Abstract
SUMMARY: Three patients are presented with slowly progressive tetraparesis caused by an intracranial dural arteriovenous fistula with exclusive perimedullary venous drainage. MR imaging showed a swollen cervicothoracic cord with central myelopathy and dilated perimedullary veins. Bilateral vertebral angiography initially failed to demonstrate the fistulas, and diagnosis was established with external carotid angiography. All 3 patients were successfully treated with glue embolization, 1 after failed surgical exploration. Angiographic cure of the fistula resulted in clinical cure in 1 patient and stabilization in 2 patients.
Intracranial dural fistula (DAVF) consists of a meshwork of arteriovenous shunts and can be localized anywhere in the dura surrounding the brain. DAVFs are acquired lesions, probably as a result of venous thrombosis. Drainage of the fistula can be into a dural sinus, with or without reflux into cortical veins, or directly into cortical veins. Drainage into cortical veins is often associated with intracranial hemorrhage or seizures. The DAVF consists of multiple dural branches of various dural arteries converging at the site of the fistula to join a single draining vein. Surgical or endovascular repair is aimed at closure of the draining vein. If only feeding arteries are occluded and not the draining vein, collateral vessels usually develop and the fistula reopens.1–3
Rarely, intracranial dural fistulas drain exclusively into veins around the brain stem and further downward into perimedullary veins. This retrograde drainage causes congestion in the perimedullary venous system, which, in turn, leads to decreased tissue perfusion with edema and progressive loss of cord function.4–6
In this article, we report 3 patients who presented with progressive cervical cord dysfunction caused by an intracranial DAVF with perimedullary venous drainage who were treated with endovascular occlusion of the draining vein with glue.
Case Reports
Case 1
A 58-year-old man presented in another hospital with progressive difficulties in walking and bladder retention. Neurologic examination revealed paresis of both lower extremities and loss of temperature and pain sense from T10 downward. MR imaging showed swelling of the cord from C1 to T1 with edema, central myelopathy, and engorged perimedullary veins (Fig 1A). Spinal and vertebral angiograms showed no abnormalities. Three months later, the patient had become tetraparetic and was referred to our institution. At that time, he was wheelchair-bound and dependent for daily activities, including feeding.
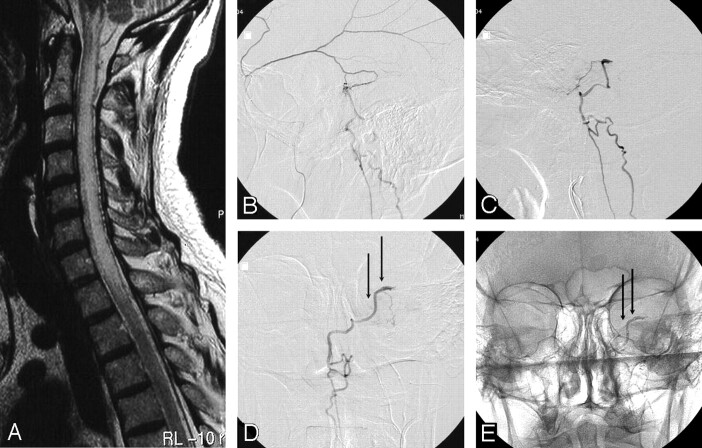
Fig 1.
A 58-year-old man with progressive cervical cord dysfunction.
A, MR image shows a swollen cervical cord with edema and central myelopathy and dilated perimedullary veins.
B, Lateral view of a selective angiogram of the left middle meningeal artery demonstrates a dural fistula, with drainage to the perimedullary veins.
C and D, Lateral (C) and anteroposterior (D) angiograms of the squamous branch of the middle meningeal artery contributing to the fistula show the beginning of the draining vein (arrows). Glue was injected from this position.
E, Anteroposterior radiograph after glue injection shows glue in the draining vein (arrows).
Angiography of the left internal and external carotid arteries showed a dural fistula fed by the tentorial artery, a branch of the ascending pharyngeal artery, and posterior and squamous branches of the middle meningeal artery, with drainage into a petrosal vein and farther downward to the anterior and posterior perimedullary veins (Fig 1B–D). A microcatheter was advanced in the posterior branch of the middle meningeal artery, and glue (a mixture of 30% Histoacryl, Braun, Melsungen, Germany; and 70% Lipiodol, Guerbet, Roissy, France), which failed to penetrate the draining vein, was injected. A 2nd glue injection, now in the feeding branch of the ascending pharyngeal artery, also failed to penetrate the vein. A 3rd microcatheter was advanced in the squamous branch of the middle meningeal artery until a wedge position was achieved (Fig 1C, -D). Under flow control, the glue was injected and pushed into the draining vein. Subsequent angiography of the internal and external carotid arteries demonstrated complete closure of the fistula. MR imaging 10 days later showed diminished cord edema and disappearance of the dilated perimedullary veins. The patient had a remarkable clinical improvement and was able to walk 2 weeks after embolization. One year later his neurologic condition was entirely normal.
Case 2
A 65-year-old man presented in another hospital with slowly progressive paraparesis and micturition problems for more than 1 year. Lately, he also experienced weakness in both upper extremities. MR imaging showed swelling and edema of the cord from C3 to T10, with engorged perimedullary veins (Fig 2A, -B). Bilateral vertebral angiography showed no abnormalities, and he was referred to our institution. Angiography of the right external carotid artery demonstrated a dural fistula supplied by the stylomastoid artery and draining into an anterior perimedullary vein downward to the conus (Fig 2C, -D). Tortuosity of brachiocephalic vessels precluded selective catheterization of the feeding branch, and the patient was offered surgery. During surgical exploration around the foramen magnum through the far lateral approach, including unilateral condyle resection, the surgeon was unable to locate the draining vein. In retrospect, the fistula was located at the petrous ridge, and this location could not be reached by the approach used by the surgeon. A second attempt of embolization was performed after direct puncture of the common carotid artery with the patient under general anesthesia. Additional 3D angiography of the external carotid artery was performed and was helpful in localizing the small stylomastoid artery supplying the fistula and in finding a working projection for catheterization. At that time, the microcatheter could be advanced in the feeding branch, and glue was injected with occlusion of the draining vein (Fig 2E, -F). Although the stylomastoid artery is the main arterial supply to the facial nerve in the facial canal, facial nerve function was intact after embolization.
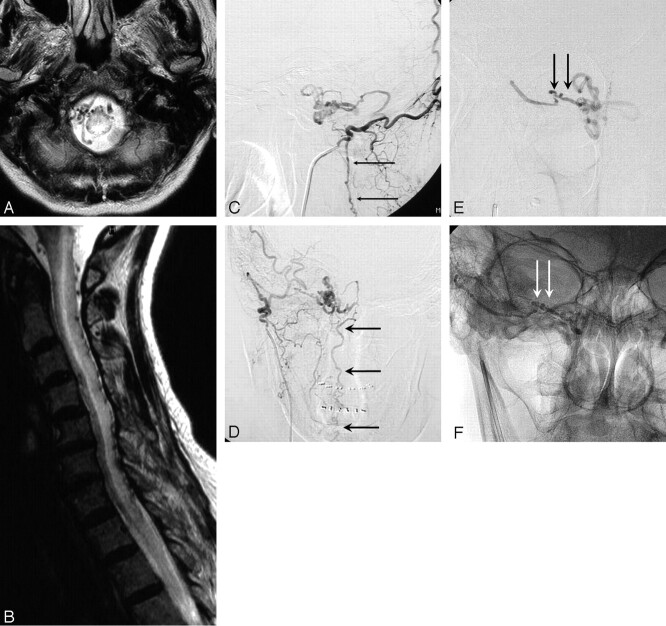
Fig 2.

A 65-year-old man with progressive cord dysfunction.
A and B, MR image shows central myelopathy in the cervicothoracic cord, with engorged perimedullary veins.
C and D, Lateral (C) and anteroposterior (D) right external carotid angiograms demonstrate a fistula with drainage to the perimedullary veins (arrows).
E, Anteroposterior projection of selective injection of a branch of the stylomastoid artery supplying the fistula. The proximal part of draining vein is marked with arrows.
F, Radiograph, same as in E, shows glue in the proximal draining vein (arrows).
G, Normal findings on MR image 1 year later.
MR imaging 2 weeks later showed improvement of the edema of the cord, and 1 year later, MR imaging findings were normal (Fig 2G). Despite closure of the fistula and normalization of MR imaging findings, the clinical condition of the patient did not improve: he remained wheelchair-bound and dependent for daily activities.
Case 3
A 72-year-old woman presented at another institution with slowly progressive paraparesis, numbness and paresthesias in both lower and upper extremities, and bladder retention for 2 years. Neurologic examination showed grades 3–4 paresis of the upper extremities, grades 2–3 paresis of the lower extremities, and loss of vital sensibility from T4 downward. MR imaging showed central myelopathy and edema from the medulla oblongata to T6, a convolute of veins at the level of the foramen magnum, and dilated posterior medullary veins (Fig 3A, -B). Spinal and bilateral vertebral angiography failed to demonstrate a fistula, and the patient was referred to our hospital. Angiography of the right internal and external carotid arteries showed a dural fistula at the skull base, likely in the marginal sinus of the foramen magnum, supplied by the transmastoid branch of the occipital artery and draining via a convolute of paramedullary veins into the posterior medullary veins (Fig 3C, -D). A microcatheter could be navigated close to the fistula site (Fig 3E), and injected glue penetrated the proximal part of the draining vein (Fig 3F). MR imaging 4 days later showed decreased cord edema and myelopathy, with disappearance of engorged perimedullary veins. Paresis of the upper extremities resolved within 1 week, but paraparesis and micturition disturbances remained. Two years after embolization, the patient is in a nursing home and dependent for daily activities.
Fig 3.
A 72-year-old woman with progressive tetraparesis.
A and B, MR images show a convolute of veins at the level of the foramen magnum, central myelopathy and edema from the medulla oblongata to T6, and dilated posterior medullary veins.
C and D, Lateral (C) and anteroposterior (D) right occipital artery angiograms show a dural fistula at the skull base, draining via a convolute of paramedullary veins into the posterior medullary veins (arrows).
E, Injection via microcatheter shows the proximal draining vein (arrows).
F, Radiograph, same as E, shows glue cast in the proximal draining vein (arrows).
Discussion
Intracranial DAVFs with perimedullary venous drainage are rare lesions. Clinically these fistulas present with slowly progressive ascending myelopathy involving first the lower limbs and then the upper limbs. Often sphincter disturbances are present. Bulbar symptoms like difficulty in swallowing, postural hypotension, and episodes of bradycardia alternating with tachycardia may be present when cord edema extends to the brain stem.4–6 The MR imaging appearance is virtually pathognomonic. A swollen cervical cord with central myelopathy and engorged perimedullary veins is indicative of the diagnosis of a fistula, either a cervical spinal DAVF or an intracranial DAVF with perimedullary venous drainage. Knowledge of the existence of these disorders with the pathophysiologic mechanisms is important to avoid unnecessary diagnostic delay. Angiography of the vertebral arteries will detect a cervical spinal DAVF only. An intracranial DAVF with perimedullary venous drainage will go undetected if internal and external carotid angiography is not performed, as was the case in all of our 3 patients.
As in all dural fistulas, treatment is directed toward closure of the draining vein, either by surgical or endovascular techniques. Surgery of these disorders requires extensive exploration of the skull base, with inherent risks7; therefore, endovascular closure of the fistula is preferred. High-quality external carotid angiography with additional 3D angiographic reconstructions facilitates the understanding of the complex anatomy of the tiny and tortuous supplying vessels. Careful navigation of the microcatheter, to avoid dissection of small arteries, to a position as close as possible to the fistula site in a wedge position with flow control allows deep penetration of the glue with occlusion of the draining vein.
After angiographic closure of the fistula, clinical evolution is variable. Some patients may show remarkable improvement, whereas others remain unchanged, despite normalization of MR imaging findings.4–6
In conclusion, intracranial DAVFs with perimedullary venous drainage are rare disorders. A clinical picture of progressive cervical cord dysfunction with a swollen cervical cord on MR imaging, with central myelopathy and dilated perimedullary veins, establishes the diagnosis. Diagnosis is confirmed with vertebral and internal and external carotid angiography. Embolization with glue is the treatment of choice; surgery can be considered when embolization has failed.
References
- 1.Mullan S. Reflections upon the nature and management of intracranial and intraspinal vascular malformations and fistulae. J Neurosurg 1994;80:606–16 [DOI] [PubMed] [Google Scholar]
- 2.Thompson BG, Doppman JL, Oldfield EH. Treatment of cranial dural arteriovenous fistulae by interruption of leptomeningeal venous drainage. J Neurosurg 1994;80:617–23 [DOI] [PubMed] [Google Scholar]
- 3.Jellema K, Sluzewski M, van Rooij WJ, et al. Embolization of spinal dural arteriovenous fistulas: importance of occlusion of the draining vein. J Neurosurg Spine 2005;2:580–83 [DOI] [PubMed] [Google Scholar]
- 4.Brunereau L, Gobin YP, Meder JF, et al. Intracranial dural arteriovenous fistulas with spinal venous drainage: relation between clinical presentation and angiographic findings. AJNR Am J Neuroradiol 1996;17:1549–54 [PMC free article] [PubMed] [Google Scholar]
- 5.Gobin YP, Rogopoulos A, Aymard A, et al. Endovascular treatment of intracranial dural arteriovenous fistulas with spinal perimedullary venous drainage. J Neurosurg 1992;77:718–23 [DOI] [PubMed] [Google Scholar]
- 6.Ricolfi F, Manelfe C, Meder JF, et al. Intracranial dural arteriovenous fistulae with perimedullary venous drainage: anatomical, clinical and therapeutic considerations. Neuroradiology 1999;4:803–12 [DOI] [PubMed] [Google Scholar]
- 7.Pannu Y, Shownkeen H, Nockels RP, et al. Obliteration of a tentorial dural arteriovenous fistula causing spinal cord myelopathy using the cranio-orbito zygomatic approach. Surg Neurol 2004;62:463–67 [DOI] [PubMed] [Google Scholar]