Abstract
SUMMARY: Parent artery occlusion (PAO) is still indicated at times for the treatment of craniocervical vascular disease. Because of the unavailability of silicone and latex balloons in the United States, costly combinations of detachable and pushable coils have been required to achieve PAO. We describe our experience with a simple and less expensive alternative for PAO in 4 carotid arteries and 1 vertebral artery. This device is limited to occlusions below the base of the skull.
Since detachable silicone balloons have been removed from the market, embolization with coils has become the standard method for occlusion by neurointerventionists in the United States. It is time consuming and expensive. One of us (I.B.R.) was recently attracted by the simplicity of a device marketed for peripheral arterial occlusions. As our initial experience, described in the case report below, was favorable, we tried it in other cases and herewith describe our findings.
Case Report
A 57-year-old woman presented with a 1-month history of retro-orbital pain, 2 weeks of numbness of her forehead, and ptosis and ophthalmoplegia, all on the left side. A catheter angiogram demonstrated a 20-mm left cavernous internal carotid artery (ICA) aneurysm with no discernable neck. This was followed by a balloon test occlusion of the left ICA for 30 minutes under full heparinization, which was well tolerated. Excellent collateral flow to the left cerebral hemisphere from the right ICA via the anterior communicating artery and from the posterior circulation via the posterior communicating artery was noted while the balloon was inflated in the left ICA. It was decided that the safest and most effective treatment would be a parent artery occlusion (PAO) of the left ICA.
A 6F guiding catheter with a curved end was already in place in the ICA for the introduction of the balloon-microcatheter for the test occlusion. We removed the balloon-microcatheter and advanced the guiding catheter into the distal cervical ICA. An 8-mm Amplatzer vascular plug (AGA Medical Corporation, Golden Valley, Minn) was then pushed out the end of the guiding catheter and detached. The initial follow-up angiogram through the guiding catheter showed persistent flow through the plug. A second follow-up study, 5 minutes later, demonstrated complete cessation of flow in the ICA (Fig 1A), despite full heparinization. The guiding catheter was pulled back approximately 10 cm, and a second 8-mm vascular plug was inserted and detached in the more proximal ICA (Fig 1B). The heparin was not reversed. The femoral access sheaths were removed the following day. By the time of discharge, her pain was gone and the ptosis had begun to reverse. Within a month, the numbness was clearing, pupillary reaction was normal, and cranial nerve VI function had returned completely.
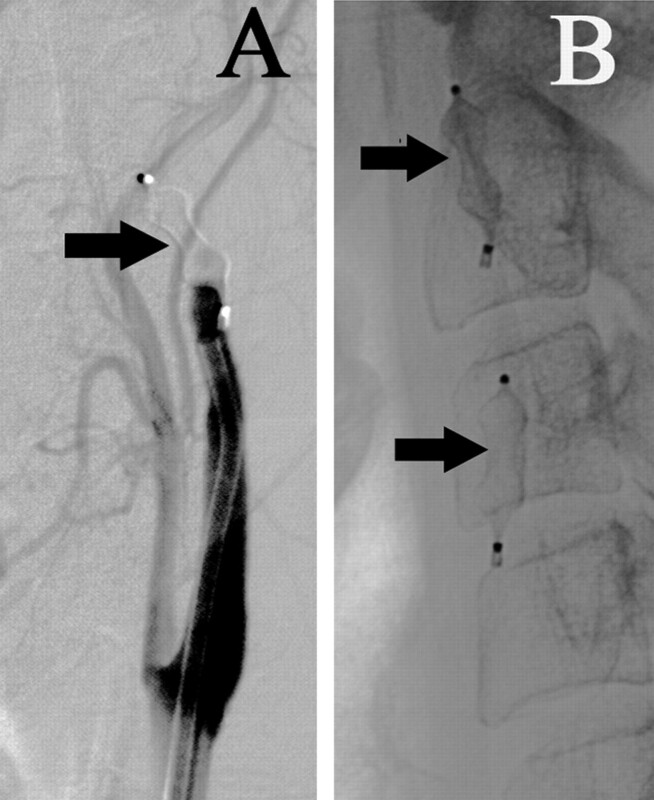
Fig 1.
A, Left ICA angiogram 5 minutes after deployment of 8-mm vascular plug (arrow) demonstrates complete ICA occlusion.
B, Lateral neck radiograph after 2 vascular plugs (arrows) have been deployed in the ICA.
Other Cases
We have had 4 other cases in which the vascular plug has been successfully used, 3 to occlude the carotid circulation and 1 to occlude the vertebral artery (VA). One of the carotid occlusions was for acute hemorrhage from a neoplastic ICA blowout. The patient had lost much blood before treatment, suffered a large stroke, and eventually died, but we were able to stop the hemorrhage and avoid immediate death. Another carotid occlusion was for definitive ICA, external carotid artery (ECA), and common carotid artery (CCA) closure after emergency surgery had controlled a neoplastic ICA blowout in another patient. The last carotid occlusion was also of the ICA, ECA, and CCA, this time for a patient with persisting transient ischemic attacks and a nearly total diffuse ICA stenosis that was not felt to be amenable to primary vessel reconstruction. We deployed no more than 2 vascular plugs per vessel occluded. In the vertebral case, in which the patient required PAO as part of the treatment of an arteriovenous fistula, we deployed the first plug at the level of the first cervical vertebra and the second slightly below this. Test occlusions were done before PAO in our elective cases, when there was a question about the adequacy of collateral flow. No patient suffered a neurologic deficit as a result of elective PAO with this device. Our experience has been that in elective cases, even with full heparinization, the vessel will occlude after the application of a second appropriately sized vascular plug. We have had no difficulty with detachment of the plugs, which is simple and rapid.
Description of Device
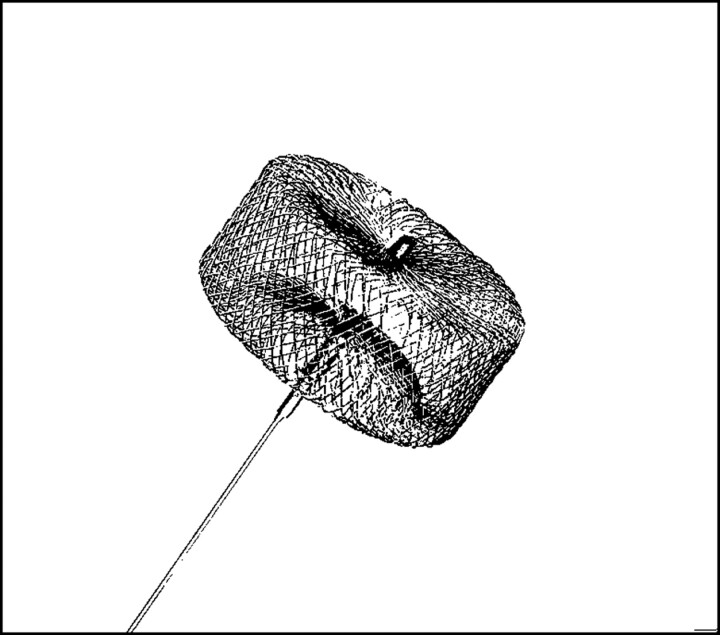
The Amplatzer vascular plug was designed and is marketed for the occlusion of the peripheral vasculature. Its use in the neurovasculature is “off-label.” The plug comes in a variety of sizes, from 4- to 16-mm diameter, in 2-mm increments. The sizes that will be of most interest to neurointerventionists will be 4-, 6-, and 8-mm plugs. The plugs of these sizes can be delivered through many 5F catheters (minimum ID = 0.056′′, maximum length = 100 cm). The cylindrical device is composed primarily of self-expanding nitinol wire mesh (Fig 2). There are platinum-iridium marker bands at each end. The proximal marker is welded to a stainless steel microscrew that allows for detachment from the 135-cm braided stainless steel delivery cable. The system is preassembled by the manufacturer; ie, the cable and vascular plug come already screwed together and loaded into an introducer sheath. It is easy to introduce into a guiding catheter through a rotating hemostatic valve and can be easily withdrawn and repositioned through the catheter before detachment. The plug is detached by simply rotating the delivery cable in a counter-clockwise direction, which unscrews the cable from the vascular plug. The manufacturer recommends selection of a device 30%–50% larger than the diameter of the vessel to be occluded.
Fig 2.
Vascular plug attached to delivery cable.
Discussion
Although direct surgical ligation of the ICA remains an option for the treatment of certain cerebral aneurysms and other vascular afflictions, endovascular techniques are popular because they are less invasive and afford the ability to assess collateral blood flow, both clinically and angiographically, at the same time as the procedure.1
Nondeconstructive techniques are now available for many pathologies that were previously treated with PAO. For instance, covered stents are becoming an option for the treatment of fistulas and large skull base aneurysms.2 Stent-assisted coiling has also been described.3 Covered stents have also been used in the management of carotid artery blowout.4
Parent vessel preservation, however, is not always possible in these situations, and PAO may at times be the only endovascular option. Other current indications for PAO are the need for vessel occlusion before major head and neck and skull base surgery by neurosurgeons and/or ear, nose, and throat surgeons, and the control of neck hemorrhage from a variety of causes, including carotid artery blowout.5,6
There is extensive experience in craniocervical vascular occlusion with detachable balloons, which are usually easy to navigate into the carotid or vertebrobasilar system. They will often flow into carotid cavernous fistulas and allow for the closure of these lesions with preservation of the lumen of the ICA. Latex balloons are difficult to obtain in the United States, and the only available silicone balloon was removed from the market several years ago by its manufacturer for regulatory reasons. Since then, interventionists in the United States have generally been forced to use coils to plug arteries. Usually, several detachable coils, followed possibly by pushable fibered coils, are necessary to achieve this end. While safe and controllable, this technique is time-consuming and expensive. Hydrogel-coated detachable coils, which swell on contact with blood, can decrease the number of coils necessary to close a vessel,7 but they are even more expensive than bare platinum coils.
We have found the vascular plug easy to deploy and fast-acting, though we have no experience with it in patients taking antiplatelet agents. Its greatest limitation is poor navigability. It opens instantly and grips the vessel wall when exited from the end of the guiding catheter. The plug cannot be navigated distal to the end of the guiding catheter from which it is delivered. Although the device can be retrieved before detachment, possible sites for deployment are limited by vessel anatomy and the navigability of the guiding catheter. A tortuous proximal ICA or VA may therefore make it impossible to deliver the vascular plug. For the same reasons, ICA and VA occlusions are presently limited to positions below the base of the skull.
References
- 1.van der Schaaf IC, Brilstra EH, Buskens E, et al. Endovascular treatment of aneurysms in the cavernous sinus. A systematic review on balloon occlusion of the parent vessel and embolization with coils. Stroke 2002;33:313–18 [DOI] [PubMed] [Google Scholar]
- 2.Redekop G, Marotta T, Weill A. Treatment of traumatic aneurysms and arteriovenous fistulas of the skull base by using endovascular stents. J Neurosurg 2001;95:412–19 [DOI] [PubMed] [Google Scholar]
- 3.Akpek S, Arat A, Morsi H, et al. Self-expandable stent-assisted coiling of wide-necked intracranial aneurysms: a single-center experience. AJNR Am J Neuroradiol 2005;26:1223–31 [PMC free article] [PubMed] [Google Scholar]
- 4.Kim HS, Lee DH, Kim HJ, et al. Life-threatening common carotid artery blowout: rescue treatment with a newly designed self-expanding covered nitinol stent. Br J Radiol 2006;79:226–31 [DOI] [PubMed] [Google Scholar]
- 5.Adams GL, Madison M, Remley K, et al. Preoperative permanent balloon occlusion of internal carotid artery in patients with advanced head and neck squamous cell carcinoma. Laryngoscope 1999;109:460–66 [DOI] [PubMed] [Google Scholar]
- 6.Cohen J, Rad I. Current management of carotid blowout. Curr Opin Otolaryngol Head Neck Surg 2004;12:110–15 [DOI] [PubMed] [Google Scholar]
- 7.Kallmes DF, Cloft HJ. The use of hydrocoil for parent artery occlusion. AJNR Am J Neuroradiol 2004;25:1409–10 [PMC free article] [PubMed] [Google Scholar]