Abstract
SUMMARY: Tongue abscess is a very rare condition about which only sparse imaging findings have been reported. In 2 patients, a submucosal malignant tumor was suspected because of the presence of a painful hard tongue mass with intact mucosal surface. Differential diagnosis of the tongue abscess or malignancy was difficult on MR imaging or positron emission tomography-CT. In careful retrospective history taking, the symptoms had dated from an episode of eating fish several months before presentation. Plain radiographs and noncontrast CT images of the pharynx revealed a foreign body within the lesion. Thus, we present the imaging findings of 2 cases of malignancy mimicking tongue abscess as a result of impaction of a fish bone.
Abscess of the tongue is a very rare condition that occurs in immunocompromised patients or in healthy persons with pierced tongues.1,2 Over the last 30 years, only 50 cases of glossal abscess have been reported in the English literature,1 and tongue abscess due to fish bone impaction is even rarer. We have encountered 2 cases of fish bone-induced tongue abscess that were initially suspected to be clinical malignancies. We now report the plain radiograph, MR, CT, and positron-emission tomography (PET)-CT findings of tongue abscess induced by a fish bone.
Case Reports
Case 1
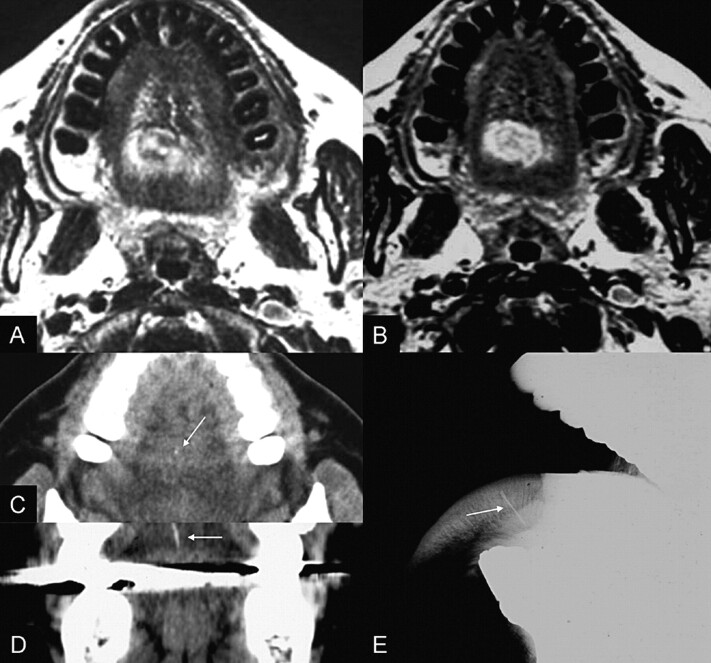
A 52-year-old woman was admitted with a painful mass found incidentally on the tongue. On physical examination, a 3-cm diameter hard mass was found at the right dorsum of the tongue, and a tongue malignancy was suspected. To rule out a malignant mass, oropharynx MR imaging was performed. An axial T2-weighted MR image revealed mixed signal intensities at the right posterior tongue (Fig 1A). An axial T1-weighted MR image demonstrated hypointensity of the lesion. An axial Gd-enhanced T1-weighted MR image showed relatively well-marginated, inhomogeneous, target-like enhancement of the lesion (Fig 1B). In retrospect, the symptoms had dated from an episode of eating fish 5 months before. For evaluation of the fish bone, a noncontrast CT image of the pharynx was obtained and revealed a subtle high-attenuation spot within the lesion (Fig 1C). Plain radiograph of the tongue demonstrated a linear radiopaque foreign body within the tongue (Fig 1D). An 11-mm long fish bone with pus was removed surgically. Follow-up MR images revealed decreased size of the inflammatory mass. The patient had no further symptoms after removal of the fish bone and treatment with antibiotics.
Fig 1.
An axial T2-weighted MR image (A) reveals mixed signal intensities with minimal surrounding edema in the right posterior mobile tongue. Gd-enhanced T1-weighted MR image (B) demonstrates relatively well-defined, lobulated, and inhomogeneous ovoid enhancement of the lesion. A small, subtle, dot-like hyperattenuation is revealed on the noncontrast axial CT image (C, arrow), and a linear hyperattenuation on the coronal reformatted CT image (D, arrow). Plain radiograph (D) reveals a linear radiopaque foreign body impacted vertically in the posterior of the mobile tongue (arrow).
Case 2
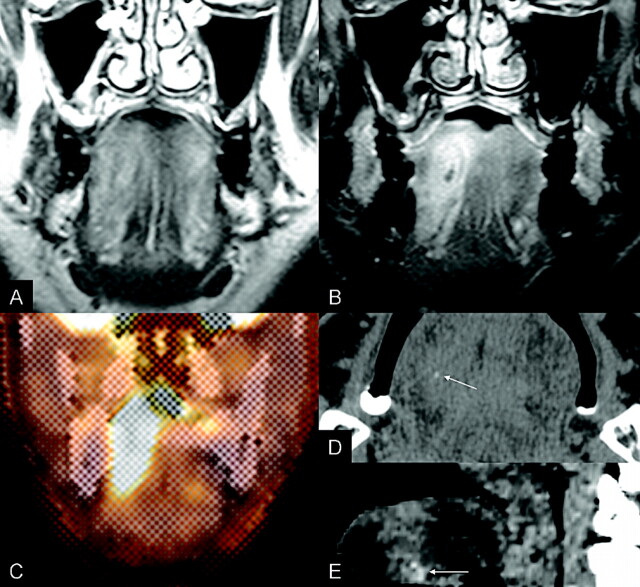
A 58-year-old man complained of a mass and of tenderness in the right tongue of 4 months’ duration. The symptoms decreased with antibiotic treatment; however, they recurred twice. On physical examination, a 3-cm diameter hard mass was palpable in the middle of the tongue, and a tongue malignancy was suspected. Oropharynx MR images were obtained. T2-weighted images (Fig 2A) revealed subtle and ill-defined hyperintensity to the right of the middle of the tongue. T1-weighted revealed hypointensity of the lesion. Gd-enhanced T1-weighted images (Fig 2B) showed a 4 × 1.6-cm, vertically ovoid, target-like enhancement. To rule out a tongue malignancy, a PET-CT scan was obtained. There was a high glucose metabolic focal lesion in the right of the middle of the tongue (standard uptake value, 7.4) (Fig 2C) supporting a malignant tumor. On physical examination and PET-CT findings, a tongue malignancy was suspected. However, an abscess could also not be ruled out on the MR images. In retrospect, the symptoms had dated from an episode of eating fish 4 months previously. To find the fish bone, a noncontrast pharynx CT scan was obtained. A faint dot of hyperattenuation was revealed within the lesion (Fig 2D). A 6-mm long fish bone with pus was removed surgically. Follow-up MR images revealed a decrease of the mass size. The patient had no symptoms after surgery and antibiotic treatment.
Fig 2.
T2-weighted MR image (A) demonstrates subtle and ill-defined hyperintensity to the right of the middle of the tongue. Gd-enhanced T1-weighted MR image (B) reveals a 4 × 1.6-cm, vertically ovoid, target-like enhancement. The PET-CT image (C) demonstrates a hypermetabolic lesion in the right tongue with a measured peak SUV of 7.4. Noncontrast axial (D) and sagittal reformatted (E) CT images show a small foreign body (arrow) within the slightly hyperattenuated lesion of the anterior tongue.
Discussion
Although the tongue is subject to constant trauma, inflammatory conditions resulting from acute trauma are rare, probably because of the tongue’s rich blood supply, unique muscular anatomy, the thickness of the covering mucous membrane, and the cleansing action of saliva.3 Tongue infection is the result of the interaction between the compromised local or systemic defense and pathogenic microorganisms. The first line of defense against an invading microorganism is the mechanical barrier of the tongue mucosa. Once this first line of defense is breached and the host immune system is compromised, tongue infection can be severe and recalcitrant.1
The differential diagnosis of tongue abscess includes a number of diseases that may appear as lingual swelling such as tumor, cyst, infarction, edema, infection, hemorrhage, metabolic macroglossia in hyperpituitarism or hypothyroidism or developmental macroglossia in lingual thyroid or ectopic lymphoid tissue.4,5 Although the impaction of a fish bone in the pharynx usually occurs at the base of the tongue or in the vallecula, it is uncommon in the mobile tongue.6 Abscesses located in the mobile tongue are easy to diagnose on the basis of the physical findings. However, those situated in the base of tongue may pose a diagnostic challenge,5 because the symptoms are less specific and other inflammatory processes, such as peritonsillitis or infection of the floor of the mouth, may be indistinguishable.7 The clinicians in the present cases had a different impression of the patient’s condition, which they assumed to involve tongue cancer. The lesions in the present cases were located deep in the tongue, and the mucosal surface of the tongue was intact on the physical examination and MR images. These findings required differential diagnosis as submucosally located nonsquamous cell malignancies, such as adenoid cystic carcinoma, mucoepidermoid carcinoma originating from the minor salivary gland or lymphoma.8 Although the radiologic findings for such submucosal neoplasms are nonspecific, CT and MR imaging can have an important role in the diagnostic work-up of these unusual tumors.
The usefulness of CT in the depiction of oral cavity tumors is well established. However, dental amalgam artifacts and beam-hardening artifacts caused by the attenuated mandibular bone may obscure the CT findings. MR imaging, however, produces superior soft-tissue detail without artifact from the mandible or dental amalgams. The main drawback of MR imaging is its lack of specificity. An area of low signal intensity on T1-weighted images, high signal intensity on T2-weighted images, and target-like enhancement on Gd-enhanced T1-weighted images may correspond to either neoplastic or inflammatory tissue.9 In the present cases, noncontrast CT was diagnostic for visualization of the hyperattenuated foreign body. With T1- or T2-weighted MR images, differential diagnosis of an abscess from a malignant mass was difficult because of the nonspecific low signal intensity of the lesions on T1-weighted images and the high signal intensity on T2-weighted MR images. Both presenting cases showed target-like enhancement (Figs 1B and 2B), which cannot differentiate an abscess from a large tongue cancer with central necrosis.10
The diagnostic accuracy of PET is 8%–43% greater than that of conventional procedures.11 However, differentiation of malignant from benign lesions is difficult using the standard uptake value of fluoro-2-deoxy-d-glucose on PET scanning.12 In the present case 2, PET scanning showed a standardized uptake value of 7.4 of the lesion, thereby suggesting a malignant tumor. It is unlikely that a nonspecific marker of metabolic activity, such as fluoro-2-deoxy-d-glucose, will be able to differentiate tumor from inflammation with complete accuracy; this will be possible only with tumor-specific markers or with significantly improved quantitative methods.13
Conclusion
Lingual abscess due to fish bone impaction is rare. We experienced 2 cases of fish bone-induced tongue abscess that were clinically suspected of being malignancies. MR or PET-CT images may confuse diagnosis. With history of fish bone impaction, the finding of a foreign body on plain radiographs or CT images may help in determining the differential diagnosis.
References
- 1.Antoniades K, Hadjipetrou L, Antoniades V, et al. Acute tongue abscess. Report of three cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004;97:570–73 [DOI] [PubMed] [Google Scholar]
- 2.Olsen JC. Lingual abscess secondary to body piercing. J Emerg Med 2001;20:409. [DOI] [PubMed] [Google Scholar]
- 3.Jain HK, Bhatia PL. Lingual abscess. J Laryngol Otol 1970;84:637–41 [DOI] [PubMed] [Google Scholar]
- 4.Rubin MM, Gatta CA, Cozzi GM, et al. Painful tongue mass. J Oral Maxillofac Surg 1990;48:728–31 [DOI] [PubMed] [Google Scholar]
- 5.Reneham A, Morton M. Acute enlargement of the tongue. Br J Oral Maxillofac Surg 1993;31:321–24 [DOI] [PubMed] [Google Scholar]
- 6.Koay CB, Herdman RC. Nasendoscopyguided removal of fish bones from the base of tongue and the vallecula. J Laryngol Otol 1995;109:534–35 [DOI] [PubMed] [Google Scholar]
- 7.Munoz A, Ballesteros AI, Brandariz Castelo JA. Primary lingual abscess presenting as acute swelling of the tongue obstructing the upper airway: diagnosis with MR. AJNR Am J Neuroradiol 1998;19:496–98 [PMC free article] [PubMed] [Google Scholar]
- 8.Kim SH, Han MH, Park SW, et al. Radiologic-pathologic correlation of unusual lingual masses: Part II: benign and malignant tumors. Korean J Radiol 2001;2:42–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ozturk M, Durak AC, Ozcan N, et al. Abscess of the tongue: findings on MR imaging. AJR Am J Roentgenol 1998;170:797–98 [DOI] [PubMed] [Google Scholar]
- 10.Richard H, Wiggins SCCa 3rd. Oral tongue. In: Harnsberger HR, ed. Diagnostic Imaging. Head and Neck. Salt Lake City: Amirsys;2004. :III-4-34–37
- 11.Phelps ME. Inaugural article: positron emission tomography provides molecular imaging of biological processes. Proc Natl Acad Sci U S A 200097:9226–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coleman RE. PET in lung cancer. J Nucl Med 1999;40:814–20 [PubMed] [Google Scholar]
- 13.Fischbein NJ, AAssar OS, Caputo GR, et al. Clinical utility of positron emission tomography with 18F-fluorodeoxyglucose in detecting residual/recurrent squamous cell carcinoma of the head and neck. AJNR Am J Neuroradiol 1998;19:1189–96 [PMC free article] [PubMed] [Google Scholar]