Abstract
BACKGROUND AND PURPOSE: Acute suppurative neck infections associated with branchial fistulas are frequently recurrent. In this study, we describe the imaging findings of acute suppurative infection of the neck caused by a third or fourth branchial fistula (pyriform sinus fistula).
METHODS: Imaging findings were reviewed in 17 patients (11 female and six male patients, 2 to 49 years old) with neck infection associated with pyriform sinus fistula. Surgery or laryngoscopic examination confirmed the diagnoses. Fourteen patients had a history of recurrent neck infection and seven had cutaneous openings on the anterior portion of the neck (all lesions were on the left side). Imaging studies included barium esophagography (n = 16), CT (n = 14), MR imaging (n = 2), and sonography (n = 3).
RESULTS: A sinus or fistulous tract was identified in eight of 16 patients on barium esophagograms. In 14 patients, CT studies showed the inflammatory infiltration and/or abscess formation along the course of the sinus or fistulous tract from the pyriform fossa to the thyroid gland. In nine patients, CT scans showed the entire course or a part of the sinus or fistulous tract as a tiny spot containing air. MR images showed a sinus or fistulous tract in two patients, whereas sonograms could not depict a sinus or fistulous tract in three patients. All 17 patients were treated with antibiotics. In one patient, the sinus tract was surgically excised, while 15 patients underwent chemocauterization of the sinus or fistulous tract with good outcome. Follow-up was possible for 16 of the 17 patients.
CONCLUSION: When an inflammatory infiltration or abscess is present between the pyriform fossa and the thyroid bed in the lower left part of the neck, an infected third or fourth branchial fistula should be strongly suspected.
Acute suppurative thyroiditis and thyroid abscess are extremely rare disorders. A rich blood supply, a generous lymphatic drainage, a high iodine level that inhibits bacterial growth, and a complete, protective fibrous capsule are factors that have been mentioned as contributing to the relatively high resistance of the thyroid gland to infection (1–5).
Congenital pyriform sinus fistula has recently been recognized as an underlying cause of acute suppurative thyroiditis or acute deep neck infection (5–13). The combination of a congenital sinus and acute suppurative thyroiditis was first described in the Japanese literature (7, 14, 15). In 1973, Tucker and Skolnick (6) described a patient with a recurrent left-sided neck abscess in whom a fistulous tract from the apex of the pyriform sinus to the lateral part of the neck was found. Several other, similar cases have been reported subsequently, which are now believed to be infections arising from an underlying congenital pyriform sinus fistula, probably a remnant of the third or fourth branchial pouch (7–13, 16–22). Most of these articles reported only a few cases of pyriform sinus fistula, with an emphasis on the surgical findings; only a few reports have emphasized the radiologic findings. We describe the imaging findings of congenital pyriform sinus fistula with neck infection in 17 patients.
Methods
The records of 17 patients seen at our institution between February 1993 and October 1998 for evaluation of neck infection, which proved to be an internal sinus or fistula originating from the pyriform sinus, were studied retrospectively. In all 17 patients, direct laryngoscopy revealed a sinus or fistulous opening into the pyriform sinus. In one case, the entire sinus tract was evident at surgery. The patients ranged in age from 2 to 49 years (mean age, 15 years); 11 patients were children and six were adults. Eleven patients were female and six were male. The most common presenting manifestation was neck swelling; 14 of the 17 patients had recurrent episodes of neck infection.
The patients underwent a variety of radiologic studies (CT, MR imaging, sonography, and barium esophagography). One patient had all of these examinations, 11 patients had CT and barium studies, and 15 patients had CT or MR imaging. In 14 patients, CT scans were obtained with 3- to 5-mm-thick sections and intravenous contrast material. Sixteen patients had a barium study, and three patients underwent sonography. MR imaging was performed in two patients by using a 1.0-T or 1.5-T scanner on which T1-weighted, T2-weighted, and fat-suppressed contrast-enhanced T1-weighted sequences were obtained.
Medical history, clinical manifestations, endoscopic findings, and results of the various imaging studies were investigated. All imaging studies were analyzed retrospectively by two experienced radiologists.
Results
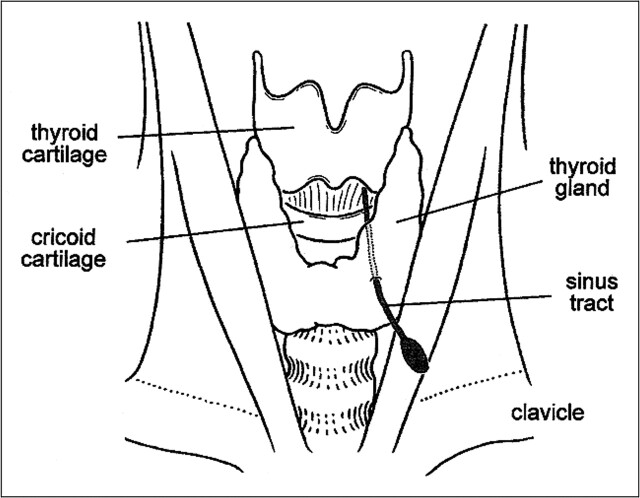
The lesions occurred on the left side of the neck in all patients. In all cases, the internal opening of the sinus or fistulous tract was confirmed by hypopharyngoscopy, and most originated from the apex of the pyriform sinus, posterior to the fold made by the internal laryngeal nerve. In one case, surgical excision of the entire sinus tract was performed. In this patient, the sinus tract originated from the apex of the pyriform sinus, passed through the thyroid gland, and terminated in perithyroid tissue (Fig 1).
FIG 1.
Schematic of a surgically proved sinus tract pathway from the pyriform sinus. The sinus originated from the apex of pyriform sinus, passed through the thyroid gland, and formed an abscess in perithyroid tissue
The CT scans (n = 14) showed disease extending from the pyriform sinus apex through the strap muscle layer to the thyroid or perithyroid tissue in all patients (Figs 2 and 3). In all patients, abnormal soft-tissue swelling and enhancement along the course of the disease were evident on CT scans. In eight patients, the lesions ended at the perithyroid level; in six patients, however, the lesions extended to the level of the clavicle. There were no cases involving the mediastinum lower than the sternal notch.
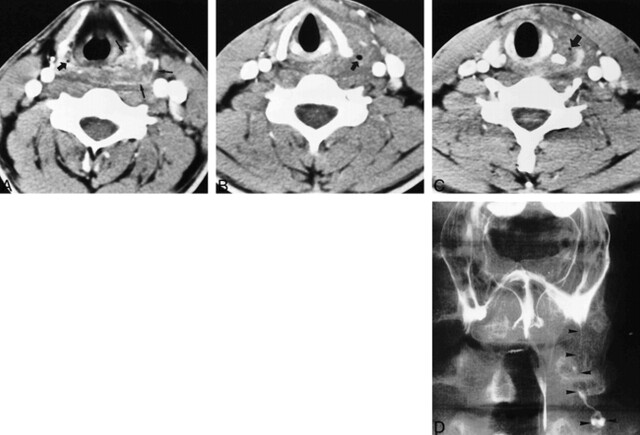
FIG 2.
24-year-old man with a recurrent episode of left-sided neck infection. The pyriform sinus fistula was diagnosed at hypopharyngoscopy.
A, Contrast-enhanced CT scan shows soft-tissue swelling and enhancement around the left pyriform sinus apex (thin arrows). Note the normal appearance of the right pyriform sinus apex (thick arrow).
B, CT scan shows diffuse soft-tissue swelling at the cricoid cartilage level. A small air density (arrow) is seen within the area of soft-tissue swelling.
C, CT scan at the level of the thyroid gland shows diffuse swelling of the thyroid gland and perithyroid soft tissue. The affected thyroid gland shows a poorly defined margin, hypodensity, and a focus of air (arrow).
D, Anteroposterior view from a barium swallow reveals the sinus tract (arrowheads) originating from the pyriform sinus apex and terminating in a focal collection near the left supraclavicular region.
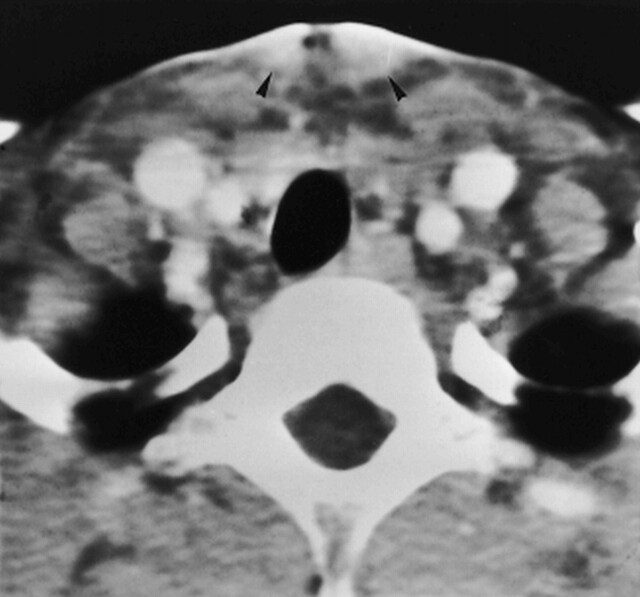
The involved pyriform sinus fossae were deformed by adjacent soft-tissue inflammation in all patients (Figs 2 and 3). Six patients had cutaneous openings in the left anterior portion of the neck, adjacent to skin thickening and enhancement seen on the CT scans (Fig 4). Thirteen patients had thyroid gland involvement, including swelling of the thyroid gland, poor definition of the thyroid margin, and loss of high attenuation of the affected lobe on CT scans after contrast enhancement (Fig 2).
FIG 4.
9-year-old girl with recurrent episodes of left-sided neck infections. Every episode was managed with antibiotics and abscess drainage. On CT scan, the skin adjacent to the cutaneous opening is thickened and enhances (arrowheads). The pyriform sinus fistula was diagnosed at hypopharyngoscopy. The cause of the sinus tract connection to the skin surface may be either a rupture of the abscess cavity or a congenital fistulous tract, but the former is more likely
On CT scans, frank abscess formation was noted in nine patients (Fig 3), and gas was noted along the course of inflammation in nine patients. In four patients, gas was seen in the affected thyroid gland (Fig 2).
FIG 3.
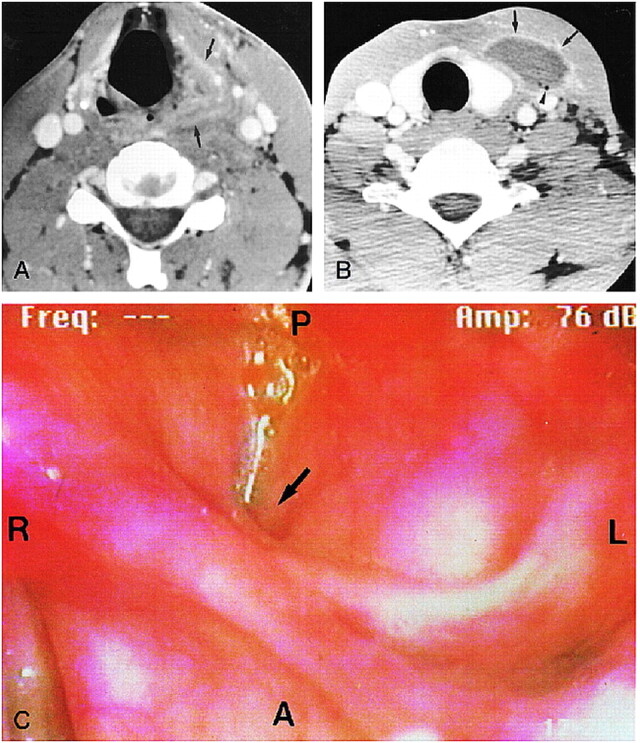
32-year-old man with a recurrent episode of left-sided neck infection.
A, CT scan shows diffuse swelling and enhancement of the soft-tissue plane (arrows) around the left pyriform fossa.
B, Axial contrast-enhanced CT scan shows an abscess in the perithyroid tissue (arrows). Note the focus of air density in the perithyroid abscess (arrowhead).
C, Hypopharyngoscopic study reveals a sinus opening at the pyriform sinus apex (arrow) with a view from above and anterior toward the bottom. R indicates right; L, left; A, anterior; P, posterior.
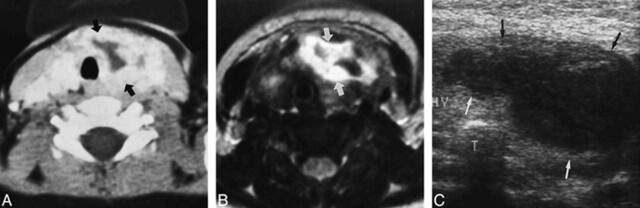
MR images, obtained in two patients, showed the same disease course as did the CT scans. In one patient, the lesion ended at the perithyroid tissue, and in the other, who was examined with both CT and MR imaging, the lesion extended to the level of the clavicle. MR images showed soft-tissue inflammation along the disease course, with intermediate signal intensity on T1-weighted images and high signal intensity on T2-weighted images and on fat-suppressed T1-weighted images after IV administration of contrast material. One of the two patients had a cutaneous opening in the left anterior portion of the neck, accompanied by skin thickening and enhancement. Involvement of the thyroid gland was seen in one patient (Fig 5). Gas density was seen in one patient, but the conspicuity of air was less visible than on CT scans, and the ability to distinguish air from a vascular signal void was difficult. In the 15 patients who had either CT or MR examinations, an inflammatory lesion was well depicted along the disease course of the sinus or fistulous tract from the left pyriform sinus apex to the left perithyroid tissue or to the more inferior lower portion of the neck, even though the sinus or fistulous tract itself was not clinically apparent.
FIG 5.
2-year-old girl with a first episode of neck abscess. The pyriform sinus fistula was diagnosed at hypopharyngoscopy.
A, Contrast-enhanced CT scan shows an abscess (arrows) in the left thyroid and perithyroid tissue.
B, T2-weighted MR image (2000/90/2 [TR/TE/excitations]) shows a collection of high signal intensity (arrows) at the same region as in A.
C, Sonogram shows a hypoechoic mass (arrows) consistent with the abscess in the left perithyroid tissue, but the sinus tract is not visible.
Sonography, performed in three patients, revealed hypoechoic lesions involving the left thyroid or perithyroid area, but could not depict a sinus or fistulous tract. This imaging technique was limited to evaluation of the hypopharyngeal lesion (Fig 5).
Barium studies, obtained in 16 patients, showed the sinus or fistulous tracts in eight cases (Fig 2). The proximal portion of the sinus or fistulous tract, extending from the apex of the pyriform sinus, was partially visible in six patients. In two of the eight patients, the entire course of the fistula was depicted.
All 17 patients were managed with antibiotic therapy. Fifteen patients underwent chemocauterization of the sinus or fistulous opening with 20% or 40% trichloracetic acid (TCA) solution. In 12 of the 15 patients, no recurrent neck infection occurred after chemocauterization; in the other three patients, recurrent disease developed, but additional chemocauterization was performed with good outcome. The follow-up period ranged from 3 months to 6 years. One of the patients treated with antibiotics was lost to follow-up.
Discussion
Congenital pyriform sinus fistula has been recognized as an underlying cause of acute suppurative thyroiditis or acute deep neck infection (5–13). Taylor et al (3), on the basis of the following facts, suggested that many of the reported cases of acute suppurative thyroiditis might have been caused by an unrecognized fourth branchial pouch sinus tract: 83% were left-sided, 66% occurred after acute illness involving the upper respiratory tract, and the rate of recurrence was relatively high (39%). In most cases, the sinus tract began from the apex of the pyriform sinus and coursed anteroinferiorly, either beside or through the thyroid gland, into the perithyroid space. In a summary of previously reported cases, Gordin et al (16) noted that the prevalence of left-sided disease in pyriform sinus fistula was 93%, higher than the 83% figure reported by Taylor et al (3). In our series, all the lesions were left-sided, and most of them manifested as repeated neck swelling, which was consistent with earlier reports.
The embryologic origin of the pyriform sinus fistula is controversial. The third and fourth pharyngeal pouches form the pyriform. Persistent ducts from either of these pharyngeal pouch sinuses may drain into the pyriform sinus (10, 21). According to Burge and Middleton (22), the third pouch fistula drains anterior to the fold made by the internal laryngeal nerve; the fourth pouch fistula drains posterior to this fold. In most of our cases, the sinus or fistula began at the apex of the pyriform sinus, posterior to this fold, thus supporting the theory of the fourth pouch origin. The ventral portion of the fourth pharyngeal pouch develops into the ultimobranchial body, which fuses with the thyroid gland and subsequently disseminates to give rise to the C cell (23). This may explain the close relationship between the fistula and the thyroid gland. However, the fact that the superior parathyroid gland, the major derivative of the fourth pharyngeal pouch, has no relationship with the sinus or fistula argues against this theory.
Embryologically, the left fourth branchial arch artery forms part of the aortic arch, while the right one becomes the right subclavian artery (16, 24–26). The embryologic asymmetry in the normal development of the lower part of the neck may therefore be related to the noted left-sided predominance of the fistula. The left-sided predominance may correspond to the fourth pouch origin of this condition.
CT or MR imaging is often the radiologic study of choice in cases of suspected deep neck infection. In our study, the cross-sectional imaging findings of pyriform sinus fistula with infection included inflammation of the pyriform sinus, strap muscle layer, thyroid gland, and perithyroid area, with or without infrahyoid gas and fluid accumulation. The pathway of pyriform sinus fistula seen on CT or MR studies was characteristic. It began at the pyriform sinus apex, coursed anteroinferiorly through the strap muscle layer, either beside or through the thyroid gland, and into the perithyroid space. In seven patients, the lesion extended to the level of the clavicle. This anatomy is exactly the same as that described by Gordin et al (16), and is the most characteristic imaging feature of this disease.
Both CT and MR studies were excellent in delineating inflammatory lesions along the tract, even though the sinus or fistulous tract was not clinically apparent. But CT was superior in detecting air density at the sinus or fistulous tract as well as in depicting thyroid gland involvement as a loss of high density in the affected thyroid gland. The resolution of CT is also superior to that of MR imaging. For these reasons, we believe that CT is the preferred method for evaluating the sinus or fistulous tract and its complications.
Extrapharyngeal air densities in the infrahyoid portion of the neck were noted in nine of 14 patients on CT scans and in one patient on MR images. The air was due to either communication with the pyriform sinus or frank abscess. Bar-Ziv et al (13) reported a higher rate of gas in the neck using the air-contrast technique.
Several authors (2, 7, 8) have advocated barium esophagography as an effective means of demonstrating the presence of a sinus or fistulous tract originating from the left pyriform sinus. In our series, however, the sinus or fistulous tract was demonstrated in only eight of the 16 patients who had a barium study. This may be a result of closure of the fistulous tract due to inflammation or reactive edema in the acute phase of infection. As Miller et al (2) pointed out, if a barium study is to be successful, the existing infection must be cleared by appropriate antibiotics before the examination.
In 1990, Hatabu et al (11) described the sonographic findings of this condition. On sonograms, the left-sided perithyroid hypoechoic area infiltrating the thyroid grand was thought to be an abscess caused by bacterial infection. In our cases, the sonographic findings were the same as those reported by Hatabu et al. Compared with CT or MR imaging, sonography was limited in its ability to depict the hypopharyngeal lesions or disease course.
Seven of our patients had cutaneous openings in the left anterior portion of the neck. Har-El et al (5) believed that a sinus tract arising from the pyriform sinus was a pure branchial pouch remnant. These authors concluded that the lesion was a sinus tract with or without a cyst, but not a fistula, since the cyst, the thyroid gland, and the pyriform sinus were all of endodermal origin, and no preformed ectodermal tract to the skin occurs. The infected cyst may connect itself to the skin surface, but only via a rupture of the abscess cavity, as may happen with any other abscess (5).
Pyriform sinus fistula and its associated infection are seen predominantly in children, but they may also occur in adults. Two thirds of our patients were children; but a third of the patients were adults, a figure also noted in other reports (2–20).
It is generally agreed that pyriform sinus fistula, including the entire tract and involved area of the thyroid, must be completely excised to achieve a definitive cure. Chemotherapy or drainage of the infection may also be required (19). Although complete excision is accepted as the best method for treating a pyriform sinus fistula, it is not easy to completely excise the whole tract, because repeated infection and previous surgery often make complete dissection of the tract hazardous, and at times impossible. Fifteen patients in our series were treated by chemocauterization of the internal sinus or fistula opening with 20% to 40% TCA, resulting in a relatively good outcome; there was no recurrent infection in 12 (80%) of 15 patients treated by chemocauterization. The rationale for this management is as follows: 1) in most cases, complete excision is very difficult and requires a wide excision; 2) in almost all cases, recurrent neck abscess follows upper respiratory infection, suggesting that spoilage from the pharyngeal secretion may be the direct cause of abscess; 3) even when this procedure fails, there still remains the opportunity to perform a total excision; and 4) all the patients who underwent this procedure were managed satisfactorily, with no scar, no prolonged anesthesia, little morbidity, and early discharge.
Conclusion
Suppurative neck infection associated with a congenital pyriform sinus fistula is a rare disorder, but has a characteristic location along the course of the sinus or fistula. When an inflammatory infiltration or abscess is present in the lower left portion of the neck, from the pyriform fossa to the thyroid bed, an underlying third or fourth branchial fistula should be strongly suspected. CT is a useful method for visualizing the sinus or fistulous tract and for evaluating the extent of the lesion. An accurate imaging diagnosis will facilitate the appropriate treatment and prevent recurrence of the infection. TCA chemocauterization of the internal opening of the pyriform sinus fistula can be an effective alternative mode of therapy, and can be successfully used in most patients, at least initially.
Footnotes
Address reprint requests to Moon Hee Han, MD, Department of Diagnostic Radiology, Seoul National University Hospital, 28 Yongon-Dong, Chongno-Ku, Seoul 110-744, Korea.
References
- 1.Womack NA, Cole WH. Thyroiditis. Surgery 1944;16:770-782 [Google Scholar]
- 2.Miller D, Hill JL, Sun CC, et al. The diagnosis and management of pyriform sinus fistula in infants and young children. J Pediatr Surg 1983;18:377-381 [DOI] [PubMed] [Google Scholar]
- 3.Taylor WE, Myer CM, Hays LL, et al. Acute suppurative thyroiditis in children. Laryngoscope 1982;92:1264-1273 [DOI] [PubMed] [Google Scholar]
- 4.Szego PL, Levy RP. Recurrent acute suppurative thyroiditis. Can Med Assoc J 1970;103:631-633 [PMC free article] [PubMed] [Google Scholar]
- 5.Har-El G, Sasaki CT, Prager D, Krespi YP. Acute suppurative thyroiditis and the branchial apparatus. Am J Otolaryngol 1991;12:6-11 [DOI] [PubMed] [Google Scholar]
- 6.Tucker HM, Skolnick ML. Fourth branchial cleft (pharyngeal pouch) remnant. Trans Am Acad Ophthalmol Otolaryngol 1973;77:368-371 [PubMed] [Google Scholar]
- 7.Takai SI, Miyauchi A, Matsuzuka F, Kuma K, Kosaki G. Internal fistula as a route of infection in acute suppurative thyroiditis. Lancet 1979;1:751-752 [DOI] [PubMed] [Google Scholar]
- 8.Ueda J, Kobayashi K, Kishino B, Fushimi H, Sawada S. Routes of infection of acute suppurative thyroiditis diagnosed by barium examination. Acta Radiol Diagn 1986;27:209-211 [DOI] [PubMed] [Google Scholar]
- 9.Tovi F, Gatot A, Bar-Ziv J, Yanay I. Recurrent suppurative thyroiditis due to fourth branchial pouch sinus. Int J Pediatr Otorhinolaryngol 1985;9:89-96 [DOI] [PubMed] [Google Scholar]
- 10.Miyauchi A, Matsuzuka F, Kuma K, Takai SI. Piriform sinus fistula: an underlying abnormality common in patients with acute suppurative thyroiditis. World J Surg 1990;14:400-405 [DOI] [PubMed] [Google Scholar]
- 11.Hatabu H, Kasagi K, Yamamoto K, et al. Acute suppurative thyroiditis associated with piriform sinus fistula: sonographic findings. AJR Am J Roentgenol 1990;155:845-847 [DOI] [PubMed] [Google Scholar]
- 12.Lukaya J, Berdon WE, Enriquez G, Regas J, Carreno JC. Congenital pyriform sinus fistula: a cause of acute left-sided suppurative thyroiditis and neck abscess in children. Pediatr Radiol 1990;21:27-29 [DOI] [PubMed] [Google Scholar]
- 13.Bar-Ziv J, Slasky BS, Sichel JY, Lieberman A, Kats R. Branchial pouch sinus tract from the piriform fossa causing acute suppurative thyroiditis, neck abscess, or both: CT appearance and the use of air as a contrast agent. AJR Am J Roentgenol 1996;167:1596-1572 [DOI] [PubMed] [Google Scholar]
- 14.Hiroto K, Shigyo H. Two cases of an atypical lateral cervical fistula. Jibirinsho 1957;50:140-145 [Google Scholar]
- 15.Inagaki H, Kobori O, Ishikawa K. A study on internal fistula originating from the fourth branchial pouch. Nippon Geka Gakkai Zasshi 1976;77:137-138 [Google Scholar]
- 16.Gordin MS, Kearns DB, Pransky SM, Seid AB, Wilson DB. Fourth branchial pouch sinus: principles of diagnosis and management. Laryngoscope 1990;100:174-178 [DOI] [PubMed] [Google Scholar]
- 17.Rosenfeld RM, Biller HF. Fourth branchial pouch sinus: diagnosis and treatment. Otolaryngol Head Neck Surg 1991;105:44-50 [DOI] [PubMed] [Google Scholar]
- 18.Takimoto T, Yoshizaki T, Ohoka H, Sakashita H. Fourth branchial pouch anomaly. J Laryngol Otol 1990;104:905-907 [DOI] [PubMed] [Google Scholar]
- 19.Naobumi N, Ikarashi F, Fujisaki T, Nakato Y. Surgical approach to pyriform sinus fistula. Am J Otolaryngol 1993;14:111-115 [DOI] [PubMed] [Google Scholar]
- 20.Yamashita H, Noguchi T, Takahashi M. Recurrent cervical abscess due to piriform sinus fistula. J Laryngol Otol 1995;109:886-888 [DOI] [PubMed] [Google Scholar]
- 21.Raven RW. Pouches of the pharynx and esophagus with special reference to the embryological and morphological aspects. Br J Surg 1933;21:235 [Google Scholar]
- 22.Burge D, Middleton A. Persistent pharyngeal pouch derivative in the neonate. J Pediatr Surg 1983;18:230-234 [DOI] [PubMed] [Google Scholar]
- 23.Moore KL. The Developing Human. 3rd ed. Philadelphia: Saunders 1982;187
- 24.Liston SL. Fourth branchial fistula. Otolaryngol Head Neck Surg 1981;89:520-522 [DOI] [PubMed] [Google Scholar]
- 25.Benson M, Dalen K, Mancuso AA, Kerr HH, Cacciarelli AA, Mafee MF. Congenital anomalies of the branchial apparatus: embryology and pathologic anatomy. Radiographics 1992;12:943-960 [DOI] [PubMed] [Google Scholar]
- 26.Proctor B. Lateral vestigial cysts and fistula of the neck. Laryngoscope 1955;65:355-401 [DOI] [PubMed] [Google Scholar]