Abstract
Objective
To examine the predictive role of social skills in youth with spina bifida (SB) on growth in medical responsibility across development.
Methods
As part of a larger, longitudinal study, 140 youth with SB were assessed across four time points (ages 8–22 across time points). Mixed-effects models were investigated for change with: (a) no predictors (i.e., change in medical responsibility across age; time was examined using the participant’s age, centered at 11.5 years); (b) social variables (i.e., observed social behaviors, parent- and teacher-reported social skills) as predictors; and (c) social variables as predictors with intelligence quotient, lesion level, and sex as covariates.
Results
Significant growth with age was identified for medical responsibility (p < .0001). Observed, parent-reported, and teacher-reported social skills did not significantly predict this growth; however, all three predicted the intercept for medical responsibility at 11.5 years of age (ps ≤ .047). Parent-reported social skills remained a significant predictor of the intercept at 11.5 years of age when including the covariates (p = .008).
Conclusions
Children with SB who exhibited more positive social skills were more likely to a have higher level of medical responsibility in late childhood, but higher levels of social skills were not associated with a more rapid increase in responsibility over time. Identifying existing social strengths and promoting the practice of prosocial skills may have additional benefits to children with SB, including their acquisition of medical responsibility.
Keywords: adherence/self-management, longitudinal research, social skills, spina bifida
Introduction
Spina bifida (SB) is the most common congenital birth defect impacting the central nervous system (Copp et al., 2015). SB is associated with highly variable motor, cognitive, and social functioning difficulties (Dennis et al., 2006), with symptom profiles that overlap with pediatric chronic conditions, physical disabilities, and intellectual disabilities (Stiles-Shields et al., 2019a). Self-management of this complex medical regimen is an important issue for people with SB. Indeed, lower engagement in self-management behaviors can lead to premature mortality in SB, and is often related to preventable complications (e.g., pressure sores, urinary tract infections; Dicianno & Wilson, 2010). As such, the stakes for understanding and improving the mechanisms supporting self-management are critical for youth with SB.
One mechanism of self-management is responsibility-sharing for medically related tasks (Modi et al., 2012). Specifically, responsibility-sharing refers to who (i.e., parent, child, or both) manages medical tasks (e.g., catheterization, bowel program). Parenting practices can foster autonomy (Devine et al., 2011) or relate to decreased levels of decision-making autonomy for youth with SB (in the cases of overprotectiveness or intrusiveness; Holmbeck et al., 2003). Although there are noted discrepancies between parent and child reports of youth responsibility for self-management tasks, youth with SB have demonstrated an increase in medical responsibility over time (Psihogios et al., 2015). However, it is worth noting that what is an ideal or normative timeline for the acquisition of medical responsibility may vary and depend on the social context, including cultural norms (Johnson et al., 2013; Ohanian et al., 2018).
Although youth are expected to take on increasing responsibility for their medical self-management, they must be practicing and growing in other domains of development as well. For example, the development and mastery of social skills are considered necessary for youth as they grow. Indeed, as youth with SB age, they must interact with an expanding social environment (e.g., friends, health care providers; Betz et al., 2015) to effectively self-manage the complex daily and medical needs associated with SB. The development and use of social skills, such as demonstrating positive affect (e.g., smiling, laughing), engaging in prosocial skills (e.g., empathy, asking questions, and/or making appropriate eye contact), or using assertive communication skills (Holbein et al., 2014), may facilitate such interactions. Although delays and vulnerabilities have been noted across multiple samples of youth with SB in the development of social skills (Devine et al., 2012; Holbein et al., 2015; Landry et al., 2013; Wallander et al., 1989), abilities akin to their typically developing peers have also been noted across development with regard to friendships (Stiles-Shields et al., 2019b). These findings are consistent with previous research indicating a delay, but eventual attainment of most milestones in youth with SB (Zukerman et al., 2011).
Social deficits in youth with SB have been cited as negatively impacting responsibility (Psihogios & Holmbeck, 2013); however, the potential benefits of harnessing existing social skill strengths have been overlooked (Dryburgh et al., 2020). Medical self-management has been associated with social support in youth with SB (Psihogios et al., 2017) and other pediatric chronic conditions (Gallant, 2003; Helms et al., 2015; La Greca et al., 2002). As social skills bolster social support (Sarason et al., 1985), it is likely that these skills are related to self-management practices. Indeed, the use of positive social skills requires specific attentional and executive functioning skills (Holbein et al., 2017; Wolfe et al., 2013), which have also been associated with medical responsibility in youth with SB (Psihogios et al., 2017). The development and use of social skills in youth with SB may therefore indicate increased cognitive capacities that could extend to medical responsibility growth. For example, communication strategies (e.g., asking questions, making assertive statements) may increase the likelihood that communication around independence with medical responsibility occurs or increases within the family–or that youth with SB are able to communicate more effectively with medical providers about their medical regimen. To date, the majority of research examining the role of social skills in pediatric self-management, such as responsibility-sharing for medically related tasks, has been conducted cross-sectionally rather than longitudinally, thereby limiting conclusions regarding this relationship.
The purpose of this study was therefore to utilize a multimethod and multi-informant approach to examine whether the social skills of youth with SB predict growth in medical responsibility across development. Previous research with the same longitudinal sample has indicated growth in medical responsibility across two time points (Psihogios et al., 2015). This study extends this research by examining changes in medical responsibility across four time points and within the context of how late childhood social skills may be associated with such changes. We hypothesized that: (a) consistent with previous findings indicating growth in medical responsibility across two time points (Psihogios et al., 2015), youth with SB would continue to demonstrate growth in medical responsibility across development, and (b) positive social skills demonstrated during late childhood by youth with SB during an observed interaction with a close friend and in their daily living (i.e., parent and teacher report) would significantly predict growth in medical responsibility.
Methods
Participants
Participants were recruited for an ongoing, longitudinal program of research examining the neurocognitive, family, and social development of children with SB (e.g., Psihogios et al., 2015). Participants were eligible for inclusion if they: (a) had a diagnosis of SB; (b) were 8–15 years old; (c) resided within 300 miles of Chicago; (d) did not have comorbid medical or psychiatric conditions; and (e) were able to speak and read English or Spanish. At Time one (T1), participants with SB were asked to invite a peer “best friend” to join them for part of their home visit assessment to complete several videotaped tasks (see the Procedure and Measures sections for more details). Peers were eligible for inclusion if they: (a) were 6–17 years old at T1 (i.e., ± 2 years from the participant age range); and (b) were able to speak and read English or Spanish. At T1 (ages 8–15), 140 participants with SB and 120 chosen peers were recruited (20 did not have a peer participate who met all inclusion criteria at T1; Devine et al., 2012). At Time two (T2; ages 10–17), Time three (T3; ages 12–19), and Time four (T4; ages 15–21), 110, 104, and 94 participants with SB participated, respectively.
Procedure
This study was approved by the university and hospital Institutional Review Boards. Time points (i.e., T1–T4) occurred approximately two years apart. At T1, data were collected across two in-home assessment sessions conducted by two trained research assistants. At T2, T3, and T4, data were collected during single in-home assessment sessions. Informed child assent and parental consent were obtained prior to all data collection. Parents also signed release forms to allow access to medical charts and teachers for data collection. For peer participation, informed child assent was obtained in person during the home visit, and parental consent was obtained in person or via mail prior to the in-home assessment session involving the peer.
This study used parent- and teacher-reported questionnaire data (T1–T4) and observational data of peer interaction tasks (T1). During the first in-home assessment session, children with SB and their parents were first provided with the peer inclusion criteria (see Participants section), and then asked to invite the child’s “closest” friend meeting these criteria to the next in-home assessment session. Parents were also asked to contact the peer’s parent(s) to obtain consent for research staff to contact the family of the peer with more information. During the second in-home assessment session, a video recording was made as the child and peer completed structured interview tasks and an observed interaction together. Mothers and fathers completed questionnaires separately. Families, teachers, and the peers were compensated for their time at alltime points with gifts (e.g., reusable water bottle) and monetary compensation ($150 for families and $50 for peers).
Measures
Demographics and SB Characteristics
Parents of the children with SB completed a questionnaire detailing the child’s demographic information (e.g., age, race/ethnicity, etc.). SB characteristics (e.g., type of SB, lesion level) were reported by parents and confirmed with medical chart review. Full scale intelligence quotient (IQ) was determined at T1 for each participant based on their performance on subtests of the Weschler-Abbreviated Scale of Intelligence (Zhu, 1999).
Medical Responsibility
The Sharing of SB Management Responsibilities (SOSBMR) was adapted from the Diabetes Family Responsibility Questionnaire (Anderson et al., 1990) and was developed specifically for youth with SB. Mothers, fathers, and youth with SB completed the SOSBMR independently across T1–4, with the exception that parents no longer completed questionnaires if their child was 18 years old or older (i.e., youth who were 18+ completed a young adult assessment battery). The SOSBMR consists of 34 items that describe SB-related responsibilities relevant to youth (e.g., youth report version: “Who has responsibility for protecting my skin from temperature, textures, and injury?”). Youth with SB, mothers, and fathers each rated tasks on a 3-point Likert scale as to who completes self-management tasks [i.e., 1 = Parent, 2 = Shared, 3 = Youth with SB, 4 = Not applicable (N/A]) participants were instructed to check the N/A box if the task was not part of their SB-related care]. Higher total scores indicate greater youth responsibility for self-management tasks. N/A responses were excluded from total score calculations. The SOSBMR has demonstrated adequate internal consistency and concurrent validity in youth and young adults with SB from the same data set (Psihogios et al., 2015; Smith & Holmbeck, Under Review). Smith and Holmbeck (Under Review) found that the one-factor solution (all 34 items loading on a single SOSBMR factor) had adequate fit and was moderately associated with other measures of medical autonomy (e.g., mastery of medical skills), thus demonstrating satisfactory concurrent and predictive validity. The reliability coefficients for the SOSBMR composite variable showed acceptable reliability (α = .90) and adequate to acceptable reliability for each reporter (mother report = .95, father report = .68, and self-report = .93).
Observations of Behavior
The children with SB and their peers completed video-taped interactions during the home visit (T1). The pair completed four-structured tasks, with the order randomized: (a) a toy-ranking activity, (b) discussion of an unfamiliar object, (c) discussion and planning of an adventure, and (d) discussion of social conflicts.
The Peer Interaction Macro-coding System (PIMS) was used to code the peer interactions for observed social behaviors (Holbein et al., 2014). Although the PIMS is comprised of four scales: control (two items), prosocial skills (six items), positive affect (six items), and conflict (five items), this study’s focus on social strengths resulted in the use of only the prosocial skills and positive affect subscales. Higher scores indicate the presence of more social behaviors related to each domain (e.g., prosocial skills). Each videotaped interaction was coded by two separate coders, including trained undergraduate and graduate students. To assess inter-rater reliability, intraclass reliability correlations (ICCs) were computed for children with SB and their peers for each scale; all ICCs were adequate (as defined as .60 or greater; Kieffer et al., 2004). Both the prosocial skills and positive affect subscales had acceptable scale reliability (αs > .80).
Parent- and Teacher-Reported Social Skills
The Social Skills Rating System (SSRS) is a standardized, norm-referenced instrument that assesses behaviors that are considered essential to social competence and adaptive functioning (Gresham & Elliott, 1990). Parents and teachers of youth with SB were administered the parent (38 items) and teacher (34 items) forms of the SSRS, respectively, at Time 1. Each item asks respondents to rate how often a child demonstrates a social skill and how important the skill is to the child’s development. Teachers and parents were asked to rate how often the child engages in the behavior on a Likert Scale (“0 = never” to “2 = very often”). Higher total and subscale scores indicate better social skills. Subscales fall into the domains of social skills and problematic behaviors; however, only the social skills subscales were used in the larger, longitudinal study since problem behaviors are assessed using other questionnaires. Consistent with previous uses of the SSRS in samples with SB (e.g., Holbein et al., 2017), raw scores were used to allow for greater variability. Both the parent and teacher report on the SSRS demonstrated acceptable reliability (as > .60).
Data Analysis
To reduce the risk of shared method variance through multiple analyses, composite scores were created by averaging across raters (Holmbeck et al., 2002). Consistent with previous composite scores created for longitudinal analyses of this sample of youth with SB (Stern et al., 2018), composites were created when there was adequate: (a) associations between two reporters and/or measures (r ≥ .40), or (b) internal consistency among three or more reporters (α > .60). Specifically, the following composite variables were created: (a) observed social skills (i.e., PIMS subscales of Prosocial Skills and Positive Affect; r > .55); (b) parent-reported social skills (i.e., mother and father report on the SSRS; r > .56); and (c) Medical Responsibility (i.e., child, mother, and father report on the SOSBMR, α > .60). Although discrepancies in mother and child report of medical autonomy in SB have previously been noted in earlier waves of this longitudinal data set (Psihogios & Holmbeck, 2013), the composite variable was utilized for the outcome variable because: (a) the appropriate level of internal consistency was reached for the three types of reporters, and (b) use of this composite variable promotes the inclusion of data on young adults with SB (parents no longer completed questionnaires at assessments where youth were 18 years of age or older). All available reporters at each time point were used to create the composite variables (e.g., for a given family, if only a mother and child report occurred at T2, the composite of their reports was used), which were created by averaging across reporters. Additionally, confirmatory factor analyses (CFAs) were run to examine the one-factor fit of each of the composite variables detailed above. Fit indices included the comparative fix index (CFI; ideal study criterion ≥ 0.95) and root mean square error of approximation (RMSEA; ideal study criterion ≤ 0.05; Hu & Bentler, 1999; Kline, 2011). For each composite variable, the one-factor CFA resulted in excellent fit: (a) observed social skills composite: RMSEA = 0.01, CFI = 0.98, free parameters = 6; (b) parent-report social skills composite: RMSEA < 0.01, CFI = 0.96, free parameters = 9; and (c) SOSBMR composite: RMSEA < 0.01, CFI = 1.00, free parameters = 9).
Analyses were conducted in SAS using PROC MIXED and the restricted maximum likelihood (REML) estimate. REML uses the sample estimate of the population mean to incorporate uncertainty in the estimation of fixed effects (Kwok et al., 2008; Raudenbush & Bryk, 2002). REML treats fixed effects as sample-based estimates, which provides less biased estimates of variance. Social predictors of changes in the Medical Responsibility outcome variable (i.e., child, mother, and father SOSBMR composite) across time were examined using the participant’s age as the predictor variable within mixed-effects models (SAS Institute Inc., n.d.). Age was selected as the means to define time to provide more insight into medical responsibility growth across development, as opposed to the arbitrary time points of the study assessment schedule (Stiles-Shields et al., 2019b). Age spanned 8–22 years of age for youth with SB (which included the age ranges of participants from T1 to T4). For the analyses, age was centered at 11.5 [the mean of the ages of youth with SB at T1; the mean was selected as opposed to the lowest age (8) so as to avoid potential “floor effects” associated with a child that young not being expected to take on a significant amount of independent care]. The mixed-effects models used were individual change models that allowed for linear change and also allowed for fixed and random effects for the individual intercepts and slopes across age. Each participant contributed up to four time points to the analysis (i.e., T1–4). Consistent with our aims, we investigated models of change with: (a) no predictors (indicating change in medical responsibility across age); (b) social variables (i.e., observed social behaviors, parent- and teacher-reported social skills) as predictors; and (c) to best interpret our findings in light of factors specific to youth with SB, we ran any significant models with IQ, lesion level, and sex as covariates. We included sex as a covariate, as males with SB have demonstrated significant differences in their prosocial development compared with peers and females with SB in this sample (Stiles-Shields et al., 2019b). In all analyses, p-values < .05 were considered statistically significant.
Results
Social Skills Predicting Growth in Medical Responsibility
Table I displays the sample demographic, social, and SB characteristics; Table II displays the results for social skills variables predicting growth in medical responsibility across age. The growth model examining medical responsibility across development indicated significant growth with age [Change in slope (△ m) = 0.083; p < .0001]. Observed Social Skills (i.e., PIMS subscales of Prosocial Skills and Positive Affect; △ m = 0.021; p = .190), parent-reported social skills (mother and father report of the SSRS; △ m = −0.012; p = .581), and teacher-reported social skills on the SSRS (△ m = 0.017; p = .282) did not significantly predict medical responsibility growth across age. However, observed social skills (b = 0.262; p = .003), parent-reported social skills (b = 0.372; p = .0008), and teacher-reported social skills on the SSRS (b = 0.181; p = .047) did significantly predict the intercept for medical responsibility at age 11.5 years old. Specifically, across all models, better social skills at Time 1 predicted a higher intercept for responsibility. To better understand the significant predictive role of the Observed Social Skills variable, the individual subscales that comprise this variable were also run as individual predictors. Neither Prosocial Skills (△ m = 0.016; p = .241) nor Positive Affect (△ m = 0.019; p = .207) significantly predicted growth in medical responsibility across age. However, Prosocial Skills significantly predicted the intercept for responsibility at age 11.5 years old (b = 0.290; p < .0001).
Table I.
Demographic, Condition-Specific, and Psychosocial Characteristics Included in Analyses
| Demographics | T1 | T2 | T3 | T4 |
|---|---|---|---|---|
| Age, M (SD) | 11.43 (2.46) | 13.37 (2.43) | 15.36 (2.43) | 17.57 (2.35) |
| Sex | ||||
| Male | 64 (45.7%) | — | — | — |
| Female | 76 (54.3%) | — | — | — |
| Race/ethnicity | ||||
| Caucasian | 78 (55.7%) | — | — | — |
| Hispanic | 34 (24.3%) | — | — | — |
| African American | 21 (15.0%) | — | — | — |
| Other | 7 (5.0%) | — | — | — |
| SB type | ||||
| Myelomeningocele | 122 (87.1%) | — | — | — |
| Other | 29 (13.6%) | — | — | — |
| Lesion level | ||||
| Thoracic | 23 (16.4%) | — | — | — |
| Lumbar | 69 (49.3%) | — | — | — |
| Sacral | 41 (29.3%) | — | — | — |
| Unknown/not reported | 7 (5.0%) | — | — | — |
| Shunt status: present | 109 (77.9%) | — | — | — |
| FSIQ, M (SD) | 85.7 (19.7) | — | — | — |
| SOSBMR, M (SD) | ||||
| Youth | 1.97 (.44) | 2.13 (.41) | 2.33 (.37) | 2.44 (.43) |
| Mother | 1.76 (.41) | 1.96 (.44) | 2.07 (.43) | 2.19 (.37) |
| Father | 1.69 (.42) | 1.86 (.47) | 2.02 (.42) | 2.10 (.39) |
| PIMS prosocial skills, M (SD; range) | 3.26 (.40; 2.03-4.07) | — | — | — |
| PIMS positive affect, M (SD; range) | 3.65 (.35; 2.66-4.49) | — | — | — |
| SSRS, M (SD; range) | ||||
| Mother | 1.29 (.30; .43-1.97) | — | — | — |
| Father | 1.27 (.30; .50-1.92) | — | — | — |
| Teacher | 1.31 (.35; 0-2.00) | — | — | — |
Note. Spina bifida characteristics defined by the medical chart. In the case of missing data, mother report of characteristics was used. One participant did not have characteristics reported by the medical chart or mother. SB = spina bifida; M = mean; SD = standard deviation; T1 = Time 1; T2 = Time 2; T3 = Time 3; T4 = Time 4; FSIQ = Full Scale Intelligence Quotient; SOSBMR = Sharing of Spina Bifida Management Responsibilities; PIMS = Peer Interaction Macro-coding System; SSRS = Social Skills Rating System.
Table II.
Social Skills as Predictors of Growth in Medical Responsibility Among Youth with Spina Bifida
| Observed social skills composite |
Observed prosocial skills |
Observed positive affect |
Parent-reported social skills |
Teacher-reported social skills |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Estimate (SE) | CI | Estimate (SE) | CI | Estimate (SE) | CI | Estimate (SE) | CI | Estimate (SE) | CI | |
| Growth models without covariates | ||||||||||
| Intercept | 0.262** (0.087) | 0.090–0.434 | 0.290*** (0.071) | 0.151–0.429 | 0.094 (0.084) | −0.073 to 0.260 | 0.372*** (0.108) | 0.159–0.585 | 0.181* (0.090) | 0.002–0.360 |
| Slope | 0.021 (0.016) | −0.011–0.053 | 0.016 (0.014) | −0.011 to 0.043 | 0.019 (0.015) | −0.011 to 0.050 | −0.012 (0.021) | −0.054 to 0.031 | 0.017 (0.016) | −0.015 to 0.049 |
| Growth models with IQ, lesion level, and sex included as covariates | ||||||||||
| Intercept | 0.100 (0.084) | −0.067 to 0.267 | 0.135 (0.072) | −0.009 to 0.279 | 0.018 (0.076) | −0.132 to 0.168 | 0.261* (0.100) | 0.063–0.458 | −0.001 (0.080) | −0.159 to 0.158 |
| Slope | 0.020 (0.016) | −0.012 to 0.051 | 0.014 (0.014) | −0.013 to 0.041 | 0.018 (0.015) | −0.011 to 0.048 | −0.021 (0.021) | −0.063 to 0.022 | 0.008 (0.016) | −0.024 to 0.040 |
Note. Table results present coefficients from growth models. The slope rows indicate the change in slope across age for each 1-unit change in social skills. IQ = intelligence quotient. CI = confidence interval.
p < .05,
p ≤ .01, and
p ≤ .001.
Predictions of Growth Adjusting for IQ, Lesion Level, and Sex
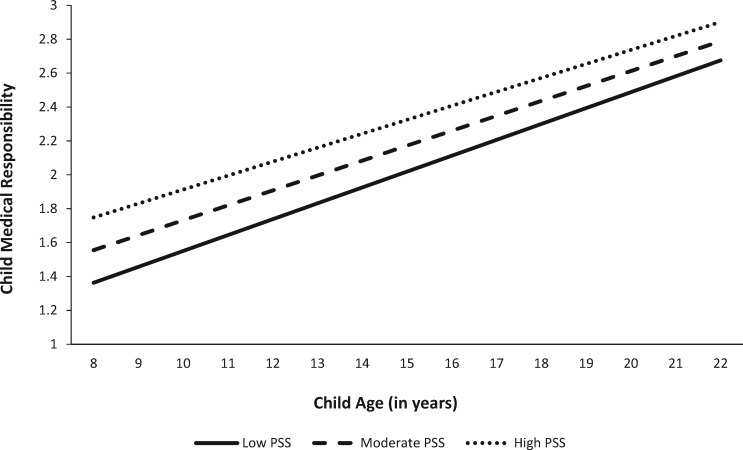
In running the models with IQ, lesion level, and sex included as covariates, none of the social skills variables significantly predicted medical responsibility growth. However, parent-reported social skills remained a significant predictor of the intercept for responsibility at age 11.5 years old (b = 0.268; p = .008; see Table II and Figure 1).
Figure 1.
Parent-reported social skills predicting change in medical responsibility across age in youth with SB. Note. Low PSS = parent-reported social skills that are one standard deviation below the sample mean. Moderate PSS = parent-reported social skills at the mean. High PSS = parent-reported social skills that are one standard deviation above the sample mean.
Discussion
This study utilized a multimethod and multi-informant approach to explore the predictive role of social skills in medical responsibility growth for youth with SB. Consistent with our hypothesis and previous findings with earlier waves of this sample (Psihogios et al., 2015), youth with SB demonstrated significant growth in their medical responsibility across development. However, our hypothesis that observed and reported social skills in youth with SB would significantly predict growth in medical responsibility was only partially supported. Indeed, social skills did not predict growth across development, but did predict the intercept of the responsibility variable at 11.5 years of age (i.e., the start of “time” by age for the growth models). This finding suggests that children with SB who exhibited more positive social skills were more likely to have higher responsibility in late childhood, but that higher levels of social skills were not associated with a steeper increase in responsibility over time. Additionally, controlling for lesion level, IQ, and sex dampened the predictive role of teacher-reported and observed social skills for the level of medical responsibility during late childhood. Yet, the predictive relationship for the responsibility starting point at 11.5 years of age remained significant for parent-reported social skills with and without the covariates, suggesting that parents may not link intelligence, sex, and/or disability status to social skills as other observers might.
Social challenges are frequently highlighted for youth with SB compared with their typically developing peers. Specifically, neuropsychological (e.g., attention difficulties, language issues such as “cocktail party syndrome”; Tew, 1979) and psychosocial differences (e.g., less after-school interactions with peers; Holmbeck et al., 2003) have been implicated in limiting social skill development in youth with SB. However, the current findings highlight that positive social skills are observed in children with SB. Further, social skills significantly predicted youth’s medical responsibility in late childhood, indicating that children with SB who have developed their social skills are more likely to assume responsibility for their medical self-management at an early age. As a result, these children have more time to practice and master self-management skills under the supervision of their parents as they develop across adolescence.
Parental report of social skills was found to be a particularly important predictor, as it was significantly associated with the level of medical responsibility in late childhood for the sample, even beyond the effects of IQ, lesion level, and sex. Although our hypotheses did not single out parent report as a significant predictor above and beyond the other variables, this finding is also not surprising. Indeed, parents have the opportunity to view their children’s social skill development across different environments and potentially in comparison to siblings or other related peers (e.g., cousins; Krivitzky et al., 2016). Although teachers may also compare children with SB to their peers, they are typically not evaluating social skills in other environments (i.e., outside of school) and domains (e.g., self-management). Parents are also likely to have communicated with their children about a variety of topics, including plans for assuming more responsibility for SB-related medical regimen tasks. How a child with SB responds to such conversations may impact parental willingness to increase their child’s level of responsibility. For example, if a child demonstrates prosocial skill use during conversations about medical tasks (e.g., asking questions, taking on the perspective of their parent or medical provider about medical management), the parent(s) might be more willing and likely to increase that child’s level of responsibility for their own care. This finding highlights the potential benefit of providers asking parents about their children’s social skill development, as these skills may be applied to other domains relevant to self-management. Indeed, noting vulnerabilities that the parent has observed in their child (e.g., less likely to use prosocial skills in daily interactions) may promote earlier identification of youth with SB who may benefit from social or other skills training (Holbein et al., 2014). Conversely, identifying potential strengths that the parent has noted in their child socially may provide clinicians with the opportunity to highlight ways parents can provide scaffolding to apply such skills towards self-management and medical responsibility in children with SB (Winning et al., 2020).
These findings also highlight specific targets for social skills training in children with SB. Observations of positive social behaviors that predicted the amount of responsibility that children with SB assumed for their own self-management tasks appeared to be driven by prosocial skills, as opposed to higher levels of positive affect (e.g., smiling, laughing; Holbein et al., 2014). Prosocial skills are behaviors that can lead to positive social outcomes—examples include decision-making skills, empathy, asking questions, and/or making appropriate eye contact (Caldarella & Merrell, 1997). As with all skills, prosocial skills may be taught and rehearsed in real life environments. Increasing opportunities for learning and practicing prosocial skills at home and school and during play may extend skills development to other domains important for youth with SB (e.g., medical responsibility for self-management tasks). This finding may be particularly important for specific subgroups of individuals with SB who may benefit from such training. For example, controlling for lesion level, IQ, and sex in the current sample dampened the predictive role of teacher-reported and observed social skills for the level of medical responsibility during late childhood. This suggests that those with more severe profiles would likely benefit from social skills—and potentially other related skills training (e.g., executive functioning; Holbein et al., 2017). Further, males with SB in the current sample have previously been identified as less likely to increase their prosocial skills with age compared with their typically developing peers and counterparts with SB who are female (Stiles-Shields et al., 2019b), implicating that males with SB might be another subgroup to assess for social skills training needs.
This study has a number of strengths, including using a multimethod and multi-informant approach. However, these findings should be interpreted in light of specific limitations. First, by the very nature of their participation and retention in a longitudinal research study, this sample of youth with SB may be unique. For example, these youth may be particularly adept socially and/or responsible (e.g., complying with longitudinal research assessment windows). As such, the level of social skills displayed in late childhood and the growth in responsibility over time might not be predicted in the same way for general clinical and community populations with SB. Second, time as defined by age spanned from 8 to 22. It is unclear how these findings extend to growth in responsibility in young adults with SB, particularly for those who start to live independently later in young adulthood. Third, potential changes in social skills across time were not examined in the current analyses. Future research should explore whether changes in social skills influence changes in growth in responsibility. Fourth, the current analyses were not examined within the context of cultural and/or familial norms for the timing of increased responsibility. Future research should include variables to assess the rate of development for youth with SB within the context of their families’ cultural norms (Johnson et al., 2013; Ohanian et al., 2018). Fifth, while all participants were recruited from the same geographic location, medical clinics and physicians may also communicate differently around medical responsibility. Clinic-level factors should also be considered in future research. Finally, while growth in medical responsibility was examined, it is unclear how these findings translate to effective self-management more broadly. Indeed, an individual with SB may assume responsibility for a self-management task, but might be inconsistent with adherence to the task (potentially placing such an individual in life-threatening circumstances; Dicianno & Wilson, 2010). Future research should examine how social skills may extend to growth in adherence, with trajectories extending into ages associated with independent adult living.
Social skills in youth with SB have often been examined from the lens of a deficit or vulnerability. However, this study lends support to a small, but growing body of literature to suggest that youth with SB possess specific social strengths, even at young ages (Cunningham et al., 2007; Devine et al., 2012; Fussell et al., 2005; Stiles-Shields et al., 2019b). Such social strengths are associated with higher medical responsibility in late childhood, thus permitting the child to practice responsibility for medical tasks under parental supervision for a longer portion of development. As such, identifying existing social strengths and promoting the practice of prosocial skills may provide additional benefits to children with SB, including their responsibility-sharing for medically related tasks.
Acknowledgments
The authors thank the Illinois Spina Bifida Association as well as staff of the Spina Bifida Clinics at Ann & Robert H. Lurie Children’s Hospital of Chicago, Shriners Hospital for Children-Chicago, and Loyola University Medical Center. We also thank the numerous undergraduate and graduate research assistants who helped with data collection and data entry. Finally, we would like to thank the parents, children, and teachers who participated in this study.
Funding
This research was supported in part by grants from the National Institute of Nursing Research and the Office of Behavioral and Social Sciences Research (R01 NR016235), National Institute of Child Health and Human Development (R01 HD048629), and the March of Dimes Birth Defects Foundation (12-FY13-271). This study is part of an ongoing, longitudinal study. Dr C.S.-S was also supported by a fellowship from the Cohn Family Foundation.
Conflicts of interest: None declared.
References
- Anderson B. J., Auslander W. F., Jung K. C., Miller J. P., Santiago J. V. (1990). Assessing family sharing of diabetes responsibilities. Journal of Pediatric Psychology, 15(4), 477–492. [DOI] [PubMed] [Google Scholar]
- Betz C. L., Smith K. A., Macias K., Deavenport-Saman A. (2015). Testing the transition preparation training program: Well-being of relationships outcomes. Journal of Pediatric Rehabilitation Medicine, 8(3), 235–246. [DOI] [PubMed] [Google Scholar]
- Caldarella P., Merrell K. W. (1997). Common dimensions of social skills of children and adolescents: A taxonomy of positive behaviors. School Psychology Review, 26(2), 264–278. [Google Scholar]
- Copp A. J., Adzick N. S., Chitty L. S., Fletcher J. M., Holmbeck G. N., Shaw G. M. (2015). Spina bifida. Nature Reviews Disease Primers, 1(1), 15007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham S. D., Thomas P. D., Warschausky S. (2007). Gender differences in peer relations of children with neurodevelopmental conditions. Rehabilitation Psychology, 52(3), 331–337. [Google Scholar]
- Dennis M., Landry S. H., Barnes M., Fletcher J. M. (2006). A model of neurocognitive function in spina bifida over the life span. Journal of the International Neuropsychological Society, 12(2), 285–296. [DOI] [PubMed] [Google Scholar]
- Devine K. A., Holmbeck G. N., Gayes L., Purnell J. Q. (2012). Friendships of children and adolescents with spina bifida: Social adjustment, social performance, and social skills. Journal of Pediatric Psychology, 37(2), 220–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devine K. A., Wasserman R. M., Gershenson L. S., Holmbeck G. N., Essner B. S. (2011). Mother-adolescent agreement regarding decision-making autonomy: A longitudinal comparison of families of adolescents with and without spina bifida. Journal of Pediatric Psychology, 36(3), 277–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dicianno B. E., Wilson R. (2010). Hospitalizations of adults with spina bifida and congenital spinal cord anomalies. Archives of Physical Medicine and Rehabilitation, 91(4), 529–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dryburgh N. S. J., Khullar T. H., Sandre A., Persram R. J., Bukowski W. M., Dirks M. A. (2020). Evidence base update for measures of social skills and social competence in clinical samples of youth. Journal of Clinical Child and Adolescent Psychology, 49, 573–594. [DOI] [PubMed] [Google Scholar]
- Fussell J. J., Macias M. M., Saylor C. F. (2005). Social skills and behavior problems in children with disabilities with and without siblings. Child Psychiatry and Human Development, 36(2), 227–241. [DOI] [PubMed] [Google Scholar]
- Gallant M. P. (2003). The influence of social support on chronic illness self-management: A review and directions for research. Health Education & Behavior: The Official Publication of the Society for Public Health Education, 30(2), 170–195. [DOI] [PubMed] [Google Scholar]
- Gresham F. M., Elliott S. N. (1990). Social skills rating system: Manual. American Guidance Service. [Google Scholar]
- Helms S. W., Dellon E. P., Prinstein M. J. (2015). Friendship quality and health-related outcomes among adolescents with cystic fibrosis. Journal of Pediatric Psychology, 40(3), 349–358. [DOI] [PubMed] [Google Scholar]
- Holbein C. E., Lennon J. M., Kolbuck V. D., Zebracki K., Roache C. R., Holmbeck G. N. (2015). Observed differences in social behaviors exhibited in peer interactions between youth with spina bifida and their peers: Neuropsychological correlates. Journal of Pediatric Psychology, 40(3), 320–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holbein C. E., Peugh J. L., Holmbeck G. N. (2017). Social skills in youth with spina bifida: A longitudinal multimethod investigation comparing biopsychosocial predictors. Journal of Pediatric Psychology, 42(10), 1133–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holbein C. E., Zebracki K., Holmbeck G. N. (2014). Development and validation of the Peer Interaction Macro-Coding System Scales (PIMS): A new tool for observational measurement of social competence in youth with spina bifida. Psychological Assessment, 26(4), 1235–1246. 10.1037/a0037062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmbeck G. N., Li S. T., Schurman J. V., Friedman D., Coakley R. M. (2002). Collecting and managing multisource and multimethod data in studies of pediatric populations. Journal of Pediatric Psychology, 27(1), 5–18. [DOI] [PubMed] [Google Scholar]
- Holmbeck G. N., Westhoven V. C., Phillips W. S., Bowers R., Gruse C., Nikolopoulos T., Totura C. M., Davison K. (2003). A multimethod, multi-informant, and multidimensional perspective on psychosocial adjustment in preadolescents with spina bifida. Journal of Consulting and Clinical Psychology, 71(4), 782–796. [DOI] [PubMed] [Google Scholar]
- Hu L., Bentler P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. [Google Scholar]
- Johnson L., Radesky J., Zuckerman B. (2013). Cross-cultural parenting: Reflections on autonomy and interdependence. Pediatrics, 131(4), 631–633. [DOI] [PubMed] [Google Scholar]
- Kieffer K. M., Cronin C., Fister M. C. (2004). Exploring variability and sources of measurement error in alcohol expectancy questionnaire reliability coefficients: A meta-analytic reliability generalization study. Journal of Studies on Alcohol, 65(5), 663–671. [DOI] [PubMed] [Google Scholar]
- Kline R. B. (2011). Principles and practice of structural equation modeling. Guilford. [Google Scholar]
- Krivitzky L. S., Walsh K. S., Fisher E. L., Berl M. M. (2016). Executive functioning profiles from the BRIEF across pediatric medical disorders: Age and diagnosis factors. Child Neuropsychology, 22(7), 870–888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwok O. M.Underhill A. T.Berry J. W.Luo W.Elliott T. R., & Yoon M. (2008). Analyzing longitudinal data with multilevel models: an example with individuals living with lower extremity intra-articular fractures. Rehabilitation psychology, 53(3), 370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Greca A. M., Bearman K. J., Moore H. (2002). Peer relations of youth with pediatric conditions and health risks: Promoting social support and healthy lifestyles. Journal of Developmental and Behavioral Pediatrics, 23(4), 271–280. [DOI] [PubMed] [Google Scholar]
- Landry S. H., Taylor H. B., Swank P. R., Barnes M., Juranek J. (2013). Longitudinal mediators of social problem solving in spina bifida and typical development. Rehabilitation Psychology, 58(2), 196–205. [DOI] [PubMed] [Google Scholar]
- Modi A. C., Pai A. L., Hommel K. A., Hood K. K., Cortina S., Hilliard M. E., Guilfoyle S. M., Gray W. N., Drotar D. (2012). Pediatric self-management: A framework for research, practice, and policy. Pediatrics, 129(2), e473–e485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohanian D., Stiles-Shields C., Afzal K., Driscoll C. F. B., Papadakis J. L., Stern A., Starnes M., Holmbeck G. N. (2018). Cultural considerations for autonomy and medical adherence in a young Palestinian-American Muslim female with spina bifida: A longitudinal case study in a research context. Clinical Practice in Pediatric Psychology, 6(4), 386–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Psihogios A. M., Holmbeck G. N. (2013). Discrepancies in mother and child perceptions of spina bifida medical responsibilities during the transition to adolescence: Associations with family conflict and medical adherence. Journal of Pediatric Psychology, 38(8), 859–870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Psihogios A. M., Kolbuck V., Holmbeck G. N. (2015). Condition self-management in pediatric spina bifida: A longitudinal investigation of medical adherence, responsibility-sharing, and independence skills. Journal of Pediatric Psychology, 40(8), 790–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Psihogios A. M., Murray C., Zebracki K., Acevedo L., Holmbeck G. N. (2017). Testing the utility of a Bio-Neuropsychosocial Model for predicting medical adherence and responsibility during early adolescence in youth with spina bifida. Journal of Pediatric Psychology, 42(9), 910–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush S. W., & Bryk A. S. (2002). Hierarchical linear models: Applications and data analysis methods (Vol. 1). Sage [Google Scholar]
- Sarason B. R., Sarason I. G., Hacker T. A., Basham R. B. (1985). Concomitants of social support: Social skills, physical attractiveness, and gender. Journal of Personality and Social Psychology, 49(2), 469–480. [Google Scholar]
- SAS Institute Inc. (n.d). SAS/ACCESS 9.4. SAS Institute Inc.
- Smith Z. R., Holmbeck G. N. (Under Review). Evaluating the factor structure of two medical autonomy scales across time and reporters in youth with spina bifida. Journal of Pediatric Psychology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern A., Driscoll C. F. B., Ohanian D., Holmbeck G. N. (2018). A longitudinal study of depressive symptoms, neuropsychological functioning, and medical responsibility in youth with spina bifida: Examining direct and mediating pathways. Journal of Pediatric Psychology, 43(8), 895–905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stiles-Shields C., Crowe A. N., Driscoll C. F. B., Ohanian D. M., Stern A., Wartman E., Winning A. M., Wafford Q. E., Lattie E. G., Holmbeck G. N. (2019. a). A systematic review of behavioral intervention technologies for youth with chronic health conditions and physical and intellectual disabilities: Implications for adolescents and young adults with spina bifida. Journal of Pediatric Psychology, 44(3), 349–362. 10.1093/jpepsy/jsy097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stiles-Shields C., Driscoll C. F. B., Rausch J. R., Holmbeck G. N. (2019. b). Friendship quality over time in youth with spina bifida compared to peers. Journal of Pediatric Psychology, 44(5), 601–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tew B. (1979). The “cocktail party syndrome” in children with hydrocephalus and spina bifida. International Journal of Language & Communication Disorders, 14(2), 89–101. 10.3109/13682827909011349 [DOI] [PubMed] [Google Scholar]
- Wallander J. L., Feldman W. S., Varni J. W. (1989). Physical status and psychosocial adjustment in children with spina bifida. Journal of Pediatric Psychology, 14(1), 89–102. [DOI] [PubMed] [Google Scholar]
- Winning A. M., Stiles-Shields C., Driscoll C. F. B., Ohanian D. M., Crowe A. N., Holmbeck G. N. (2020). Development of an observational parental scaffolding measure for youth with spina bifida. Journal of Pediatric Psychology, 45(6), 695–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfe K. R., Walsh K. S., Reynolds N. C., Mitchell F., Reddy A. T., Paltin I., Madan-Swain A. (2013). Executive functions and social skills in survivors of pediatric brain tumor. Child Neuropsychology, 19(4), 370–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu J. (1999). WASI Wechsler abbreviated scale of intelligence manual. NCS Pearson. [Google Scholar]
- Zukerman J. M., Devine K. A., Holmbeck G. N. (2011). Adolescent predictors of emerging adulthood milestones in youth with spina bifida. Journal of Pediatric Psychology, 36(3), 265–276. [DOI] [PMC free article] [PubMed] [Google Scholar]