Abstract
BACKGROUND AND PURPOSE: There are limited data correlating MR imaging and anatomic findings of ligamentous injury in cervical spine trauma. This study compares acute MR imaging with surgical observations of disk/ligamentous injury after blunt cervical trauma.
MATERIALS AND METHODS: Consecutive patients with acute cervical spine trauma who underwent preoperative MR imaging and surgery from 1998 to 2001 were identified. MR imaging was obtained within 48 hours of injury for most patients. All scans included sagittal T1, T2 fat-saturated, and short tau inversion recovery sequences. At surgery, extent of injury at the operated level was recorded on a standardized form for either anterior or posterior structures or both depending upon the operative approach. MR examinations were separately evaluated by 2 readers blinded to the intraoperative findings. Radiologic and surgical findings were then correlated.
RESULTS: Of 31 patients, an anterior surgical approach was chosen in 17 patients and a posterior approach in 13 patients. In one patient anterior and posterior approaches were utilized. Seventy-one percent of patients had spinal cord injury on MR imaging. MR imaging was highly sensitive for injury to disk (93%), posterior longitudinal ligament (93%), and interspinous soft tissues (100%), but it was less sensitive for injury to the anterior longitudinal ligament (71%) and ligamentum flavum (67%). For most ligamentous structures, there was limited agreement between specific MR imaging findings and injury at surgery.
CONCLUSION: In acute cervical spine trauma, MR imaging has moderate to high sensitivity for injury to specific ligamentous structures but limited agreement between specific MR imaging findings and injury at surgery. MR imaging may overestimate the extent of disruptive injury when compared with intraoperative findings, with potential clinical consequences.
MR imaging has become part of the standard imaging protocols for patients with acute cervical spine injury. There are 2 distinct patient populations for which MR imaging is recommended. One consists of patients with negative radiographs and negative CT who have neurologic symptoms or persistent neck pain. The other population consists of patients with fracture or unstable injury noted on radiographic or CT work-up. These patients often go on to MR imaging for preoperative planning. It is this second population that is the focus of our study.
In the severely injured patient, MR imaging has utility in defining the status of the spinal cord and nerve roots and in determining the extent of ligamentous and soft tissue injury. In particular, the spine surgical literature stresses the importance of evaluating the disk and anterior ligamentous structures before posterior fusion for facet joint disruption.1,2 Patients who undergo posterior fusion without attention to an overlooked disk injury are at risk for progressive cord compression. Therefore, the status of the annulus and longitudinal ligaments as evaluated on MR imaging potentially plays a very important role in determining the surgical approach.
The spectrum of posttraumatic injury to the cervical spinal cord and the relationship between cord abnormality and clinical course have been well documented.3–7 For injury to the ligamentous and soft tissue structures, MR imaging findings have also been described.8–15 However, there is a conspicuous paucity of data confirming posttraumatic MR imaging observations with in vivo injury for these structures. Many of the studies evaluating MR imaging did not have a true external reference standard but indirectly compared MR imaging with CT or radiography by excluding cases with positive CT or radiographic findings16–20 whereas others have directly compared MR imaging with other imaging modalities.21–28 Some studies included neurologic outcome as the reference standard.21,29
Only 4 studies attempted direct correlation between anatomic or surgical findings and MR imaging findings, either utilizing cadavers30 or intraoperative verification for those patients who went on to surgery based on clinical or imaging findings.31–33 Most of these studies have concluded that MR imaging is accurate and/or efficacious. However, because most of these studies do not have an independent external standard for verification, they cannot address the potential for false- positive MR imaging findings. Other studies evaluating outcome, however, suggest that regardless of findings, MR imaging has limited impact on clinical outcome.4,6,27 In contrast, one pediatric study of MR imaging use in acute spine injury claims that MR imaging is cost-effective.34 We undertook the current study to directly compare preoperative MR imaging findings with intraoperative findings in severely injured patients. We hypothesized that MR imaging tends to overestimate the degree of disruptive soft tissue injury due to its remarkable sensitivity.
Methods
The study was approved by our Institutional Review Board. Consecutive patients who underwent operative fixation for acute cervical spine trauma between 1998 and 2001 at a level I trauma center were identified. Of these, only patients who had an available preoperative MR imaging of the cervical spine and whose operative level was C3 and below were further evaluated.
Operative findings were recorded prospectively by the spine surgeon at the time of surgery on a standard form that was designed to collect information for an ongoing spinal injury data base. Patients for whom operative findings were not thus recorded were excluded. For the ligaments, the operating surgeon recorded whether at surgery the structure was intact or partially or completely torn. For the disk and facet capsules, the operating surgeon recorded whether at surgery the structure was intact or partially or completely disrupted. For the vertebral body and posterior osseous elements, the surgeon recorded whether they were fractured. The operating surgeon was aware of the preoperative MR imaging interpretation on the medical record.
Importantly, the operative approach determined which structures were adequately visualized by the surgeon. For the anterior approach, the anterior longitudinal ligament (ALL), disk annulus, vertebral body, and posterior longitudinal ligament (PLL) were generally visualized at the level of surgery. There was limited to absent visualization of posterior structures. Similarly for the posterior approach, the superficial dorsal soft tissues, interspinous soft tissues, ligamentum flavum, and posterior osseous elements were visualized at the level of surgery. From this approach the anterior structures were difficult to assess. Therefore, depending on the approach, surgical information was available for either the anterior or the posterior structures. Furthermore, the extent of operative exposure limited evaluation of spine levels that were above, below, or remote from the primary operative level.
All MR imaging scans were obtained on a 1.5T system (GE Signa, General Electric Medical Systems, Milwaukee, Wis). All included sagittal T1 (TR 500–600 ms, TE 10 ms), sagittal T2 fat-saturated (TR 2700–4000 ms, TE 75), sagittal short tau inversion recovery (STIR) (TR 3500–4300 ms, TE 30 ms, TI 140–180 ms), and axial multiplanar gradient-recalled (TR 610 ms, TE 17 ms, flip angle 10°) sequences. Images were evaluated on film. Retrospective evaluation of the preoperative MR imaging scans was performed by 2 radiologists, both of whom were blinded to the intraoperative findings and to the preoperative MR imaging study interpretation but not to the level of surgery. They were also blinded to the results of any other preoperative imaging that was performed such as radiography or CT. The retrospective evaluation focused on the operated level, and the findings were decided by consensus. This retrospective evaluation was independent of the initial preoperative MR imaging interpretation in the patient medical record.
Patient age, sex, and presence or absence of cord injury on MR imaging were noted. The following structures were evaluated on MR imaging (at the operative level only): ALL, intervertebral disk annulus, PLL, vertebral body, ligamentum flavum, posterior osseous elements (consisting of pedicles, facets, and laminae), facet capsules, and interspinous soft tissues. Presence and degree of injury were identified.
The ALL and PLL were considered abnormal if they demonstrated high T2 signal intensity or displacement or complete tear. The disk annulus, ligamentum flavum, and interspinous soft tissues were considered abnormal if they demonstrated high T2 signal intensity or complete disruption. The facet capsules were considered abnormal if they demonstrated high T2 signal intensity relative to other levels or widening (>2 mm) or dislocation. These evaluations are consistent with descriptions of injury patterns in the literature.8–15 The vertebral body was considered abnormal if it demonstrated marrow edema (abnormal high marrow T2 signal intensity) or fracture (change in shape). The posterior osseous structures were considered abnormal only if a fracture was demonstrated, regardless of signal intensity (Table 1).
Table 1:
Patterns of abnormality seen on MR imaging for ligamentous structures and disks as described in the literature8–15
| Structure | Abnormality on MR Images |
|---|---|
| Anterior longitudinal ligament | High T2 signal |
| Displacement/elevation | |
| Disruption | |
| Disk | High T2 signal |
| Widening | |
| Posterior longitudinal ligament | High T2 signal |
| Displacement/elevation | |
| Disruption | |
| Vertebral body | Abnormal marrow signal (bone contusion) |
| Deformity of shape/contour (fracture) | |
| Posterior osseous structures | Deformity of shape/contour (fracture) |
| Facet capsules | High T2 signal |
| Widening | |
| Dislocation | |
| Ligamentum flavum | High T2 signal |
| Disruption | |
| Interspinous soft tissues | High T2 signal |
| Disruption |
The MR imaging findings were then compared with the intraoperative findings to determine accuracy of MR imaging and to calculate kappa values for measuring reliability between specific MR imaging findings and intraoperative findings of injury.35 Statistical analysis was performed by using STATA 8.0 (Stata, College Station, Tex).
Results
Sixty-five consecutive patients underwent operative fixation between 1998 and 2001 for acute blunt cervical spine trauma. Of these, 31 met the inclusion criteria. There were 23 men and 8 women (age range of 15–76 years). Mechanisms of injury were distributed as follows: motor vehicle collision in 24 patients, diving injury in 2, fall in 2, skiing injury in 2, and crush injury in 1. All patients except 2 had a cervical spine MR imaging within 48 hours of presentation after injury and underwent surgery within 7 days after the MR imaging. Of the 2 in whom work-up was delayed, one patient underwent MR imaging at our institution 6 days following injury after transfer from an outside facility. The other patient was followed with serial radiographs and CT for 30 days following injury before having a cervical spine MR imaging.
Seventeen patients underwent an anterior surgical approach, 13 a posterior approach, and one underwent both anterior and posterior fusion. Therefore, overall there were 18 sets of anterior structures evaluated and 14 sets of posterior structures evaluated. Six posterior osseous structures were evaluated for each patient, consisting of 2 pedicles, 2 laminae, and 2 facets.
The results from intraoperative correlation with MR imaging findings are shown in Tables 2 and 3.
Table 2:
Sensitivity of MR imaging relative to intraoperative findings for soft tissue and ligamentous structures in the subdental cervical spine
| Structure | No. Injured at Surgery | N | Sensitivity (%) |
|---|---|---|---|
| Anterior longitudinal ligament | 14 | 18 | 71 |
| Disk | 15 | 18 | 93 |
| Posterior longitudinal ligament | 15 | 18 | 93 |
| Vertebral body | 6 | 18 | 100 |
| Posterior osseous structures | 22 | 77 | 45 |
| Facet capsules | 22 | 26 | 86 |
| Ligamentum flavum | 6 | 14 | 67 |
| Interspinous soft tissues | 6 | 14 | 100 |
Note:—Sensitivity here is defined as the proportion of injuries at surgery that were abnormal on MR imaging: that is, (True-positive)/(True-positive + False-negative).
Table 3:
Kappa values for agreement between MR imaging findings and intraoperative findings of injury to osseous and soft tissue/ligamentous structures
| Anatomic Structure | Surgical Finding(s) | MRI Finding(s) | κ |
|---|---|---|---|
| Anterior longitudinal ligament | Partial or complete tear | Abnormal signal | minus;0.12 |
| Partial or complete tear | Ligament elevation | 0.069 | |
| Partial or complete tear | Complete disruption | 0.053 | |
| Partial or complete tear | Any of above abnormalities | −0.033 | |
| Partial or complete tear | Elevation or disruption | 0.18 | |
| Complete tear | Abnormal signal | 0.11 | |
| Complete tear | Ligament elevation | −1.0 | |
| Complete tear | Complete disruption | 0.32 | |
| Complete tear | Any of above abnormalities | 0.18 | |
| Complete tear | Elevation or disruption | 0.31 | |
| Posterior longitudinal ligament | Partial or complete tear | Abnormal signal | −0.054 |
| Partial or complete tear | Ligament elevation | 0.18 | |
| Partial or complete tear | Complete disruption | 0.0 | |
| Partial or complete tear | Any of above abnormalities | 0.31 | |
| Partial or complete tear | Elevation or disruption | 0.29 | |
| Complete tear | Abnormal signal | 0.16 | |
| Complete tear | Ligament elevation | 0.14 | |
| Complete tear | Complete disruption | −0.07 | |
| Complete tear | Any of above abnormalities | 0.27 | |
| Complete tear | Elevation or disruption | 0.077 | |
| Intervertebral disk | Partial or complete disruption | Abnormal signal | 0.077 |
| Partial or complete disruption | Complete disruption | −0.24 | |
| Partial or complete disruption | Any of above abnormalities | −0.09 | |
| Complete disruption | Abnormal signal | 0.18 | |
| Complete disruption | Complete disruption | −0.09 | |
| Complete disruption | Any of above abnormalities | 0.21 | |
| Right facet capsule | Partial or complete disruption | Abnormal signal | 0.041 |
| Partial or complete disruption | Widening of joint | 0.26 | |
| Partial or complete disruption | Complete disruption | 0.018 | |
| Partial or complete disruption | Any of above abnormalities | 0.58 | |
| Partial or complete disruption | Widening or disruption | 0.44 | |
| Left facet capsule | Partial or complete disruption | Abnormal signal | −0.12 |
| Partial or complete disruption | Widening of joint | 0.20 | |
| Partial or complete disruption | Complete disruption | 0.20 | |
| Partial or complete disruption | Any of above abnormalities | 0.43 | |
| Partial or complete disruption | Widening or disruption | 0.53 | |
| Ligamentum flavum | Partial or complete tear | Abnormal signal | −0.13 |
| Partial or complete tear | Complete disruption | 0.32 | |
| Partial or complete tear | Any of above abnormalities | 0.21 | |
| Complete tear | Abnormal signal | −0.098 | |
| Complete tear | Complete disruption | 0.0187 | |
| Complete tear | Any of above abnormalities | −0.017 | |
| Interspinous ligament | Partial or complete tear | Abnormal signal | −0.29 |
| Partial or complete tear | Complete disruption | 0.42 | |
| Partial or complete tear | Any of above abnormalities | 0.11 | |
| Complete tear | Abnormal signal | −0.29 | |
| Complete tear | Complete disruption | 0.39 | |
| Complete tear | Any of above abnormalities | 0.060 | |
| Vertebral body | Fracture | Abnormal signal | −0.37 |
| Fracture | Fracture (change in shape) | 0.48 | |
| Fracture | Any of above abnormalities | 0.19 | |
| Right lamina | Fracture | Fracture (change in shape) | 0.19 |
| Fracture | |||
| Left lamina | Fracture | Fracture (change in shape) | 0.074 |
| Fracture | |||
| Right pedicle | Fracture | Fracture (change in shape) | 0.41 |
| Fracture | |||
| Left pedicle | Fracture | Fracture (change in shape) | 0.62 |
| Fracture | |||
| Right facet | Fracture | Fracture (change in shape) | 0.39 |
| Fracture | |||
| Left facet | Fracture | Fracture (change in shape) | 0.51 |
Anterior.
Of the 18 patients who underwent anterior fusion, 14 were noted to have ALL injury and 15 were noted to have disk and/or PLL injury at surgery. Vertebral body fractures were demonstrated intraoperatively in 6 patients. MR imaging was highly sensitive (93%) for injury to the intervertebral disk and to the posterior longitudinal ligament. MR imaging had limited sensitivity (71%) for the anterior longitudinal ligament.
Posterior.
Of the 14 patients who underwent posterior fusion, 6 had ligamentum flavum or interspinous ligament injury at surgery. In one patient, the parasagittal MR imaging images were nondiagnostic for the posterior osseous elements and facet capsules. Similarly, in another patient, the left pedicle could not be evaluated. These structures were therefore excluded. Of the remaining 77 posterior osseous structures and 26 facet joint capsules, 22 osseous structures and 22 facet joint capsules were found injured at surgery. MR imaging was sensitive for injury to the facet capsules (86%) and interspinous soft tissues (100%), with more limited sensitivity for the ligamentum flavum (67%).
Reliability between MR imaging and intraoperative findings was variable, ranging from almost zero agreement to good agreement (Table 3). In general, there was poor agreement between abnormal MR imaging ligament signal intensity and intraoperative findings (κ = [ms]0.029–0.13). Moderate agreement was observed between the presence of facet capsular widening or disruption on MR imaging and intraoperative findings (κ = 0.44–0.53). Vertebral body fractures with deformity on MR also agreed moderately well with fracture identified intraoperatively (κ = 0.48). We did not identify consistent patterns between other MR imaging findings and intraoperative findings. However, agreement overall tended to be low.
Discussion
Our study compared MR imaging findings with prospectively gathered intraoperative findings at the level of injury and found low agreement overall for disruptive injury to soft tissue and ligamentous structures. We note good sensitivity for the intervertebral disk, PLL, and interspinous soft tissues, and lower sensitivity for the ALL and the ligamentum flavum.
MR imaging is utilized in patients with acute cervical spine trauma for 2 distinct reasons. One is an evaluation of neurologic or ligamentous integrity in the symptomatic patient with negative radiographic work-up, and the other is preoperative planning in the patient with an unstable fracture noted on other imaging. Many studies have examined the role of MR imaging in the evaluation of instability. Benzel et al studied 174 patients with negative radiographs and found that 36% had positive findings on MR imaging.16 Goldberg et al evaluated 100 patients after acute trauma and found that 31 had positive MR imaging findings.17 In separate studies, Kihiczak et al, D’Alise et al, and Geck et al looked at MR imaging in posttraumatic patients with negative radiographs and found that MR imaging picked up injuries,18–20 thereby implying that MR imaging is effective in this setting relative to radiographs or/and CT. These studies did not have an external reference standard.
Other studies have directly compared MR imaging with CT or radiographs. Mirvis et al reported on patients with neurologic deficits after trauma who had myelography, CT myelography, radiographs, or intraoperative sonography in addition to MR imaging.25 He concluded that MR imaging is superior to other modalities for evaluation of the cord and the intervertebral disk while CT was superior for fractures. Orrison et al compared MR imaging with CT and radiographs and found that the rate of positive findings was higher for MR imaging for the soft tissues and ligaments.26 Levitt et al studied 49 patients with MR imaging, 33 of whom also underwent CT, and they also found that MR imaging was superior to CT for injury to the spinal cord and the intervertebral disk.28 Similarly, Tarr et al found that MR imaging was superior to CT for soft tissue and ligamentous injury.23 Klein et al evaluated MR imaging for bony injury by using CT as the reference standard, and they found that CT was more sensitive.22 Katzberg et al calculated weighted sensitivities for radiographs versus MR imaging in their study and found that MR imaging depicted 79% of injuries whereas radiographs depicted only 23%.24 Three studies have used clinical outcome as the reference standard.21,27,29
Although they support the use of MR imaging in cervical spine trauma, the above studies do not use a surgical reference standard and do not address the issue of using MR imaging for surgical planning. We are aware of 4 studies that utilized direct anatomic correlation (whether intraoperative or cadaveric) to confirm MR imaging observations. Kliewer et al correlated MR imaging findings with pathologic findings in 28 cadavers and found that MR imaging correctly identified 79% of ligament disruptions.30 In this study, ALL and PLL injuries were detected in all 7 cases, but for the ligamentum flavum, facet capsules, and the interspinous tissues, there were 3 false-positives and 11 false-negatives. In the study by Emery et al, MR imaging detected ligament damage in 17 of 19 patients found to have injury at surgery and there were no false-positives.32 Terk et al found a high degree of correlation of MR imaging with surgical findings in 6 patients, albeit in the thoracolumbar spine.33 Warner et al reported on 163 patients who had MR imaging of which there were 43 injuries, 24 of which underwent internal fixation.31 In the 6 patients where operative notes were adequate, they found that MR imaging identified 6 of 6 injured ALLs, 4 injured PLLs (with 2 false-positives), 2 of 2 injured ligamenta flava, and 2 of 2 injured interspinous soft tissues.
Our study confirms the high sensitivity of MR imaging for most ligamentous injuries. In particular, in our data, MR imaging was sensitive for injury to the PLL, interspinous ligaments, disk annulus, and facet capsular ligaments. Ligamentous injury was best evaluated on the parasagittal images; axial images were useful for evaluating injuries to the osseous posterior elements and the facet joints only.
We observed less sensitivity of MR imaging to ALL injury. The relatively lower sensitivity for the ALL on our study may be accounted for in 2 ways: 1) this structure is inherently difficult to accurately evaluate for integrity; and/or 2) patients went on to surgery based on disk morphology regardless of ALL imaging findings, thereby lowering the verification bias for this particular structure. Despite the high sensitivity of MR imaging, our study does raise concerns regarding the relative lack of agreement between specific MR-detected abnormalities and corresponding intraoperative findings.
Limitations of this study include small sample size and limited surgical visualization as discussed above. The issue of utilizing surgical findings as the reference standard is not without limitations; however, this approach provides a ready comparison that is directly suited to our goal of determining how MR imaging might potentially affect surgical decision making, in addition to providing an external anatomic standard that is lacking in most other studies on this subject. We suspect that the exquisite soft tissue contrast afforded by MR imaging picks up subtle ligamentous sprains and soft tissue contusions. Such findings may not be appreciated at surgery if there is no frank structural disruption. Nevertheless, soft tissue contusion without disruption seen on MR imaging is important in that it may falsely suggest disruptive injury and potential surgical instability. Whether clinical decisions based on this limited accuracy are of consequence should be evaluated prospectively.
The use of a consensus reading, rather than independent blinded readers, is another limitation of the study because it does not allow quantification of reproducibility and reliability of findings between the MR imaging readers. We are in the process of implementing another prospective study of the use of MR imaging in cervical spine trauma that will also include independent blinded readers as part of the protocol.
Another very pertinent limitation of this study is the inherent verification bias. For example, only patients with abnormal anterior structures on MR imaging went on to surgery with the anterior approach, and this could potentially falsely inflate sensitivity. Verification bias is not practical to eliminate in studies such as this for the same reason that it is difficult to obtain controls by subjecting patients with normal imaging to spinal surgery. Finally, because we only studied subjects who underwent operations, we were unable to confirm diagnoses in all subjects with normal MR imaging appearance, preventing us from calculating MR specificity.
The upper cervical spine through C2 was excluded from the study because this region is anatomically and functionally distinct from the remainder of the spine with regard to ligamentous architecture. The current imaging protocol for acute cervical spine trauma at our institution includes sagittal T1, T2 with fat saturation, and STIR, as well as axial multiplanar gradient-recalled sequences. This protocol is utilized for evaluation of the subdental cervical spine. For the upper cervical spine, a separate protocol is employed that uses a dedicated high-resolution surface coil to obtain high-resolution images. In the acutely injured patient this protocol accentuates the presence of abnormal T2 signal intensity as well as anatomically visualized separation of structures to determine the presence of injury.
There is some controversy in the statistical literature regarding use of the kappa statistic in the measurement of intra- and interobserver reliability.36–38 Several issues are pertinent to this study. One is that kappa values are paradoxically lowered in the setting of a high prevalence index, which is the case here for many of the structures evaluated.39 Second, the measured observations were made on different modalities by different observers: the surgeons evaluated intraoperative findings, whereas the radiologists evaluated MR imaging findings. Moreover, the surgeons used 3 categories for most structures (normal, partial, or complete), whereas the MR imaging findings for some structures (such as the ALL, PLL, and facet capsules) had 4 categories. Finally, to make practical sense out of numerical kappa values in the clinical context, they are often assigned qualitative descriptors (eg, “poor,” “fair,” “moderate”). The classification used here is that proposed by Landis and Koch,40 though other differing grading schemes exist.40 The process of assigning and using qualitative descriptors such as poor or fair as a substitute for numerical kappa values in studies of observer agreement is inherently arbitrary and its meaningfulness in the clinical setting is subject to debate.39
Note that the severely injured population undergoing MR imaging for preoperative planning is the target population for this study. Caution should therefore be exercised in generalizing the above conclusions to the separate radiographically normal population with persistent pain or neurologic symptoms. Nonetheless, it is not unreasonable to suspect that even in the absence of a radiographic fracture, MR imaging has the potential to overestimate the extent of soft tissue disruption when evaluating instability.
Conclusion
There are very few studies evaluating posttraumatic cervical spine MR imaging with an external reference standard. In our study, we retrospectively compared MR imaging findings at the injured level with prospectively gathered intraoperative findings and found that MR imaging is sensitive for injury to the disk, PLL, and interspinous ligament/soft tissues. In general, there was poor reliability between individual findings on MR imaging and intraoperative injury to specific structures, though for displaced vertebral body fractures and facet joint disruption agreement was moderate. Based on these results, some caution should be used in relying on MR imaging for preoperative planning, as MR imaging may falsely overestimate the degree and extent of disruptive injury.
Fig 1.

True-positive injuries to the ALL, disk, and PLL. Sagittal STIR image demonstrates disruption of the ALL (arrow), intervertebral disk, and PLL (arrowhead) at C6–7. Injuries were confirmed at surgery.
Fig 2.

True-positive injuries to the ALL, disk, and PLL. Sagittal fast spin-echo T2-weighted image shows elevation of the ALL (white arrow), disruption of the intervertebral disk, and elevation of the PLL at C4–5 (black arrow). Injuries were confirmed at surgery.
Fig 3.

True-positive ligamentum flavum and interspinous ligament injuries. Sagittal STIR image demonstrates complete disruption of the ligamentum flavum (arrow) and interspinous ligament complex (paired small arrows) at C6–7, which was confirmed at surgery.
Fig 4.

True-positive facet fracture-dislocation. Parasagittal fast spin-echo T2 image shows a C6 facet fracture (arrowhead) with C6–7 facet dislocation (arrows), which were confirmed at surgery.
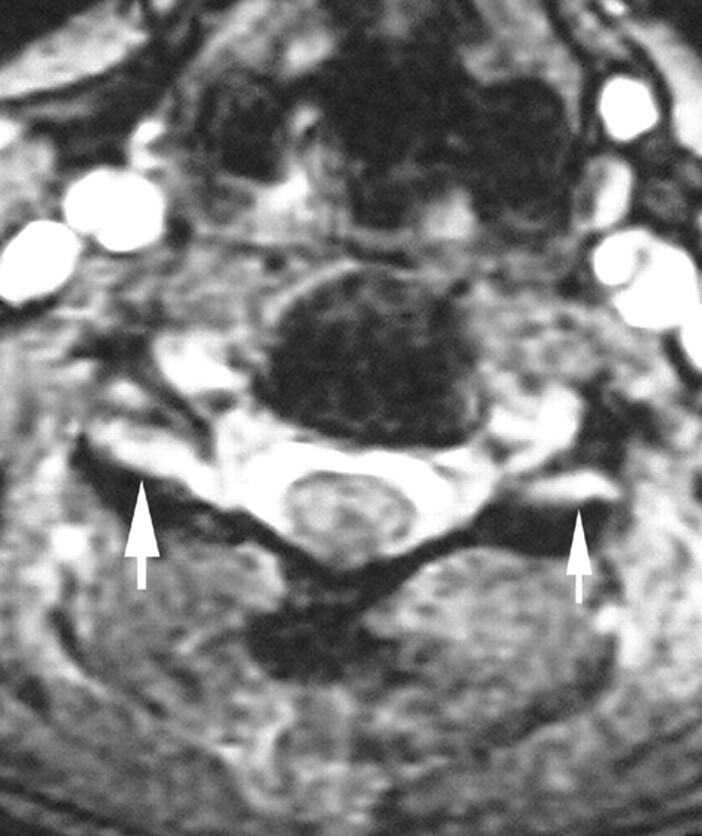
Fig 5.
Axial image of true-positive facet joint injury. Axial fast spin-echo T2-weighted image demonstrates widening of bilateral facet joints, more so on the right. Both facet capsules were injured at surgery.
Fig 6.

False-negative ALL. Sagittal fast spin-echo T2-weighted image demonstrates widening of the intervertebral disk and disruption of the PLL at C5–6, which were confirmed at surgery. The ALL, however, appears intact on the MR imaging but was found injured at surgery.
Fig 7.

False-positive ALL and disk and true-positive PLL injury manifesting as high T2 signal intensity. On this sagittal fast spin-echo T2-weighted image, there is high signal intensity along the PLL (arrow) manifesting as interruption of the normal dark linear PLL at C5–6. At the same level, the ALL appears disrupted and the disk appears widened compared with the level above, especially anteriorly. However, at surgery only the PLL was found injured and the disk and ALL were intact.
Fig 8.

True-positive ligamentum flavum and false-positive interspinous soft tissues. Sagittal STIR image demonstrates disruption of the ligamentum flavum at multiple levels. Injury at the operative level C3–4 (arrow) was confirmed at surgery. On the image, there is also increased T2 signal intensity with stretching of the interspinous ligamentous complex; however, at surgery, this complex was intact.
Fig 9.
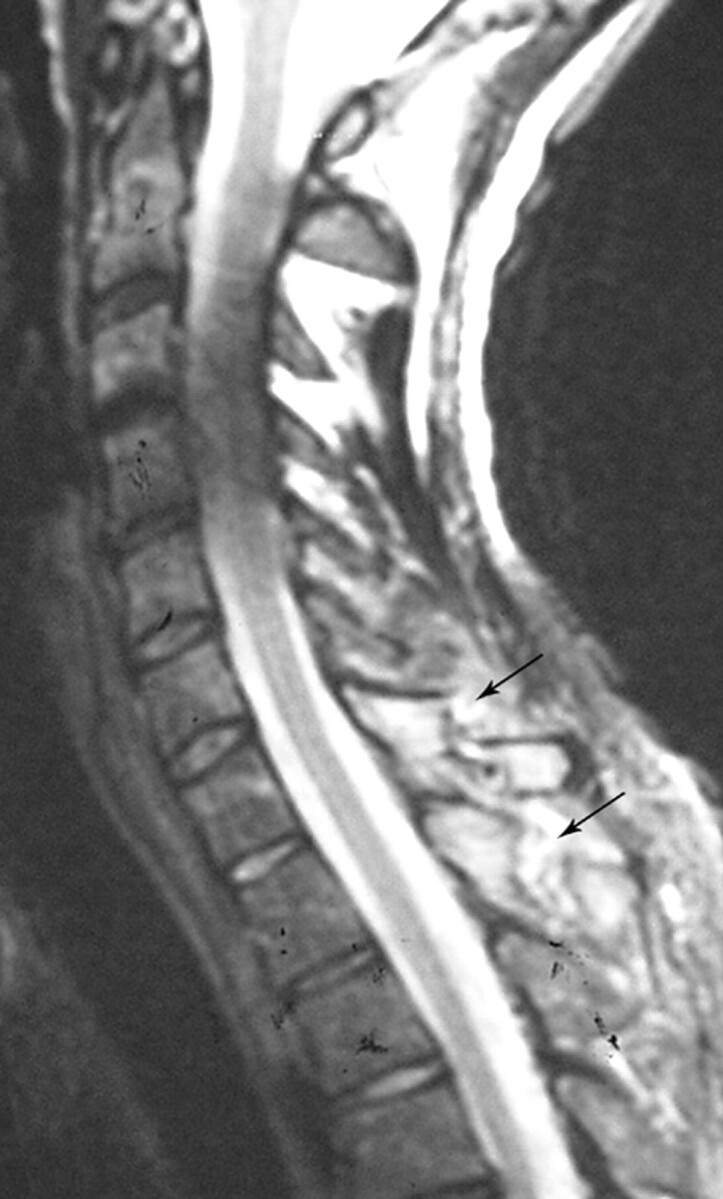
False-negative ligamentum flavum and true-positive interspinous soft tissue injury. Sagittal T2-weighted image shows spinous process fractures of C7 and T1 (arrows). There is increased T2 signal intensity and stretching of the interspinous ligament complex (injury confirmed at surgery). The ligamentum flavum at the level of injury appears intact on the MR imaging but was found to be injured at surgery.
Footnotes
Paper previously presented at: Annual meeting of the American Society of Neuroradiology, May 21–27, 2005; Toronto, Ontario, Canada.
References
- 1.Robertson PA, Ryan MD. Neurological deterioration after reduction of cervical subluxation. Mechanical compression by disc tissue. J Bone Joint Surg Br 1992;74:224–27 [DOI] [PubMed] [Google Scholar]
- 2.Mahale YJ, Silver JR, Henderson NJ. Neurological complications of the reduction of cervical spine dislocations. J Bone Joint Surg Br 1993;75:403–09 [DOI] [PubMed] [Google Scholar]
- 3.Kulkarni MV, McArdle CB, Kopanicky D, et al. Acute spinal cord injury: MR imaging at 1.5 T. Radiology 1987;164:837–43 [DOI] [PubMed] [Google Scholar]
- 4.Flanders AE, Schaefer DM, Doan HT, et al. Acute cervical spine trauma: correlation of MR imaging findings with degree of neurologic deficit. Radiology 1990;177:25–33 [DOI] [PubMed] [Google Scholar]
- 5.Hackney DB, Asato R, Joseph PM, et al. Hemorrhage and edema in acute spinal cord compression: demonstration by MR imaging. Radiology 1986;161:387–90 [DOI] [PubMed] [Google Scholar]
- 6.Schaefer DM, Flanders A, Northrup BE, et al. Magnetic resonance imaging of acute cervical spine trauma. Correlation with severity of neurologic injury. Spine 1989;14:1090–95 [DOI] [PubMed] [Google Scholar]
- 7.Flanders AE, Spettell CM, Tartaglino LM, et al. Forecasting motor recovery after cervical spinal cord injury: value of MR imaging. Radiology 1996;201:649–55 [DOI] [PubMed] [Google Scholar]
- 8.Tehranzadeh J, Kerr R, Amster J. Magnetic resonance imaging of tendon and ligament abnormalities: Part I. Spine and upper extremities. Skeletal Radiol 1992;21:1–9 [DOI] [PubMed] [Google Scholar]
- 9.Hall AJ, Wagle VG, Raycroft J, et al. Magnetic resonance imaging in cervical spine trauma. J Trauma 1993;34:21–26 [DOI] [PubMed] [Google Scholar]
- 10.Davis SJ, Teresi LM, Bradley WG Jr, et al. Cervical spine hyperextension injuries: MR findings. Radiology 1991;180:245–51 [DOI] [PubMed] [Google Scholar]
- 11.el-Khoury GY, Kathol MH, Daniel WW. Imaging of acute injuries of the cervical spine: value of plain radiography, CT, and MR imaging. AJR Am J Roentgenol 1995;164:43–50 [DOI] [PubMed] [Google Scholar]
- 12.Leite CC, Escobar BE, Bazan C 3rd, et al. MRI of cervical facet dislocation. Neuroradiology 1997;39:583–88 [DOI] [PubMed] [Google Scholar]
- 13.Silberstein M, Tress BM, Hennessy O. Prevertebral swelling in cervical spine injury: identification of ligament injury with magnetic resonance imaging. Clin Radiol 1992;46:318–23 [DOI] [PubMed] [Google Scholar]
- 14.Saifuddin A. MRI of acute spinal trauma. Skeletal Radiol 2001;30:237–46 [DOI] [PubMed] [Google Scholar]
- 15.White P, Seymour R, Powell N. MRI assessment of the pre-vertebral soft tissues in acute cervical spine trauma. Br J Radiol 1999;72:818–23 [DOI] [PubMed] [Google Scholar]
- 16.Benzel EC, Hart BL, Ball PA, et al. Magnetic resonance imaging for the evaluation of patients with occult cervical spine injury. J Neurosurg 1996;85:824–29 [DOI] [PubMed] [Google Scholar]
- 17.Goldberg AL, Rothfus WE, Deeb ZL, et al. The impact of magnetic resonance on the diagnostic evaluation of acute cervicothoracic spinal trauma. Skeletal Radiol 1988;17:89–95 [DOI] [PubMed] [Google Scholar]
- 18.Kihiczak D, Novelline RA, Lawrason JN, et al. Should an MR scan be performed routinely after a normal clearance CT scan in the trauma patient? Experience with 59 cases. Emerg Radiol 2001;8:276–78 [Google Scholar]
- 19.D’Alise MD, Benzel EC, Hart BL. Magnetic resonance imaging evaluation of the cervical spine in the comatose or obtunded trauma patient. J Neurosurg 1999;91:54–59 [DOI] [PubMed] [Google Scholar]
- 20.Geck MJ, Yoo S, Wang JC. Assessment of cervical ligamentous injury in trauma patients using MRI. J Spinal Disord 2001;14:371–77 [DOI] [PubMed] [Google Scholar]
- 21.Albrecht RM, Kingsley D, Schermer CR, et al. Evaluation of cervical spine in intensive care patients following blunt trauma. World J Surg 2001;25:1089–96 [DOI] [PubMed] [Google Scholar]
- 22.Klein GR, Vaccaro AR, Albert TJ, et al. Efficacy of magnetic resonance imaging in the evaluation of posterior cervical spine fractures. Spine 1999;24:771–74 [DOI] [PubMed] [Google Scholar]
- 23.Tarr RW, Drolshagen LF, Kerner TC. MR imaging of recent spinal trauma. J Comput Assist Tomogr 1987;11:412–17 [DOI] [PubMed] [Google Scholar]
- 24.Katzberg RW, Benedetti PF, Drake CM, et al. Acute cervical spine injuries: prospective MR imaging assessment at a level 1 trauma center. Radiology 1999;213:203–12 [DOI] [PubMed] [Google Scholar]
- 25.Mirvis SE, Geisler FH, Jelinek JJ, et al. Acute cervical spine trauma: evaluation with 1.5-T MR imaging. Radiology 1988;166:807–16 [DOI] [PubMed] [Google Scholar]
- 26.Orrison WW Jr, Benzd EC, Willis BK, et al. Magnetic resonance imaging evaluation of acute spine trauma. Emerg Radiol 1995;2:120–28 [Google Scholar]
- 27.Vaccaro AR, Kreidl KO, Pan W, et al. Usefulness of MRI in isolated upper cervical spine fractures in adults. J Spinal Disord 1998;11:289–93 [DOI] [PubMed] [Google Scholar]
- 28.Levitt MA, Flanders AE. Diagnostic capabilities of magnetic resonance imaging and computed tomography in acute cervical spinal column injury. Am J Emerg Med 1991;9:131–35 [DOI] [PubMed] [Google Scholar]
- 29.Keiper MD, Zimmerman RA, Bilaniuk LT. MRI in the assessment of the supportive soft tissues of the cervical spine in acute trauma in children. Neuroradiology 1998;40:359–63 [DOI] [PubMed] [Google Scholar]
- 30.Kliewer MA, Gray L, Paver J, et al. Acute spinal ligament disruption: MR imaging with anatomic correlation. J Magn Reson Imaging 1993;3:855–61 [DOI] [PubMed] [Google Scholar]
- 31.Warner J, Shanmuganathan K, Mirvis SE, et al. Magnetic resonance imaging of ligamentous injury of the cervical spine. Emerg Radiol 1996;3:9–15 [Google Scholar]
- 32.Emery SE, Pathria MN, Wilber RG, et al. Magnetic resonance imaging of posttraumatic spinal ligament injury. J Spinal Disord 1989;2:229–33 [PubMed] [Google Scholar]
- 33.Terk MR, Hume-Neal M, Fraipont M, et al. Injury of the posterior ligament complex in patients with acute spinal trauma: evaluation by MR imaging. AJR Am J Roentgenol 1997;168:1481–86 [DOI] [PubMed] [Google Scholar]
- 34.Frank JB, Lim CK, Flynn JM, et al. The efficacy of magnetic resonance imaging in pediatric cervical spine clearance. Spine 2002;27:1176–79 [DOI] [PubMed] [Google Scholar]
- 35.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159–74 [PubMed] [Google Scholar]
- 36.Brennan P, Silman A. Statistical methods for assessing observer variability in clinical measures. BMJ 1992;304:1491–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Maclure M, Willet WC. Misinterpretation and misuse of the kappa statistic. Am J Epidemiol 1987;126:161–69 [DOI] [PubMed] [Google Scholar]
- 38.Hutchinson TP. Focus on psychometrics. Kappa muddles together two sources of disagreement: tetrachoric correlation is preferable. Res Nurs Health 1993;16:313–16 [DOI] [PubMed] [Google Scholar]
- 39.Feinstein AR, Cicchetti DV. High agreement but low kappa: I. The problems of two paradoxes. J Clin Epidemiol 1990;43:543–49 [DOI] [PubMed] [Google Scholar]
- 40.Shrout PE. Measurement reliability and agreement in psychiatry. Stat Methods Med Res 1998;7:301–17 [DOI] [PubMed] [Google Scholar]