Abstract
BACKGROUND AND PURPOSE: Conventional transforaminal epidural steroid injection (TFESI) has several problems. The purpose of this study was to compare the temporary diagnostic relief and advantages of TFESI performed using the conventional and posterolateral approaches.
METHODS: From August to December 2004, 187 patients received TFESI for lumbar radicular pain. A total of 108 patients (65 women, 43 men; mean age, 56 years) fulfilled the inclusion criteria. In essence, the needle target point was the “safe triangle,” but if there was a possibility that the needle could penetrate the nerve root or that the injectate could contact spinal nerve, posterolateral TFESI was used as an alternative. Image analyses of needle positions and chart reviews were performed. Logistic regression analysis and t test were used for statistical analysis.
RESULTS: Of the 108 patients, 75 (69.4%) showed an improvement at 2 weeks after TFESI. In 46 patients (42.6%), the needle was located in the posterolateral epidural space, and 33 (71.7%) of those experienced pain relief. Of the 62 patients in whom the needle was located in the anterior epidural position, 42 (68%) experienced pain relief. There was a significant reduction in pain sense for the posterolateral approach (P < .05). However, no statistical difference was found between the 2 approaches and temporary diagnostic relief, and no correlation was found between the other variables tested and temporary diagnostic relief (P > .05).
CONCLUSION: Our findings suggest that the posterolateral approach is an alternative method for TFESI in cases where needle tip positioning in the anterior epidural space is difficult.
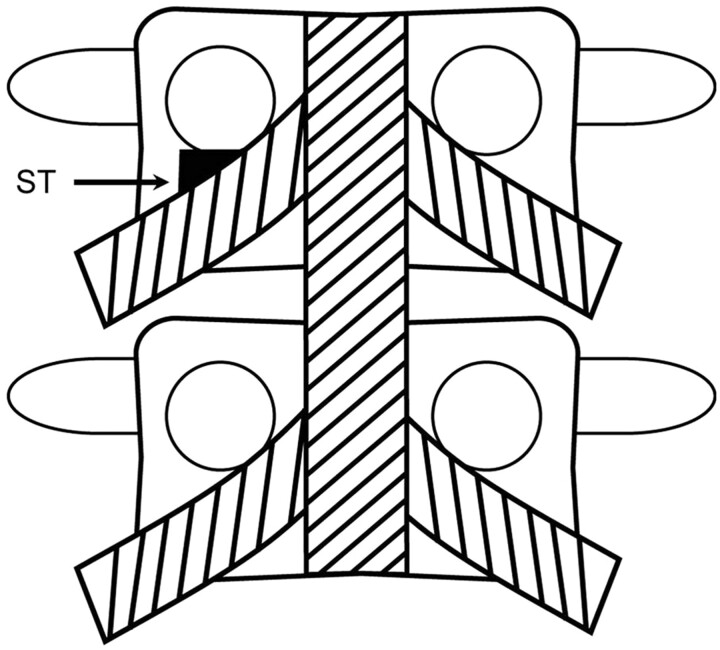
Epidural steroid injections have been used to treat lumbar radicular pain syndromes since 1952.1 Although meticulous needle placement is essential to ensure that the injectate flows into the correct compartment, the injection approach dictates whether the injectate is delivered at or as close to the target structure as possible.2 The techniques of epidural steroid injection may be classified as interlaminar, caudal, or transforaminal according to the approach taken to the epidural space. The transforaminal epidural steroid injection (TFESI) route has been preferred in many cases because it can deliver the injectate closer to the dorsal root ganglion and better facilitates ventral epidural flow to the involved nerve root complex compared with other methods.2,3 In conventional TFESI, the target needle position is located in the so-called “safe triangle,” which has a base tangential to the pedicle, one leg in line with the outer margin of the intervertebral foramen, and a hypotenuse coincident with the upper margin of the spinal nerve and dorsal root ganglion4 (Fig 1).
Fig 1.
Schematic description of the “safe triangle” for the conventional TFESI technique. The triangle is composed of a roof made up by the pedicle, a tangential base corresponding to the exiting nerve root, and the lateral border of the vertebral body. ST, safe triangle.
However, in our experience, conventional TFESI has several problems. First, in many cases, injectate is spilled along spinal nerve. Second, the needle needs to cross the nerve root in many cases to achieve a location anterior to the neural foramen. Moreover, in severe foraminal stenosis, it is more difficult to position the needle anterior to the neural foramen. Thus, we modified TFESI as follows. We targeted the needle tip medially with respect to the conventional safety triangle, to the median inferior margin of the pedicle on oblique view. We positioned the needle tip posterior to the neural foramen on lateral view (Fig 2). Using this technique, we were able to inject drug into the posterolateral epidural space and avoid spillage of injectate into the spinal nerve. In addition, this technique enabled us to avoid pricking the nerve root. We refer to this technique as posterolateral TFESI.
Fig 2.
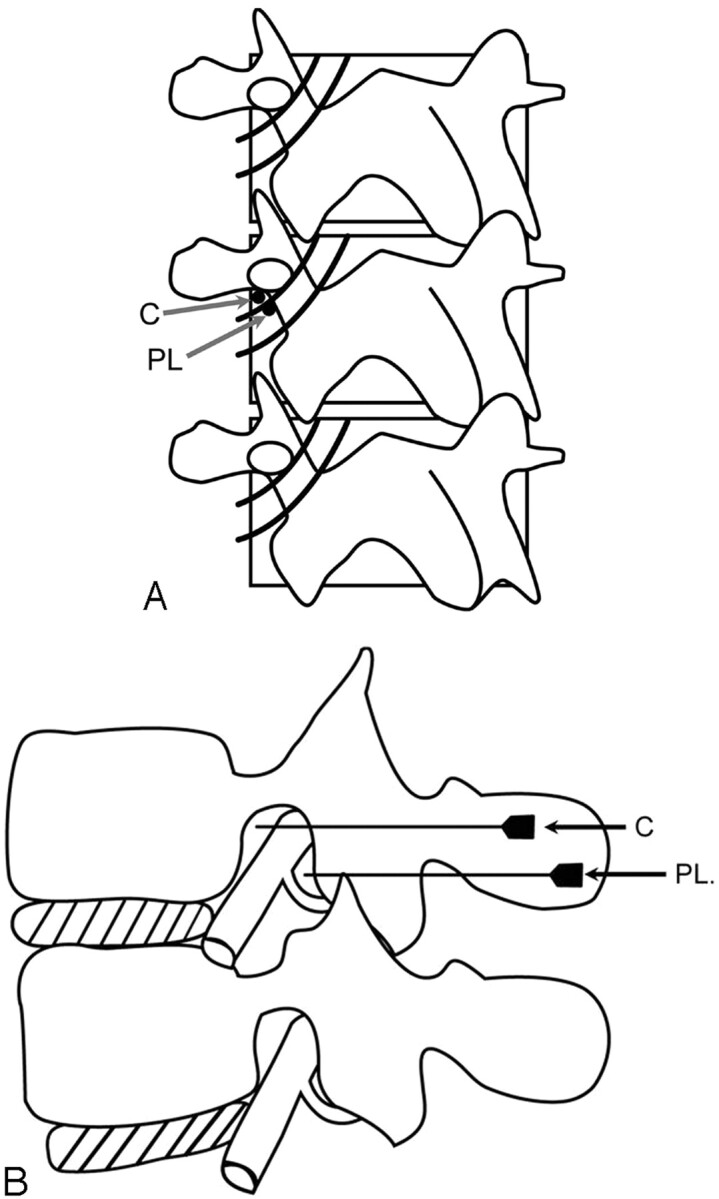
Schematic description of the conventional and posterolateral TFESI techniques. In oblique view (A), the needle tip is located in the safe triangle using the conventional technique, and the median inferior margin of pedicle with posterolateral approach. The needle appears end-on in this view. Lateral view (B) shows the needle located in the anterior and superior aspect of a nerve root using the conventional technique and at the posterior aspect using the posterolateral technique. C, conventional TFESI; PL, posterolateral TFESI.
The current study was undertaken to analyze and evaluate the temporary diagnostic relief and advantages of the posterolateral approach versus the conventional TFESI approach.
Subjects and Methods
Patient Selection
Between August and December 2004, 187 patients were treated with TFESI for lumbar radicular pain. From these patients, we selected those who met the following inclusion criteria: 1) lumbar radiculopathy, 2) clear identification of the affected nerve root by clinical and imaging studies, 3) no previous lumbar surgery, 4) no prior epidural injection, and 5) the absence of cauda equina syndrome. Our institutional review board approved all procedures.
A total of 108 patients (65 women, 43 men; mean age, 56 years; age range, 17–65 years) who fulfilled the above inclusion criteria were enrolled. All patients had undergone CT or MR imaging before the procedure. Patients were informed of the potential risks associated with the procedure and the use of steroids and provided informed consent. Patients also completed a pain diagram and questionnaire related to the distribution and the degree of their symptoms before, during, and after the procedure. TFESIs were performed at the L3 level in 5 patients, L4 in 45, and L5 in 58.
Techniques of TFESI
Patients were placed in the prone position on a fluoroscopy table. Skin was marked under C-arm tilted posterolaterally approximately at 30° to 45° and with craniocaudal angulation to profile the caudal undersurface of the pedicle above the target foramen. After sterile preparation using an iodine-based antiseptic solution, draping, and local anesthesia with a 25-gauge needle, a 22-gauge, 12-cm spinal needle was advanced into the region of the involved nerve root under fluoroscopic guidance using the technique described by Bogduk et al5 in approximately the first 120 patients. The target point was the “safe triangle,” which was composed of a roof formed by the pedicle, a tangential base that corresponded to the exiting nerve root, and the lateral border of the vertebral body (Fig 1). Biplane fluoroscopic guidance, including anteroposterior and lateral projections, was used to control correct needle positioning.
The method above is known to allow needle advancement without contacting the nerve root, and its precise location in the anterior epidural space. However, in some cases, the needle could not be placed in the anterior epidural space without crossing or pricking the nerve root. In these 28 of the 120 patients who were initially treated using the conventional approach and in the later 67, we used the posterolateral TFESI approach as an alternative. The target point of the posterolateral approach was the median inferior margin of the pedicle on oblique view and the region immediately posterior to the neural foramen on lateral view (Fig 2). We distinguished between the anterior and posterolateral TFESI approaches in terms of needle tip location within the epidural space. On lateral projection fluoroscopic image, if the needle tip was located on the anterior aspect of the neural foramen, then it was defined as an anterior TFESI approach and, if in the posterior aspect of neural foramen, the posterolateral TFESI approach. To confirm epidural flow and avoid intravascular, intradural, or soft tissue infiltration, approximately 1 mL of contrast material (Omnipaque 300; GE Healthcare, Little Chalfont, Buckinghamshire, UK) was injected before drug injection. After a meticulous review of a patient’s epidurogram, 0.5 mL of 0.5% bupivacaine hydrochloride (Marcaine Spinal 0.5% Heavy; AstraZeneca Pharmaceuticals LP, Wilmington, Del) and 40 mg (1 mL) of triamcinolone acetonide suspension (Tamceton; Hanall Pharmaceutical, Seoul, Korea) were slowly injected. Plain radiographs in the anteroposterior and lateral views were obtained after all injections had been administered to document both contrast pattern and needle position.
All injections were performed in an angiography suite equipped with biplanar fluoroscopy by a radiologist experienced at spinal intervention. Injections were performed at a level that best matched the clinical presentation and MR imaging findings. No case received an intradural or intravascular injection.
Image Analysis
Image analysis was performed individually by 3 radiologists who performed the spine injections. Needle positions were classified as anteriorly or posterolaterally located based on lateral fluoroscopic views. Causes of sciatica were determined by using preintervention imaging studies and by reviewing clinical information, and these were classified as herniated disk or spinal stenosis.
Review of Clinical Data
Follow-up interviews were conducted in a hospital visit 2 weeks after TFESI. Pain was assessed by questionnaire using a visual analog scale (VAS) before and immediately after TFESI and at the 2-week follow-up interview. VAS was presented as a 100-mm line with anchors on either end. The distance between the left anchor and the position representing the pain experienced was expressed in millimeters.6 We also adopted a 5-point patient outcome scale as follows: 0 (aggravated), 1 (stationary), 2 (improved), 3 (much improved), and 4 (no residual symptoms) for posttreatment pain assessments. We asked patients who visited the hospital 2 weeks after TFESI about the degree of pain compared with the status of pre-treatment according to the 5-point patient outcome scale. A successful outcome was defined as a score of 3 or more and a VAS score reduction of more than 60% after TFESI.
Patients were stratified by age into 6 groups; ≤29 years old, 30–39, 40–49, 50–59, 60–69, and ≥70 years old for statistical analysis. Duration of sciatica was divided into acute (<6 months) and chronic (>6 months).
Statistical Analysis
Logistic regression was performed to reveal the correlation between the temporary diagnostic relief and possible outcome predictors: conventional versus posterolateral TFESI, age, sex, duration of symptoms, and cause of radiculopathy. We used the t test to reveal pain intensity differences according to the approach used (ie, conventional or posterolateral). All statistical analyses were performed using the SPSS software package (version 10.0; SPSS, Chicago, Ill). P values of <0.05 were considered to indicate statistical significance.
Results
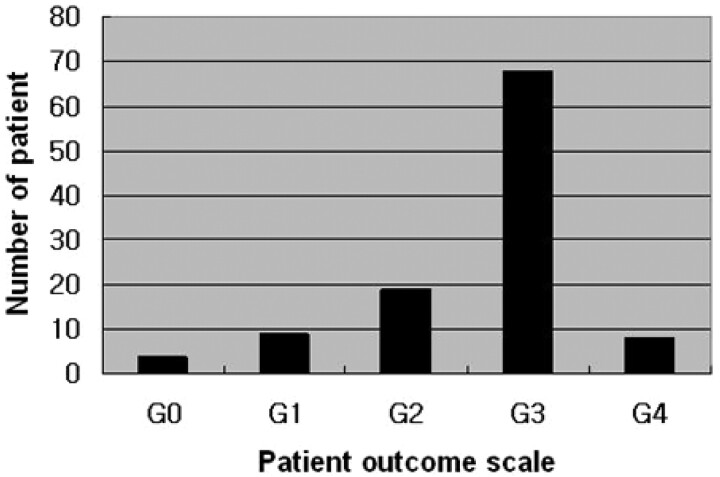
Of the 108 patients enrolled in this study, 75 patients (69.4%) showed improvement 2 weeks after TFESI as measured by the 5-point patient outcome scale and the VAS score. We investigated the 5-point patient outcome scale for all 108 patients enrolled in our study. Black bars (Fig 3) represent the number of patients according to each grade. In 46 (42.6%) of the 108 patients, the needle was located in the posterolateral epidural space, and in 62 patients (57.4%), the needle tip was located in the anterior epidural space. Thirty-three (71.7%) of the 46 patients who received a posterolateral epidural injection showed pain relief (Fig 4). Of the 62 patients with an anterior epidural needle position, 42 patients (68%) showed pain relief after the procedure (Fig 5).
Fig 3.
Bar graph showing the number of patients with respect to temporary diagnostic relief according to the 5-point patient outcome scale when interviewed 2 weeks after TFESI. G0 = 0 (aggravated), G1 = 1 (stationary), G2 = 2 (improved), G3 = 3 (much improved), G4 = 4 (no residual symptom).
Fig 4.

A 68-year-old female patient with chronic pain of the anterior aspect of the right leg and a tingling sensation in the L4 dermatome. MR imaging (not shown) showed degenerative spondylolisthesis at the L3/4 level with foraminal stenosis. There was no pain relief in follow-up of 2 weeks after a conventional transforaminal epidural steroid injection (TFESI) at the L3 level.
Fig 5.

A 26-year-old female patient with acute onset radiculopathy in the L3 dermatome. A left paracentral disk protrusion was observed at the L3/4 level in MR images (not shown). A lateral fluoroscopic view showing the needle tip positioned in the posterior aspect of the neural foramen and contrast filling into the posterolateral epidural space. The patient had no pain 2 weeks after posterolateral TFESI of L3.
No statistical difference was observed between needle position and temporary diagnostic relief. In addition, all other variables tested by logistic regression, including age, sex, duration of radiculopathy, and cause of sciatica, showed no correlation with outcome (P > .05, logistic regression). These results are summarized in the Table.
Statistical relationship between temporary diagnostic relief and the variables tested
| Outcome Predictors | No Effect (%) | Effect (%) | P-Value* |
|---|---|---|---|
| Sex | |||
| Female | 24 (36.9) | 41 (63.1) | .091 |
| Male | 9 (20.9) | 34 (79.1) | |
| Needle position | |||
| Anterior | 20 (32.3) | 42 (67.7) | .679 |
| Posterolateral | 13 (28.3) | 33 (71.7) | |
| Duration | |||
| Acute | 16 (27.1) | 43 (72.9) | .410 |
| Chronic | 17 (34.7) | 32 (65.3) | |
| Cause | |||
| HIVD | 14 (29.8) | 33 (70.2) | .895 |
| Spinal stenosis | 17 (30.9) | 38 (69.1) | |
| Others | 2 (40) | 3 (60) | |
| Age group | |||
| ≤29 years | 1 (14.3) | 6 (85.7) | .189 |
| 30-39 years | 2 (18.2) | 9 (81.8) | |
| 40-49 years | 1 (7.7) | 12 (92.3) | |
| 50-59 years | 9 (34.6) | 17 (65.4) | |
| 60-69 years | 13 (43.3) | 17 (56.7) | |
| ≥70 years | 7 (33.3) | 14 (66.7) |
Note:—HIVD indicates herniated intervertebral disk.
Compared by logistic regression.
Mean VAS length during intervention was 21.6 mm for the posterolateral approach and 53.6 mm for the conventional approach. Pain was significantly less for the posterolateral approach (P < .05, t test).
Discussion
Mechanical pressure on a nerve root caused by a herniated disk can result in radiculopathy. In addition to mechanical pressure, concomitant chemical irritation of the nerve root caused by ruptured disk material, which is capable of generating local inflammation, might also be an important factor in the development of radiculopathy.3,7 Thus, the rationale for using epidural steroid injection is based on the results of studies that have demonstrated abnormal concentrations of nociceptive and inflammatory mediators around lumbosacral disk herniations and their associations with the development of chemical neuroradiculitis.8–10 The object of an epidural steroid injection is to place corticosteroids in or near an area of inflammation, either an inflamed nerve root or the cauda equina.11 Therefore, many authors,2 including us, have anticipated that the temporary diagnostic relief of an epidural steroid injection is more pronounced in cases with an anterior epidural drug distribution.
The epidural steroid injection can be done with either CT (CT) or fluoroscopic guidance. In the 1980s, periradicular and epidural injection under CT guidance was established as a fast and exact alternative to the fluoroscopic-controlled procedure, allowing repeated and image-documented injection therapy along the altered nerve root.12 But we chose to perform all of epidural steroid injections under fluoroscopy because the technique is easier to execute and results in a cost savings. In addition, fluoroscopy more easily provides complete confidence that one’s injection is not within the vertebral artery, which could be catastrophic, and fluoroscopy-guided injections have been proved to be safe and fast injections in the axial skeleton.9,13–15 Some authors16 have recommended CT guidance to improve the learning curve in inexperienced physicians or in patients with difficult access to the epidural space (especially patients with postoperative epidural scars). However, in our study, all procedures were done by radiologists experienced at the spinal intervention, and there were no cases of failure of the epidural steroid injection under fluoroscopic guidance.
The transforaminal approach to the epidural space has gained acceptance because of its greater specificity and its utility as a diagnostic as well as a therapeutic intervention.17 Several studies have demonstrated the efficacy of TFESI for the treatment of lumbosacral radicular pain.1,2,8,18 Delivery of a therapeutic injectate transforaminally at the involved nerve root maximizes steroid concentration at the site of a pathology and minimizes the dilution effect within the epidural space. TFESI was described by Derby et al19 as a means of allowing a needle to be positioned without provoking pain. Their needle placement targeted the “safe triangle,” just below the inferior aspect of the pedicle, which allows the needle to lie above laterally with respect to the nerve. In this location, drugs can be instilled into the anterior epidural space.1,20 Using this approach, the needle tip may penetrate the lateral half of the foramen at its superior margin with minimal risk of dural puncture.2 Previous studies1,2,8 have reported that the ideal target site of a needle for TFESI is the anterior epidural space as a result of inflammation between the anterior aspect of the lumbar nerve root sleeve and the posterior aspect of the disk herniation. Thus, the so-called “safe triangle” region is usually recommended. We also have used this needle approach through the “safe triangle” region. However, even in the hands of a skilled and experienced specialist, the needle does not always head for the anterior epidural space correctly in a single puncture, and in some cases, nerve root penetration by a needle or intraneural injection have occurred when using the anterior approach. Based on our experience, a background state of severe spinal stenosis, postsurgical scarring, epidural fibrosis, advanced disk degeneration with collapse, L5 nerve root level, or transitional lumbosacral segments presents technical challenges. In such cases, we have used the posterolateral approach. In this study, we analyzed correlations between needle positions in the anterior or posterolateral epidural spaces and temporary diagnostic relief, and found no significant differences. However, patients complained of less pain sense for the posterolateral approach (P < .05). In the similar manner of our results, Pfirrmann et al7 suggested that the lateral part of the safe triangle is the best target point for the needle tip because they found less treatment induced pain when the needle tip was in that location.
Some questions arise concerning differences between posterolateral epidural and interlaminar epidural injections. Interlaminar epidural injections are easy to perform, even when using a blind approach, and present a low complication risk, whereas transforaminal injections are technically more complex and require fluoroscopic control.21–23 Moreover, therapeutic agents injected using the interlaminar approach may remain in the posterior epidural space without spreading to the affected nerve root in the anterior epidural space.24 Husemeyer and White4 reported that the anterior and both dorsolateral compartments of the lumbar epidural space appear to communicate with each other and that filling of the various compartments is asymmetric in many cases. Dorsomedian connective tissue in the posterior epidural space and deformation of the dural sac after epidural injection was found to prevent the spread of injected local anesthetic throughout the entire epidural space and to result in unilateral epidural block.25 In addition, Savolaine et al26 showed that the posterior epidural space is divided by the plica mediana dorsalis and an additional transverse connective tissue plane. Thus, if an interlaminar approach is used, larger volumes of anesthetic and corticosteroid must be injected to overcome the distance between a lesion and the epidural space compartment, which can dilute the potency of the injectate. Moreover, an interlaminar approach may be not appropriate in patients with unilateral radicular pain.
Our study has several limitations. First, it was retrospective in design. Second, we did not include other epidural steroid injection techniques, such as, interlaminar or caudal injections in this comparative study. Third, the duration of our study was short and the number of patients enrolled was small.
Based on the pathophysiology of radiculopathy as suggested by previous studies, many investigators have concluded and advocated that the injection of drugs into the anterior epidural space near the interface between a prolapsed disk and nerve root would be the most effective treatment. However, in daily practice, needles are not always located in the anterior epidural space. From time to time, drugs must be injected into the posterolateral epidural space to avoid contacting nerve root or because of other anatomic difficulties. In these cases, we question the merits of attempting to reposition a needle in an anterior epidural location, regardless of a patient’s discomfort, the time involved, and the additional radiation exposure required. The results of our study suggest that a posterolateral approach is as efficacious as the conventional approach and that it offers considerable advantages (ie, less pain during the procedure, lower risk of nerve penetration, less radiation exposure, and technical simplicity).
Conclusion
We conclude that the posterolateral approach represents an alternative TFESI method in cases with difficult needle tip positioning in anterior epidural space, because it is technically straightforward, causes less pain during the procedure, has lower risks of nerve penetration and intraneural injection, and reduces radiation exposure.
References
- 1.Botwin KP, Gruber RD, Bouchlas CG, et al. Fluoroscopically guided lumbar transforaminal epidural steroid injections in degenerative lumbar stenosis. Am J Phys Med Rehabil 2002;81:898–905 [DOI] [PubMed] [Google Scholar]
- 2.Slipman CW, Chow DW. Therapeutic spinal corticosteroid injections for the management of radiculopathies. Phys Med Rehabil Clin N Am 2002;13:697–711 [DOI] [PubMed] [Google Scholar]
- 3.Vad VB, Bhat AL, Lutz GE, et al. Transforaminal epidural steroid injections in lumbosacral radiculopathy: a prospective randomized study. Spine 2002;27:11–15 [DOI] [PubMed] [Google Scholar]
- 4.Husemeyer RP, White DC. Topography of the lumbar epidural space. A study in cadavers using injected polyester resin. Anaesthesia 1980;35:7–11 [DOI] [PubMed] [Google Scholar]
- 5.Bogduk N, Aprill C, Derby R. Epidural spinal injections. In: White AH, Schollerman J, eds. Spinal Care: Diagnosis and Treatment. St Louis: Mosby,1995. :322–43
- 6.Huskisson EC, Jones J, Scott PJ. Application of the visual-analogue scales to the measurement of functional capacity. Rheumatol Rehabil 1976;15:185–87 [DOI] [PubMed] [Google Scholar]
- 7.Pfirrmann CW, Oberholzer PA, Zanetti M, et al. Selective nerve root blocks for the treatment of sciatica: evaluation of injection site and effectiveness: A study with patients and cadavers. Radiology 2001;221:704–11 [DOI] [PubMed] [Google Scholar]
- 8.Praemer A, Furnes S, Rice DP. Musculoskeletal conditions in the United States. Am Acad Orthop Surg 1976;22:1–199 [Google Scholar]
- 9.Blankenbaker DG, Davis KW, Choi JJ. Selective nerve root blocks. Semin Roentgenol 2004;39:24–36 [DOI] [PubMed] [Google Scholar]
- 10.Marshall LL, Trethewie ER, Curtain CC. Chemical radiculitis: a clinical, physiological, and immunological study. Clin Orthop 1977;129:61–67 [PubMed] [Google Scholar]
- 11.Saal JA, Saal JS, Herzog RH. The natural history of lumbar intervertebral disc extrusions treated nonoperatively. Spine 1990;15:683–86 [DOI] [PubMed] [Google Scholar]
- 12.Schmid G, Vetter S, Göttmann D, et al. CT-guided epidural/perineural injections in painful disorders of the lumbar spine: short- and extended-term results. Cardiovasc Intervent Radiol 1999;22:493–98 [DOI] [PubMed] [Google Scholar]
- 13.el-Khoury GY, Ehara S, Weinstein JN, et al. Epidural steroid injection: a procedure ideally performed with fluoroscopic control. Radiology 1988;168:554–57 [DOI] [PubMed] [Google Scholar]
- 14.Dussault RG, Kaplan PA, Anderson MW. Fluoroscopy-guided sacroiliac joint injections. Radiology 2000;214:273–77 [DOI] [PubMed] [Google Scholar]
- 15.Link SC, el-Khoury GY, Guilford WB. Percutaneous epidural and nerve root block and percutaneous lumbar sympatholysis. Radiol Clin North Am 1998;36:509–21 [DOI] [PubMed] [Google Scholar]
- 16.Kraemer J. Orthopaedische Schmerztherapie. Dt Aerztebl 1996;93A:1961–65 [Google Scholar]
- 17.Slosar PJ, White AH. The use of selective nerve root blocks: diagnostic, therapeutic, or placebo? Spine 1998;23:2253–54 [DOI] [PubMed] [Google Scholar]
- 18.Tiso RL, Cutler T, Catania JA, et al. Adverse central nervous system sequelae after selective transforaminal block: the role of corticosteroids. Spine J 2004;4:468–74 [DOI] [PubMed] [Google Scholar]
- 19.Derby R, Bogduk N, Kine G. Precision percutaneous blocking procedures for localizing spinal pain: part 2. The lumbar neuroaxial compartment. Pain Digest 1993;3:175–88 [Google Scholar]
- 20.Johnson BA, Schellhas KP, Pollei SR. Epidurography and therapeutic epidural injections: technical considerations and experience with 5334 cases. AJNR Am J Neuroradiol 1999;20:697–705 [PMC free article] [PubMed] [Google Scholar]
- 21.Lew HL, Coelho P, Chou LH. Preganglionic approach to transforaminal epidural steroid injections. Am J Phys Med Rehabil 2004;83:378. [DOI] [PubMed] [Google Scholar]
- 22.Weinstein SM, Herring SA, Derby R. Contemporary concepts in spine care: epidural steroid injections. Spine 1995;20:1842–46 [DOI] [PubMed] [Google Scholar]
- 23.Botwin KP, Gruber RD, Bouchlas CG, et al. Complications of fluoroscopically guided transforaminal lumbar epidural injections. Arch Phys Med Rehabil 2000;81:1045–50 [DOI] [PubMed] [Google Scholar]
- 24.Thomas E, Cyteval C, Abiad L, et al. Efficacy of transforaminal versus interspinous corticosteroid injection in discal radiculalgia-a prospective, randomized, double-blind study. Clin Rheumatol 2003;22:299–304 [DOI] [PubMed] [Google Scholar]
- 25.Tetsushi F, Tatsuhiko K, Tomomi S. Radiographic investigation of unilateral epidural block after single injection. Anesthesiology 1997;87:1574–75 [DOI] [PubMed] [Google Scholar]
- 26.Savolaine ER, Pandya JB, Greenblatt SH, et al. Anatomy of the human lumbar epidural space: new insights using CT-epidurography. Anesthesiology 1988;68:217–20 [DOI] [PubMed] [Google Scholar]