Abstract
SUMMARY: We report a case of a 54-year-old man who presented with a right middle cerebral artery territory infarct and was treated with systemic thrombolytics. He continued to fluctuate neurologically and, with the use of angiography, was found to have an occlusion of the right M2 artery (superior division). This occlusion was successfully revascularized with a coronary stent.
The recanalization rates for M1 and M2 middle cerebral artery (MCA) occlusions after administration of intravenous tissue plasminogen activator (tPA) are approximately 20% and 30%.1 Bridging therapies have thus been advocated with administration of systemic thrombolytics followed by infusion of intra-arterial tPA to help dissolve clots.2 Endovascular approaches via mechanical disruption can lead to faster recanalization and theoretically reduce the risk of intracranial hemorrhage. We present a patient who underwent primary stent placement in a M2 superior division branch in the setting of fluctuations in neurologic symptoms after delivery of intravenous tPA.
Case Report
A 54-year-old man with a history of coronary disease, hypertension, and hyperlipidemia developed a sudden onset of left hemiparesis and right gaze preference at an outside hospital. Laboratory evaluation and an urgent CT scan of his head were unrevealing, and he was treated with 0.9 mg/kg intravenous tPA 2.5 hours after the onset of symptoms. He was urgently transferred to our facility for further management. On arrival, the patient was noted to have fluctuating neurologic deficits with new visual and sensory neglect and left-sided hemiplegia. His National Institutes of Health Stroke Scale (NIHSS) score fluctuated between 10 and 15. Repeat head CT obtained to look for an intraparenchymal hemorrhage after tPA administration was found to be negative except for loss of the insular ribbon in the right hemisphere. The patient was urgently taken for angiography with the intent to mechanically recanalize a right MCA occlusion.
Cerebral arteriography revealed a right M2 superior division MCA occlusion (Fig 1 A, -B) without significant vessel tortuosity of the internal carotid artery (ICA) 5.5 hours after the onset of symptoms and administration of systemic tPA. Intra-arterial pharmacologic thrombolysis was contemplated but ultimately determined to be risky because the patient had some evidence of hypoattenuation in this vascular territory on CT and had already received systemic thrombolytics. We believed that a coronary stent could rapidly be delivered to the site of occlusion. The M2 segment was measured to be 2.2 mm just proximal to the site of occlusion. This measurement was made via an electronic ruler that has been calibrated for measuring cerebral vessels. A 6F guiding catheter was placed in the right ICA. A microcatheter and microwire were gently navigated through the M2 occlusion. Contrast injections through the microcatheter demonstrated no evidence of thrombus distal to the focal segment of occlusion in the superior division. A 0.014-in exchange length floppy wire was introduced through the microcatheter into a distal M3 branch. The microcatheter was removed, and a 2 × 10-mm BiodivYsio (Abbott Laboratories, Abbott Park, Ill) was navigated over the 0.014-in microwire to the site of occlusion under roadmapping guidance. A right ICA injection after stenting demonstrated the patency of the superior division (Fig 1 C,-D). The patient was transferred back to the intensive care unit and had neurologically stabilized with a NIHSS score of 10. CT of the head 24 hours after stent placement revealed no evidence of hemorrhage or hypoattenuation in the right insular region.
Fig 1.
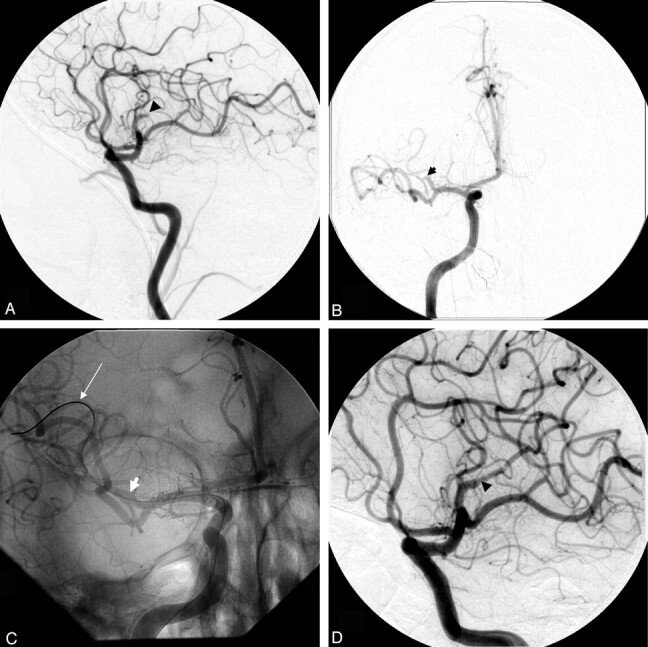
A, Lateral right common carotid artery (CCA) injection reveals a M2 superior division (black arrowhead) occlusion (TIMI 0).
B, AP view of the right CCA injection visualizing the M2 superior division occlusion (black arrowhead).
C, BiodivYsio 2 × 10 mm stent (white arrowhead) deployed over the occlusion by use of a 0.014-in (white arrow) wire.
D, Lateral projection revealing TIMI 3 flow in the M2 division with the stent maintaining patency of the vessel (black arrowhead).
Discussion
Intra-arterial delivery of thrombolytics has been shown to be relatively safe but often requires time, which is of the essence in such patients. Thus, mechanical retrieval devices and angioplasty have been reported as alternative methods of achieving recanalization.3,4 Urgent stent placement has not been used as frequently, because of difficulties of delivery of stents in tortuous cerebral vessels. In theory, this approach would be useful because it would reduce times to recanalization, reduce the possibility of vessel reocclusion that occurs roughly 15% of the time,5 and according to the coronary literature be more beneficial than primary angioplasty after administration of systemic thrombolytics.6
This case report demonstrates that urgent stent placement of a distal intracranial vessel is feasible in certain patients. This particular patient was young and lacked the tortuosity of the intracranial vasculature that is often noted in elderly stroke patients, thus allowing for rapid delivery of a coronary stent. Primary stent placement offers several advantages over chemical and other mechanical methods commonly used to recanalize occluded vessels. First, data from the coronary literature reveal that patients who undergo stent placement in the setting of an acute myocardial infarction have better angiographic results and are less likely to require revascularization of the target vessel in comparison to primary angioplasty.7 Thus, long-term patency of the vessel is more likely with stent placement. Second, intra-arterial infusions of pharmacologic agents take valuable time, with a partial or complete recanalization rate of roughly 66%.8 Time to recanalization, which has been linked to beneficial outcomes, is vital. Third, mechanical methods may have lower rates of intracranial hemorrhage and higher rates of recanalization compared with intra-arterial thrombolytics.4 This may be particularly true in patients who have been treated with systemic thrombolytics. Primary angioplasty has the risk of fragmenting the clot, causing distal embolization of smaller debris.9 In theory, this risk would be lower with primary stent placement. As more navigable stents are introduced, primary stent placement may prove to be a rapid and safe method to recanalize cerebral vessels.
Systemic thrombolysis does not prohibit endovascular treatment in acute stroke. The Interventional Management of Stroke Study was a multicenter trial of 80 patients who underwent combined intravenous and intra-arterial delivery of tPA. Groin hematomas requiring transfusions occurred in 3 patients (3.8%),2 which is within the range of groin complications seen after coronary interventions.10 A second concern is the rate of restenosis after placement of stents in small intracranial vessels. Restenosis rates are reported to range between 10% and 30% with bare metal stents placed in the intracranial circulation.11 These rates may be lower in the future with the advent of drug-eluting stents. We plan to follow this patient with a cerebral angiogram in 6 months, because CT angiography can overestimate in-stent restenosis.12
This report demonstrates that urgent stent placement of the M2 division is technically feasible in select patients and stent placement may be used to recanalize intracranial vessels quickly. Larger series are required to determine the safety and recanalization rates of this therapy as a primary technique of treatment.
References
- 1.Wolpert S, Bruckmann H, Greenlee R, et al. Neuroradiologic evaluation of patients with acute stroke treated with recombinant tissue plasminogen activator. AJNR Am J Neuroradiol 1993;14:3–13 [PMC free article] [PubMed] [Google Scholar]
- 2.IMS Study Investigators. Combined intravenous and intra-arterial recanalization of acute ischemic stroke the Interventional Management of Stroke Study. Stroke 2004;35:904–11 [DOI] [PubMed] [Google Scholar]
- 3.Gobin YP, Starkman S, Duckwiler GR, et al. MERCI 1: a phase 1 study of mechanical embolus removal in cerebral ischemia. Stroke 2004;35:2848–54 [DOI] [PubMed] [Google Scholar]
- 4.Nakano S, Iseda T, Yoneyama T, et al. Direct percutaneous transluminal angioplasty for acute middle cerebral artery trunk occlusion: an alternative option to intra-arterial thrombolysis. Stroke 2002;33:2872–76 [DOI] [PubMed] [Google Scholar]
- 5.Qureshi AI, Siddiqui AM, Kim SH, et al. Reocclusion of recanalized arteries during intra-arterial thrombolysis for acute ischemic stroke. AJNR Am J Neuroradiol 2004;25:322–28 [PMC free article] [PubMed] [Google Scholar]
- 6.Schomig A, Ndrepepa G, Mehilli J, et al. A randomized trial of coronary stenting versus balloon angioplasty as a rescue intervention after failed thrombolysis in patients with acute myocardial infarction. J Am Coll Cardiol 2004;44:2073–79 [DOI] [PubMed] [Google Scholar]
- 7.Stone GW, Grines CL, Cox DA, et al. Comparison of angioplasty with stenting, with or without abciximab, in acute myocardial infarction. N Engl J Med 2002;346:957–66 [DOI] [PubMed] [Google Scholar]
- 8.Furlan A, Higashida R, Wechsler L, et al. Intra-arterial prourokinase for acute ischemic stroke: the PROACT II study: a randomized controlled trial: Prolyse in Acute Cerebral Thromboembolism. JAMA 1999;282:2003–11 [DOI] [PubMed] [Google Scholar]
- 9.Nakano S, Yokogami K, Ohta H, et al. Direct percutaneous transluminal angioplasty for acute middle cerebral artery occlusion. AJNR Am J Neuroradiol 1998;19:767–72 [PMC free article] [PubMed] [Google Scholar]
- 10.Koreny M, Riedmuller E, Nikfardjam M, et al. Arterial puncture closing devices compared with standard manual compression after cardiac catheterization: systematic review and meta-analysis. JAMA 2004;291:350–57 [DOI] [PubMed] [Google Scholar]
- 11.SSYLVIA Study Investigators. Stenting of symptomatic atherosclerotic lesions in the vertebral or intracranial arteries (SSYLVIA): study results. Stroke 2004;35:1388–92 [DOI] [PubMed] [Google Scholar]
- 12.Trossbach M, Hartmann M, Braun C, et al. Small vessel stents for intracranial angioplasty: in vitro evaluation of in-stent stenosis using CT angiography. Neuroradiology 2004;46:459–63 [DOI] [PubMed] [Google Scholar]


