Abstract
SUMMARY: We describe a rare complication of myelography. A subarachnoid filling defect was apparent on the postmyelographic CT but not on conventional myelography. MR imaging performed later showed a spinal subarachnoid hematoma (SSAH), extending from L3 to L5. Lumbar puncture may rarely be a cause for SSAH and is more common in patients with coagulopathy. Significant back pain, paresis, radiculopathy, and even altered consciousness or meningeal signs may herald an SSAH.
Myelography carries risks, including infection, spinal hematoma, CSF leak, contrast reaction, radiculopathy, spinal headache, intracranial hemorrhage, and tonsillar herniation. Patients should be monitored closely for these adverse reactions. In particular, severe back pain or new neurologic symptoms following myelography should be investigated further for spinal hematoma, including the rare spinal subarachnoid hematoma (SSAH).
The first surgical description of a hematoma in the spinal subarachnoid space was by Plotkin et al in 1966.1 It was originally described as a type of subarachnoid hemorrhage, and only later was the term “spinal subarachnoid hematoma” used. The first published case of a SSAH resulting from myelography occurred in 1975 and was associated with a subdural component as well.2 Two additional cases of SSAH have been reported in the literature, both from cervical myelography.3,4
Case Report
The patient was a 46-year-old woman who had previously undergone an L5-S1 instrumented fusion. She later developed recurrence of left S1 radiculopathy and underwent repeat lumbar MR imaging, followed by diagnostic myelography.
The patient had no history of coagulopathy, and results of laboratory studies were normal. The procedure was performed with the patient prone on the x-ray table with the dural puncture at the L4–5 level by using a 22-gauge spinal needle. CSF emanated from the hub, and the contrast flowed freely into the subarachnoid space, outlining the nerve roots in the thecal sac. The patient experienced no discomfort during the procedure.
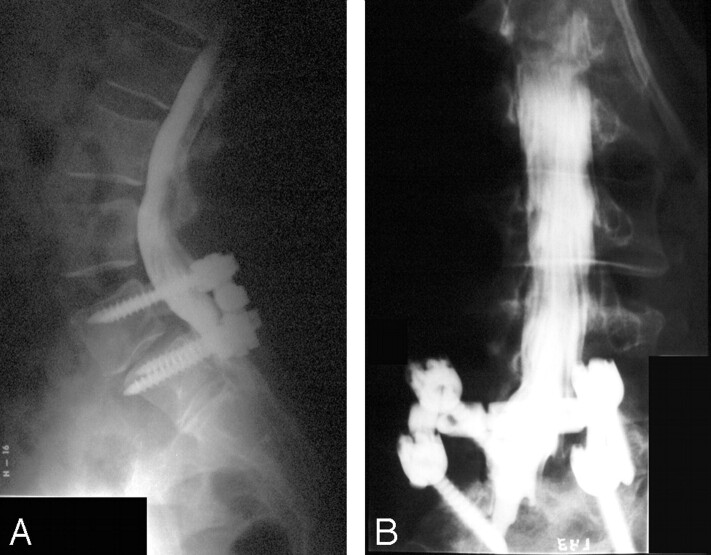
The lateral and oblique myelograms showed only small ventral and dorsal extradural filling defects, but the nerve roots were clearly seen, and there was no subarachnoid abnormality (Fig 1A, -B). CT myelography performed approximately 2 hours after dural puncture showed a subarachnoid filling defect extending from L3 to L5 (Fig 2). The possibility of a neoplasm was suggested, and follow-up MR imaging was recommended.
Fig 1.
Myelograms demonstrate small dorsal and ventral extradural filling defects but normal delineation of nerve roots, indicating no subarachnoid abnormality.
A, Cross-table lateral position.
B, Left-oblique position.
Fig 2.
Representative axial CT at L4–5 with large subarachnoid filling defect displacing the CSF and the nerve roots.
During the next 6 days, the patient developed progressive severe bilateral lower extremity pain and distal L5 and S1 motor weakness. A lumbar MR imaging revealed a subarachnoid hematoma extending from L3 to L5 (Fig 3A, -B). She was taken emergently to the operating room. The dura was dark blue; and once incised, along with the intact arachnoid, the hematoma delivered itself through the opening.
Fig 3.

MR imaging, saggital series, demonstrating spinal subarachnoid hematoma.
A, T1-weighted image showing heterogeneous signal intensity consistent with acute and subacute hematoma from L3 to L5.
B, T2-weighted image showing heterogeneous signal intensity consistent with acute and subacute hematoma.
The discordance between the relatively normal findings on the myelogram and markedly abnormal delayed CT myelogram findings was thought to be secondary to the high attenuation of the contrast material on the myelogram, which might obscure the subarachnoid finding seen on the CT myelogram. Retrospectively, however, the explanation is obvious; the hematoma was not present on the myelogram because the patient hemorrhaged during the 2-hour delay between the myelogram and the CT.
Discussion
A recent article by Sandow and Donnal5 reviewed the potential complications of myelography, including seizures, allergic contrast dye reactions, contrast-induced renal insufficiency in patients on metformin therapy, and rare cases of spinal cord or conus medullaris puncture. However, no specific mention was made of the rare occurrence of SSAH resulting from diagnostic myelography.
Domenicucci et al6 reviewed 69 cases of SSAH and found that 44.9% were iatrogenically caused by lumbar puncture (LP) performed for spinal anesthesia, CSF control, or myelography. Of the patients undergoing LP, approximately 68% had coagulopathy.6 Thus, LP is rarely a cause of SSAH in the absence of coagulopathy, unless the procedure is technically difficult. This finding makes our case quite rare because the myelography was not technically difficult and the patient did not have a coagulopathy.
A literature review performed by Kreppel et al7 of 613 patients with spinal hematomas also found anticoagulant therapy to be a higher risk, representing the second largest causative factor in that series. Anticoagulant therapy alone was not a risk for spontaneous hematoma formation; but in the setting of vascular malformations, tumors, mild trauma, and lumbar puncture, it posed a higher risk.7
These studies by Domenicucci et al6 and Kreppel et al7 suggest the importance of scrutinizing patients for coagulopathy before dural puncture. However, a review of myelography practice patterns revealed that 58% of myelographers studied did not advise discontinuing aspirin or nonsteroidal anti-inflammatory drugs, and 73% did not routinely check prothrombin time (PT) and partial thromboplastin time (PTT).1 Because a much higher proportion of patients with coagulopathy undergoing dural puncture do sustain a complicating SSAH, practice guidelines should favor routinely checking platelet count, PT, and PTT and the discontinuation of antiplatelets and anticoagulants.
Kreppel el al7 also pointed out that although spinal hematomas in general are localized, SSAHs can extend along the entire spine. Spinal hematomas usually present with back pain and developing paresis, yet SSAHs can occasionally be differentiated by their ability to mimic cerebral processes, with altered consciousness, meningeal signs and symptoms, and seizures.7 However, these intracranial symptoms may cause difficulty in distinguishing SSAH from an intracranial hemorrhage, which can occur following myelography. More important, the leading symptom of this complication is postpuncture headache.8
The neuroradiologic characteristics of SSAH are often difficult to separate from those of the more common spinal subdural hematoma. On myelography, the most significant and distinguishing feature is “capping,” described by Frager et al.9 This was not seen in our patient because the hematoma was not apparent until the delayed CT images. However, the CT scans and MR images (Figs 2 and 3) showed a mass that was surrounded by CSF and separated from the dura, which is consistent with subarachnoid location.
Conclusion
SSAH is a rare complication of dural puncture, such as that performed in myelography. It is more predominant in patients with coagulopathy, suggesting the importance of routine laboratory studies and discontinuation of antiplatelet and anticoagulant medications. The myelographer should have a high degree of suspicion for a spinal hematoma and a low threshold for MR imaging of the spine when the patient develops significant back pain, paresis, or radiculopathy. Altered consciousness, meningeal signs, and headache may, more specifically, herald an SSAH or intracranial hemorrhage. CT myelograms are nonspecific. MR imaging is more sensitive to the by-products of acute and subacute hematoma. SSAH should be considered in the differential diagnosis for intradural abnormalities following dural puncture.
Acknowledgments
We thank Debi Smedlund for image preparation.
References
- 1.Plotkin HB, Ronthal M, Froman C. Spontaneous spinal subarachnoid hemorrhage: report of 3 cases. J Neurosurg 1966;25:443–46 [DOI] [PubMed] [Google Scholar]
- 2.Kirkpatrick D, Goodman SJ. Combined subarachnoid and subdural hematoma following spinal puncture. Surg Neurol 1975;3:109–11 [PubMed] [Google Scholar]
- 3.Abla AA, Rothfu WE, Maroon JC, et al. Delayed spinal subarachnoid hematoma: a rare complication of C1–C2 cervical myelography. AJNR Am J Neuroradiol 1986;7:526–28 [PMC free article] [PubMed] [Google Scholar]
- 4.Aghi M, Couman JV, Brisman JL. Subarachnoid haematoma, hydrocephalus, and aseptic meningitis resulting from a high cervical myelogram. J Spinal Disord Tech 2004;17:348–51 [DOI] [PubMed] [Google Scholar]
- 5.Sandow BA, Donnal JF. Myelography complications and current practice patterns. AJR Am J Roentgenol 2005;185:768–71 [DOI] [PubMed] [Google Scholar]
- 6.Domenicucci M, Ramieri A, Paolini S, et al. Spinal subarachnoid hematomas: our experience and literature review. Acta Neurochir (Wien) 2005;147:741–50 [DOI] [PubMed] [Google Scholar]
- 7.Kreppel D, Antoniadis G, Seeling W. Spinal hematoma: a literature survey with meta-analysis of 613 patients. Neurosurg Rev 2003;26:1–49 [DOI] [PubMed] [Google Scholar]
- 8.Suess O, Stendel R, Baur S, et al. Intracranial haemorrhage following lumbar myelography: case report and review of literature. Neuroradiology 2000;42:211–14 [DOI] [PubMed] [Google Scholar]
- 9.Frager D, Zimmerman RD, Wisoff HS, et al. Spinal subarachnoid hematoma. AJNR Am J Neuroradiol 1982;3:77–79 [PMC free article] [PubMed] [Google Scholar]