Abstract
BACKGROUND AND PURPOSE: We report 6 cases of retrograde flow through the anterior spinal artery (ASA) from cervical vertebral artery (VA) to intracranial distal VA because the perfusion from bilateral vertebral arteries was tenuous. Its hemodynamic and clinical implications are discussed.
METHODS: In association with bilateral steno-occlusive disease of vertebral arteries, 6 cases of retrograde flow through ASA were reviewed in terms of clinical and angiographic characteristics. All 6 patients presented with stroke in the posterior fossa and underwent conventional angiography as part of diagnostic evaluation and/or therapeutic intervention.
RESULTS: On the angiography, 2 patients showed bilateral VA occlusion, and the other 4 patients showed VA occlusion on 1 side and severe stenosis in the other VA. Distal perfusion by ASA was prominent in 2, and not prominent in 4. Reversal or disappearance of the retrograde flow through ASA was observed after successful recanalization of the occluded VA in 4 patients. In 1 patient, increased perfusion through ASA was observed because the stenosed VA was completely occluded.
CONCLUSION: When the vertebral arteries were occluded bilaterally or when a single VA was occluded and the other carried a severe stenosis and, as a result, the basilar arterial blood supply was tenuous, retrograde flow through ASA could be observed. This is a potentially important source of collateral supply to the posterior fossa neural contents. The degree and extent of perfusion via this collateral channel varied depending on presence of other collateral routes and patency of the vertebrobasilar junction.
Occlusive disease of the intracranial vertebral artery (VA) is a major vascular lesion in patients with posterior circulation stroke, along with those originating in the VA and basilar artery.1 Intracranial VA disease accounts for 21% of patients with posterior circulation stroke and is frequently bilateral.2 Up to 10% of patients with posterior circulation disease have bilateral intracranial VA disease,3 which may result in mortality if combined with basilar artery disease. In this article, we report 6 cases of retrograde flow through the anterior spinal artery (ASA) from cervical VA to intracranial distal VA because perfusion from the bilateral VAs was tenuous. We discuss its hemodynamic and clinical implications.
Materials and Methods
Six cases with patients showing retrograde flow through ASA were collected in association with bilateral steno-occlusive disease of vertebral arteries. Clinical and angiographic characteristics were reviewed. All 6 patients presented with strokes in the posterior circulation territory and underwent conventional angiography as part of diagnostic evaluation and/or therapeutic intervention. Angiographic data analyzed included VA lesions (occlusion or stenosis), location and/or side of origin of ASA, its connecting side(s) on distal VA, arteries irrigated by ASA, patency of vertebrobasilar junction, collateral supply from the anterior circulation.
In patients undergoing therapeutic interventions, we compared the preprocedural and postprocedural angiography. In 4 patients, interventional procedures (emergent intra-arterial thrombolysis in 3 patients and elective stent-assisted angioplasty in another) were attempted and successful recanalization and/or luminal gain were achieved in all of them. Among them, subacute stent thrombosis occurred in 1 patient. In 1 patient, progression to complete occlusion of the stenosed VA was observed.
All the patients underwent MR imaging at time of presentation. Acute ischemic lesions were divided into large territorial and small focal (nonterritorial) and by anatomic location. Outcome at discharge was measured with modified Rankin scale (mRS).
Results
In this series, there were 3 men and 3 women, aged from 40 to 81 years (median age, 64 years). The clinical and angiographic characteristics of the cases are summarized in Tables 1 and 2, respectively. Clinical presentation included dizziness and gait ataxia (n = 3), unilateral weakness of limbs and face (n = 2), swallowing difficulty (n = 2), and quadriparesis (n = 1). All the patients showed acute ischemic lesions in the cerebellar hemisphere. There were small multifocal lesions in 4 patients and large territorial lesions in 2 patients. Other acute ischemic lesions were distributed at the pons (n = 3), midbrain (n = 2), and occipital lobe (n = 1).
Table 1:
Clinical characteristics and MR imaging features of the patients
| No/Gender/Age | Presentation | Acute Ischemic Lesions on MRI | Extent of Parenchymal Lesions | Interventional Procedure | mRS at Discharge |
|---|---|---|---|---|---|
| 1/F/62 | Dizziness, gait disturbance | L pons, both CH | Focal | IA thrombolysis w/ stent-assisted angioplasty | 3 |
| 2/M/64 | R hemiparesis, R facial palsy | R midbrain, L CH, R occipital lobe | Focal | IA thrombolysis w/ stent-assisted angioplasty | 2 |
| 3/F/75 | L hemiplegia, L facial palsy, dysphagia | R pons, both CH | Focal | NA | 4 |
| 4/F/63 | Dizziness, gait ataxia | R CH | Focal | Stent-assisted angioplasty | 1 |
| 5/M/40 | Dizziness, gait ataxia | L CH | Territorial | NA | 2 |
| 6/M/81 | Quadriparesis, aphagia | L midbrain, L pons, L CH | Territorial | IA thrombolysis w/ stent-assisted angioplasty | 4 |
Note:—MRI indicates MR imaging; mRS, modified Rankin scale; CH, cerebellar hemisphere; IA, intra-arterial; R, right; L, left; NA, not attempted.
Table 2:
Angiographic characteristics of the patients
| No | Right VA | Left VA | Course of ASA | Perfusion via ASA | Collateral Supply from PcomA | VBJ Patency | Comment |
|---|---|---|---|---|---|---|---|
| 1 | Occlusion | Occlusion | L VA → R VA | R AICA & PICA | Both SCAs filling from L PcomA | Yes | Reversed flow of ASA disappeared after recanalization; reappearance of ASA |
| 2 | Occlusion | Severe stenosis | R VA → L VA | Part of BA | Nil | Yes | BA filling from L VA; reversal of ASA flow direction after recanalization |
| 3 | Occlusion | Occlusion | L VA → R VA | Not profuse | BA trunk filling from L PcomA | No | |
| 4 | Severe stenosis | Occlusion | R & L VA → L VA | Not profuse | Both SCAs filling from R PcomA | Yes | Reversal of ASA flow direction after recanalization |
| 5 | Occlusion | Occlusion | R VA → both VAs | R AICA & PICA; L AICA | Nil | Yes | Increased perfusion through ASA after occlusion of L VA |
| 6 | Occlusion | Severe stenosis | R VA → R VA | Not profuse | Nil | Yes | Reversal of ASA flow direction after recanalization |
Note:—VA, vertebral artery; ASA, anterior spinal artery; PcomA, posterior communicating artery; VBJ, vertebrobasilar junction; L, left; R, right; AICA, anterior inferior cerebellar artery; PICA, posterior inferior cerebellar artery; SCA, superior cerebellar artery; BA, basilar artery.
On the angiographic evaluations, 2 patients showed bilateral VA occlusion, and the other 4 patients showed VA occlusion on one side and severe stenosis in the other VA. Overall, there were 5 occlusions and 1 stenosis on the right VAs, and 3 occlusions and 3 stenoses on the left. Locations of VA steno-occlusive lesions were proximal to the posterior inferior cerebellar artery (PICA) in 8 sides and distal to it in 4 sides. Origins of the ASA were at the right VA in 4 cases, and at the left VA in 3 cases (thus, bilateral origins in one patient). Sites of distal connection were at the right VA in 3 patients, at the left VA in 2 patients, and at both the VAs in 1 patient. Distal perfusion by ASA was prominent (that is, filling multiple cerebellar arteries) in 2 patients (Figs 1 and 4), and not prominent in 4 patients (Figs 2 and 3).
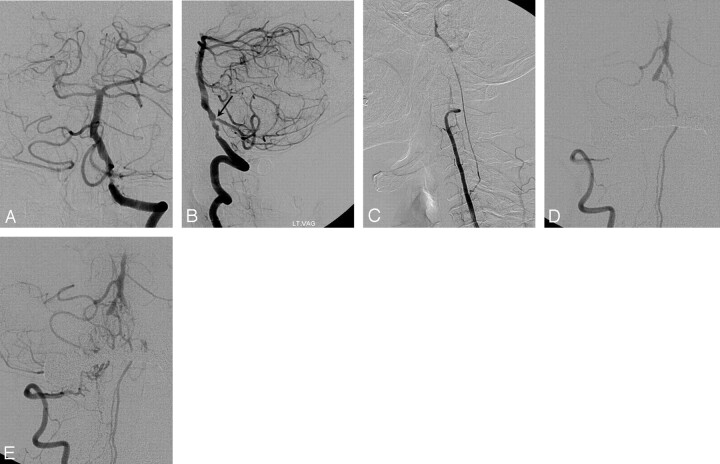
Fig 1.
Left vertebral angiograms in anteroposterior (A and C) and lateral (B and D) views show the occluded vertebral artery (VA) and retrograde upward flow through the anterior spinal artery (ASA) at early arterial (A and B) and later (C and D) phases in patient 1. The ASA is connected to the right distal VA and supplies the right anterior and posterior inferior cerebellar arteries.
Fig 4.
Irregular stenosis of the left vertebral artery (VA) is shown on the left vertebral angiograms in anteroposterior (AP) (A) and lateral (B) views in patient 5. Severe stenosis of the left posterior inferior cerebral artery (PICA) orifice is also noted (arrow). Right vertebral angiogram in the lateral view shows retrograde flow through the anterior spinal artery (ASA) (C). There is minimal perfusion to right distal VA. Follow-up angiography after 9 months shows increased perfusion through the ASA at early arterial (D) and later (E) phases. Both distal VAs are connected to the ASA, and perfusion to the common trunk of the right anterior interior cerebellar artery (AICA) and PICA and left AICA is maintained by this collateral route. The left VA was completely occluded (not shown).
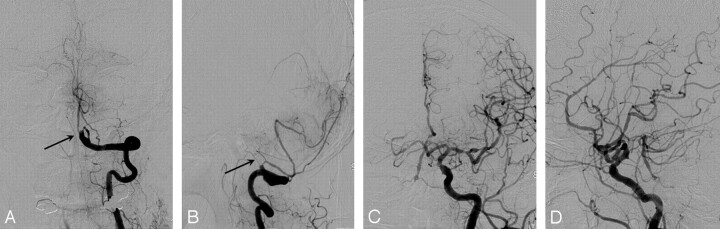
Fig 2.
Left vertebral angiograms in anteroposterior (AP) (A) and lateral (B) views show the anterior spinal artery (ASA; arrow) filled in retrograde direction as well as the occluded VA in patient 3, though it is not clear that the ASA is providing any significant collateral support to the posterior circulation. Left common carotid angiograms in AP (C) and lateral (D) views reveal contrast filling of the basilar artery from the posterior communicating artery. Diffuse severe arteriosclerotic narrowing and dilation of cerebral arteries is also noted.
Fig 3.
Right vertebral angiograms in lateral views (A and B) demonstrate the occluded vertebral artery (VA) and retrograde flow through the anterior spinal artery (ASA) and perfusion to pontine perforators after filling of the basilar artery at later phase (B, arrow) in patient 2. Angiograms in right anterior oblique view at early arterial (C) and later (D) phases reveals reversal (normalization) of blood flow through the ASA after successful stent-assisted recanalization of the right VA.
In terms of collateral supply from the anterior circulation via the posterior communicating artery (PcomA), there was no supply to the posterior circulation in 3 patients. The supply was extensive enough to fill the basilar trunk in 1 patient (case 3; Fig 2), and both superior cerebellar arteries were perfused by a PcomA in the other 2 patients.
The vertebrobasilar junction was patent in all patients except 1 (case 3; Fig 2). In the latter case, the perfusion by ASA was not profuse, combined with extensive basilar artery filling from the PcomA.
In 4 patients, interventional procedures for revascularization were performed with successful recanalization of occluded or stenosed vertebral arteries. We observed that retrograde flow through ASA was reversed or disappeared after successful recanalization of the occluded VA (Fig 3). Increased perfusion through ASA was observed in 1 patient because the stenosed VA was completely occluded (Fig 4). In 1 patient (case 1), collateral supply from ASA reappeared with occurrence of subacute stent thrombosis.
Outcome at discharge was favorable (mRS 1 or 2) in 3 patients and unfavorable (mRS 3 or 4) in the other 3 patients (cases 1, 3, and 6), as shown in Table 1. It is noteworthy that there was no mortality. The initial functional outcome of patient 1 was excellent after successful recanalization. However, stent thrombosis, possibly related to discontinuation of antiplatelet medications, contributed to the worsened outcome (mRS 3). Patient 3 refused interventional procedure, resulting in recurrent cerebellar and pontine infarctions. In patient 6, advanced age (81 years) seemed to be the cause for the unfavorable outcome despite successful recanalization.
Discussion
Reports regarding ASA as a collateral channel are rarely found.4–6 ASA originates from the VA distal to the PICA when the PICA originates from the VA,7 as 1 of the 2 major medial branches of the intracranial VA, along with the branches to the foramen caecum.8 The point of origin of ASA is 5–17 mm proximal to the vertebrobasilar junction. Sometimes the anterior spinal communicating artery is found to connect both ASAs at the anterior surface of the medulla oblongata. There are always 1 or 2 ASAs, arising from the intracranial vertebral arteries.9 Three types of origin are documented: bilateral origin (77%), unilateral origin (10%), and origin in an intervertebral transverse anastomosis (13%).
In our series of 6 cases, upward retrograde flow through the ASA was observed in patients with unilateral VA occlusion and severe stenosis of the contralateral VA as well as in cases of bilateral VA occlusion. They presented with neurologic symptoms and signs referable to brain stem and/or cerebellar infarction and showed acute ischemic lesions at the corresponding locations. It is peculiar that no large territorial infarction with mass effect or fatal brain stem infarction was observed, and there was no mortality in our series.
In our patients, ASA was found to be an important potential source of perfusion to the brain stem and cerebellum if blood supply from the VAs was tenuous or absent, and the degree and extent of contribution from the ASA to the intracranial perfusion depended on presence or absence of another source of collateral supply (such as PcomA), and on the patency of the adjacent vertebrobasilar junction as a route for the further flow. In patient 3, for instance, an upward retrograde flow through the ASA was observed, but the more distal perfusion thereafter amounted to very little, because there was profuse blood supply from the left PcomA, and the vertebrobasilar junction was not patent.
After successful recanalization of the occluded VA, disappearance of reversed flow through the ASA or normalization of ASA flow direction (to downward) was observed in 4 patients. On the other hand, we observed increased flow through the ASA in reverse direction because the stenosed VA was occluded in patient 5 and reappearance of reversed ASA flow after occlusion of the stented VA in patient 1. In no case was a symptom or sign referable to the cervical spinal cord ischemia or hyperperfusion found during the hospital course or at the outpatient checkup.
Proximal VA occlusion at the neck is usually compensated by anastomotic flow to the upper part of the artery via the thyrocervical, deep cervical, occipital, and ascending pharyngeal arteries (via its continuation to the C3 anastomotic branch) or reflux from the circle of Willis. Moreover, occlusion or tight stenosis of 1 VA tends to be asymptomatic if there is sufficient flow through the other VA. On the other hand, patients with bilateral distal VA disease are not supposed to have such compensatory collateral channels as described above; as a result, they frequently have transient ischemic attacks and stroke, with symptoms of faintness, blurred vision, dizziness, and bilateral weakness.10 In this desperate situation, the anterior spinal artery can have a significant role in supplying blood to the brain stem and cerebellum when a certain conditions are met.
Conclusion
When VAs were occluded bilaterally or when 1 VA was occluded and the other carried a severe stenosis and, as a result, the basilar arterial blood supply was tenuous, retrograde flow through the ASA was observed and was an important source of collateral supply to the posterior circulation. The degree and extent of perfusion via this collateral channel varied depending on presence of other collateral routes and patency of the vertebrobasilar junction.
References
- 1.Caplan LR, Wityk RJ, Glass TA, et al. New England Medical Center Posterior Circulation registry. Ann Neurol 2004;56:389–98 [DOI] [PubMed] [Google Scholar]
- 2.Muller-Kuppers M, Graf KJ, Pessin MS, et al. Intracranial vertebral artery disease in the New England Medical Center Posterior Circulation Registry. Eur Neurol 1997;37:146–56 [DOI] [PubMed] [Google Scholar]
- 3.Shin HK, Yoo KM, Chang HM, et al. Bilateral intracranial vertebral artery disease in the New England Medical Center, Posterior Circulation Registry. Arch Neurol 1999;56:1353–58 [DOI] [PubMed] [Google Scholar]
- 4.Uchiyama S, Yoshida M, Shimizu H. [MR imaging of the anterior spinal artery in a case of bilateral vertebral arterial occlusion]. Rinsho Shinkeigaku 1995;35:60–63 [PubMed] [Google Scholar]
- 5.Garnier P, Januel AC, Demasles S, et al. Collateralization of vertebral arteries. Neurology 2003;60:720. [DOI] [PubMed] [Google Scholar]
- 6.Hott JS, Vishteh G, Wallace R, et al. Anterior spinal artery supplying posterior circulation. Neurology 2004;62:468. [DOI] [PubMed] [Google Scholar]
- 7.Akar ZC, Dujovny M, Gomez-Tortosa E, et al. Microvascular anatomy of the anterior surface of the medulla oblongata and olive. J Neurosurg 1995;82:97–105 [DOI] [PubMed] [Google Scholar]
- 8.Akar ZC, Dujovny M, Slavin KV, et al. Microsurgical anatomy of the intracranial part of the vertebral artery. Neurol Res 1994;16:171–80 [DOI] [PubMed] [Google Scholar]
- 9.Rodriguez-Baeza A, Muset-Lara A, Rodriguez-Pazos M, et al. Anterior spinal arteries. Origin and distribution in man. Acta Anat (Basel)1989;136:217–21 [PubMed] [Google Scholar]
- 10.Fisher CM. Occlusion of the vertebral arteries. Causing transient basilar symptoms. Arch Neurol 1970;22:13–19 [DOI] [PubMed] [Google Scholar]