Abstract
SUMMARY: In this retrospective review, we demonstrate the utility of using a commercially available gated navigator sequence (prospective acquisition correction technique [PACE]) to reduce rhythmic breathing motion on brain MR images. For purposes of this report, we studied 2 sedated patients who had marked head rocking, one due to deep breathing and snoring and the other due to ventilator support. Motion degraded the routine images, which, despite a short acquisition time, were nondiagnostic. After application of PACE, a technique commonly used in abdominal studies, the brain images in both patients were judged to be of acceptable diagnostic quality. The use of PACE to diminish head motion is now routine at our institution when sedated or ventilated patients degrade images with involuntary head rocking.
Prospective acquisition correction technique (PACE) effectively removes breathing motion during abdominal MR imaging studies (including cholangiopancreatography) using a real-time gradient navigator pulse to trigger acquisition at a specified portion of the respiratory cycle.1,2 The real-time pulse is a 2-dimensional section that can produce a continuous representation of tissue location as it moves. Therefore, as the tissue fills more and less of the slab volume, the navigator image produces a continuous wave-like image representing the tissue location over time. It is then possible to identify a spot on the wave (the accept position) that represents a specific location of the tissue at one point during its movement and selectively acquire phase encoding steps only at that location. Thus, PACE may be used to remove extreme patient motion from MR imaging studies when the motion is 1-dimensional and rhythmic. At our institution, we have extended the routine use of PACE to diminish motion-related artifacts in brain MR imaging. To demonstrate the utility of this technique in brain MR imaging, we retrospectively reviewed 2 sedated patients, one snoring and the other on a ventilator, in whom conventional sequences were degraded. The application of PACE, however, yielded images of diagnostic quality.
Technique and Representative Cases
The study was performed under an Institutional Review Board exemption letter that allows for retrospective review of medical records, as long as no patient identifying information is retained or reported. Two patients, one under conscious sedation and the other being mechanically ventilated, underwent brain MR imaging to rule out pathologic processes. Studies were performed on a 1.5T system with a 12-channel head coil. In the first patient, motion was due to high-pressure ventilator support; in the second, head rocking was secondary to deep snoring. Both patients underwent basic T1 and T2 fast spin-echo (FSE), T1 gradient-echo, and navigator PACE T1 and T2 FSE sequences with integrated parallel acquisition technique (IPAT) on an Avanto device (Siemens, Erlangen, Germany).
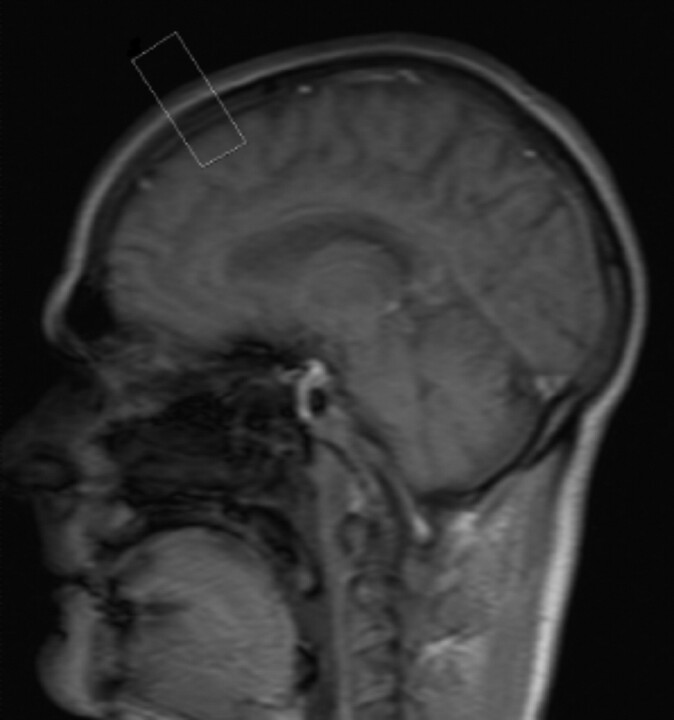
The first patient's sequences are reflected in Table 1. The patient presented with exaggerated breathing motion in response to high-pressure ventilator support. Initial FSE sequences were run with immobilization devices but were deemed nondiagnostic. We then switched to our standard noncooperative protocol that includes gradient-echo sequences, but fell short of producing a diagnostic result. At this point, we repeated the initial T1 and T2 FSE sequences with the addition of the navigator PACE correction pulse. The 2-dimensional PACE navigator pulse was positioned at a 90° angle to the sagittal suture just posterior to the bregma as demonstrated in Fig 1. The navigator's acceptance window was set to 32 ± 2 mm, TR to 150 ms, and the accept position was determined. Scans were run to completion by increasing scan time by 50%–150% depending on patient movement. Acquisition times for T1 and T2 sequences were 3.5 and 5 minutes, respectively, and resulted in images that were independently deemed by 2 neuroradiologists to be of diagnostic quality.
Table 1:
Sequences run on patient 1
| Acquisition Time (min:sec) | TR (ms) | TE (ms) | Echo Train | Resolution | IPAT Acceleration Factor | Comments | |
|---|---|---|---|---|---|---|---|
| T1 SAG FSE | 2:08 | 429 | 10 | 3 | 256 × 205 | 2 | Nondiagnostic due to motion |
| T2 Ax FSE | 2:22 | 5890 | 104 | 21 | 256 × 205 | 2 | Nondiagnostic due to motion |
| T1 GRE, 3 planes | 0:32 | 102 | 4.8 | NA | 256 × 156 | 2 | Nondiagnostic due to motion |
| T1 FSE with navigator, 3 planes | 3:30–4:00 | 429 | 10 | 3 | 256 × 205 | 2 | Diagnostic |
| T2 Ax FSE | 3:00 | 5890 | 104 | 21 | 256 × 205 | 2 | Nondiagnostic |
| T2 Ax FSE navigator | 5:00 | 6635 | 89 | 21 | 256 × 205 | 2 | Diagnostic |
Note:—IPAT indicates integrated parallel acquisition technique; SAG, sagittal; FSE, fast spin-echo; Ax, axial; GRE, gradient-echo; NA, not applicable. Both the TR and the acquisition time will be a variable of the frequency of patient motion. They should be adjusted inversely with concatenations to keep the effective TR short for T1 sequences.
Fig 1.
The navigator box is positioned midsagittal just posterior to the bregma.
The second patient (Table 2) was sedated for claustrophobia and discomfort before undergoing brain MR imaging to rule out cancerous processes. The initial scans demonstrated exaggerated head rocking secondary to snoring and deep breathing. Immobilization devices and noncooperative images failed to produce a diagnostic result, and the navigator sequence was once again used. By gating the patient's head movements, the scan time was increased by a factor of 3, but the resulting images were deemed diagnostic by 2 independent neuroradiologists.
Table 2:
Sequences run on patient 2
| Acquisition Time (min:sec) | TR (ms) | TE (ms) | Echo Train | Resolution | IPAT AccelerationFactor | Comments | |
|---|---|---|---|---|---|---|---|
| T1 SAG and Cor FSE | 2:18 | 475 | 16 | 3 | 256 × 256 | 2 | Nondiagnostic due to motion |
| T2 Ax FSE | 2:22 | 5890 | 104 | 21 | 256 × 205 | 2 | Nondiagnostic due to motion |
| T1 GRE, 3 planes | 0:32 | 102 | 4.8 | NA | 256 × 156 | 2 | Nondiagnostic due to motion |
| T1 FSE with navigator, 3 planes | 4:00–6:00 | 429 | 10 | 3 | 256 × 205 | 2 | Diagnostic |
| T2 Ax FSE | 4:30 | 5890 | 104 | 21 | 256 × 205 | 2 | Diagnostic |
Note:—IPAT indicates integrated parallel acquisition technique; SAG, sagittal; Cor, coronal; FSE, fast spin-echo; Ax, axial; GRE, gradient-echo; NA, not applicable. Both the TR and the acquisition time will be a variable of the frequency of patient motion. They should be adjusted inversely with concatenations to keep the effective TR short for T1 sequences.
Discussion
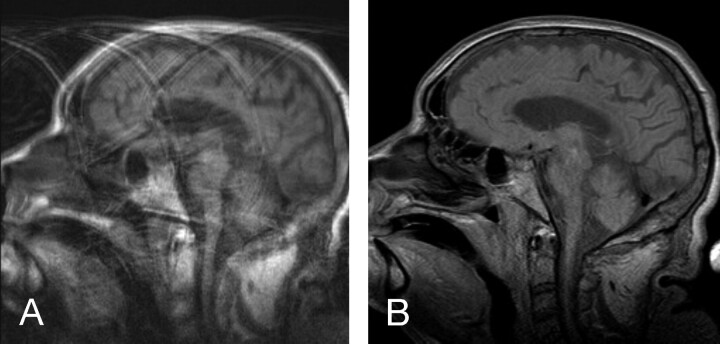
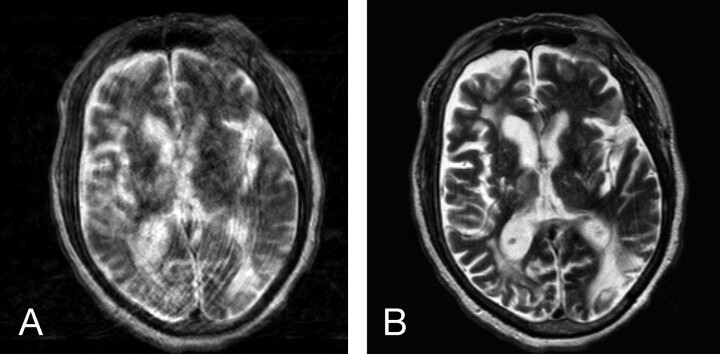
Image degradation is occasionally seen secondary to exaggerated respiratory patterns in ventilated and heavily sedated patients. In both of our patients, 1-dimensional, involuntary head movement occurred in the anterior-to-posterior dimension. Standard FSE sequences failed to produce diagnostic images despite external immobilization, as seen in Figs 2 and 3.
Fig 2.
A, Sagittal T1 FSE (TR, 429 ms; TE, 10 ms; acquisition time, 2 minutes) demonstrates considerable motion artifacts in our patients undergoing mechanical ventilation.
B, Sagittal T1 FSE (TR, 429 ms; TE, 10 ms) with the navigator pulse to gate the same as patient's head rocking motion. Although the acquisition time for this sequence was 3.5 minutes, it is still far superior in quality to the original FSE (A).
Fig 3.
A, Axial T2 FSE (TR, 5890 ms; TE, 104 ms; echo train, 21; acquisition time, 2 minutes) performed without gating and resulting in a nondiagnostic image due to head rocking secondary to high-pressure ventilation.
B, Axial T2 FSE (TR, 6635 ms; TE, 89 ms; echo train, 21; acquisition time, 5 min). This is the same sequence and patient seen in A but with the addition of the navigator pulse.
The free breather PACE navigator pulse is currently used in abdominal MR imaging and MR cholangiopancreatography to remove breathing motion, producing diagnostic images of higher resolution than those achievable with a standard breath-holding sequence.1,2 The navigator's low TR and flip angle produce real-time gating that is superior to other gating methods.1,2 Because of the image clarity associated with the navigator, fine structures, such as infant bile ducts, can be accurately evaluated.3 When the navigator is used in conjunction with IPAT, the acquisition times remain in a reasonable range.4,5 In addition, this technique can be adapted to brain MR imaging when 1-dimensional, rhythmic motion significantly degrades images.
We have previously studied this type of patient using gradient-echo and echo-planar imaging with short acquisition times in an attempt to reduce the motion artifacts. These sequences produce images of lower resolution and lower contrast and are less sensitive to smaller or low contrast abnormalities. The navigated pulse sequence, on the other hand, allows one to obtain standard resolution FSE images by acquiring phase encoding steps at the same location throughout the patient's motion. The result is better resolution and demonstration of anatomy as seen in Figs 2 and 3. The navigator's selectivity results in a significant increase in scan times, as seen in Tables 1 and 2. It should also be noted that this navigator sequence only gates 1-dimensional motion and is not useful for complex motion. It has been our experience that patients benefiting from this approach are those on high-pressure ventilators and obese patients who require sedation for imaging but experience deep breathing and snoring that rocks the head with inspiration and expiration. We now routinely use this technique for brain imaging in patients with simple 1-dimensional motion when immobilization fails to eliminate head motion. This sequence is not a substitute for those used in the imaging of nonsedated claustrophobic patients, because these take longer to acquire. They are, however, a simple way to considerably improve motion-degraded images, as we demonstrated in the patients described herein. In addition, the PACE navigator is easy to use and is commercially available. This technique should be particularly helpful to centers imaging patients undergoing mechanical ventilation and conscious sedation.
References
- 1.Klessen C, Asbach P, Kroencke TJ, et al. Magnetic resonance imaging of the upper abdomen using a free-breathing T2-weighted turbo spin-echo sequence with navigator-triggered prospective acquisition correction. Magn Reson Imaging 2005;21:576–82 [DOI] [PubMed] [Google Scholar]
- 2.Asbach P, Klessen C, Kroencke TJ, et al. Magnetic resonance cholangiopancreatography using a free-breathing T2-weighted turbo spin-echo sequence with navigator-triggered prospective acquisition correction. Magn Reson Imaging 2005;23:939–45 [DOI] [PubMed] [Google Scholar]
- 3.Schaefer JF, Kirshner HJ, Lichy M, et al. Highly resolved free-breathing magnetic resonance cholangiopancreatography in the diagnostic workup of pancreaticobiliary diseases in infants and young children–initial experiences. J Pediatr Surg 2006;41:1645–51 [DOI] [PubMed] [Google Scholar]
- 4.Asbach P, Klessen C, Stemmer A, et al. Respiratory-triggered MRCP applying parallel acquisition techniques. J Magn Reson Imaging 2006;24:1095–100 [DOI] [PubMed] [Google Scholar]
- 5.Zech CJ, Herrmann KA, Huber A, et al. High-resolution MR-imaging of the liver with T2-weighted sequences using integrated parallel imaging: comparison of prospective motion correction and respiratory triggering. J Magn Reson Imaging 2004;20:443–50 [DOI] [PubMed] [Google Scholar]