Abstract
Summary: A case of recurrent glomus tympanicum presenting with epistaxis is described. CT and MR imaging revealed a homogeneously enhancing mass extending along the entire course of the eustachian tube, with a portion protruding into the nasopharynx. Glomus tumors tend to spread along the path of least resistance and may extend into the eustachian tube. The unique imaging appearance should place a glomus tumor high on the list of differential diagnoses.
Glomus tumors of the head and neck have been well described in the radiology and surgical literature. They arise from glomus bodies, which are chemoreceptors in the temporal bone derived from primitive neural crest cells. The most common, glomus jugulare, often presents as an enhancing vascular mass with local destruction in the jugular foramen. Within the head and neck, glomus tumors can also occur within the middle ear (glomus tympanicum), along the vagus nerve (glomus vagale), and at the common carotid artery bifurcation (carotid body tumor). Glomus tympanicum tumors are identified by their characteristic location within the tympanic cavity, lateral to the cochlear promontory, and by the absence of jugular bulb involvement. These tumors tend to spread along the path of least resistance and dissect along fascial planes. We present a case of glomus tympanicum extending along the entire course of the eustachian tube. This has been described in older literature (1–3), but the imaging correlate in this particular location, to our knowledge, has not been described. The characteristic appearance on contrast-enhanced CT scans and MR images is presented in this report.
Case Report
A 65-year-old woman presented with a history of intermittent epistaxis of several months' duration. These episodes prompted recurrent visits to the emergency department and required nasopharyngeal packing. The patient was seen by her otorhinolaryngologic surgeon during follow-up. A fiberoptic endoscopic examination revealed a reddish mass bulging into the nasopharynx from the eustachian tube. A contrast-enhanced CT scan showed a 3.2 × 1.0 × 1.0-cm enhancing mass along the course of the eustachian tube (Fig 1). The mass extended superolaterally to the tegmen, which was dehiscent. Enhancing dura at the skull base was also noted. The jugular bulb was normal.
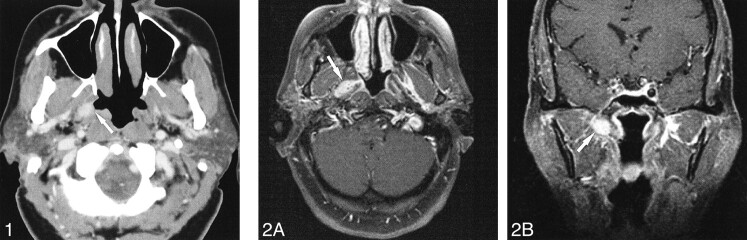
fig 1.
CT shows enhancing mass in the eustachian tube (arrow).fig 2.
A, T1-weighted contrast-enhanced spin-echo image (500/8 [TR/TE]) shows that the mass extends into the eustachian tube (arrow).
B, Coronal T1-weighted contrast-enhanced (arrow) spin-echo image (400/8) shows the mass extending superiorly up the eustachian tube.
The patient's medical history was significant for a right-sided glomus tumor in 1993. At that time, she presented with pulsatile tinnitus and hearing loss. CT revealed opacification of the middle ear and a normal eustachian tube (not shown). Surgical resection was attempted, but the procedure was terminated because of severe bleeding. The case was thereafter managed conservatively for several years. In 1996, the patient was diagnosed with recurrent tumor. At surgery, tumor was found in the epitympanum and mesotympanum and appeared to track down the eustachian tube. It was thought that complete surgical removal of the tumor and the portion extending down the eustachian tube had been achieved; however, no postoperative imaging had been performed to confirm this. The patient had remained well until her present symptoms.
A presumptive diagnosis of recurrent glomus tumor extending down the eustachian tube was made. MR imaging was performed and confirmed extension of the tumor superiorly to the dura and the enhancing eustachian tube mass (Fig 2A and B). The patient was subsequently referred for radiotherapy. At her most recent follow-up examination, 2 months after completing radiotherapy, she was well and reported no recurrence of her epistaxis.
Discussion
Glomus tympanicum tumors are the most common primary neoplasms of the middle ear (4). They arise from glomus bodies, which are nonfunctioning chemoreceptors in the temporal bone derived from primitive neural crest cells. The origin is typically along the tympanic branch of the glossopharyngeal nerve (Jacobson's nerve). They are vascular tumors composed of capillary and precapillary blood vessels interspersed with epithelioid cells (5). The blood supply is from the inferior tympanic branch of the ascending pharyngeal artery. Other words used to describe these masses include paraganglioma and chemodectoma.
Clinically, glomus tympanicum tumors most often present with pulsatile tinnitus. This is followed by hearing loss, otalgia, and aural fullness (4). In our case, the patient's recurrent tumor presented with epistaxis secondary to its extension to the nasopharynx through the eustachian tube.
The most characteristic location of glomus tympanicum tumors is lateral to the cochlear promontory. An intact jugular bulb is an important feature in distinguishing a glomus tympanicum from the more common glomus jugulare. CT with bone windows is best to show an intact jugular fossa and caroticotympanic spine. However, if the tumor is large and involves the jugular bulb, it cannot be distinguished from a glomus jugulare tumor. In our case, the tumor grew inferiorly through the eustachian tube, following the path of least resistance (6).
In considering the differential diagnoses of lesions along the eustachian tube, one needs to include diseases extending from both the middle ear cavity and nasopharynx. Squamous cell carcinoma is a common tumor found in the nasopharynx and can uncommonly extend superiorly into the mastoid air cells. It appears that spread into the eustachian tube is limited by its cartilaginous portion and the pharyngobasilar fascia (7). The enhancement of nasopharyngeal carcinoma is also less intense than glomus tumors and should therefore be easily distinguishable. Theoretically, vascular lesions such as Kaposi's sarcoma or hemangioma may involve the eustachian tube and could appear similar to the lesion in our case. Lymphoma may involve the nasopharynx; however, bulky disease and other areas of adenopathy are usually seen.
A number of treatment options are available for patients presenting with glomus tumors of the head and neck. Because of the benign nature of these tumors, some authors recommend follow-up only for small asymptomatic lesions (8). Cases with larger, symptomatic lesions can be effectively managed with surgical resection (9–11) with preoperative embolization or primary radiation therapy (12, 13).
This case illustrates an unusual manifestation of a glomus tympanicum presenting as recurrent epistaxis. The cause was evident on the CT scan, which showed tumor extending down the eustachian tube bulging into the nasopharynx. If a vascular mass is seen along the eustachian tube, a glomus tumor should be high on the list of differential diagnoses.
Footnotes
Presented as an excerpta extraordinaire, at the 38th Annual Meeting of the American Society of Neuroradiology, Atlanta, April 2000.
Address reprints requests to Dr. M.A. Keller, Department of Medical Imaging (3–920), Princess Margaret Hospital, 610 University Avenue, Toronto, Ontario, M5G 2M9 Canada.
References
- 1.Dickens WJ, Million RR, Cassisi NJ, et al. Chemodectomas arising in temporal bone structures. Laryngoscope 1982;92:188-191 [DOI] [PubMed] [Google Scholar]
- 2.Brown JS. Glomus jugulare tumors: methods and difficulties of diagnosis and surgical treatment. Laryngoscope 1967;77:26-67 [DOI] [PubMed] [Google Scholar]
- 3.Chakeres DW, LaMasters DL. Paragangliomas of the temporal bone: high-resolution CT studies. Radiology 1984;150:749-753 [DOI] [PubMed] [Google Scholar]
- 4.O'Leary MJ, Shelton C, Giddings NA, Kwartler J, Brackmann DE. Glomus tympanicum tumors: a clinical perspective. Laryngoscope 1991;101:1038-1043 [DOI] [PubMed] [Google Scholar]
- 5.Guild SR. The glomus jugular: a non-chromaffin paraganglioma in man. Ann Otol Rhinol Laryngol 1953;62:1043-1071 [DOI] [PubMed] [Google Scholar]
- 6.Donald PJ. Surgery of the Skull Base.. Philadelphia: Lippincott-Raven 1998;475
- 7.Som PM, Curtin HD, eds. Head and Neck Imaging.. 3rd ed. St. Louis: Mosby 1996;446
- 8.van der Mey AG, Frijns JH, Cornelisse CJ, et al. Does intervention improve the natural course of glomus tumors? A series of 108 patients seen in a 32-year period. Ann Otol Rhinol Laryngol 1992;101:635-642 [DOI] [PubMed] [Google Scholar]
- 9.Brammer RE, Graham MD, Kemink JL. Glomus tumors of the temporal bone: contemporary evaluation and therapy. Otolaryngol Clin North Am 1984;17:499-512 [PubMed] [Google Scholar]
- 10.Manolidis S, Shohet JA, Jackson CG, Glasscock ME III. Malignant glomus tumors. Laryngoscope 1999;109:30-34 [DOI] [PubMed] [Google Scholar]
- 11.Briner HR, Linder TE, Pauw B, Fisch U. Long-term results of surgery for temporal bone paragangliomas. Laryngoscope 1999;109:577-583 [published erratum appears in Laryngoscope 1999;109:1355] [DOI] [PubMed] [Google Scholar]
- 12.Cummings BJ, Beale FA, Garrett PG, et al. The treatment of glomus tumors in the temporal bone in megavoltage radiation. Cancer 1984;53:2635-2640 [DOI] [PubMed] [Google Scholar]
- 13.Springate SC, Weichselbaum RR. Radiation or surgery for chemodectoma of the temporal bone: a review of local control and complications. Head Neck 1990;12:303-307 [DOI] [PubMed] [Google Scholar]