Abstract
Summary: Inflammatory myofibroblastic tumors (IMT) comprise a rare group of lesions characterized histologically by acute and chronic inflammatory cells with a variable degree of fibrous stroma. Occurrence in the extracranial head and neck in children is unusual, and involvement in the pterygopalatine fossa has not, to our knowledge, been reported as occurring in this age group. We present the CT findings of an IMT of the pterygopalatine fossa in a 6-year-old female patient with a 2-week history of fever and a painless swelling of the left cheek. The diagnosis of IMT should be included in the differential diagnosis of a child presenting with an aggressive mass associated with systemic features such as fever, elevated sedimentation rate, and leukocytosis.
Inflammatory myofibroblastic tumors (IMT) comprise a rare group of lesions characterized histologically by acute and chronic inflammatory cells with a variable degree of fibrous stroma. IMT of the head and neck are most commonly seen in the orbits and the upper aerodigestive tract. The presenting symptoms are nonspecific and depend on location. As a result, differentiation from a neoplasm cannot be based on clinical findings alone. We present an unusual case of an IMT arising in the pterygopalatine fossa in a 6-year-old child.
Case Report
A 6-year-old African-American female patient presented with a 2-week history of progressive painless swelling of the left cheek. There were no associated orbital symptoms. There was no history of any trauma or previous dental procedures. The swelling was accompanied by a daily fever of 103°F. The patient's medical history was otherwise unremarkable. A physical examination revealed a fleshy lesion that measured approximately 5 cm, extending into the oral cavity behind the molars. There was no tenderness, discharge, or facial numbness. Laboratory studies revealed an elevated erythrocyte sedimentation rate of 80 mm. It was initially thought that the patient had an odontogenic infection, and antibiotics were administered for 10 days. After treatment, there was no change in the swelling or in the patient's recurrent fever.
Imaging studies were performed (Fig 1). Plain film radiography of the sinuses revealed destruction of the left maxilla. Contrast-enhanced CT of the face (contiguous 3-mm axial and coronal scans) showed a moderately enhancing mass centered in the left pterygopalatine fossa. The mass eroded the posterior wall of the maxillary sinus and extended into the posterior portion of the maxillary sinus. Laterally, the mass extended through the pterygomaxillary fissure and appeared to invade the buccinator muscle. There was reticulation of the adjacent fat in the buccal space. The mass extended posteriorly and displaced but did not appear to invade the lateral pterygoid muscle. There was no evidence of any calcification within this mass. There were no enlarged lymph nodes. The differential diagnosis based on the imaging findings included lymphoma and low-grade rhabdomyosarcoma. A contrast-enhanced MR imaging examination of the brain and CT examinations of the chest and abdomen showed no evidence of metastases.
fig 1.
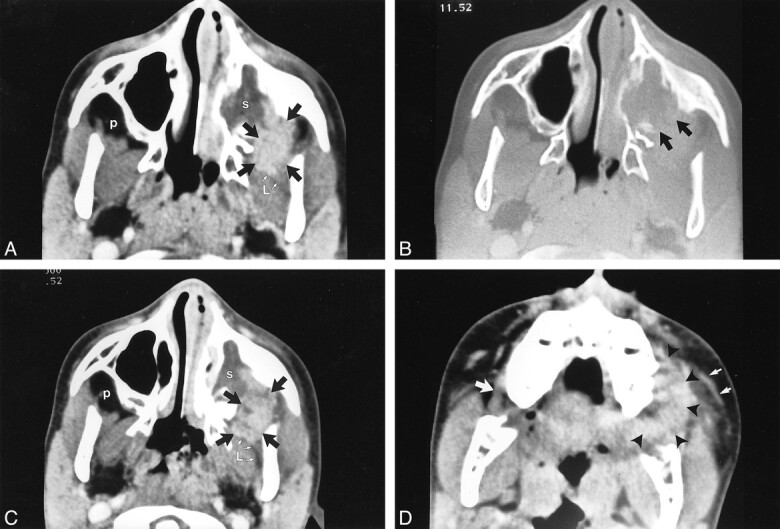
Images from the case of a 6-year-old African-American female patient who presented with a 2-week history of progressive painless swelling of the left cheek.
A, Axial contrast-enhanced CT scan shows a moderately enhancing mass centered in the left pterygopalatine fossa (black arrows). Note the appearance of the normal pterygopalatine fossa on the right (p). The mass extends into the posterior portion of the left maxillary sinus. Hypodense contents within the sinus likely indicate obstructed secretions (s). The fat plane (white arrows) between the lateral pterygoid muscle (L) and the mass is preserved.
B, Bone algorithm scan obtained at the same level as the scan shown in A shows erosion of the posterior wall of the left maxillary sinus (black arrows).
C, Axial contrast-enhanced CT scan obtained at a lower level again shows the enhancing mass centered in the left pterygopalatine fossa (black arrows), extending into the left deep buccal space. Note the preservation of the fat (white arrows) between the mass and lateral pterygoid muscle (L), indicating that the mass is arising anterior to the masticator space in the pterygopalatine fossa. p = normal appearance of the pterygopalatine fossa on the contralateral side.
D, Axial contrast-enhanced CT scan obtained through the maxillary alveolar ridge shows the enlarged buccinator muscle on the left (arrowheads), with reticulation of the adjacent fat (small white arrows). Note the normal appearance of the buccinator muscle on the contralateral side.
Biopsy of the mass revealed spindle cells with architectural fascicle formation that were storiform. Individual cells showed cigar-shaped nuclei with significant pleomorphism and rare mitotic figures. A prominent lymphoid infiltrate was evident. Special stains were negative for fungi, acid-fast bacillus, and nocardia. The morphologic and immunophenotypic features were diagnostic of inflammatory myofibroblastic tumor. Treatment with corticosteroids was administered, and marked clinical improvement was achieved. Follow-up contrast-enhanced CT showed regression in the size of the mass.
Discussion
IMT is a chronic inflammatory mass that follows a benign clinical course. Most of the lesions occur in adults, although a few cases have been reported as occurring in children. The incidence in male patients is equal to the incidence in female patients. The majority of IMT lesions present in the lungs (1, 2). Extrapulmonary sites include the abdomen, head, neck, and CNS. The most common sub-sites in the head and neck include the orbit, larynx, mouth, tonsils, parapharyngeal space, thyroid, and parotid and lacrimal glands (3). Primary involvement of the pterygopalatine fossa has not, to our knowledge, been reported.
Histologically, IMT is composed of inflammatory cells, histiocytes, and fibroblasts. The specific components of IMT can vary and range from those that are dominated by plasma cells to those primarily comprised of myofibroblasts and fibroblasts (1, 4). In the past, this entity has been variably referred to as plasma cell granuloma, inflammatory pseudotumor, xanthogranuloma, histiocytoma, and myofibrohistiocytic proliferation. The diverse nomenclature is probably due to the differing histopathologic subtypes.
The cause of IMT is not known. It has been suggested that IMT may occur as an immune response to an inflammatory stimulus and could represent a reaction to previous trauma or irritation (2).
IMT usually has a benign clinical course. These lesions usually respond to systemic corticosteroids. Characteristics of IMT that are associated with a more aggressive course include an extrapulmonary location and predominance of myofibroblastic or fibroblastic components (5). In children, IMT may be associated with microcytic hypochromic anemia, hypergammaglobulinemia, and a high erythrocyte sedimentation rate (6). Associated clinical findings include fever and tenderness and erythema over the affected region. The exact percentage of the occurrence of these symptoms is not known.
The imaging findings of IMT are a mildly enhancing soft-tissue mass without any internal calcification or bone destruction revealed by contrast-enhanced CT. There is usually no evidence of central necrosis. The reticulation of the adjacent fat suggests an inflammatory component. These lesions tend to be localized without evidence of spread to the cervical lymph nodes. Bone destruction has been described but is unusual.
We thought that the diagnosis, based on the imaging findings, was suggestive of a low-grade neoplasm. Although there was erosion of the posterior wall of the maxillary sinus, the margins of the mass were well defined and the transition between the mass and the adjacent intact bone was sharp. On the basis of these findings, our differential diagnosis included rhabdomyosarcoma, lymphoma, Ewing's sarcoma, and metastases. The lack of a periosteal reaction and absence of a known primary tumor made Ewing sarcoma and metastases less likely. Squamous cell carcinomas may involve this area; however, they usually occur in adults.
In summary, IMT is an unusual lesion that should be considered in children with masses in the extracranial head and neck. The diagnosis should be considered in a febrile child with a solid homogeneous mass that lacks the highly aggressive characteristics usually observed in the malignant tumors that more commonly occur in this area.
Footnotes
Address reprint requests to Suresh K Mukherji, MD, Department of Radiology, University of Michigan Health System, 1500 East Medical Center Drive, B2-B311, Ann Arbor, MI 48109.
References
- 1.Som PM, Brandwein MS, Maldjian C, Reino AJ, Lawson W. Inflammatory pseudotumor of the maxillary sinus: CT and MR findings in six cases. AJR Am J Roentgenol 1994;163:689-692 [DOI] [PubMed] [Google Scholar]
- 2.Hytiroglou P, Brandwein MS, Strauchen JA, Mirante JP, Urken ML, Biller HF. Inflammatory pseudotumor of the parapharyngeal space: case report and review of the literature. Head Neck 1992;14:230-234 [DOI] [PubMed] [Google Scholar]
- 3.Ide F, Shimoyama T, Horie N. Inflammatory pseudotumor in the mandibular retromolar region. J Oral Pathol Med 1998;27:508-510 [DOI] [PubMed] [Google Scholar]
- 4.Van Dorpe J, Ectors N, Geboes K, D'Hoore A, Sciot R. Is calcifying fibrous pseudotumor a late sclerosing stage of inflammatory myofibroblastic tumor? Am J Surg Pathol 1999;23:329-335 [DOI] [PubMed] [Google Scholar]
- 5.Batsakis JG, Luna MA, El-Naggar AK, Goepfert H. “Inflammatory pseudotumor”: What is it? How does it behave? Ann Otol Rhinol Laryngol 1995;104:329-332 [DOI] [PubMed] [Google Scholar]
- 6.Maldjian JA, Norton KI, Groisman GM, Som PM. Inflammatory pseudotumor of the maxillary sinus in a 15-year-old boy. AJNR Am J Neuroradiol 1994;15:784-786 [PMC free article] [PubMed] [Google Scholar]


