Abstract
Mineralocorticoid receptor antagonists (MRA) improve clinical outcomes in patients with heart failure with reduced ejection fraction (HFrEF) and reduce risk of heart failure (HF) hospitalization in patients with heart failure with preserved ejection fraction (HFpEF). However, the benefit and risks of MRA use are not clear in HF patients and chronic kidney disease (CKD) with estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m2. We conducted a systematic review evaluating the efficacy and safety of MRA in patients with HF and CKD. PubMed, Embase, and Cochrane Central databases were searched for relevant studies on patients with HF and reduced renal function (defined as eGFR <60 mL/min/1.73 m2). Seven studies with 5,522 patients were included. We found 3 studies in patients with HFrEF, 1 study with HFpEF, and 2 in acute HF and 1 with mixed patient population of HF. Post hoc analyses from randomized controlled trials demonstrated reduction of risk in the primary end point (adverse cardiovascular outcomes and/or all-cause mortality and/or HF hospitalization) with MRA use in the CKD subgroup (eGFR 30 to 60 mL/min/1.73 m2) despite a greater risk of hyperkalemia and higher rates of drug discontinuation. In 3 observational studies, propensity score matching was performed to compare patients treated with and without MRA and did not identify benefits, but conclusions from these studies were limited due to residual confounding and concern for bias. In conclusion, benefits of MRA use in HF appear to be consistent in patients with reduced renal function (eGFR 30 to 60 mL/min/1.73 m).
Mineralocorticoid receptor antagonists (MRA) improve clinical outcomes in patients with heart failure with reduced ejection fraction (HFrEF).1 The American College of Cardiology (ACC)/American Heart Association (AHA)/Heart Failure Society of America (HFSA) and European Society of Cardiology (ESC) guidelines recommend MRA use to reduce morbidity and mortality in HFrEF patients (class of recommendation [COR] I, level of evidence [LOE] A).2,3 In heart failure with preserved ejection fraction (HFpEF), MRA may reduce risk of heart failure (HF) hospitalization.4 The 2017 ACC/AHA/HFSA updated guidelines recommend MRA use in appropriately selected HFpEF patients to decrease hospitalization (COR IIb, LOE B).5 Despite these recommendations, MRAs remain underutilized compared with other evidence-based therapy in eligible HF patients.6,7 It is estimated that only one-third of eligible hospitalized HF patients are prescribed a MRA on discharge.6 The risk of inducing hyperkalemia and renal dysfunction are identified as significant factors limiting the use of MRAs. Real-world observational studies reported relatively higher incidence of hyperkalemia and renal dysfunction compared with randomized controlled trials (RCT) especially in patients with chronic kidney disease (CKD).8,9 Additionally, the benefits of MRA use are not clear in patients with HF and Stage 3 CKD with an estimated glomerular filtration rate (eGFR) between 30 and 60 mL/min/1.73 m2. We therefore performed a systematic review to synthesize available data regarding efficacy and safety of MRA in patients with HF and CKD.
Methods
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA).10 PubMed, Embase, and Cochrane Central databases were systematically searched from inception to March 2019. Detailed search strategy for each database is provided in Appendix 1 of the supplement. The search was restricted to articles published in peer-reviewed journals. No filter for the type of study was applied; however, abstracts, meeting presentations, and case reports were excluded. There was no restriction of language. We also manually searched reference lists of retrieved articles to identify any relevant studies. All results were imported into EndNote x8.2 (Clarivate Analytics) and duplicate results were removed.
Two authors (MSK and AM) independently screened and selected studies using the defined search strategy. Any disagreements between the 2 authors were discussed with a third author (SK) and resolved with consensus. We included studies that reported outcomes of HF patients who were on MRA (spironolactone or eplerenone) and had reduced renal function, which was defined as eGFR <60 mL/min/1.73 m2. No restriction was applied based on the type of HF.
Data were independently extracted into a prespecified data extraction table. The efficacy outcomes of interest were adverse cardiovascular events, hospitalization for HF, and all-cause mortality. The safety outcomes of interest were incidence of hyperkalemia and worsening renal function (WRF) leading to dose reduction or drug discontinuation. Due to significant differences in study design and variation in reported outcome measures, meta-analysis was not performed. Risk of bias assessment was performed using Newcastle-Ottawa Score (NOS) for observational studies.11 NOS rates studies based on 3 broad perspectives: selection, comparability among study groups, and exposure/outcome assessment. It assigns a score between 0 and 9 to each study. Study with a score of less than 5 are considered of low quality, score of 5 to 7 of moderate quality, and score of more than 7 of high quality.
Results
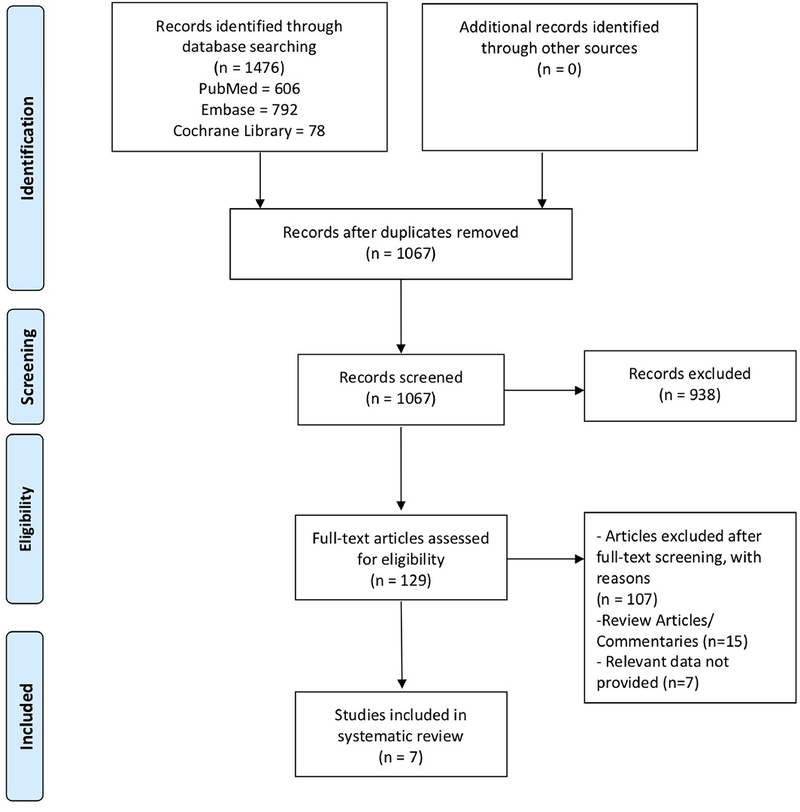
Figure 1 shows the PRISMA flow chart summarizing the search strategy. Initial search identified 1,476 potentially relevant articles, of which 1,067 remained after removing duplicates. After screening the titles and abstracts, 938 were excluded for not meeting the study criteria. Full text of the remaining 129 studies was obtained and after assessing the relevance, 7 studies consisting of 5,522 participants were included in the systematic review.12–18 Characteristics of included studies are outlined in Table 1. Of the 7 included studies, 3 were done in HFrEF,12–14 1 in HFpEF,15 2 in acute HF,16,17 and 1 in mixed patient population of HF.18 Three studies were post hoc analyses of multicenter RCTs,12,15,16 1 was a prespecified subgroup analysis of a multicenter RCT,13 2 were prospective observational studies,14,18 and 1 was a retrospective observational study.17 Six of the 7 studies used spironolactone12,14–18 as the MRA. Efficacy and safety outcomes reported in the included studies are summarized in Tables 2 and 3, respectively.
Figure 1. PRISMA flow chart outlining the literature search.
PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Table 1.
Baseline characteristics of included studies.
| Study authors, Year | Design | N | MRA | NYHA Functional Class | EF | eGFR Categories | Risk of Bias (NOS) |
|---|---|---|---|---|---|---|---|
| HFrEF | |||||||
| Vardney et al, 2012 | Post-hoc analysis of multi-centre RCT (RALES) | 792 | Spironolactone | III/IV | <35% | eGFR<60ml/min/1.73m2 | 9/9 |
| Eschalier et al, 2013 | Pre-specified subgroup analysis of multi-centre RCT (EMPHASIS-HF) | 912 | Eplerenone | II | 30<eGFR<60ml/min/1.73m2 | 7/9 | |
| Inampudi et al, 2014 | Prospective, Observational Study (Alabama Heart Failure Project) | 1140 | Spironolactone | Hospitalized HF | <45% | eGFR<60 ml/min/1.73m2 | 6/9 |
| HFpEF | |||||||
| Beldhuis et al, 2019 | Post-hoc analysis of multi-centre RCT (TOPCAT Americas study) | 944 | Spironolactone | II/III/IV | ≥45% | 45<eGFR<60ml/min/1.73m2 30<eGFR<45ml/min/1.73m2 |
9/9 |
| Acute HF | |||||||
| Greene et al, 2019 | Post hoc analysis of multicentre RCT (ATHENA-HF) | 360 | Spironolactone | Acute HF | All EF | 51<eGFR<71ml/min/1.73m2 30<eGFR<51ml/min/1.73m2 |
9/9 |
| Oh et al, 2015 | Retrospective, Observational Study (Korean Heart Failure Registry) | 1035 | Spironolactone | Hospitalized HF | All EF | eGFR<45 ml/min/1.73m2 | 6/6 |
| Mixed HF | |||||||
| Stubnova et al, 2017 | Prospective, Observational Study (Norwegian Heart Failure Registry) | 339 | Spironolactone | II/III/IV | All EF | eGFR<60 ml/min/1.73m2 | 6/6 |
Footnote: ejection fraction (EF), estimated glomerular filtration rate (eGFR), heart failure (HF), mineralocorticoid receptor antagonist (MRA), Newcastle-Ottawa scale (NOS), New York Heart Association functional class (NYHA), number of patients (n), randomized controlled trial (RCT).
Table 2.
Summary of reported efficacy outcomes of MRA as compared to placebo in included studies.
| Study authors, Year | All-cause Mortality | Heart Failure Readmission | All-Cause Readmission* | Composite Endpoint of CV mortality and/or HF readmission | Composite Endpoint of all-cause mortality and/or HF hospitalization |
|---|---|---|---|---|---|
| HFrEF | |||||
| Vardney et al, 2012 | HR 0.68, 95% CI 0.56–0.84 | NR | NR | NR | HR 0.67, 95% CI 0.56–0.81 |
| Eschalier et al, 2013 | NR | NR | NR | HR 0.62 95% CI 0.49–0.79, p=0.0001 | NR |
| Inampudi et al, 2014 | 30 day: PS adjusted HR 1.05 95% CI 0.60–1.82, p=0.866 1 year: PS adjusted HR 1.05 95% CI 0.83–1.31, p=0.706 |
30 day: PS adjusted HR 0.90 95% CI 0.57–1.41, p=0.635 1 year: PS adjusted HR 1.02 95% CI 0.80–1.30, p=0.847 |
30 day: PS adjusted HR 1.41 95% CI 1.04–1.90, p=0.027 1 year: PS adjusted HR 1.36 95% CI 1.13–1.63, p=0.001 |
NR | 30 day: PS adjusted HR 1.31 95% CI 0.99–1.73, p=0.058 1 year: PS adjusted HR 1.30 95% CI 1.09–1.54, p=0.003 |
| HFpEF | |||||
| Beldhuis et al, 2019 | NR | NR | NR | eGFR 45–60: HR 0.99, 95% CI 0.73–1.36; eGFR 30–45: HR 0.89, 95% CI 0.66–1.21, p=0.13 eGFR 45–60: 4-Yr ARD +1%, 95% CI −8% to +11%; eGFR 30–45: 4-Yr ARD – 9%, 95% CI −21% to +3% |
NR |
| Acute HF | |||||
| Greene et al, 2019 | NR | NR | 60 day: eGFR 51–71, HR 5.54, 95% CI 0.57–53.88, p=0.140; eGFR ≤50, HR, 12.11 95% CI 1.37–107.22, p=0.025 | NR | 30 day: eGFR 51–71, HR 0.51 95% CI 0.22–1.18, p=0.117; eGFR ≤50, HR, 0.98 95% CI 0.43–2.21, p=0.960 |
| Oh et al, 2015 | PS adjusted HR 0.65, 95% CI 0.35–1.19, p=0.16 | NR | IR 39.5% vs 35.7%, log rank P= 0.72 | NR | NR |
| Mixed HF | |||||
| Stubnova et al, 2017 | PS adjusted HR 0.59 95% CI 0.37–0.92 | NR | NR | NR | NR |
Footnote: absolute risk difference (ARD), cardiovascular (CV), confidence interval (CI), estimated glomerular filtration rate (eGFR), hazards ratio (HR), heart failure (HF), heart failure with preserved ejection fraction (HFpEF), heart failure with reduced ejection fraction (HFrEF), incidence rate (IR), mineralocorticoid receptor antagonist (MRA), not reported (NR), odd ratio (OR), propensity scored (PS), versus (vs).
eGFR values are reported in mL/min/1.73 m2.
Table 3:
Summary of reported safety outcomes of MRA as compared to placebo in included studies.
| Study authors, Year | Hyperkalemia * | Worsening renal function (change in eGFR) ** | Dose reduction or drug discontinuation due to adverse effects |
|---|---|---|---|
| HFrEF | |||
| Vardney et al, 2012 | Serum K+ >5.5 mmol/l: OR 3.7, 95% CI 2.5–5.7 | IR 17% vs 7%, p< 0.001 | OR 2.3, 95% CI 1.2–4.7 |
| Eschalier et al, 2013 | Serum K+ >5.5 mmol/l: IR 16.6% vs 9.3%, p=0.002 Serum K+ >6 mmol/l: IR 1.9% vs 3.3%, p=0.29 |
Mean ±SD 2.04 ±17.0 vs 4.15 ±14.9 | IR 16.1% vs 22.3%, p<0.05 |
| Inampudi et al, 2014 | NR | NR | NR |
| HFpEF | |||
| Beldhuis et al, 2019 | NR | eGFR 45–60, HR 3.80 95% CI 2.24–6.45; eGFR 30–45, HR 2.12 95% CI 1.41–3.19, p=0.46 eGFR 45–60: 4-Yr ARD +24%, 95% CI + 14% to +33%; eGFR 30–45: 4-Yr ARD +27%, 95% CI +12% to +42% |
NR |
| Acute HF | |||
| Greene et al, 2019 | 30 day: IR of ≤ 2% for both groups. | NR | NR |
| Oh et al, 2015 | NR | NR | NR |
| Mixed HF | |||
| Stubnova et al, 2017 | Δ potassium: Mean ± SD 0.31 ± 0.55 vs 0.05 ± 0.41 mmol/l, p<0.0001 | Δ eGFR: Mean ± SD −4.12 ± 12.2 vs −0.98 ± 7.88 ml/min/1.73 m2, p= 0.006 | NR |
Footnote: absolute risk difference (ARD), change (Δ), confidence interval (CI), estimated glomerular filtration rate (eGFR), hazards ratio (HR), heart failure (HF), heart failure with preserved ejection fraction (HFpEF), heart failure with reduced ejection fraction (HFrEF), incidence rate (IR), mineralocorticoid receptor antagonist (MRA), not reported (NR), odd ratio (OR), propensity scored (PS), standard deviation (SD), serum potasium (K+), versus (vs).
Serum K+ values are reported in mmol/L.
eGFR values are reported in mL/min/1.73 m2.
Quality of included studies varied from high to moderate (range 6 to 9; Table 1). Post hoc analyses of RCTs were of high quality with no evidence of selection bias and with good comparability between cases and controls as well as outcome assessment. However, propensity scored observational studies were of moderate quality and lacked good comparability between cases and controls.
We identified 3 studies which evaluated the outcomes related to MRA use in HFrEF and CKD: (1) post hoc analysis of Randomized Aldactone Evaluation Study (RALES),12 (2) prespecified analysis of Eplerenone in Mild Patients Hospitalization and Survival Study in Heart Failure (EMPHASIS-HF),13 and (3) prospective observational propensity scored cohort study in hospitalized Medicare beneficiaries (Alabama Heart Failure Project).14
In the post hoc analysis of RALES, patients with reduced baseline eGFR (<60 mL/min/1.73 m2) had similar relative risk reductions in all-cause mortality and combined end point of death or hospital stays for HF compared with those with higher baseline eGFR (>60 mL/min/1.73 m2); and greater absolute risk reduction than those with higher baseline eGFR (10.3% vs 6.4%, respectively). Although the incidence of WRF (defined as ≥30% reduction in estimated eGFR from baseline up to 12 weeks of follow up) was higher in spironolactone group, it was not associated with increased mortality in these patients (hazard ratio [HR] 1.1, 95% confidence interval [CI] 0.8 to 1.5). However, in the placebo group, patients with WRF exhibited increased mortality compared with those without WRF (HR 1.9, 95% CI 1.3 to 2.6).
In the prespecified analysis of EMPHASIS-HF study, eplerenone was effective in reducing primary composite end point of cardiovascular mortality or HF hospitalization in patients with reduced renal function (HR 0.62, 95% CI 0.49 to 0.79, p = 0.0001). Although use of eplerenone was associated with increased incidence of mild hyperkalemia (serum potassium >5.5 mmol/L) compared with placebo (16.6% vs 9.3%, p = 0.002), the rate of serious hyperkalemia (serum potassium >6 mmol/L) did not significantly differ between the 2 groups (1.9% vs 3.3%, p = 0.29). Also, there was no significant increase in the frequency of WRF between 2 groups (change in eGFR from baseline to final visit, mean [SD] 2.04 [17.0] vs 4.15 vs [14.9]).
Inampudi et al14 examined spironolactone use and hospital readmission rate in hospitalized Medicare beneficiaries using data from Alabama Heart Failure Project. They derived propensity scores for spironolactone treatment to create matched cohort and calculated HR. They found no association of spironolactone use with all-cause mortality and HF readmissions in patients with HFrEF (EF <45%) and advance CKD (eGFR <45 mL/min/1.73 m2) (HR 1.05, 95% CI 0.60 to 1.82; p = 0.866 and HR 0.90, 95% CI 0.57 to 1.41; p = 0.635, respectively). However, individuals on spironolactone therapy had a higher 30-day and 1-year risk of all-cause readmissions than those not on MRA therapy (HR 1.41, 95% CI 1.04 to 1.90; p = 0.027 and HR 1.36, 95% CI 1.13 to 1.63; p = 0.001, respectively).
We found only 1 study that reported outcomes of MRA use in patients with HFpEF and CKD, post hoc analysis of Treatment of Preserved Cardiac Function Heart Failure With an Aldosterone Antagonist Trial (TOPCAT) Americas study. The study assessed the association between baseline eGFR (stratified in to 3 categories: <45, 45 to 59, and ≥60 mL/min/1.73 m) and primary efficacy outcome (cardiovascular mortality, aborted cardiac arrest, or HF hospitalization) as well as safety outcomes (hyperkalemia, WRF, and permanent drug discontinuation). They found that risk for primary composite end point of cardiovascular death, HF hospitalization, and aborted cardiac death was similarly reduced across all GFR categories with spironolactone use compared with placebo (p for interaction = 0.13). However, spironolactone use was associated with higher incidence of hyperkalemia of >5.5 mmol/L and worsening function leading to permanent drug discontinuation (eGFR 45 to 60 mL/min/1.73 m, HR 3.80; 95% CI 2.24 to 6.45; eGFR 30 to 45 mL/min/1.73 m, HR 2.12; 95% CI 1.41 to 3.19; p = 0.46). The difference in absolute risk for permanent drug discontinuation for adverse events with spironolactone use was much higher in lower eGFR categories, p for interaction = 0.003). The authors concluded that the use of spironolactone in patients with HFpEF and impaired renal function should only be considered when close laboratory surveillance is possible.
We found 2 studies which evaluated the role of MRA in acute HF patients and CKD: post hoc analysis of Aldosterone Targeted Neurohormonal Combined with Natriuresis Therapy in Heart Failure (ATHENA-HF) trial16 and retrospective observational propensity scored study from Korean Heart Failure Registry.17
In the post hoc analysis of ATHENA-HF trial, there was no significant difference in the primary end point of change in log NT-pro-BNP (eGFR 51 to 71 mL/min/1.73 m, HR 0.23, 95% CI 0.01 to 0.45, p = 0.041; eGFR ≤50 mL/min/1.73 m, HR 0.22, 95% CI 0.01 to 0.43, p = 0.041), as well as secondary clinical end points of 30-day worsening HF (eGFR 51 to 71 mL/min/1.73 m, HR 0.51, 95% CI 0.22 to 1.18, p = 0.117; eGFR ≤50 mL/min/1.73 m, HR 0.98, 95% CI 0.43 to 2.21, p = 0.960) and 60-day all-cause mortality (eGFR 51 to 71 mL/min/1.73 m, HR 5.54, 95% CI 0.57 to 53.88, p = 0.140; eGFR ≤50 mL/min/1.73 m, HR 12.11, 95% CI 1.37 to 107.22, p = 0.025) between spironolactone and usual care regardless of baseline eGFR. There was no increased risk of hyperkalemia or WRF with spironolactone therapy. In the Korean Heart Failure Registry, they found no significant difference in all-cause mortality between spironolactone users and nonusers (19.0% vs 25.7%, respectively, log rank p = 0.115).
We identified 1 study which reported outcomes on spironolactone use in a mixed patient population of HF and reduced renal function (eGFR <60 mL/min/1.73 m).18 Using data from Norwegian Heart Failure Registry, authors identified patients started on spironolactone in outpatient HF clinics and created a matched cohort by deriving propensity scores. Patients receiving spironolactone had a lower 2-year all-cause mortality compared with those not receiving spironolactone therapy (HR 0.59, 95% CI 0.37 to 0.92, p = 0.020). The survival benefit was observed in spironolactone group despite increases in potassium concentrations (change in potassium 0.31 ± 0.55 vs 0.05 ± 0.41 mmol/L, p = 0.006) and decreases in eGFR over time (change in eGFR −4.12 ± 12.2 vs −0.98 ± 7.88 mL/min/1.73 m2, p = 0.006).
Discussion
There is consistent ample evidence supporting use of MRA in patients with HF from randomized controlled studies. However, most of these randomized studies have either underrepresented or excluded individuals with CKD. In this systematic review, we found evidence for benefit of MRA use in patients with reduced renal function and HF, both HFrEF and HFpEF. The post hoc analyses of randomized control trials in CKD patients found consistent efficacy in reducing morbidity and mortality with MRA use irrespective of renal functions. Although there was increased risk of hyperkalemia and WRF with MRA use, the overall benefit of improving cardiovascular outcomes and mortality was preserved in patients with reduced renal function (eGFR between 30 and 60 mL/min/1.73 m). These results were not reflected in the prospective observational propensity-based studies, but conclusions from these studies were limited due to residual confounding and concern for bias. Therefore, it appears that MRA use is reasonable in patients with HFrEF and reduced renal function (eGFR between 30 and 60 mL/min/1.73 m) to decrease mortality and cardiovascular morbidity and in appropriately selected patients of HFpEF (with EF ≥45%, elevated BNP levels or HF admission within 1 year, eGFR >30 mL/min/1.73 m, creatinine <2.5 mg/dL, potassium <5.0 mEq/L) to decrease hospitalization, as recommended by recent updated 2017 ACC/AHA/HFSA guidelines. Also, it is important to note that patients with impaired renal function who are started on MRA, should undergo close monitoring of serum potassium and renal function.
Mineralocorticoid receptor (MR) is a ligand-activated transcription factor that belongs to nuclear hormone receptor superfamily. Besides mineralocorticoids, it also binds to glucocorticoids with equal or higher affinity.19 MRs are expressed in a variety of tissues including kidneys, heart, blood vessels, adipose tissue, and central nervous system. In kidneys, activation of MRs in distal nephrons by aldosterone fulfills the major physiological function of maintaining sodium, potassium balance, and blood pressure regulation. However, when inappropriately activated, they are associated with deleterious effects. Dysregulation and overactivation of MRs has been shown to play crucial role in pathophysiology of cardiac and renal diseases.20 Studies in animals support that abnormal activation of MRs lead to increased oxidative stress, inflammation, and fibrosis. This is associated with pathologic remodeling of tissues.21 MR blockade attenuates some of these deleterious effects and improve outcomes. Beneficial effects of MRA in HF patients are well demonstrated in large randomized studies. Similarly MRAs have shown to have renoprotective effects by reducing proteinuria and delaying progression of CKD.22 Despite these benefits, use of MRA remains limited in CKD patients due to the risk of inducing hyperkalemia. In our systematic review as well, studies reported increased risk of hyperkalemia with MRA use in individuals with HF and CKD. Novel potassium binders just released on the market and approved by US Food and Drug Administration (FDA) may alleviate some of the concerns regarding hyperkalemia in individuals on MRA therapy (Table 4). Agents such as patiromer and sodium zirconium cyclosilicate (SZC) can potentially allow long-term use of MRA at adequate doses along with other renin angiotensin aldosterone system inhibitor therapy in patients with HF and CKD.23 However, their long-term efficacy and safety in individuals with HF and CKD still needs to be established.
Table 4:
Summary of clinical trials with novel potassium binders reporting RAASi use.
| Trial Name, Year | Drug | Study Design | Patients | Intervention | RAASi Dose |
|---|---|---|---|---|---|
| PEARL-HF, Pitt et al, 2011 | Patiromer | Multicenter RCT | 105 HF patients on standard therapy and spironolactone. 27% had an eGFR <60 mL/min/1.73 m2 | Patiromer treatment with 3g/day vs placebo for 4 weeks | 91% patients on patiromer had spironolactone dose increased to 50 mg/day (vs 74% in the control group, p = 0.019) |
| OPAL-HK, Weir et al, 2015 | Patiromer | Multicenter RCT | 243 CKD (eGFR, 15 to <60 mL/min/1.73 m2) patients with hyperkalemia (K+ levels 5.1 –6.5 mmol/L) on RAASi therapy | Initial Phase: Patiromer treatment with 4.2 or 8.4 g/day twice daily for 4 weeks Randomized Phase: Patiromer continued at same dose or switched to placebo for 8 weeks |
52% of controls discontinued RAASi compared with 5% on patiromer |
| ZS-002, Ash et al, 2015 | Sodium Zirconium Cyclosilicate | Phase 2 Double-Blinded Multicenter RCT | 90 CKD (eGFR, 30 to 60 mL/min/1.73 m2) patients with hyperkalemia (K+ levels 5 –6 mmol/L). 62% of patients were on RAASi | SZC treatment with 0.3g or 3g or 10g three times/day or placebo through 48 hrs | In patients on RAASi, −1.05 ± 0.47 (mean± SD) change in serum potassium from baseline on ZS-9 (10g) compared to −0.25 ±0.46 on placebo (p<0.001) |
| ZS 005, Spinowitz et al, 2017 | Sodium Zirconium Cyclosilicate | Phase 3 Open-Label Multicenter Single Arm Trial | 751 patients with hyperkalemia (K+ >5.1 mmol/l). 74% had an eGFR <60 mL/min/1.73 m2. At baseline, 65% of patients were on RAASi | Acute phase: SZC treatment with 10g three times/ day for 24–72 hr Maintenance phase: SZC treatment with 5mg/ day titrated to maintain normokalemia |
74% of the patients maintained RAASi dose while 13% increased their dose |
CKD = chronic kidney disease; eGFR = estimated glomerular filtration rate; g = grams, HF = heart failure; mg = milligram; RAASi = renin-angiotensinaldosterone-system inhibitor; RCT = randomized controlled trial; K+ = serum potassium; SD = standard deviation; SZC = sodium zirconium cyclosilicate; vs = versus.
eGFR values are reported in mL/min/1.73 m2, K+ levels are reported in mmol/L.
Another important high-risk group of patients in which the role of MRAs is unclear are patients with end stage renal disease (ESRD). Cardiovascular diseases remain the leading cause of mortality in dialysis patients.24 ESRD patients have elevated circulating levels of aldosterone and may benefit from MRA treatment. There are a number of studies that have shown cardioprotective effects of MRA in dialysis patients and demonstrated safety especially in regard to hyperkalemia.25,26 A study by Taheri et al27 enrolled 16 hemodialysis patients with HF and low EF ≤45% and randomized them to receive spironolactone or placebo. After 6 months, they found significant improvement in mean EF in spironolactone group compared with placebo (6.2 ± 1.64 vs 0.83 ± 4.9%, p = 0.046) without significant increase in the incidence of hyperkalemia. However, most of the studies, including aforementioned study, have small sample sizes with limited follow-up duration. Further studies investigating the efficacy and safety of MRA use in patients with ESRD are needed.
A recent meta-analysis reported a 66% relative risk reduction of cardiovascular mortality with MRA use compared with placebo or standard care in dialysis patients. All-cause mortality was significantly reduced with MRA use (RR 0.40, 95% CI 0.23, 0.69); however, there was 3-fold increase risk of hyperkalemia. The effect of MRAs was attenuated and results were not statistically significant when authors performed sensitivity analysis to account for loss of follow-up as well as when assuming the worst-case scenario.28 Limitations in study design make this meta-analysis difficult to interpret; however, it fills an important gap in the literature and demonstrates the lack of quality evidence guiding our clinical decision-making regarding the use of MRA in patients with ESRD. The are 2 ongoing large scale, multicenter, RCTs; ALCHEMIST (ALdosterone antagonist Chronic HEModialysis Interventional Survival Trial; NCT01848639) and ACHIEVE (Aldosterone bloCkade for Health Improvement EValuation in End-stage Renal Disease trial; NCT03020303), which are likely to provide important information regarding use of MRA in dialysis patients.
Although we conducted a thorough review of the literature with strict selection criteria, we acknowledge a number of limitations. First, any systematic review may have a component of publication bias. Second, all the included studies were observational or post hoc analyses of RCTs. Third, the baseline characteristics of patients differed in studies with difference in the severity of heart failure as well as renal dysfunction.
In conclusion, MRAs are an important part of the treatment of HF and associated with improved clinical outcomes. This benefit appears to be preserved in patients with reduced renal function (eGFR between 30 and 60 mL/min/1.73 m).
Supplementary Material
Footnotes
Disclosures
The authors have no conflict of interest to disclose.
Supplementary materials
Supplementary material associated with this article can be found in the online version at https://doi.org/10.1016/j.amjcard.2019.11.014.
References
- 1.Zannad F, Gattis Stough W, Rossignol P, Bauersachs J, McMurray JJ, Swedberg K, Struthers AD, Voors AA, Ruilope LM, Bakris GL, O’Connor CM, Gheorghiade M, Mentz RJ, Cohen-Solal A, Maggioni AP, Beygui F, Filippatos GS, Massy ZA, Pathak A, Pina IL, Sabbah HN, Sica DA, Tavazzi L, Pitt B. Mineralocorticoid receptor antagonists for heart failure with reduced ejection fraction: integrating evidence into clinical practice. Eur Heart J 2012;33:2782–2795. [DOI] [PubMed] [Google Scholar]
- 2.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr., Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL. American College of Cardiology F. American Heart Association Task Force on Practice G. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol 2013;62:e147–e239. [DOI] [PubMed] [Google Scholar]
- 3.Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, Gonzalez-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P. Authors/Task Force M. Document R. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 2016;18:891–975. [DOI] [PubMed] [Google Scholar]
- 4.Pfeffer MA, Braunwald E. Treatment of heart failure with preserved ejection fraction: reflections on its treatment with an aldosterone antagonist. JAMA Cardiol 2016;1:7–8. [DOI] [PubMed] [Google Scholar]
- 5.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr., Colvin MM, Drazner MH, Filippatos GS, Fonarow GC, Givertz MM, Hollenberg SM, Lindenfeld J, Masoudi FA, McBride PE, Peterson PN, Stevenson LW, Westlake C. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines and the Heart Failure Society of America. Circulation 2017;136:e137–e161. [DOI] [PubMed] [Google Scholar]
- 6.Fonarow GC, Yancy CW, Hernandez AF, Peterson ED, Spertus JA, Heidenreich PA. Potential impact of optimal implementation of evidence-based heart failure therapies on mortality. Am Heart J 2011;161:1024–1030. e1023. [DOI] [PubMed] [Google Scholar]
- 7.Albert NM, Yancy CW, Liang L, Zhao X, Hernandez AF, Peterson ED, Cannon CP, Fonarow GC. Use of aldosterone antagonists in heart failure. JAMA 2009;302:1658–1665. [DOI] [PubMed] [Google Scholar]
- 8.Wang TY, Vora AN, Peng SA, Fonarow GC, Das S, de Lemos JA, Peterson ED. Effectiveness and safety of aldosterone antagonist therapy use among older patients with reduced ejection fraction after acute myocardial infarction. J Am Heart Assoc 2016;5:e002612. 10.1161/JAHA.115.002612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hernandez AF, Mi X, Hammill BG, Hammill SC, Heidenreich PA, Masoudi FA, Qualls LG, Peterson ED, Fonarow GC, Curtis LH. Associations between aldosterone antagonist therapy and risks of mortality and readmission among patients with heart failure and reduced ejection fraction. JAMA 2012;308:2097–2107. [DOI] [PubMed] [Google Scholar]
- 10.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle−Ottawa Scale (NOS) for Assessing the Quality of Non-randomized Studies in Meta-Analysis. Ottawa, Ontario: The Ottawa Health Research Institute. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (April 03, 2019, date last accessed). [Google Scholar]
- 12.Vardeny O, Wu DH, Desai A, Rossignol P, Zannad F, Pitt B, Solomon SD, Investigators R. Influence of baseline and worsening renal function on efficacy of spironolactone in patients with severe heart failure: insights from RALES (Randomized Aldactone Evaluation Study). J Am Coll Cardiol 2012;60:2082–2089. [DOI] [PubMed] [Google Scholar]
- 13.Eschalier R, McMurray JJ, Swedberg K, van Veldhuisen DJ, Krum H, Pocock SJ, Shi H, Vincent J, Rossignol P, Zannad F, Pitt B, Investigators E-H. Safety and efficacy of eplerenone in patients at high risk for hyperkalemia and/or worsening renal function: analyses of the EMPHASIS-HF study subgroups (Eplerenone in Mild Patients Hospitalization And Survival Study in Heart Failure). J Am Coll Cardiol 2013;62:1585–1593. [DOI] [PubMed] [Google Scholar]
- 14.Inampudi C, Parvataneni S, Morgan CJ, Deedwania P, Fonarow GC, Sanders PW, Prabhu SD, Butler J, Forman DE, Aronow WS, Allman RM, Ahmed A. Spironolactone use and higher hospital readmission for Medicare beneficiaries with heart failure, left ventricular ejection fraction <45%, and estimated glomerular filtration rate <45 ml/min/1.73 m(2.). Am J Cardiol 2014;114:79–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beldhuis IE, Myhre PL, Claggett B, Damman K, Fang JC, Lewis EF, O’Meara E, Pitt B, Shah SJ, Voors AA, Pfeffer MA, Solomon SD, Desai AS. Efficacy and safety of spironolactone in patients with HFpEF and chronic kidney disease. JACC Heart Fail 2019;7:25–32. [DOI] [PubMed] [Google Scholar]
- 16.Greene SJ, Felker GM, Giczewska A, Kalogeropoulos AP, Ambrosy AP, Chakraborty H, DeVore AD, Fudim M, McNulty SE, Mentz RJ, Vaduganathan M, Hernandez AF, Butler J. Spironolactone in acute heart failure patients with renal dysfunction and risk factors for diuretic resistance: from the ATHENA-HF trial. Can J Cardiol 2019;35:1097–1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Oh J, Kang SM, Song MK, Hong N, Youn JC, Han S, Jeon ES, Cho MC, Kim JJ, Yoo BS, Chae SC, Oh BH, Choi DJ, Lee MM, Ryu KH. Clinical benefit of spironolactone in patients with acute decompensated heart failure and severe renal dysfunction: data from the Korean Heart Failure Registry. Am Heart J 2015;169:713–720. e713. [DOI] [PubMed] [Google Scholar]
- 18.Stubnova V, Os I, Grundtvig M, Atar D, Waldum-Grevbo B. Spironolactone treatment and effect on survival in chronic heart failure patients with reduced renal function: a propensity-matched study. Cardiorenal Med 2017;7:128–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hawkins UA, Gomez-Sanchez EP, Gomez-Sanchez CM, Gomez-Sanchez CE. The ubiquitous mineralocorticoid receptor: clinical implications. Curr Hypertens Rep 2012;14:573–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tesch GH, Young MJ. Mineralocorticoid receptor signaling as a therapeutic target for renal and cardiac fibrosis. Front Pharmacol 2017;8:313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bertocchio JP, Warnock DG, Jaisser F. Mineralocorticoid receptor activation and blockade: an emerging paradigm in chronic kidney disease. Kidney Int 2011;79:1051–1060. [DOI] [PubMed] [Google Scholar]
- 22.Currie G, Taylor AH, Fujita T, Ohtsu H, Lindhardt M, Rossing P, Boesby L, Edwards NC, Ferro CJ, Townend JN, van den Meiracker AH, Saklayen MG, Oveisi S, Jardine AG, Delles C, Preiss DJ, Mark PB. Effect of mineralocorticoid receptor antagonists on proteinuria and progression of chronic kidney disease: a systematic review and meta-analysis. BMC Nephrol 2016;17:127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rosano GMC, Tamargo J, Kjeldsen KP, Lainscak M, Agewall S, Anker SD, Ceconi C, Coats AJS, Drexel H, Filippatos G, Kaski JC, Lund L, Niessner A, Ponikowski P, Savarese G, Schmidt TA, Seferovic P, Wassmann S, Walther T, Lewis BS. Expert consensus document on the management of hyperkalaemia in patients with cardiovascular disease treated with renin angiotensin aldosterone system inhibitors: coordinated by the working group on cardiovascular pharmacotherapy of the European Society of Cardiology. Eur Heart J Cardiovasc Pharmacother 2018;4:180–188. [DOI] [PubMed] [Google Scholar]
- 24.Saran R, Li Y, Robinson B, Ayanian J, Balkrishnan R, Bragg-Gresham J, Chen JT, Cope E, Gipson D, He K, Herman W, Heung M, Hirth RA, Jacobsen SS, Kalantar-Zadeh K, Kovesdy CP, Leichtman AB, Lu Y, Molnar MZ, Morgenstern H, Nallamothu B, O’Hare AM, Pisoni R, Plattner B, Port FK, Rao P, Rhee CM, Schaubel DE, Selewski DT, Shahinian V, Sim JJ, Song P, Streja E, Kurella Tamura M, Tentori F, Eggers PW, Agodoa LY, Abbott KC. US renal data system 2014 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis 2015;66. Svii, S1–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Matsumoto Y, Mori Y, Kageyama S, Arihara K, Sugiyama T, Ohmura H, Yakushigawa T, Sugiyama H, Shimada Y, Nojima Y, Shio N. Spironolactone reduces cardiovascular and cerebrovascular morbidity and mortality in hemodialysis patients. J Am Coll Cardiol 2014;63:528–536. [DOI] [PubMed] [Google Scholar]
- 26.Pitt B, Rossignol P. Mineralocorticoid receptor antagonists in patients with end-stage renal disease on chronic hemodialysis. J Am Coll Cardiol 2014;63:537–538. [DOI] [PubMed] [Google Scholar]
- 27.Taheri S, Mortazavi M, Shahidi S, Pourmoghadas A, Garakyaraghi M, Seirafian S, Eshaghian A, Ghassami M. Spironolactone in chronic hemodialysis patients improves cardiac function. Saudi J Kidney Dis Transpl 2009;20:392–397. [PubMed] [Google Scholar]
- 28.Quach K, Lvtvyn L, Baigent C, Bueti J, Garg AX, Hawley C, Haynes R, Manns B, Perkovic V, Rabbat CG, Wald R, Walsh M. The safety and efficacy of mineralocorticoid receptor antagonists in patients who require dialysis: a systematic review and meta-analysis. Am J Kidney Dis 2016;68:591–598. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.