discrepancy indicative of severe injury (11) as well as in the characterization of the frequency and nature of brain stem injury (12). Conventional imaging techniques have generally proved insensitive to the detection of abnormalities associated with mild TBI in patients with persistent cognitive deficits. In contrast, preliminary work using MTI has shown promise in the detection of diffuse axonal injury in both animal and human studies (4, 5, 9). Results of studies in an animal model of rotational acceleration injury suggested that quantitative MTI offered increased sensitivity to histopathologically proved damage as compared with conventional MR imaging techniques. Parallel studies in a cohort of patients with moderate to severe head injuries yielded encouraging findings and also suggested a possible future diagnostic role for quantitative MTI in a similar population (9). These and other studies in human degenerative brain disease (8, 13–15) were based on the hypothesis that microscopic changes in the structural status of the brain, undetectable via conventional MR techniques, can be identified with changes in MT measures.
There exists a paradox in the study of mild head injury in that, despite results in the normal range on standard diagnostic tests, patients report persistent deficits related to cognition. In a study of 26 patients with minor head injury, defined as warranting overnight stay in the hospital but with posttraumatic amnesia of less than 12 hours, brain stem auditory evoked potentials were obtained upon admission and again at 6 weeks after the injury. Results suggested that the postconcussion syndrome followed three different courses. The first of these, experienced by more than 50% of the patients, was characterized by recovery within 6 weeks; approximately half these patients had normal evoked potentials immediately after the injury. The second course was characterized by persistent brain stem dysfunction over 6 months, and the third course by an increase in symptoms over a 6-month period but largely without evidence of brain stem dysfunction. The authors suggested that their findings represented both cortical and brain stem damage from minor head injury, with the brain stem damage being more persistent (16). These findings are consistent with our detection of abnormal brain tissue in some, but not all, patients who were judged to be cognitively impaired.
A challenge to the study of mild head injury is that patients may be unaware of a cognitive deficit (3). On the other hand, after a traumatic head injury, a patient might be overly sensitive to the presence of a cognitive problem, attributing, for example, a transient memory difficulty to the injury. This may have medicolegal implications when a patient is attempting to substantiate a claim of long-term injury in the face of negative imaging results. In any case, such deficits are difficult to quantify and characterize by diagnostic tools currently available. Finally, patients may conceal or deny cognitive difficulties because of the societal stigma attached to disorders of mentation. In this regard, our study was expected to be self-selective to some degree of more seriously affected patients who were still within the mild or minor injury definition. Study of a broader group of patients with mild head trauma, including those without complaints of cognitive difficulties, is a logical next step.
The distinction between normal tissue and tissue injured as a result of minor head trauma was established by the use of statistical measures in both the splenium and the pons and by statistically based contour plots only in the splenium. Our results indicate that this approach might have more validity than would a comparison of group averages in patients in whom inclusion of normal tissue in the averages might mask the presence of an abnormality. The contour plotting technique is designed to provide a tool to be applied on a case-by-case basis, but it also relies on careful incorporation of control data to support the significance of the result. In the homogeneous splenium, evidence of the validity of this approach is supported by current state-of-the-art quantitative MTI. On the other hand, the inherent heterogeneity of pontine tissue, in which gray matter structures (such as nuclei of the tegmentum of the pons) are interspersed between regions of white matter, limited the usefulness of the MTI technique in this study of subtle damage. Future work is indicated to more carefully evaluate the characteristics of the normal pons from the standpoint of quantitative MTI. It is possible that regional or global histographic analysis may overcome some of the problems we encountered in that structure (17).
A physiological explanation for lowered MTR in head trauma has not been positively established. Patients who have experienced moderate to severe head injury have been shown to have neuropathologic and imaging evidence of diffuse axonal injury (white matter shearing) (3, 12). Models of the MT effect predict alteration of MTR consequent to the presence of edema (via changes in relaxation times) but they also predict structural alterations such as, but not limited to, demyelination (via changes in molecular ratios and exchange rates) (18, 19). Several studies in animal models and in human disease have established a link between microscopic alterations of brain structures (terminal clubs and axonal swelling) and changes in MT contrast (4); and recent findings of neuronal transection in patients with multiple sclerosis (20) suggest a link with reports of lowered MTR in normal-appearing white matter (8). In a study of wallerian degeneration, it was noted that a bimodal pattern of MTR change followed unilateral enucleation in a cat model (21). A decrease in MTR was reported in edematous lesions of experimental autoimmune encephalomyelitis, an animal model of multiple sclerosis, as well as in human studies of multiple sclerosis (8, 22, 23). These findings are consistent with others discussed above and are related to head trauma (4, 9). In general, it has been shown that the extent of abnormality usually increases as the MTR values decrease (24–26). Thus, although the precise mechanism(s) for MTR reduction have not been elucidated for mild head trauma, there is considerable evidence of a link between tissue abnormality and lowered MTR, and a reasonable argument for the supposition that lower MTR portends a less-favorable outcome. With regard to the subtlety of the findings and their clinical significance, it is known that lesions in these locations are frequently associated with significant cognitive difficulties. While the abnormalities we have detected may not represent the entire extent of brain injury, it is not surprising that such lesions are associated with dysfunction.
Although a correlation between MTR values and results of neuropsychological analysis was found for only two individual tests, it is possible that potential correlations were masked by partial volume effects of the ROI methodology. It is also possible, although unlikely given the contour plot results, that the significant correlations were artifacts of the repeated comparisons made necessary by the design of the neuropsychological testing. A more likely explanation is that the diversity of injuries in this small sample resulted in a variety of demonstrated neuropsychological impairments. Future work targeting specific injury mechanisms or classifications may thus be indicated. Finally, any lack of correlation between a particular neuropsychological test and MTI results may reflect the targeting of neuropsychological tests to specific cognitive functions of gray matter, whereas the MTR analysis was carried out wholly in white matter. A regional analysis to overcome this problem is not currently feasible, as spatial localization of neurocognitive testing to specific areas of the brain is inexact, and the details of connecting pathways and their roles in cognition have not been established.
Some individual results were suggestive of the diagnostic or prognostic potential of this technique. For example, the most abnormal MTR values were detected in a recent PhD recipient who had experienced a mild TBI but was found on examination to have a significant memory deficit and an executive function deficit. Her exceptional intellect and ability to compensate for deficits might have obscured some of her clinical test results, producing some average scores that, while not appearing decreased, may have represented a significant decrement in functioning for this patient. This is particularly relevant given the negative findings on conventional imaging studies. Another patient with significantly lowered MTR showed impaired auditory attention as well as concentration. Results of previous studies suggest that these abnormalities may very well reflect parenchymal injury (3).
The results of this study suggest a future role for MTR-based analysis in imaging-supported diagnosis of mild head trauma but also potentiate the development of a grading system that may be used to predict the extent of injury. A correlation between MTR abnormality and successively more serious injury by clinical reference standards would confirm the need for a method to predict the extent of injury by assessing areas of abnormal MTR values. Potential application of these techniques could include evaluation of new pharmaceutical agents for the treatment of TBI.
Conclusion
Quantitative MTI analysis can detect abnormalities associated with mild head trauma that are undetectable on routine MR images but that are consistent with results of neurocognitive test results in some patients. Our findings suggest that such analysis may represent an advantage in specificity over conventional MR studies. The potential value of the proposed MTI technique includes its use in diagnosis as well as prognosis. We speculate that further refinements of this application may enhance the reproducibility of the analysis and aid in the discrimination of smaller abnormalities.
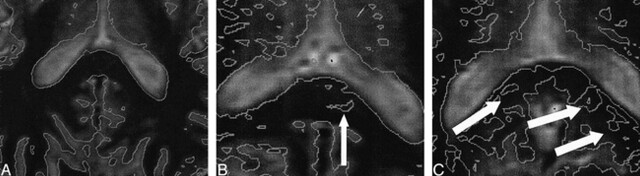
fig 3.
A, Detail of an MT-weighted image overlaid with contours corresponding to 2 SD below normal white matter MTR. The image in the axial plane shows the region of the splenium in a healthy volunteer.
B, MT contour map of a patient with TBI shows a region of MTR lowered in excess of 2 SD below normal (arrow). This patient had a pattern of cognitive weakness and impairments consistent with TBI, including fluctuating auditory attention and impaired sustained attention and visual concentration.
C, MT contour map of a different patient with TBI shows multiple regions (arrows) of abnormality. This patient had impairments consistent with TBI, including deficits in executive function and delayed short-term memory.
Footnotes
Address reprint requests to Joseph C. McGowan, PhD, Department of Radiology, University of Pennsylvania, 3400 Spruce St, Philadelphia, PA 19104.
Presented at the annual meeting of the International Society of Magnetic Resonance in Medicine, Sydney, Australia, April 1998.
Supported in part by NIH grants NS34353, NS29029, and NS08803.
References
- 1.Gilroy J, Basic Neurology. 2nd ed. New York: Pergamon Press 1982:329-351 [Google Scholar]
- 2.Long C, Ross L, Handbook of Head Trauma: Acute Care to Recovery.. New York: Plenum Press;1992
- 3.Mittl R, Grossman R, Hiehle J, et al. Prevalence of MR evidence of diffuse axonal injury in patients with mild head injury and normal head CT findings. AJNR Am J Neuroradiol 1994;15:1583-1589 [PMC free article] [PubMed] [Google Scholar]
- 4.McGowan JC, McCormack TM, Grossman R, et al. Diffuse axonal pathology detected with magnetization transfer imaging following brain injury in the pig. Magn Reson Med 1999;41:727-733 [DOI] [PubMed] [Google Scholar]
- 5.Kimura H, Meaney DF, McGowan JC, et al. Magnetization transfer imaging of diffuse axonal injury following experimental brain injury in the pig: characterization by magnetization transfer ratio with histopathologic correlation. J Comput Assist Tomogr 1996;20:540-546 [DOI] [PubMed] [Google Scholar]
- 6.Kibby M, Long C. Minor head injury: attempts at clarifying the confusion. Brain Injury 1996;10:159-186 [DOI] [PubMed] [Google Scholar]
- 7. American College of Rehabilitation Medicine. Definition of mild traumatic brain injury. J Head Trauma Rehabil 1993;8:86-88 [Google Scholar]
- 8.Dousset V, Grossman RI, Ramer KN, et al. Experimental allergic encephalomyelitis and multiple sclerosis: lesion characterization with magnetization transfer imaging [published erratum appears in Radiology. 1992;183:878 ]. Radiology. 1992;182: 483-491 [DOI] [PubMed] [Google Scholar]
- 9.Bagley L, McGowan J, Grossman R, et al. Magnetization transfer imaging of traumatic brain injury: a predictor of patient outcome. J Magn Reson Imaging 2000;11:1-8 [DOI] [PubMed] [Google Scholar]
- 10.Cecil KM, Hills EC, Sandel ME, et al. Proton magnetic resonance spectroscopy for detection of axonal injury in the splenium of the corpus callosum of brain-injured patients. J Neurosurg 1998;88:795-801 [DOI] [PubMed] [Google Scholar]
- 11.Wilberger J, Deeb Z, Rothfus W. Magnetic resonance imaging in cases of severe head injury. Neurosurgery 1987;20:571-576 [DOI] [PubMed] [Google Scholar]
- 12.Gentry L, Godersky J, Thompson B. Traumatic brain stem injury: MR imaging. Radiology 1989;171:171-187 [DOI] [PubMed] [Google Scholar]
- 13.van Buchem MA, McGowan JC, Kolson DL, Polansky M, Grossman RI. Quantitative volumetric magnetization transfer analysis in multiple sclerosis: estimation of macroscopic and microscopic disease burden. Magn Reson Med 1996;36:632-636 [DOI] [PubMed] [Google Scholar]
- 14.Petrella JR, Grossman RI, McGowan JC, Campbell G, Cohen JA. Multiple sclerosis lesions: relationship between MR enhancement pattern and magnetization transfer effect. AJNR Am J Neuroradiol 1996;17:1041-1049 [PMC free article] [PubMed] [Google Scholar]
- 15.Filippi M, Campi A, Dousset V, et al. A magnetization transfer imaging study of normal-appearing white matter in multiple sclerosis. Neurology 1995;45:478-482 [DOI] [PubMed] [Google Scholar]
- 16.Montgomery E, Fenton G, McClelland R, MacFlynn G, Rutherford W. The psychobiology of minor head injury. Psychol Med 1991;21:375-384 [DOI] [PubMed] [Google Scholar]
- 17.van Buchem MA, Grossman RI, Armstrong C, et al. Correlation of volumetric magnetization transfer imaging with clinical data in MS. Neurology 1998;50:1609-1617 [DOI] [PubMed] [Google Scholar]
- 18.Henkelman RM, Huang X, Xiang Q, Stanisz GJ, Swanson S, Bronskill MJ. Quantitative interpretation magnetization transfer. Magn Reson Med 1993;29:759-766 [DOI] [PubMed] [Google Scholar]
- 19.McGowan JC, Leigh JS, Jr. Selective saturation in magnetization transfer experiments. Magn Reson Med 1994;32:517-522 [DOI] [PubMed] [Google Scholar]
- 20.Trapp B, Peterson J, Ransohoff R, Rudick R, Mork S, Bo L. Axonal transection in the lesions of multiple sclerosis. N Engl J Med 1998;338:278-285 [DOI] [PubMed] [Google Scholar]
- 21.Lexa FJ, Grossman RI, Rosenquist AC. MR of wallerian degeneration in the feline visual system: characterization by magnetization transfer rate with histopathologic correlation. AJNR Am J Neuroradiol 1994;15:201-212 [PMC free article] [PubMed] [Google Scholar]
- 22.Filippi M, Campi A, Martino G, Colombo B, Comi G. A magnetization transfer study of white matter in siblings of multiple sclerosis patients. J Neurol Sci 1997;147:151-153 [DOI] [PubMed] [Google Scholar]
- 23.Filippi M, Rocca MA, Martino G, Horsfield MA, Comi G. Magnetization transfer changes in the normal appearing white matter precede the appearance of enhancing lesions in patients with multiple sclerosis. Ann Neurol 1998;43:809-814 [DOI] [PubMed] [Google Scholar]
- 24.Hiehle JF Jr, Grossman RI, Ramer KN, Gonzalez-Scarano F, Cohen JA. Magnetization transfer effects in MR-detected multiple sclerosis lesions: comparison with gadolinium-enhanced spin-echo images and nonenhanced T1-weighted images. AJNR Am J Neuroradiol 1995;16:69-77 [PMC free article] [PubMed] [Google Scholar]
- 25.Hiehle JF Jr, Lenkinski RE, Grossman RI, et al. Correlation of spectroscopy and magnetization transfer imaging in the evaluation of demyelinating lesions and normal appearing white matter in multiple sclerosis. Magn Reson Med 1994;32:285-293 [DOI] [PubMed] [Google Scholar]
- 26.Gomori J, Grossman R, Asakura T, et al. An in-vitro study of magnetization-transfer and relaxation rates of hematoma. AJNR Am J Neuroradiol 1993;14:871-880 [PMC free article] [PubMed] [Google Scholar]