Abstract
SUMMARY: Intraosseous lipomas are very rare slow-growing benign tumors that may appear as congenital lesions or may be acquired (metaplasia from a pre-existing lipoma). Only a handful of head and neck cases have been reported in the literature. We present the first reported case of a solitary osteolipoma involving the sinonasal tract in a 66-year-old man with sinonasal symptoms. CT showed a lesion involving the left frontal sinus, extending into the ethmoid sinus with insinuation along the left middle turbinate. It appeared to be an atypical mass with areas of high attenuation (calcification) within.
Osteolipoma is a rare histologic variant of lipoma, accounting for less than 1% of bone tumors.1 Lipomas rarely undergo osseous metaplasia and become osteolipomas. In the head and neck region, osteolipomas have been reported in the intraoral region,2 the left gingivolabial sulcus,3 the sublingual space,4 the submandibular space,5 the retropharyngeal space,6 the parapharyngeal space, and the right lateral skull base.2 The treatment consists of surgical resection, and the postoperative prognosis is excellent without recurrence after total resection.
Case Report
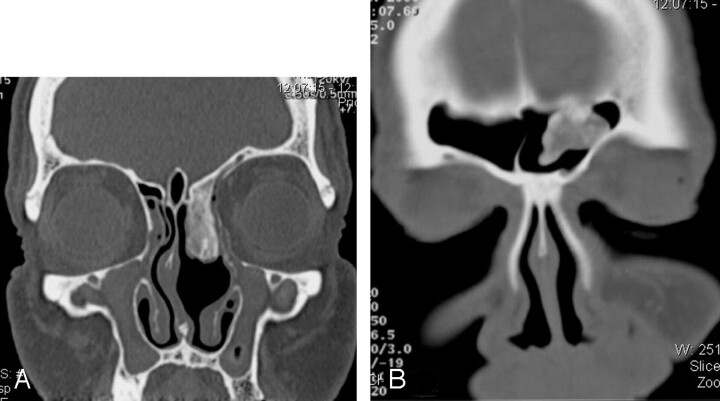
A 66-year-old man presented to the otolaryngology department of our institution with nasal congestion symptoms. On endoscopic examination, the right nasal cavity was unremarkable and the left demonstrated a large polypoidlike mass filling most of the anterior ethmoid sinus with obstruction of the middle meatus and adjacent to the middle turbinate. The oral cavity was clear. A noncontrast CT scan of the paranasal sinuses revealed a well-defined heterogeneous lesion of increased attenuation in the left nasal cavity, inseparable from the superior attachment of the middle turbinate and sparing the very anterior portion of the left middle turbinate. The lesion was obstructing the left middle meatus extending into the ethmoid bulla area and posteriorly progressing to the left sphenoethmoid recess. Anteriorly, the lesion was obscuring the frontal cells and Agger Nasi cells, extending through the frontal recess into the medial left frontal sinus, and adhering to the roof of the left frontal sinus without obstruction. The lesion was also adhering to the cribriform plate and to the lamina papyracea. There was no inflammatory mucosa throughout the paranasal sinuses (Fig 1). This appearance raised the possibility of an inverted papilloma.
Fig 1.
A, Coronal CT scan of the paranasal sinuses (bone window setting) shows the osteolipoma passing through the left ethmoidal sinus into the left nasal cavity. B and C, Coronal CT scan of the paranasal sinuses (bone window setting) (B) and sagittal reformatted image (C) show the osteolipoma based on the roof of the left frontal sinus.
Elective surgery was scheduled. Left endoscopic anterior ethmoidectomy and partial excision/debulking of the large left middle meatus bony mass were performed with identification of the middle and superior turbinates remnants medial to the mass. The appearance and consistency were of a bony lesion with no soft-tissue component, mostly covered by normal mucosa, which was piecewise debulked to avoid fracturing the cribriform plate. The superior portion of the mass was left in place because it extended up into the frontonasal duct and into the frontal sinus as shown by CT (Fig 1).
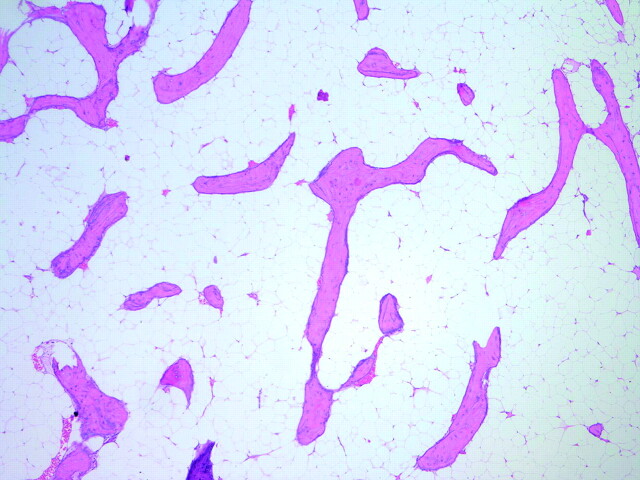
Histopathologic study of the excised specimen revealed a bone-lined respiratory mucosa with mild chronic inflammation. There was extensive fatty infiltration between trabeculae of mature lamellar bone, consistent with an intraosseous lipoma (Fig 2).
Fig 2.
Low-power photomicrograph (hematoxylin-eosin, original magnification ×40) shows mature adipose tissue surrounding spicules of lamellar bone.
Because of the benign nature of the lesion, after partial surgical excision, only conservative management was required, and the patient was followed up once a year. Five years after the endoscopic debulking of the mass, a suspected regrowth (rather than recurrence because the tumor was not fully excised from the beginning) was noted during a follow-up visit, and the patient presented with increasing nasal obstruction. A noncontrast CT scan revealed a postoperative status that consisted of a partial left middle turbinectomy and a left uncinectomy, with excision of the inferior aspect of the previously described mass. Prominent inflammatory mucosa was bilaterally present within the maxillary sinus (more on the right side), involving the Agger Nasi cells and ethmoidal bulla and extending into the posterior ethmoidal cells and left anterior sphenoid sinus. A heterogeneous oval increased attenuation lesion having a ground-glass-like appearance was occupying the region of the left middle meatus and extending posteriorly to the sphenoethmoid recess. On the sagittal reconstructed image, it was evident that the lesion anterior to the basal lamella was adherent to the roof of the anterior ethmoid sinus and extending forward through the frontal recess into the frontal sinus. The previously noted prominent central bony component was now replaced with a more ground-glass-like appearance (Fig 3).
Fig 3.
A and B, Follow-up coronal CT scans (bone window setting) show regrowth of the osteolipoma.
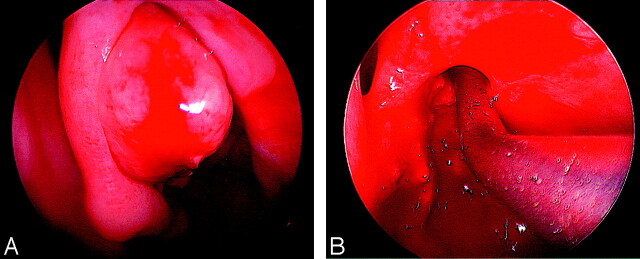
Endoscopic debulking of the suspected regrowth of the mass was performed, and the histopathologic study of the specimen again confirmed the tumor to be an osteolipoma (Fig 4).
Fig 4.
A and B, Preoperative (A) and postoperative (B) views of the left nasal cavity.
Discussion
Lipomas are the most common benign soft-tissue tumors of adults and also the most common tumor of the head and neck region, corresponding to approximately 13% of lipomas,1 with patients ranging between 40–60 years of age and a slight male predominance.1 They rarely occur in the sinonasal tract.
Lipomas are composed of mature fat cells with no cellular atypia and are by far the most common mesenchymal neoplasms.2 Despite the close histologic similarity to normal adipose tissue, most lipomas have chromosomal aberrations such as translocations involving 12q13–15, interstitial deletions of 13q, and rearrangements involving 8q11–13.4.1 Osteolipomas are a histologic variant of lipomas that have undergone osseous metaplasia. Osteolipomas are primarily encountered in chronic large-sized lipomas. Some pathologists believe that osteolipomas are variants of lipomas and hence consider them to be benign mesenchymomas.2 Congenital osteolipomas are regarded as hamartomas of osseous and lipomatous differentiation.7
An osteolipoma contains a variable mixture of adipose tissue, lamellar bone, woven bone, and osteoblasts. The terms ossifying lipoma and osseous lipoma have been used interchangeably with osteolipomas. Lipomas can also undergo secondary changes as a result of impaired blood supply and traumatic injury. Prolonged ischemia may lead to infarction, hemorrhage, and calcification.2 Such lipomas that undergo calcification may mimic osteolipomas radiologically, but histologically they may be differentiated from osteolipoma because they also have other features of prolonged ischemia such as infarction, hemorrhage, and cystic degeneration.2 Lipomas and osteolipomas are benign slow-growing tumors and are usually asymptomatic in the head and neck region, only producing symptoms by compression or obstruction when they enlarge.2
Osteolipomas are benign and do not recur, though resection can be difficult because of their tendency to adhere to the neighboring tissues.8,9 CT and reformatted 2D reconstructions are extremely useful for diagnosis and also to assess the exact site and extent of the growth. Characteristic features, such as areas of hypoattenuation (fat attenuation) with surrounding areas of hyperattenuation, (calcification) suggest the diagnosis.
The differential diagnosis would be of an inverted papilloma because it has a similar extension, age group, and sex predominance. An inverted papilloma may be associated with calcification; however, the lack of adjacent inflammatory mucosa is unusual for this entity and, given the lack of erosive changes, is unlikely to represent malignancy. The appearance would be most closely related to that of a fibro-osseous pathologic entity; however, this usually calcifies from the periphery inwards. In contrast, in this patient, most of the calcification was centrally located. Another differential diagnosis that needs to be considered is fibrous dysplasia. This lesion is associated with a ground-glass-like appearance closest to that of the lesion in question.
Various surgical approaches can be used to resect a mass with the extension and relations of the case presented here; however, endoscopic surgery was performed in this patient to avoid exposing him to a major open surgery and because there was no frontal sinus obstruction.
References
- 1.Castilho RM, Squarize CH, Nunes FD, et al. Osteolipoma: a rare lesion in the oral cavity. Br J Oral Maxillofac Surg 2004;42:363–64 [DOI] [PubMed] [Google Scholar]
- 2.Hazarika P, Pujary K, Kundaje HG, et al. Osteolipoma of the skull base. J Laryngol Otol 2001;115:136–39 [DOI] [PubMed] [Google Scholar]
- 3.Barnes L. Tumours and tumour-like lesions of the head and neck. In: Rice DH, Batsakis JG, eds. Surgical Pathology of the Head and Neck. New York: Marcel Dekker Inc;1985. :725–844
- 4.Kennedy KS, Wotowic PJ, St John JN. Parapharyngeal fibrolipoma. Head Neck 1990;12:84–87 [DOI] [PubMed] [Google Scholar]
- 5.Abdullah BJJ, Liam CK, Kaur H, et al. Parapharyngeal space lipoma causing sleep apnoea. Br J Radiol 1997;70:1063–65 [DOI] [PubMed] [Google Scholar]
- 6.Allard RH, Blok P, Van der Kwast WA, et al. Oral lipomas with osseous and chondrous metaplasia: report of two cases. J Oral Pathol 1982;11:18–25 [DOI] [PubMed] [Google Scholar]
- 7.Piattelli A, Fioroni M, Iezzi G, et al. Osteolipoma of the tongue. Oral Oncol 2001;37:468–70 [DOI] [PubMed] [Google Scholar]
- 8.Shuangshoti S, Suwanwela C, Suwanwela N. Congenital osteolipoma of the skull. Arch Otolaryngol 1982;108:454–57 [DOI] [PubMed] [Google Scholar]
- 9.Turkoz HK, Varnali Y, Comunoglu C. A case of osteolipoma of head and neck area. Kulak Burun Bogaz Ihtis Derg 2004;13:84–86 [PubMed] [Google Scholar]