Abstract
SUMMARY: Arachnoid granulations are rarely seen on high-resolution CT (HRCT) at the posterior temporal bone wall, where they appear as erosions, without bone spicules and often with a lobulated surface. Differential diagnosis includes endolymphatic sac tumor, paraganglioma, chordoma, and chondromatous and metastatic tumors. MR imaging can confirm the diagnosis because arachnoid granulations behave like CSF without gadolinium enhancement. This report aims to illustrate the appearance and differentiation of temporal bone arachnoid granulations on HRCT and MR imaging.
Arachnoid granulations are primarily located in the parasagittal region along the superior sagittal sinus. Occasionally, they are seen at the posterior temporal bone wall. We report the high-resolution CT (HRCT) and MR imaging appearance of such arachnoid granulations and provide a differential diagnosis.
Case Reports
Case 1
A 57-year-old female patient with an osseouslike structure in the left external auditory canal was referred for temporal bone HRCT. Extensive bilateral tympanosclerosis was diagnosed, with a tympanic membrane perforation (Fig 1B). The inner ear was normal on both sides. An erosion of the posterior temporal bone wall was bilaterally present, with sharp but slightly irregular margins (Fig 1A, -B). No mass was identified, nor were calcifications or bone spicules present. The finding was located anteromedial to the sigmoid sinus and posterolateral and slightly superior to the normal-sized endolymphatic duct (Fig 1B). MR imaging showed bilaterally a T2 hyperintense (Fig 1C) and T1 hypointense lesion, with hypointense signal intensity on fluid-attenuated inversion recovery (FLAIR) images and without gadolinium enhancement. In view of their CT and MR imaging appearance and location, the erosion was identified as an arachnoid granulation.
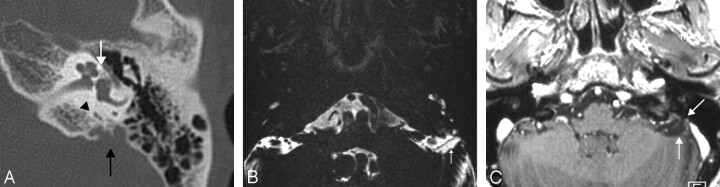
Fig 1.
A, The axial HRCT image of the right temporal bone in case 1 shows an erosion in the posterior temporal bone wall (arrow). The erosion does not contain calcifications or bone spicules and was identified as an arachnoid granulation.
B, On the axial HRCT image obtained 3 mm below A, the normal endolymphatic duct (black arrowhead) is identified anterior to the arachnoid granulation (black arrow). Tympanosclerosis is present (white arrowhead).
C, The axial 0.7-mm-thick T2-weighted image of the posterior fossa confirms the right (arrowhead) and left (arrow) arachnoid granulation. On the right side, the internal fibrous structure is seen as hypointense lines within the granulation.
Case 2
A 62-year-old woman with conductive hearing loss was referred for temporal bone HRCT. Fenestral otospongiosis was diagnosed, but as an incidental finding, a posterior temporal bone wall erosion was identified on the expected location of the endolymphatic sac (Fig 2A). The lesion was less prominent and more lobulated than that in the first patient. No bone spicules or calcifications were present. A normal-sized endolymphatic duct was also depicted. MR imaging showed a T2 hyperintense and T1 hypointense lesion, without gadolinium enhancement, located adjacent to the temporal bone and sigmoid sinus (Fig 2B, -C). No mass lesion was found. On the basis of the CT and MR imaging findings, the diagnosis of arachnoid granulation was proposed.
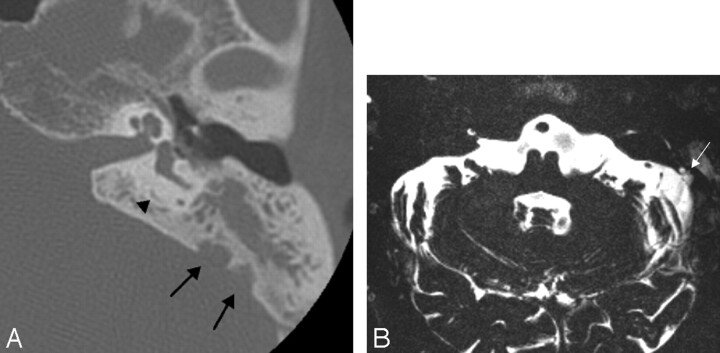
Fig 2.
A, On the axial HRCT image of the left temporal bone in case 2, a defect is seen at the posterior surface of the left temporal bone (black arrow), with a normal endolymphatic duct (arrowhead). Note the presence of a hypoattenuated otospongiotic focus in the fissula antefenestram region (white arrow).
B, The axial 0.4-mm-thick T2-weighted image again demonstrates the arachnoid granulation (arrow). It has the same signal intensity as CSF.
C, The axial 0.8-mm-thick T1-weighted image after intravenous administration of gadolinium shows a hypointense nonenhancing arachnoid granulation (arrows).
Case 3
An 80-year-old woman with chronic otomastoiditis and suspected associated cholesteatoma was referred for temporal bone HRCT, which showed a partially evacuated cholesteatoma without fistulization. As a coincidental finding, a small lobulated and sharply delineated posterior temporal bone wall erosion was noted (Fig 3A). The normal-sized endolymphatic duct was demonstrated. MR imaging showed a T2 hyperintense (Fig 3B) and T1 hypointense lesion. No enhancing mass was found after gadolinium administration. Because of the appearance and location of the lesion, again arachnoid granulation was the proposed diagnosis.
Fig 3.
A, The axial HRCT image of the opacified temporal bone in case 3 shows the presence of an arachnoid granulation (arrows), easily differentiated from an endolymphatic sac tumor by identifying the normal and unenlarged endolymphatic duct (arrowhead).
B, The axial 0.4-mm-thick T2-weighted image confirms the arachnoid granulation (arrow), with CSF signal intensity.
Discussion
An arachnoid granulation is a penetration of the arachnoid membrane in the dura directly beneath the vascular endothelium of the great dural sinuses. Its function is drainage of CSF to the lower pressure venous system. It is primarily located beneath the superior sagittal sinus and the venous lacunae, which are located in the parasagittal region, and it communicates with the superior sagittal sinus.1 In decreasing frequency, it is thought to be present in the transverse sinus, cavernous sinus, superior petrosal sinus, and straight sinus.2
For unknown reasons, arachnoid granulations can be seen at the floor of the anterior and middle cranial fossa and, less frequently, at the posterior temporal bone wall. At these aberrant locations, they contain CSF but do not communicate with the venous sinuses. Instead, the pressure of the CSF will cause bone erosion.3 As they grow, these arachnoid granulations can cause defects in the posterior temporal bone wall or the tegmen tympani. Thus CSF leakage and otorrhea can occur.4 Arachnoid granulations in this specific location may also be, in the inverse direction, the entry point for bacterial invasion to the meninges.5 In this context, it is important to report their presence to the otologist because they are known to enlarge with age.
On HRCT examinations of the temporal bone, arachnoid granulations present as erosions in the posterior temporal bone wall, without mass, often with a lobulated surface, and with an attenuation varying from that of CSF to that of brain tissue.2 The lesion can be bilaterally present as was the case in one of our patients. Calcifications in arachnoid granulations were reported by 1 author,6 but they were not seen in a similar but larger study.2 In our patients, no calcifications were identified within the erosions.
On HRCT, differentiation should be primarily made from papillary endolymphatic sac tumor, which is a rare tumor thought to originate in the endolymphatic sac. The characteristic CT appearance7,8 of papillary endolymphatic sac tumor is an aggressive soft-tissue mass eroding the posterior temporal bone surface at the expected location of the endolymphatic sac and containing intratumoral bone spicules and a peripheral rim of calcifications. In our patients, the differential diagnosis was directed toward arachnoid granulations and not to endolymphatic sac tumor by identifying the normal endolymphatic duct9 and noting the absence of bone spicules and a peripheral rim of calcifications. The fact that the finding was bilateral in 1 patient was not helpful because endolymphatic sac tumors can be bilateral in a number of cases. In patients with von Hippel-Lindau disease, bilateral endolymphatic sac tumors are not even a rare entity, with a frequency of 28% as reported by Bambakidis et al,10 whereas they are only seen in 1% of the patients without von Hippel-Lindau disease. Differential diagnosis also includes jugular paraganglioma, chordoma, and chondromatous and metastatic tumors. These lesions have locally a more aggressive appearance than arachnoid granulations. Moreover, they are located in the temporal bone more anteriorly at the petro-occipital synchondrosis (chondromatous tumors) and petrous apex (chordoma) or more posteriorly at the jugular foramen (paraganglioma).11
The diagnosis of arachnoid granulations can be confirmed in case of doubt with MR imaging. The signal-intensity characteristics of arachnoid granulations are typically these of CSF on T1- and T2-weighted images. On high-resolution T2-weighted images, linear hypointense components of the internal fibrous structure of the arachnoid granulation can be seen. On FLAIR, arachnoid granulations are mostly hypointense but occasionally slightly hyperintense compared with CSF. No gadolinium enhancement is noted.1,12 Endolymphatic sac tumors, on the contrary, are characterized by heterogeneous signal intensities on T1- and T2-weighted images with typically focal high T1 signal intensities due to hemorrhagic and proteinaceous components.7 Moreover, they enhance heterogeneously after gadolinium administration. Other lesions such as chordoma, paraganglioma, and chondromata and metastatic disease have varying signal-intensity characteristics but also enhance after gadolinium administration11 and can thus not be confused with arachnoid granulations.
Conclusion
The radiologist should be aware of the existence of arachnoid granulations of the temporal bone wall because they can be incidentally noted. On HRCT, differentiation from endolymphatic sac tumors is straightforward by identifying the normal endolymphatic duct and the absence of peripheral calcifications and bone spicules. Other tumoral lesions have a more aggressive appearance and typical location. On MR imaging, arachnoid granulations behave like CSF. The presence of arachnoid granulations should be reported to the otologist because they can enlarge with age and cause CSF leakage, otorrhea, or meningitis.
References
- 1.Okamoto K, Ito J, Tokiguchi S, et al. Arachnoid granulations of the posterior fossa: CT and MR findings. Clin Imaging 1997;21:1–5 [DOI] [PubMed] [Google Scholar]
- 2.Leach JL, Jones BV, Tomsick TA, et al. Normal appearance of arachnoid granulations on contrast-enhanced CT and MR of the brain: differentiation from dural sinus disease. AJNR Am J Neuroradiol 1996;17:1523–32 [PMC free article] [PubMed] [Google Scholar]
- 3.Gacek RR. Arachnoid granulation cerebrospinal fluid otorrhea. Ann Otol Rhinol Laryngol 1990;99:854–62 [DOI] [PubMed] [Google Scholar]
- 4.Gacek RR, Gacek MR, Tart R. Adult spontaneous cerebrospinal fluid otorrhea: diagnosis and management. Am J Otol 1999;20:770–76 [PubMed] [Google Scholar]
- 5.Perry BP, Rubinstein JT. Meningitis due to acute otitis media and arachnoid granulations. Ann Otol Rhinol Laryngol 2000;109:877–79 [DOI] [PubMed] [Google Scholar]
- 6.Roche J, Warner D. Arachnoid granulations in the transverse and sigmoid sinuses: CT, MR, and MR angiographic appearance of a normal anatomic variation. AJNR Am J Neuroradiol 1996;17:677–83 [PMC free article] [PubMed] [Google Scholar]
- 7.Mukherji SK, Albernaz VS, Lo WW, et al. Papillary endolymphatic sac tumors: CT, MR imaging, and angiographic findings in 20 patients. Radiology 1997;202:801–08 [DOI] [PubMed] [Google Scholar]
- 8.Patel NP, Wiggins RH 3rd, Shelton C. The radiologic diagnosis of endolymphatic sac tumors. Laryngoscope 2006;116:40–46 [DOI] [PubMed] [Google Scholar]
- 9.Valvassori GE, Clemis JD. The large vestibular aqueduct syndrome. Laryngoscope 1978;88:723–28 [DOI] [PubMed] [Google Scholar]
- 10.Bambakidis NC, Megerian CA, Ratcheson RA. Differential grading of endolymphatic sac tumor extension by virtue of von Hippel-Lindau disease status. Otol Neurotol 2004;25:773–81 [DOI] [PubMed] [Google Scholar]
- 11.Bonneville F, Sarrazin JL, Marsot-Dupuch K, et al. Unusual lesions of the cerebellopontine angle: a segmental approach. Radiographics 2001;21:419–38 [DOI] [PubMed] [Google Scholar]
- 12.Ikushima I, Korogi Y, Makita O, et al. MRI of arachnoid granulations within the dural sinuses using a FLAIR pulse sequence. Br J Radiol 1999;72:1046–51 [DOI] [PubMed] [Google Scholar]