Abstract
BACKGROUND AND PURPOSE: Passing from the supine to the upright position favors cerebral venous outflow into vertebral venous systems rather than into the internal jugular veins. We sought to determine venous connections between dural venous sinuses of the posterior cranial fossa and craniocervical vertebral venous systems.
METHODS: Corrosion casts of the cranial and cervical venous system were obtained from 12 fresh human cadavers, and anatomic confirmation was made by dissection of three previously injected fresh human specimens. MR venography was performed to provide radiologic correlation.
RESULTS: The lateral, posterior, and anterior condylar veins and the mastoid and occipital emissary veins were found to represent the venous connections between the dural venous sinuses of the posterior cranial fossa and the vertebral venous systems. This study revealed the nearly constant presence of the anterior condylar confluent (ACC) located on the external orifice of the canal of the hypoglossal nerve. The ACC offered multiple connections with the dural venous sinuses of the posterior cranial fossa, the internal jugular vein, and the vertebral venous system. All these structures were shown by MR venography.
CONCLUSION: The lateral, posterior, and anterior condylar veins and the mastoid and occipital emissary veins connect the dural venous sinuses of the posterior cranial fossa with the vertebral venous systems. These connections are clinically relevant, because encephalic drainage occurs preferentially through the vertebral venous system in the upright position. The ACC is a constant anatomic structure that may play an important role in the redirection of cerebral blood in the craniocervical region.
Most of the cerebral venous drainage collects ultimately into the transverse and sigmoid sinuses of the skull base. In the supine position, cerebral venous drainage occurs primarily through the internal jugular veins, as seen on venous-phase cerebral angiograms (1). However, several authors have shown that the internal and external vertebral venous systems (2–5) represent the major outflow track of cerebral venous drainage in the erect position and that outflow through the internal jugular veins is absent or negligible in this position (6–9).
Whereas the pathway from the dural sinuses of the posterior fossa into the internal jugular veins is anatomically obvious through the jugular foramen, connections with the vertebral plexus are numerous and complex. Several authors have stressed the importance of the emissary veins of the posterior cranial fossa (10, 11); in particular, the anterior and posterior condylar and mastoid emissary veins.
Recently, Arnautovic et al (12) studied the microsurgical anatomy of the venous plexus surrounding the horizontal portion of the third segment of the vertebral artery, which they named the suboccipital cavernous sinus. In their study, the authors emphasized the importance of the internal and external vertebral venous plexus in the cerebral drainage, particularly the role played by the suboccipital cavernous sinus in connecting indirectly the internal vertebral venous plexus to the dural venous sinuses of the skull base.
Classical anatomic dissections of the craniocervical region are difficult because of difficult access to the skull base and anatomic complexity. Angiographic studies might fail to show certain tributaries because of countercurrent blood flows (13) and because they are performed only with the patient in the supine position. These technical limitations might explain why the current descriptions of the venous anatomy of the craniocervical region often remain fragmentary and incomplete. For instance, the radiologic and surgical literature does not mention, to our knowledge, the anterior condylar confluent (ACC). This venous confluent is located extracranially in front of the aperture of the hypoglossal canal and was described by Trolard as far back as 1868 (14). We, therefore, undertook a vascular corrosion cast study supplemented by anatomic dissections and MR phlebography imaging, aimed at showing the possible connections between the cerebral venous circulation and the cervical outflow tracks.
Methods
The cerebral, neurocranial, and cervical venous systems were studied by using vascular corrosions. These allow for visualization of venous structures that would otherwise be difficult to reliably observe by performing standard anatomic dissections, even after previous vascular injection.
Corrosion Cast
Corrosion casts of the cranial, cerebral, and cervical venous system were obtained from 12 nonfixed human cadavers from our anatomy institute (eight female and four male cadavers; average age at time of death, 85 years). In each case, the internal jugular veins were carefully dissected in the neck and cannulated with 6-mm metallic probes. The venous system was then rinsed with a saline solution, which also allowed for identification and ligature of possible leak points. A mixture of methylmethacrylate (Beracryl; Troller, Fulenbach, Switzerland) and barium sulfate powder (HD 200 plus; Lafayette, Anaheim, CA) was then injected through both internal jugular veins until the angular veins became engorged. The specimens were then placed in a bath of 40% potassium hydroxide solution at a constant temperature of 40°C until all surrounding soft and bony tissues were dissolved. The connections between the sigmoid-transverse sinuses, internal jugular veins, and internal and external vertebral venous plexuses were then studied.
Standard Anatomic Dissection
Corrosion cast findings were compared with standard dissection findings of three fresh cadavers (two female and one male cadaver; average age at time of death, 82 years). Venous filling before dissection was obtained, as described above, for the corrosion casts. The skull was then opened by circular craniotomy, and the brain was removed. The veins around the internal and external surfaces of the skull base were studied. Special attention was given to the region of the jugular foramen, hypoglossal and condylar canal, and atlanto-occipital region.
Imaging Studies
Standard radiographic images of the corrosion casts were obtained to illustrate the ideal angiographic appearance of the veins at the craniocervical junction. Imaging was obtained by using biplane angiographic equipment (BN3000; Philips, Best, the Netherlands) and standard anteroposterior and lateral projections.
An example of normal venous anatomy of the craniocervical region was also obtained by MR venography sequences of a healthy, 32-year-old female volunteer who provided informed consent. Two-dimensional time-of-flight gradient echo images with magnetization transfer were obtained with the following settings: 40/7 (TR/TE); field of view, 15 cm; 18; flip angle, 35 degrees; resolution, 220/256; section thickness, 1.5 mm; section overlap, 0.5 mm; matrix, 256 × 256 (1.5-T Eclipse System; Marconi Medical Systems, Cleveland, OH).
Results
Only the corrosion casts were used for the statistical analysis. Nine of the 12 corrosion casts (18 sides) showed filling of the entire intracranial venous system (ie, cerebral and neurocranial veins) and the cervical venous system. The three remaining casts showed filling of the neurocranial and cervical venous systems only, which we had set out to study.
Dural Sinuses
The transverse and sigmoid sinuses did not display any anomaly and were present in all casts (24 sides). An occipital sinus was noted in one case (Fig 1). The marginal sinus was noted in 10 casts (83.3% of the cases) and was not completely circular in seven of these cases, most likely because of incomplete filling. The marginal sinus connected anteriorly with the anterior condylar vein in all cases, and on one occasion, it bridged the anterior condylar vein with a suboccipital vein.
Fig 1.

Posterior view of a corrosion cast shows an occipital emissary vein (o) draining into the deep cervical veins and a left occipital sinus (p). Black arrowhead and white arrowhead, extracranial connection of the occipital emissary vein; b, transverse sinus; m, deep cervical vein.
Internal Vertebral Venous Plexus
The anterior internal vertebral venous plexus was present in all the cases and was particularly developed at the C1 and C2 vertebral levels (Figs 2A and 3A and B). It displayed communications with the vertebral artery venous plexus laterally (see below) and the anterior condylar vein cranially in all the cases studied. It also showed connections to the basilar plexus on nine occasions (37.5% of the sides) (Fig 2A).
Fig 2.
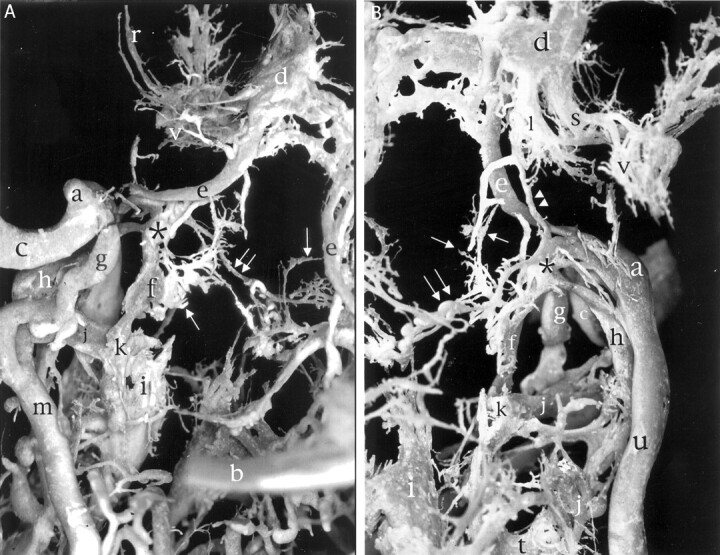
Left jugular bulb region. The ACC (asterisk) and its connections with surrounding veins are shown. The proximal portions of both transverse sinuses and confluens sinuum have been removed for better visualization. Double arrowhead, inferior petrooccipital vein; arrow, basilar plexus; double arrow, branch to prevertebral venous plexus; r, middle meningeal veins; d, cavernous sinus; a, superior jugular bulb; e, inferior petrosal sinus; c, sigmoid sinus; g, posterior condylar vein; h, lateral condylar vein; f, anterior condylar vein; j, vertebral artery venous plexus; k, anastomosis between anterior internal vertebral venous plexus and vertebral artery venous plexus; i, anterior internal vertebral venous plexus; m, deep cervical vein; b, transverse sinus; l, internal carotid artery venous plexus of Rektorzik; s, emissary vein of the foramen ovale; v, pterygoid plexus; t, intervertebral veins, including inter atlanto-occipital vein.
A, Posterior view.
B, Anterior view.
Fig 3.
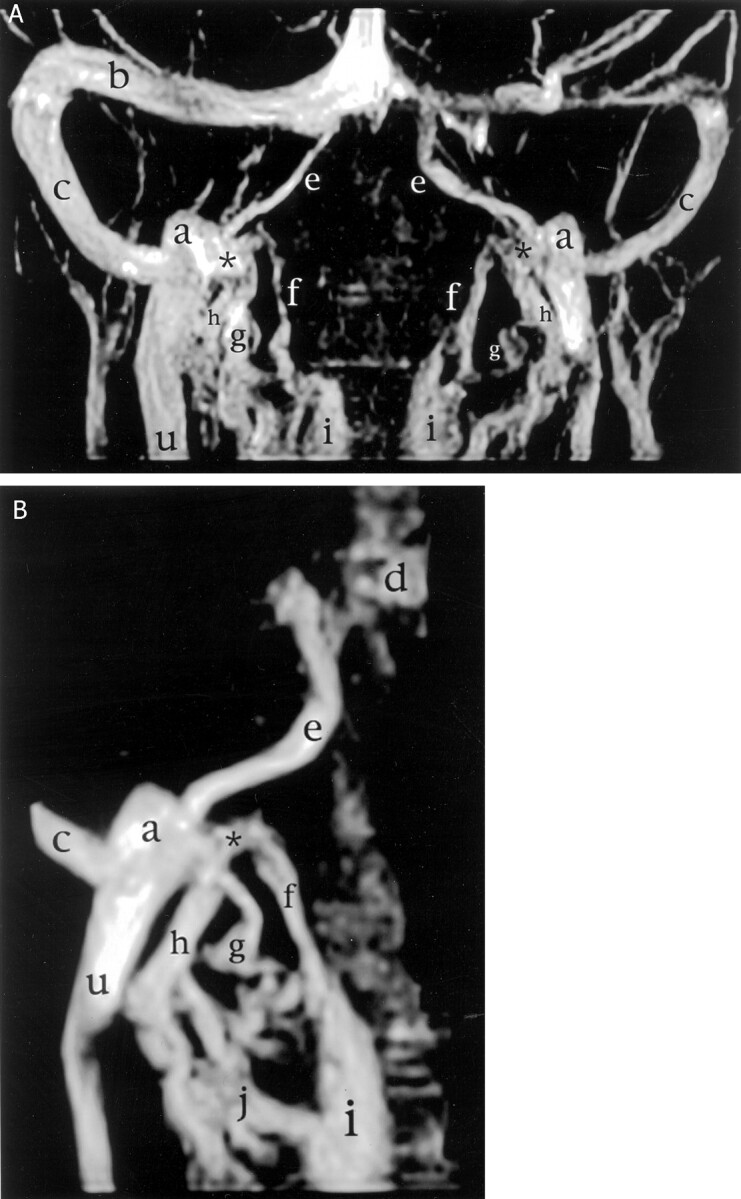
MR venograms of the craniocervical region (2D time-of-flight gradient echo images with magnetization transfer; 40/7; field of view, 15 cm; 18; flip angle, 35 degrees; resolution, 220/256; section thickness, 1.5 mm; section overlap, 0.5 mm; matrix, 256 × 256). The ACC (asterisk) and the anterior (f), posterior (g), and lateral (h) condylar veins are shown. b, transverse sinus; c, sigmoid sinus; e, inferior petrosal sinus; a, superior jugular bulb; u, internal jugular vein; i, anterior internal vertebral venous plexus; d, cavernous sinus; j, vertebral artery venous plexus.
A, Overview.
B, Focused on the right superior jugular bulb.
The posterior internal vertebral venous plexus was observed in only one case, and it extended over the C2–C3 vertebral region. It was less developed than its anterior homolog.
Vertebral Veins
The vertebral veins were present in all cases, and the term used by Arnautovic et al (12), vertebral artery venous plexus, seemed appropriate for this venous plexus surrounding the vertebral artery (Fig 4). The initial horizontal portion of the vertebral artery venous plexus was found in the atlanto-occipital space and constantly connected with the proximal portion of the anterior internal vertebral venous plexus, in the manner of an intervertebral vein (Fig 2A and B). The initial horizontal portion of the vertebral artery venous plexus seemed to correspond to the suboccipital cavernous sinus presented by Arnautovic.
Fig 4.
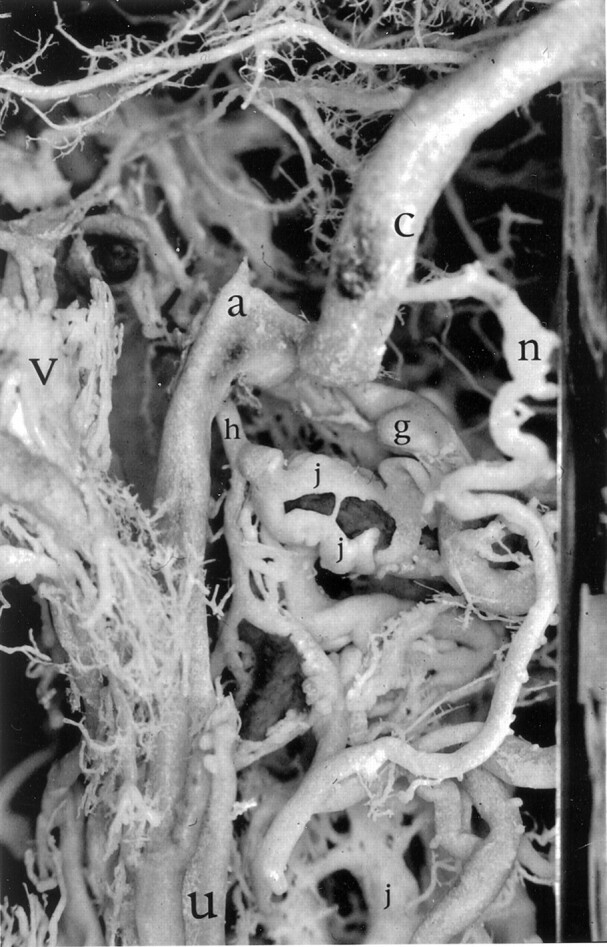
Left lateral view of the sigmoid sinus/jugular bulb junction. The mastoid emissary vein (n) and lateral (h) and posterior (g) condylar veins are shown. The plexiform nature of the vertebral artery venous plexus (j), shown here around the horizontal portion of V3, is well seen. c, sigmoid sinus; a, superior jugular bulb; v, pterygoid plexus; u, internal jugular vein.
The deep cervical veins were completely filled in 22 sides (92% of the sides), and displayed prominent diameters in most cases (Figs 5 and 6). They showed multiple anastomosis with cervical soft tissue veins, such as the suboccipital venous plexus, and with the horizontal portion of the vertebral artery venous plexus.
Fig 5.
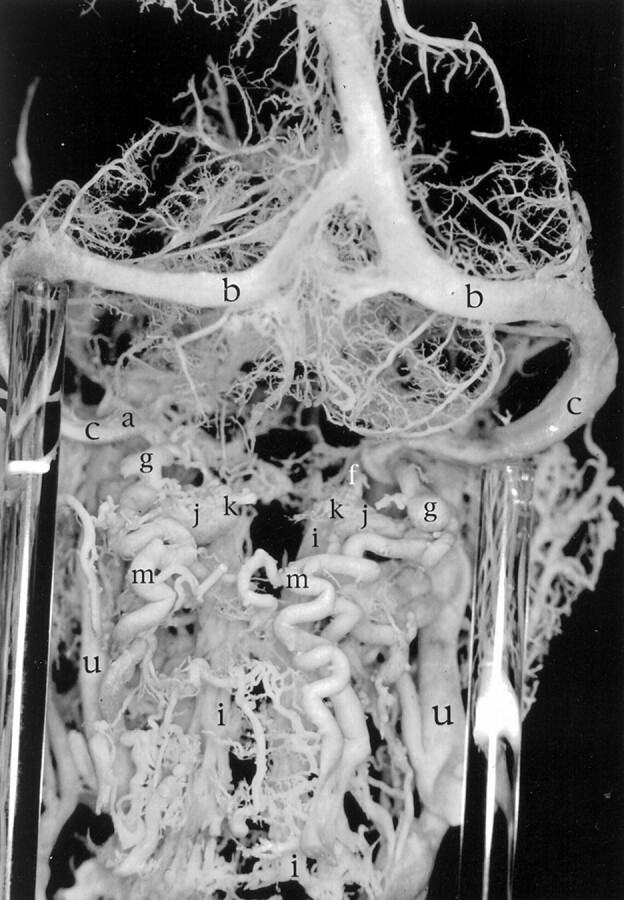
Posterior overview of the craniocervical junction in a venous corrosion cast. Note prominent deep cervical veins bilaterally (m). The left posterior condylar vein (g) is clearly seen to drain into both the horizontal portion of the left vertebral artery venous plexus at the C1 level (j) and the left deep cervical vein (m). b, transverse sinus; c, sigmoid sinus; a, superior jugular bulb; f, anterior condylar vein; k, anastomosis between anterior internal vertebral venous plexus and vertebral artery venous plexus; i, anterior internal vertebral venous plexus; u, internal jugular vein.
Fig 6.

Right lateral view of the craniocervical junction in a venous corrosion cast. Note the presence of a prominent mastoid emissary vein (n) connecting to a deep cervical vein (m). The carotid artery venous plexus is clearly visible (l). b, transverse sinus; d, cavernous sinus; c, sigmoid sinus; a, superior jugular bulb; v, pterygoid plexus; g, posterior condylar vein; h, lateral condylar vein; u, internal jugular vein.
Anterior, Posterior, and Lateral Condylar Veins and Other Emissary Veins
The posterior condylar vein (condylar emissary vein in the international anatomic nomenclature [15]) was present in 19 of 24 sides (79% of the sides), and its diameter was usually larger than that of the anterior condylar vein (Figs 2A and B, 3A and B, 4–7). It generally took its origin from the superior bulb of the internal jugular vein, although it was seen to arise from the medial side of the distal portion of the sigmoid sinus in one occasion. It drained into the deep cervical vein and also communicated with the horizontal portion of the vertebral artery venous plexus.
Fig 7.
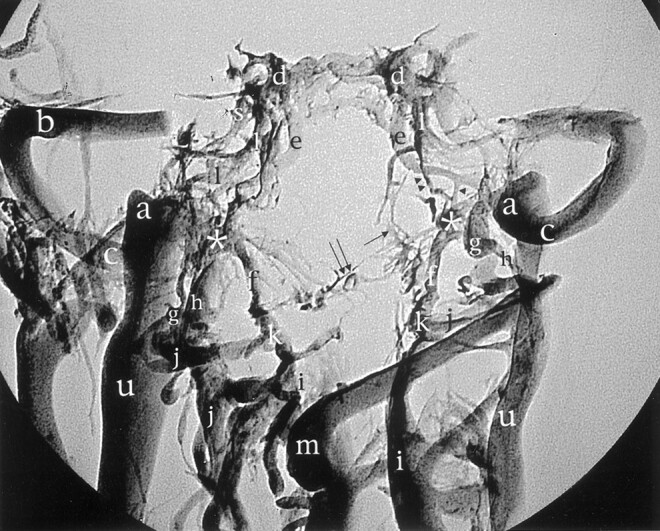
Standard radiographic picture of the corrosion cast from Figure 2 in the anteroposterior projection shows the ACC (asterisk) and its relation with surrounding veins. The proximal portions of the transverse sinus (b), confluens sinuum, and straight and superior longitudinal sinuses have been removed for better visualization. Arrowhead, branch between the inferior petrosal sinus and the ACC; double arrowhead, inferior petrooccipital vein; arrow, basilar plexus; double arrow, branch to prevertebral venous plexus; d, cavernous sinus; e, inferior petrosal sinus; l, internal carotid artery venous plexus of Rektorzik; a, superior jugular bulb; g, posterior condylar vein; c, sigmoid sinus; h, lateral condylar vein; k, anastomosis between anterior internal vertebral venous plexus and vertebral artery venous plexus; j, vertebral artery venous plexus; u, internal jugular vein; i, anterior internal vertebral venous plexus; m, deep cervical vein.
The anterior condylar vein (venous plexus of the hypoglossal nerve in the international anatomic nomenclature [15]) was present in all except one side (96% of the sides) (Figs 2A and B, 3A and B, 4–7). It appeared as a plexiform connection of the anterior internal vertebral venous plexus with the ACC. On occasions, it was traversed longitudinally by a channel for the hypoglossal nerve. In six sides, small plexiform anastomosis was observed with the basilar plexus (25% of the sides) (Fig 2A and B).
The lateral condylar vein (13) connecting with the vertebral artery venous plexus was observed in 19 sides (79% of the sides). Its origin was generally found on an anastomotic branch between the ACC and the internal jugular vein and not directly on the internal jugular vein as in the cases described by Arnautovic et al (12) (Figs 2B, 3A, and 4). According to Trolard (14), the proximal portion of the lateral condylar vein might sometimes be found within an osseous canal in front of the condyle.
An occipital emissary vein was observed on one cast and was seen to join the confluens sinuum region and an occipital vein (Fig 1). A mastoid emissary vein was noted on 15 sides (63% of the sides). It arose from the middle portion of the sigmoid sinus and joined either a posterior auricular vein, an occipital vein, or the deep cervical vein (Figs 4 and 6).
ACC of Trolard
A venous confluent that responded to Trolard’s description of the ACC (14) was found in all cases (Figs 2A and B, 3A and B, 7). The ACC was located extracranially in front of the aperture of the hypoglossal canal. The size of the ACC was between 3 and 5 mm in an anterior view and approximately 2 mm in its ventrodorsal extension. The following veins regularly contributed in forming the ACC: 1) the anterior condylar vein; 2) one or several branches from the internal jugular vein or its bulb; 3) the lateral condylar vein, sometimes arising from one or several branches from the internal jugular vein or its bulb; 4) anastomoses with the inferior petrosal sinus at a variable distance from its termination into the internal jugular vein; 5) branches from the internal carotid artery venous plexus of Rektorzik (Figs 2B and 6), corresponding to Trolard’s inferior petrooccipital vein (14) found coursing extracranially along the petrooccipital suture; and 6) branches from the prevertebral venous plexus found on the anterior atlanto-occipital membrane (Fig 2A and B). A graphic synopsis of these veins is provided in Figure 8.
Fig 8.
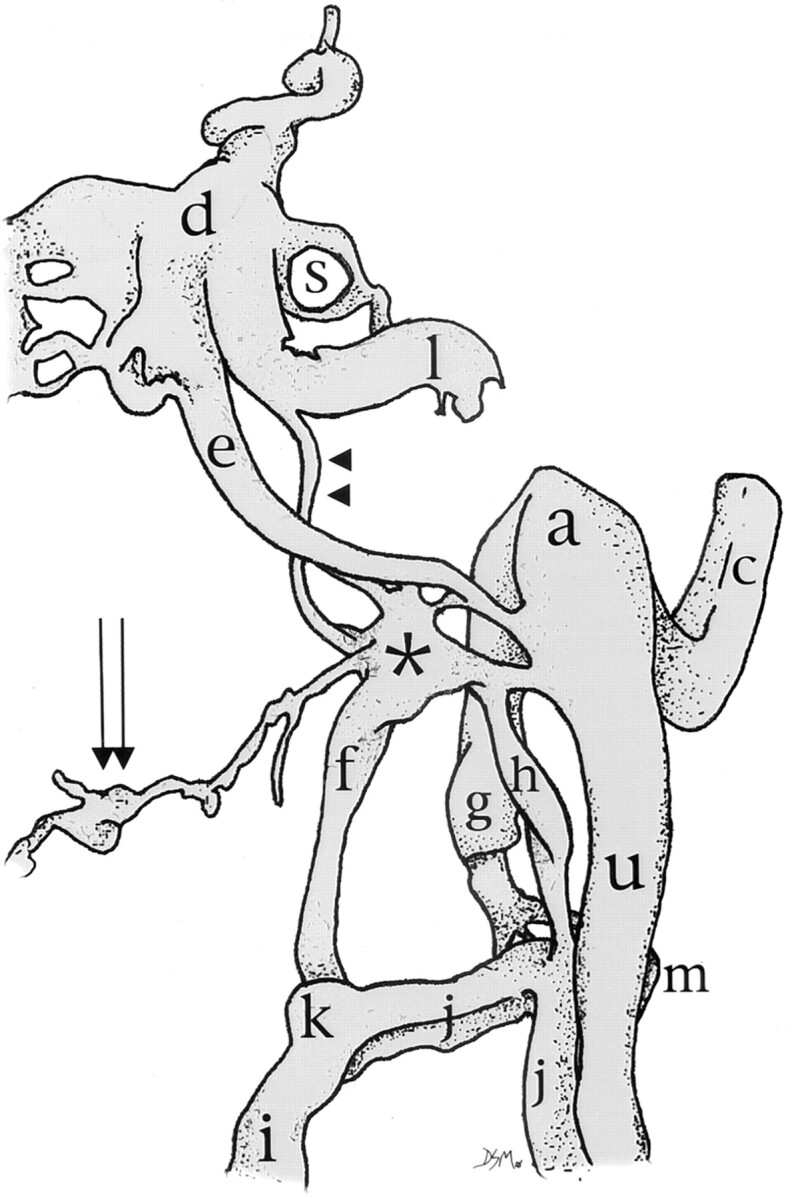
Schematic representation of anterior view of the ACC and its connections. Note the six main contributions, from the anterior condylar vein (f), the lateral condylar vein (h), the internal jugular vein (u), the inferior petrosal sinus (e), the venous plexus of Rektorzik (double arrowhead), and the prevertebral venous plexus (double arrow). d, cavernous sinus; s, emissary vein of the foramen ovale; a, superior jugular bulb; c, sigmoid sinus; g, posterior condylar vein; k, anastomosis between anterior internal vertebral venous plexus and vertebral artery venous plexus; j, vertebral artery venous plexus; m, deep cervical vein; i, anterior internal vertebral venous plexus.
The anatomic dissections of the injected specimens allowed for recognition of all the cervical outflow pathways, particularly the ACC. The anatomic relationship between the ACC, its tributaries, and the surrounding anatomic structures, such as cranial nerves IX through XII, was readily identified.
The optimal angiographic anatomy of the venous elements described above are shown in Figure 7. Figure 3 shows the normal venous anatomy of the craniocervical junction observed in the living by a phlebographic MR imaging study. All the major tributaries of the ACC and outflow pathways of the cerebral venous system were shown on the phlebographic MR images.
Discussion
The venous drainage of the brain follows different outflow tracks, depending on the position of the body (6–9). In the prone position, the outflow through the internal jugular veins is favored, whereas passing to the upright position transfers most of the encephalic drainage to the internal and external vertebral venous systems (6). The purpose of this report was to study the possible connections between the cerebral, neurocranial, and cervical venous systems. We will discuss only the outflow pathways of the bulk of the cerebral venous drainage (ie, through the transverse-sigmoid sinus) without taking into consideration other outflow pathways, such as the superficial and deep middle cerebral vein, which ultimately drain through emissary veins of the middle cranial fossa (16, 17).
The corrosion cast findings in the present study confirm the complexity of the venous network in the craniocervical junction. Schematically, two descending cerebral venous outflow tracks can be distinguished: the internal jugular veins anteriorly and the vertebral venous system posteriorly. The latter is composed of the external and internal vertebral venous plexuses, which are anastomosed by way of the intervertebral and basivertebral veins. In the cervical region, the vertebral venous system is mainly represented by the anterior internal vertebral venous plexus, the vertebral artery venous plexus, and the deep cervical veins.
As far as this posterior outflow track is concerned, our findings suggest that the anterior, posterior, and lateral condylar veins and the ACC represent the most important connections between the intracranial cerebral venous circulation and the vertebral venous systems, in terms of diameters (size) and frequency of occurrence. All the venous elements were readily shown by using 2D MR venography. Standard radiographic analysis of the corrosion casts provided correlation to the angiographic anatomy of the craniocervical junction venous system. Although not all the vessels are shown simultaneously in the venous phase during routine cerebral digital subtraction angiography studies, isolated emissary veins do appear and need to be identified.
The posterior and lateral condylar veins allow for connections with the external vertebral venous system, whereas the anterior condylar veins are predominantly related to the internal vertebral venous plexus. It is noteworthy that even though the diameters of the anterior and lateral condylar veins were important, they were connected to the internal jugular vein by only a small anastomosis between the jugular bulb or internal jugular vein and the ACC. However, phlebography studies of live monkeys and humans clearly illustrate that not only the vertebral artery venous plexuses but also the anterior internal vertebral venous plexus are shown in the upright position and during compression maneuvers of the internal jugular veins (7, 8). This observation suggests that venous flow from the jugular bulb through the anterior condylar vein and into the anterior internal vertebral venous plexus occurs efficaciously by way of the ACC regardless of how indirect this pathway might seem. It is, therefore, difficult to predict the functional importance of a connecting vein involved in the outflow of cerebral blood flow based uniquely on size and on directness of the route.
The ACC appeared as an anatomic constant whose major tributaries, size-wise, were the anterior and lateral condylar veins, inferior petrosal sinus, and internal jugular vein. The ACC was also connected to the carotid artery venous plexus by the inferior petrooccipital vein (14) and to the prevertebral venous plexus. The numerous anastomoses of the ACC make it a crossroad between the cavernous sinus, dural venous sinuses of the posterior fossa, and posterior cervical outflow tracks.
Much literature has been devoted to the anatomy of the outflow pathways of the cavernous sinus and the region around the jugular foramen in relation to skull base surgery and endovascular inferior petrosal sinus sampling (18–25). The ACC has not been specifically mentioned, although it has been shown by several reports. Saleh et al (18), in a microsurgical anatomic study of the skull base, noted the presence of a venous confluence receiving the anterior condylar vein (plexus) and connecting with the jugular bulb and inferior petrosal sinus in one of 45 specimens. Miller et al (23) studied the phlebographic anatomy of the junction of the inferior petrosal sinus and internal jugular vein and refined the classification presented by Shiu et al (22) of the termination of the inferior petrosal sinus. Miller et al’s illustrations of retrograde inferior petrosal sinus phlebograms show the ACC but not all its tributaries. Aubin et al (25) clearly showed the ACC on several retrograde inferior petrosal sinus phlebograms and described it as a “common canal” of the inferior petrosal sinus and the anterior condylar vein.
Anatomic knowledge of the ACC allows for a good understanding of the various types of inferior petrosal sinus termination described by Miller et al (23), which is essential when performing retrograde inferior petrosal phlebography or when accessing the cavernous sinus posteriorly. Although the condylar emissary veins are variably present, we have always encountered connections both between the inferior petrosal sinus and the internal jugular vein and between the inferior petrosal sinus and the internal and external vertebral venous plexus (anterior or lateral condylar vein).The failure by Miller et al to show these connections could be explained by the phlebograms having been obtained in the supine position only, whereas both the supine and upright positions are probably necessary to show all the major connections of the ACC.
From a physiological point of view, one should also consider that the same postural influences affecting cerebral venous drainage might redirect the circulation of the internal and external vertebral venous systems. For instance, the cranial (as opposed to caudal) connections of the anterior internal vertebral venous plexus with the anterior condylar vein could offer a cranial escape route for thoracic and abdominal venous return when thoracic pressure and abdominal pressure are increased concomitantly. One could even consider venous blood from the anterior internal vertebral venous plexus draining into the superior ophthalmic vein and cavernous sinus through the basilar plexus and inferior petrosal sinuses and thus terminally into the pterygoid plexus and facial veins. Parkinson (26) recently described the extradural neural axis compartment. The extradural neural axis compartment contains a continuum of veins that extends from the ophthalmic to the coccygeal veins and offers numerous longitudinal and transverse venous anastomoses. In the craniocervical region, the basilar plexus, inferior petrosal sinuses, and anterior condylar veins represent the venous elements of this extradural neural axis compartment. This venous continuum finds its clinical significance in pathologic situations such as dural AVFs of the anterior condylar vein, which retrogradely fill the inferior petrosal and cavernous sinuses and clinically manifest with chemosis and proptosis (27).
A very complex drainage system, therefore, appears in which cerebral, neurocranial, and cervical venous blood might take different common, but variable, outflow tracks depending on posture, pressure, and anatomic variations. It remains to be determined which physiological mechanisms (eg, Starling valve phenomena) favor one outflow track over another. Noninvasive radiologic techniques, such as sonography and Doppler ultrasonography, might be a valuable tool aiding in understanding this complex physiology. Valdueza et al (6) used sonography and Doppler ultrasonography studies to observe variations of craniocervical venous drainage with postural changes. Other factors affecting craniocervical venous drainage, such as Valsalva maneuvers or increases in abdominal pressure, could very well be investigated by sonography and Doppler ultrasonography.
Conclusion
Anterior, lateral, and posterior condylar veins and occipital and mastoid emissary veins provide connections between the posterior fossa dural sinuses and internal jugular vein system with the cervical vertebral venous system. These emissary veins allow for encephalic blood to drain into the cervical internal and external vertebral venous plexuses, which represent the major outflow tract for encephalic drainage in the upright position. The ACC, a venous entity ignored since Trolard described it in 1868, represents a major venous crossroad of the base of the skull. Thorough anatomic knowledge of the venous system of the craniocervical region is necessary not only to understand the physiology of craniocervical venous drainage but also when attempting selective retrograde venous catheterization or when interpreting venous imaging studies, such as MR venography studies, that readily show the major emissary veins. Emissary veins must no longer be considered to be of secondary physiological importance, mainly acting as safety venous outlet routes, but as obligatory outflow pathways for encephalic drainage in the upright position. The constant presence of emissary veins and the size proportionality relation they exhibit strongly support their major functional importance.
Footnotes
Presented at the 39th Annual Meeting of the American Society of Neuroradiology, Boston, April 2001.
References
- 1.Hacker H. Superficial supratentorial veins and dural sinuses. In: Potts DG, Newton TH, eds. Radiology of the Skull and Brain. vol 2, book 3. St Louis: The CV Mosby Company;1974. :1851–1877
- 2.Breschet G. Recherches Anatomiques, Physiologiques et Pathologiques sur le Système Veineux et Spécialement sur les Canaux Veineux des Os [in French]. Paris: Villeret et Rouen;1829:1–42 [Google Scholar]
- 3.Clemens H. 1. Beitrag zur Histologie des Plexus venosi vertebrales interni. Zeitschrift für mikr.-anat Forshung 1961;67:183–189 [Google Scholar]
- 4.Batson O. The vertebral vein system. AJR Am J Roentgenol 1957;78:195–212 [PubMed] [Google Scholar]
- 5.Groen RJ, Groenewegen HJ, van Alphen HA, Hoogland PV. Morphology of the human internal vertebral venous plexus: a cadaver study after intravenous Araldite CY 221 injection. Anat Rec 1997;249:285–294 [DOI] [PubMed] [Google Scholar]
- 6.Valdueza JM, von Munster T, Hoffman O, et al. Postural dependency of the cerebral venous outflow. Lancet 2000;355:200–201 [DOI] [PubMed] [Google Scholar]
- 7.Théron J, Moret J. Spinal Phlebography: Lumbar and Cervical Techniques. 1st ed. Berlin: Springer-Verlag;1978. :3–7
- 8.Epstein HM, Linde HW, Crampton AR, Ciric IS, Eckenhoff JE. The vertebral venous plexus as a major cerebral venous outflow tract. Anesthesiology 1970;32:332–337 [DOI] [PubMed] [Google Scholar]
- 9.Eckenhoff J. The physiologic significance of the vertebral venous plexus. Surg Gynecol Obstet 1970;131:72–78 [PubMed] [Google Scholar]
- 10.Zouaoui A, Hidden G. The cervical vertebral venous plexus and anastomoses with the cranial venous sinuses [in French]. Bull Assoc Anat (Nancy) 1987;71:7–13 [PubMed] [Google Scholar]
- 11.Braun JP, Tournaire A. Venous drainage in the craniocervical region. Neuroradiology 1977;13:155–158 [DOI] [PubMed] [Google Scholar]
- 12.Arnautovic KI, al-Mefty O, Pait TG, Krisht AF, Husain MM. The suboccipital cavernous sinus. J Neurosurg 1997;86:252–262 [DOI] [PubMed] [Google Scholar]
- 13.Theron J. Cavernous plexus affluents. Neurochirurgie 1972;18:623–638 [PubMed] [Google Scholar]
- 14.Trolard P. Anatomie du système veineux de l’encéphale et du crane [in French]. Paris: Thèse de la Faculté de Médecine de Paris 1868. :1–32
- 15.Federative Committee on Anatomical Terminology (FCAT). Terminologia Anatomica. Stuttgart: Thieme;1998
- 16.San Millán Ruíz D, Gailloud P, de Miquel Miquel MA, et al. Laterocavernous sinus. Anat Rec 1999;254:7–12 [DOI] [PubMed] [Google Scholar]
- 17.Gailloud P, San Millán Ruíz D, Muster M, et al. Angiographic anatomy of the laterocavernous sinus. AJNR Am J Neuroradiol 2000;21:1923–1929 [PMC free article] [PubMed] [Google Scholar]
- 18.Saleh E, Naguib M, Aristegui M, Cokkeser Y, Sanna M. Lower skull base: anatomic study with surgical implications. Ann Otol Rhinol Laryngol 1995;104:57–61 [DOI] [PubMed] [Google Scholar]
- 19.Rhoton AL Jr, Buza R. Microsurgical anatomy of the jugular foramen. J Neurosurg 1975;42:541–550 [DOI] [PubMed] [Google Scholar]
- 20.Doppman JL, Krudy AG, Girton ME, Oldfield EH. Basilar venous plexus of the posterior fossa: a potential source of error in petrosal sinus sampling. Radiology 1985;155:375–378 [DOI] [PubMed] [Google Scholar]
- 21.Kveton JF, Cooper M. Microsurgical anatomy of the jugular foramen region. Am J Otol 1988;9:109–112 [PubMed] [Google Scholar]
- 22.Shiu PC, Hanafee W, Wilson GH, Rand RW. Cavernous sinus venography. Am J Roentgenol Radium Ther Nucl Med 1968;104:57–62 [DOI] [PubMed] [Google Scholar]
- 23.Miller DL, Doppman JL, Chang R. Anatomy of the junction of the inferior petrosal sinus and the internal jugular vein. AJNR Am J Neuroradiol 1993;14:1075–1083 [PMC free article] [PubMed] [Google Scholar]
- 24.Gailloud P, Fasel JH, Muster M, et al. Termination of the inferior petrosal sinus: An anatomical variant. Clin Anat 1997;10:92–96 [DOI] [PubMed] [Google Scholar]
- 25.Aubin ML, Paleirac R, Traserra J. Radioanatomy of the jugular sinus and its anterior collaterals [in French]. Ann Radiol (Paris) 1974;17:247–252 [PubMed] [Google Scholar]
- 26.Parkinson D. Extradural neural axis compartment. J Neurosurg 2000;92:585–588 [DOI] [PubMed] [Google Scholar]
- 27.Ernst R, Bulas R, Tomsick T, van Loveren H, Aziz KA. Three cases of dural arteriovenous fistula of the anterior condylar vein within the hypoglossal canal. AJNR Am J Neuroradiol 1999;20:2016–2020 [PMC free article] [PubMed] [Google Scholar]


