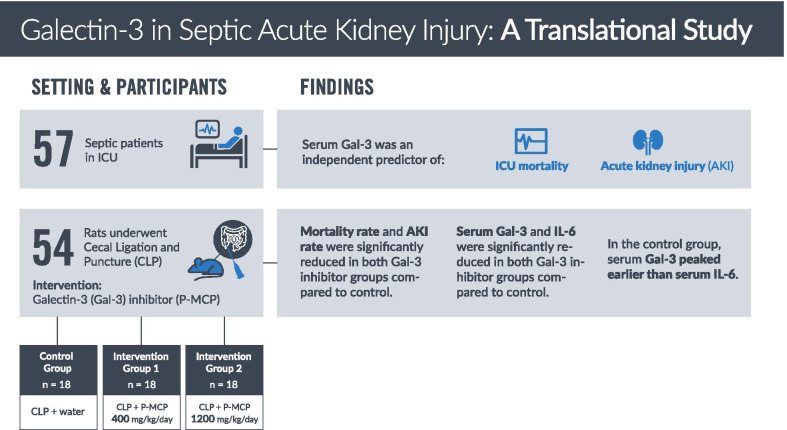
Abstract
Background
Galectin-3 (Gal-3) is a pleiotropic glycan-binding protein shown to be involved in sepsis and acute kidney injury (AKI). However, its role has never been elucidated in sepsis-associated AKI (S-AKI). We aimed to explore Gal-3’s role and its potential utility as a therapeutic target in S-AKI.
Methods
In 57 patients admitted to the intensive care unit (ICU) with sepsis, serum Gal-3 was examined as a predictor of ICU mortality and development of AKI. In a rat model of S-AKI induced by cecal ligation and puncture (CLP), 7-day mortality and serum Gal-3, Interleukin-6 (IL-6), and creatinine were examined at 2, 8, and 24 hours (h) post-CLP. Two experimental groups received the Gal-3 inhibitor modified citrus pectin (P-MCP) at 400 mg/kg/day and 1200 mg/kg/day, while the control group received water only (n = 18 in each group).
Results
Among 57 patients, 27 developed AKI and 8 died in the ICU. Serum Gal-3 was an independent predictor of AKI (OR = 1.2 [95% CI 1.1–1.4], p = 0.01) and ICU mortality (OR = 1.4 [95% CI 1.1–2.2], p = 0.04) before and after controlling for age, AKI, and acute physiology and chronic health evaluation (APACHE II) score. In the CLP rat experiment, serum Gal-3 peaked earlier than IL-6. Serum Gal-3 was significantly lower in both P-MCP groups compared to control at 2 h post-CLP (400 mg: p = 0.003; 1200 mg: p = 0.002), and IL-6 was significantly lower in both P-MCP groups at all time points with a maximum difference at 24 h post-CLP (400 mg: p = 0.015; 1200 mg: p = 0.02). In the Gal-3 inhibitor groups, 7-day mortality was significantly reduced from 61% in the control group to 28% (400 mg P-MCP: p = 0.03) and 22% (1200 mg P-MCP: p = 0.001). Rates of AKI per RIFLE criteria were significantly reduced from 89% in the control group to 44% in both P-MCP groups (400 mg: p = 0.007; 1200 mg: p = 0.007).
Conclusions
This translational study demonstrates the importance of Gal-3 in the pathogenesis of S-AKI, and its potential utility as a therapeutic target.
Graphic abstract
Keywords: Galectin-3, Sepsis, Acute kidney injury
Introduction
Sepsis-associated acute kidney injury (S-AKI) is common among critically ill patients [1–4]. S-AKI is associated with an increased risk of Intensive Care Unit (ICU) or hospital mortality [5, 6]. Further, the individual syndromes of sepsis and AKI each render a patient more vulnerable to the other [7]. Available evidence does not suggest that standard renal replacement therapies improve outcomes beyond control of fluid balance and azotemia [8]. Thus, novel approaches are necessary to prevent and treat S-AKI.
Sepsis and S-AKI result from a dysregulated immune response [9]. Foreign antigens bind to innate immune receptors and subsequently activate inflammasome components, ultimately leading to the elevated release of proinflammatory cytokines both systemically and locally [9]. The resultant cytokine storm is associated with increased levels of Interleukin-6 (IL-6) [10]. Multiple reports indicate that IL-6 is an excellent biomarker of severity and a prognostic indicator in patients with sepsis [11–15]. Findings pertaining to the therapeutic utility of IL-6 inhibition in S-AKI remain mixed [16, 17], suggesting that processes upstream of IL-6 may be responsible for triggering the deleterious effects in sepsis and S-AKI.
Galectin-3 (Gal-3) is a pleiotropic glycan-binding protein involved in numerous physiological and pathological events [18], including those that relate to immune function [19]. Epidemiologic studies have found an association between serum Gal-3 level and risk of sepsis [20–22] as well as development of chronic kidney disease (CKD) [23–25]. Pertinent findings show that serum Gal-3 predicts 30-day all-cause mortality in sepsis [26], preoperative serum Gal-3 predicts AKI after cardiac surgery [27], and serum Gal-3 at ICU discharge is associated with severity of AKI [28]. However, no previous study has examined the relationship between serum Gal-3 at the time of admission and the subsequent development of AKI in patients with sepsis. Additionally, the temporal relationship between Gal-3 and IL-6 in the pathophysiology of S-AKI has never before been explored.
Prior murine studies have demonstrated the importance of Gal-3 in the pathogenesis of sepsis [29, 30] and kidney disease [31, 32], including AKI [28, 33–36]. Pharmacologic inhibition of Gal-3 has ameliorated nephropathy induced by renal ischemia–reperfusion (IR) [28], unilateral ureteral obstruction [29], folic acid [34], hypertension [37, 38], aldosterone [39], unilateral nephrectomy [40], obesity [41], aortic stenosis [41], and cisplatin [42]. However, no murine experiment has evaluated the relationship between Gal-3 and AKI in sepsis.
Here, we present a translational study of serum Gal-3 in sepsis and S-AKI. We aimed to explore the role of Gal-3 in the pathophysiology of S-AKI and its potential utility as a therapeutic target. We examined patients admitted to the ICU with sepsis and determined whether serum Gal-3 levels predicted subsequent development of AKI and ICU mortality. In a rat model of sepsis induced by cecal ligation and puncture (CLP), we evaluated the role of Gal-3 in the pathogenesis of S-AKI, as well as the potential utility of Gal-3 as a therapeutic target. We studied the effect of an oral Gal-3 inhibitor, modified citrus pectin, on S-AKI occurrence, mortality, and levels of serum Gal-3, IL-6, and creatinine, as well as the temporal relationship between the rise of serum Gal-3 and IL-6.
Methods
Patient study
A prospective observational study was conducted with the approval of the Ethics Committee of Zhongnan Hospital of Wuhan University at the general ICU of Zhongnan Hospital of Wuhan University, Hubei Province, China. From January 1, 2019 to October 31, 2019, consecutive patients were enrolled following a diagnosis of sepsis according to the Third International Consensus (Sepsis-3) Definitions [43]. Patients with pre-existing AKI, CKD, renal replacement therapy, end-stage renal disease, malignancy, or organ transplantation were excluded from the study. Patients without a consent form, less than 18 years old, or over 80 years old were also excluded. An acute physiology and chronic health evaluation (APACHE II) assessment was also performed [44]. The two primary outcomes were survival in the ICU and development of subsequent AKI.
Serum biochemical measurements
A blood sample was obtained from patients within 6 hours (h) of admission to the ICU. Serum Gal-3 was measured by the human Gal-3 enzyme-linked immunosorbent assay (ELISA) Kit (BG Medicine, Corgenix, Inc., Broomfield, CO, USA; detection range: 1.4 ng/ml to 94.8 ng/ml), and serum creatinine (Cr) was measured using AU5831 Clinical Chemistry Analyzers (Beckman Coulter, Inc. Brea, CA, USA). In addition, serum neutrophil gelatinase-associated lipocalin (NGAL) and cystatin C (CysC) were measured with ELISA kits (Proteintech, Rosemont, IL, USA) according to the manufacturer`s instructions. Procalcitonin (PCT) was also measured using the ELFA (Enzyme-Linked Fluorescent Assay) technique by VIDAS® B•R•A•H•M•S PCT™ (bioMérieux, Inc., Marcy-l'Étoile, France).
Evaluation of renal function and survival
AKI was evaluated according to Kidney Disease: Improving Global Outcomes (KDIGO) clinical practice guidelines based on serum Cr criteria [45]. In addition, patient survival during ICU stay was evaluated.
Animal study
Male adult (weight 400–600 g) Sprague–Dawley rats were purchased from the Center for Animal Experiment of Wuhan University. All animals were housed in individually ventilated cages and had free access to water and food. All performed procedures were previously reviewed and approved by the Animal Care and Use Committee of Wuhan University.
Cecal ligation and puncture model
CLP was performed with a predetermined 25% ligated length of cecum. Following ligation, the cecum was punctured twice using a 20-gauge needle inferior to the ileocecal valve. The abdomen was then closed and 20 ml/kg of prewarmed saline was administered subcutaneously as fluid resuscitation. Rats were returned to their cages and allowed food and water ad libitum.
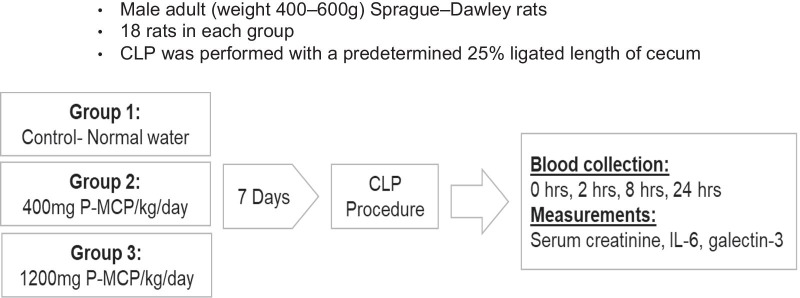
Animal experimental protocol
The animal study included three groups (Fig. 1). All rat groups underwent CLP. Two intervention groups were administered low molecular weight modified citrus pectin (P-MCP) (PectaSol-C®, EcoNugenics, Santa Rosa, CA, USA) in drinking water for seven days prior to CLP. P-MCP is a dietary supplement comprised of low molecular weight pectin, which directly inhibits Gal-3 by binding to the carbohydrate recognition domain of Gal-3 [46]. The pectin is derived from the pith of citrus peels, after which it is enzymatically treated to yield pectin fibers with a molecular weight less than 15 kDa and less than 5% esterification [46]. The effect of P-MCP has been validated in multiple animal models of AKI [36, 38, 39, 41, 42].
Fig. 1.
CLP experimental strategy. All rats underwent CLP. Control group (n = 18) received normal drinking water, while two intervention groups received a Gal-3 inhibitor, PMCP, at 400 mg/kg/d and 1200 mg/kg/d 7 d prior to CLP. Following CLP, blood was drawn at baseline, 2, 8, and 24 h post-CLP for serum biochemical measurements
The first intervention group (n = 18) received P-MCP at 400 mg/kg/day, while the second intervention group (n = 18) received P-MCP at 1200 mg/kg/day. The control group (n = 18) was not provided with P-MCP prior to CLP and received water ad libitum. P-MCP was not provided to any group following the CLP procedure.
Serum biochemical measurements
Blood (1.0 ml) was drawn from the jugular vein at 24 h prior to CLP (as baseline), and at 2, 8, and 24 h post-CLP. Serum was collected using EDTA as an anticoagulant. Samples were centrifuged for 15 min at 1000 × g at 2–8 °C within 30 min of collection. The supernatant was collected for assaying.
Serum Gal-3 levels were measured at baseline, 2, 8, and 24 h post-CLP, using an enzyme-linked immunosorbent assay (ELISA) (Lifespan Biosciences, Seattle, WA, USA; detection range: 0.156 ng/ml to 10 ng/ml), and serum IL-6 level was measured at baseline, 2, 8, and 24 h post-CLP, using an ELISA (R&D Systems, Minneapolis, MN, USA). Additionally, rat serum Cr levels were measured to assess renal function using a Cr assay kit (Nanjing Jiancheng Bioengineering Institute, Nanjing, China).
Evaluation of renal function and survival rate
Serum Cr was measured at baseline, 2, 8, and 24 h post-CLP to assess renal function using a Cr enzymatic assay kit. AKI occurrence was determined by Risk, Injury, Failure, Loss of kidney function, and End-stage kidney disease (RIFLE) criteria at 24 h post-CLP. Per RIFLE criteria, AKI was defined as Cr level at least 150% of baseline at 24 h, and severity was categorized as risk (RIFLE-R), injury (RIFLE-I), and failure (RIFLE-F) according to Cr level at 150%, 200%, and 300% of baseline respectively at 24 h [47, 48]. Survival was evaluated at 7 days post-CLP.
Statistical analysis
All numerical data were expressed as mean ± standard error of the mean (SEM) or median and interquartile range. Statistical p < 0.05 was considered significant. Sample means were compared between groups using two-tailed t-tests and analysis of variance (ANOVA), and within-group differences were analyzed using the Wilcoxon signed-rank test. Additionally, Pearson’s chi-squared test was used to evaluate for associations between categorical variables. Survival analysis was conducted using Kaplan–Meier analysis, and mortality in each group was compared using the log-rank test.
Multivariate logistic regression was performed to analyze Gal-3 as an independent predictor of death with and without controlling for age, AKI, and APACHE II score. Multivariate logistic regression was also used to evaluate Gal-3 as an independent predictor of AKI with and without adjusting for age and APACHE II score. Area under the receiver operating characteristic curve (AUC-ROC) was estimated to evaluate the performance of Gal-3 as a predictor of S-AKI and death in ICU patients [49]. Statistical analyses were performed using R software and Microsoft 365 Excel data analysis software.
Results
Patient characteristics
The study sample included 57 patients who were admitted to the ICU with a diagnosis of sepsis. Table 1 summarizes patient characteristics at the time of admission and mean serum Gal-3 levels, as well as additional serum biomarkers CysC, NGAL, and PCT levels. There was no significant difference in mean age between patients that developed S-AKI and patients that did not develop S-AKI following ICU admission (age: 60.6 ± 1.6 years vs. 59 ± 2.0 years, p = 0.53). APACHE II score was significantly higher among patients that developed S-AKI as compared to patients that did not (18.6 ± 1.2 vs 15.2 ± 1.1, p < 0.05).
Table 1.
Characteristics of patients at ICU admission
| Variable | All patients (n = 57) | Patients without subsequent AKI (n = 30) | Patients with subsequent AKI (n = 27) | P value |
|---|---|---|---|---|
| Age (years) | 59 (53–66) | 59 (53–66.8) | 61 (55–66) | 0.53 |
| Female sex, n (%) | 32 (56) | 18 (60) | 14 (52) | 0.73 |
| ICU stay (days) | 13 (9–15) | 11 (8.3–13) | 15 (11.5–19.5) | < 0.001 |
| APACHE II score | 16 (12–21) | 14 (11–17) | 20 (13.5–23) | < 0.05 |
| Serum Gal-3 (ng/ml) | 5.7 (3.6–8.9) | 4.2 (3.5–7) | 7.9 (4.7–16.6) | 0.002 |
| Serum CysC (μg/ml) | 1.5 (1.1–2.2) | 1.2 (0.9–1.5) | 2 (1.7–4.1) | 0.002 |
| Serum NGAL (ng/ml) | 302.9 (175.3–514.2) | 243.4 (170.6–421.9) | 430 (215–561) | 0.406 |
| Serum PCT (ng/ml) | 11.2 (3.1–52.4) | 7.7 (2.9–27.3) | 32.6 (3.7–91) | 0.007 |
Characteristics of patients in AKI and non-AKI groups. Characteristics were compared using chi-square tests or two-tailed t-tests. AKI acute kidney injury, APACHE II acute physiology and chronic health evaluation II, CysC cystatin C, Gal-3 galectin-3, ICU intensive care unit, NGAL neutrophil gelatinase-associated lipocalin, PCT procalcitonin
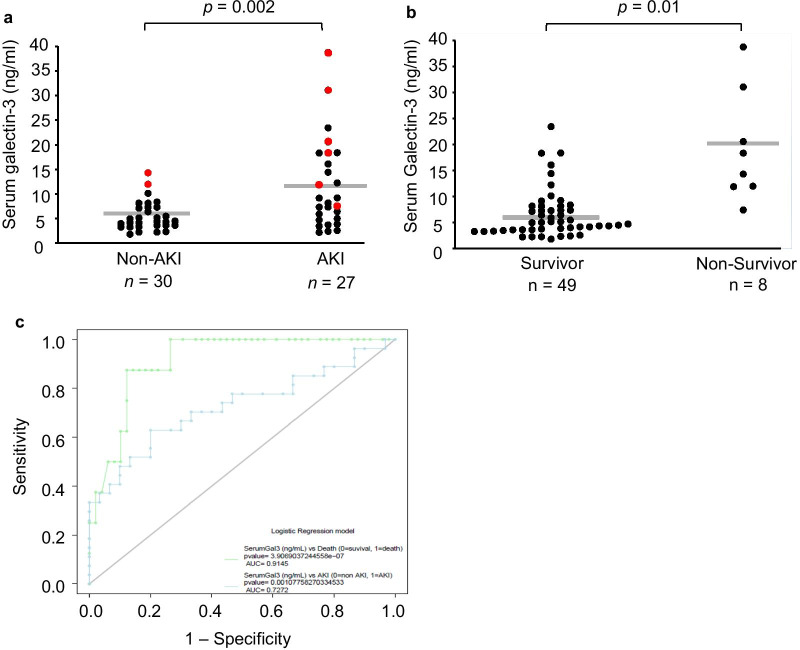
Serum Galectin-3, AKI, and survival
Of the 57 patients admitted to the ICU, 27 (47%) subsequently developed S-AKI. Additionally, 8 patients (14%) died during the ICU stay: 6 were in the S-AKI group and 2 were in the non-AKI group. Mean serum Gal-3 level was significantly higher among patients that developed subsequent S-AKI as compared to patients that did not develop S-AKI (11.2 ± 1.6 ng/ml vs. 5.3 ± 0.5 ng/ml; p = 0.002) (Fig. 2a). Mean serum Gal-3 level was also significantly higher among patients that died as compared to patients that did not die (18.7 ± 3.6 ng/ml vs. 6.4 ± 0.7 ng/ml; p = 0.01) (Fig. 2b). Using multivariate logistic regression, serum Gal-3 was associated with an increased odds of death before and after adjusting for age, AKI occurrence, and APACHE II score (OR = 1.4 [95% CI 1.1–2.2], p = 0.04). Serum Gal-3 was also associated with an increased odds of AKI before and after adjusting for age and APACHE II score (OR = 1.2 [95% CI 1.1–1.4], p = 0.01). The AUC-ROC for serum Gal-3 predicting subsequent AKI was 0.73, and the AUC-ROC for serum Gal-3 predicting ICU mortality was 0.91 (Fig. 2c).
Fig. 2.
Serum galectin-3 levels at ICU admission predict subsequent acute kidney injury and ICU mortality among patients. Means are shown by the gray horizontal bars and displayed numerically above the corresponding columns. a Serum galectin-3 levels in AKI vs non-AKI groups following ICU admission (11.2 ± 1.6 ng/ml vs. 5.3 ± 0.5 ng/ml, p = 0.002). Red dots represent data from non-survivors, while black dots represent data from survivors. b Serum galectin-3 levels in survivor vs non-survivor groups following ICU admission (18.7 ± 3.6 ng/ml vs. 6.4 ± 0.6 ng/ml, p = 0.0002). c Area under the receiver operating characteristic curves for serum galectin-3 in survival (green curve) and galectin-3 in AKI (blue curve)
Rat Cecal ligation and puncture model
In total, 54 animals underwent the CLP procedure: 18 rats in the control group, and 18 rats in each P-MCP-treated group.
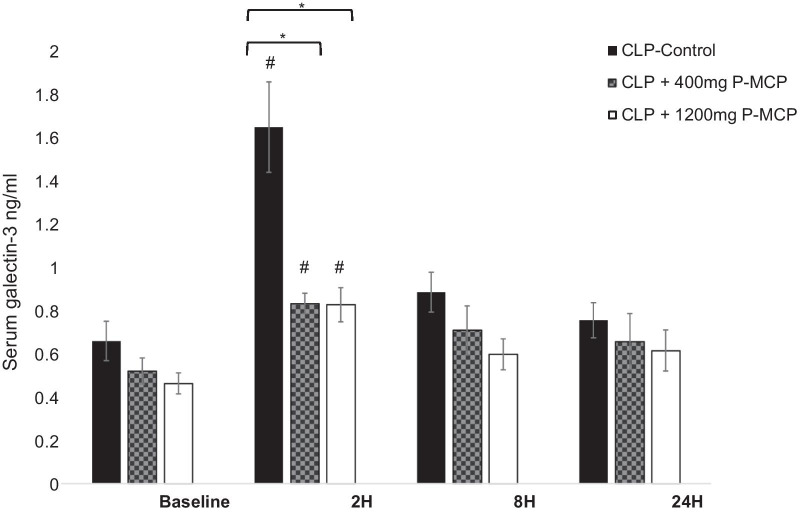
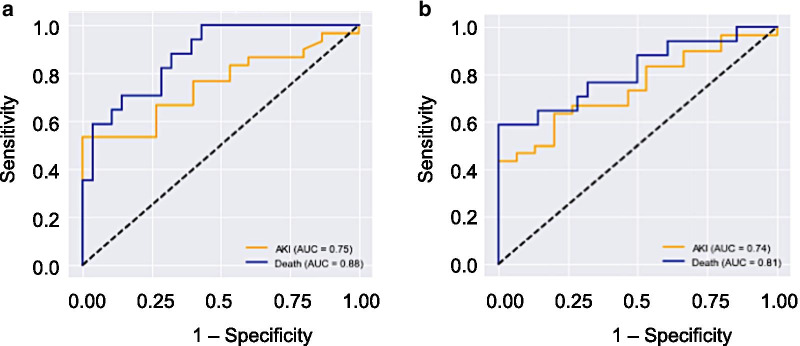
Galectin-3
Differences in serum Gal-3 concentrations between control and P-MCP-treated rats are shown in Fig. 3. Baseline serum values were not significantly different among the three rat groups (F = 3.2, p = 0.15). In both P-MCP-treated groups, mean serum Gal-3 levels were significantly lower than control at 2 h post procedure (400 mg P-MCP: 0.83 ± 0.05 ng/ml vs 1.63 ± 0.22 ng/ml, p = 0.003; 1200 mg P-MCP: 0.82 ± 0.08 ng/ml vs 1.63 ± 0.22 ng/ml, p = 0.001). Serum Gal-3 levels in all groups peaked at 2 h post-CLP and were significantly higher than their respective baseline values (control: p = 0.0001; 400 mg P-MCP: p = 0.001; 1200 mg P-MCP: p = 0.004). Gal-3 levels in all three groups subsided rapidly and were no longer significantly elevated at 8 h post CLP compared to their respective baseline values. The AUC-ROC for serum Gal-3 predicting subsequent AKI was 0.75, and the AUC-ROC for serum Gal-3 predicting mortality was 0.88 (Fig. 4a).
Fig. 3.
Serum galectin-3 levels with and without P-MCP pretreatment at baseline, 2 h, 8 h, and 24 h post-CLP in a rat CLP model. * indicates p < 0.05 for comparison between control group and P-MCP-treatment group. # indicates p < 0.05 for within group comparison to baseline value
Fig. 4.
Serum galectin-3 and IL-6 predict AKI and death in a rat CLP model. a Area under the receiver operating characteristic curve for serum galectin-3 in AKI (yellow curve) and mortality (blue curve). b Area under the receiver operating characteristic curve for IL-6 in AKI (yellow curve) and mortality (blue curve)
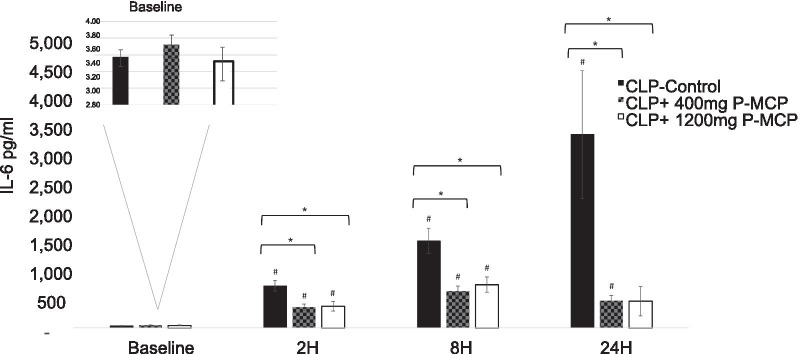
Interleukin-6
Differences in serum IL-6 concentrations between control and P-MCP-treated rats are shown in Fig. 5. Baseline values were not significantly different among the three groups (F = 3.2, p = 0.56). Concentrations of serum IL-6 in both P-MCP-treated groups were significantly lower than control values at all post-CLP time points, with the maximum difference at 24 h post-CLP (400 mg P-MCP: 468.0 ± 89.5 pg/ml vs 1344.5 ± 1103.4 pg/ml, p = 0.015; 1200 mg P-MCP: 458.8 ± 251.9 pg/ml vs 1344.5 ± 1103.4, p = 0.02) (Fig. 5). Serum IL-6 in the control group increased over time and peaked at 24 h post-CLP (3,344.5 ± 1,103.4 pg/ml). In both Gal-3 inhibitor groups, IL-6 levels decreased between 8 and 24 h post-procedure. The reduction in IL-6 levels between 8 and 24 h post-CLP was statistically significant in the 1200 mg P-MCP group only (631 [IQR 494.7–828.2] pg/ml vs 187.2 [IQR 156.5–272.6] pg/ml, p = 0.006). The AUC-ROC for serum IL-6 predicting subsequent AKI was 0.74, and the AUC-ROC for serum IL-6 predicting ICU mortality was 0.81 (Fig. 4b).
Fig. 5.
Serum IL-6 levels with and without P-MCP pretreatment in a rat CLP model. IL-6 concentrations were significantly lower in the P-MCP 400 mg and P-MCP 1200 mg group vs. the control group. * indicates p < 0.05 for comparison between control group and P-MCP-treatment group. # indicates p < 0.05 for within group comparison to baseline value
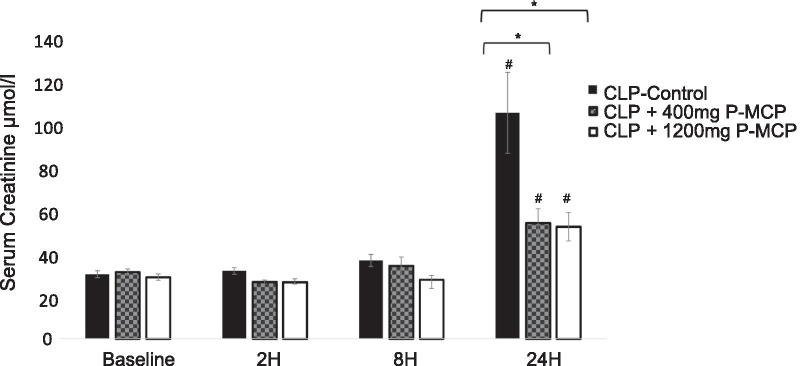
Creatinine
Differences in serum Cr concentrations between control and P-MCP-treated rats are shown in Fig. 6. Baseline values were not significantly different between the three groups (F = 3.2, p = 0.54). Serum Cr concentration in the 1200 mg P-MCP-treated group was significantly lower than control at all time points post-CLP, reaching a peak difference at 24 h post-procedure (51.8 ± 6.7 µmol/l vs 104.6 ± 18.8 µmol/l, p = 0.016). Serum Cr concentration in the 400 mg P-MCP-treated group was significantly lower than control group at 2 h and 24 h post-CLP (2 h: 26.3 ± 0.9 µmol/l vs 31.3 ± 1.6 µmol/l, p = 0.009; 24 h: 53.5 ± 4.2 µmol/l vs 104.6 ± 18.8 µmol/l, p = 0.005).
Fig. 6.
Serum creatinine levels with and without P-MCP pretreatment in a rat CLP model. * indicates p < 0.05 for comparison between control group and P-MCP-treatment group. # indicates p < 0.05 for within group comparison to baseline value
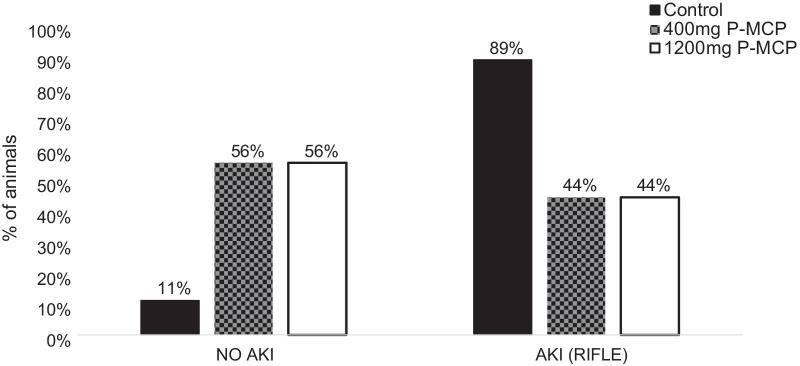
AKI
The percent of animals that developed AKI at 24 h post-CLP in the control and P-MCP-treated groups are shown in Fig. 7. As determined by RIFLE criteria, 89% (16) of rats in the control group developed AKI, while 44% (8) of rats developed AKI in the 400 mg P-MCP group and 44% (8) developed AKI in the 1200 mg P-MCP group. There was a statistically significant difference in AKI rate between the control group and both the 400 mg P-MCP group (p = 0.007) and 1200 mg P-MCP group (p = 0.007). In the control group, 8 (44%) rats were classified as RIFLE-R, 2 (11%) rats were RIFLE-I, and 6 (33%) rats were RIFLE-F. In the 400 mg P-MCP group, 1 (6%) rat was classified as RIFLE-R, 4 (22%) rats were RIFLE-I, and 3 (17%) rats were RIFLE-F. In the 1200 mg P-MCP group, 1 (6%) rat was classified as RIFLE-R, 4 (22%) rats were RIFLE-I, and 3 (17%) rats were RIFLE-F.
Fig. 7.
Acute kidney injury occurrence with and without P-MCP pretreatment in a rat CLP model. Percent AKI with or without P-MCP pretreatment per RIFLE criteria. Within the control group, 16 (89%) rats developed AKI. In each P-MCP group (400 mg and 1200 mg), 8 (44%) rats developed AKI
Survival
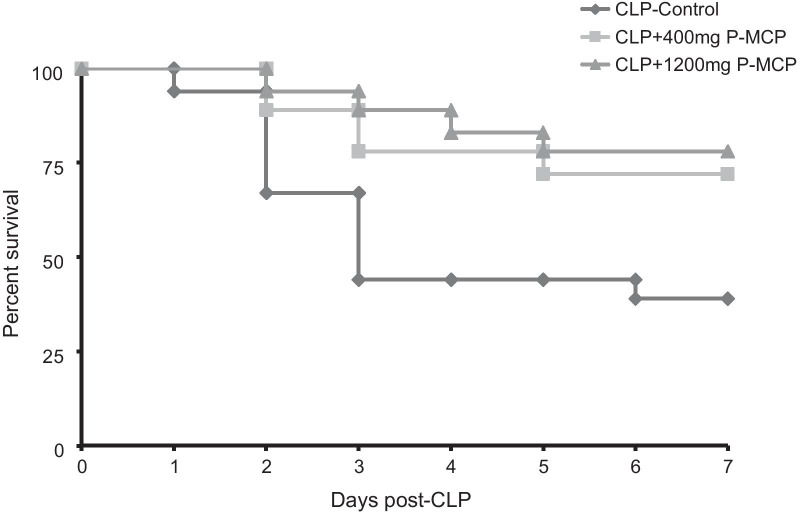
Survival data are shown in Fig. 8. Each group began with 18 rats prior to CLP. At 7 days post-CLP, 11 (61%) rats had died in the control group compared to 5 (28%) rats in the 400 mg P-MCP group and 4 (22%) rats in the 1200 mg P-MCP group. Mortality was significantly lower in both P-MCP treated groups as compared to controls (400 mg P-MCP: p = 0.03; 1200 mg P-MCP: p = 0.001).
Fig. 8.
Survival curves with and without P-MCP pretreatment in a rat CLP model. Each group started with 18 rats prior to CLP procedure. By day 7, 11 (61%) rats had died in the control group, compared to only 5 (28%) rats in the 400 mg P-MCP group (p = 0.03) and 4 (22%) rats in the 1200 mg P-MCP group (p = 0.001)
Discussion
In this translational study, we evaluated the role of Gal-3 in sepsis and S-AKI. We found that elevated Gal-3 levels at ICU admission predicted S-AKI and mortality in patients with sepsis, while inhibition of Gal-3 in a CLP rat model resulted in a statistically significant reduction in S-AKI and mortality. Together, these findings suggest that Gal-3 plays an important role in the pathophysiology of S-AKI and sepsis mortality.
In patients admitted to the ICU with sepsis, elevated serum Gal-3 levels at admission predicted ICU mortality. Our findings are consistent with other clinical research in which serum Gal-3 levels predicted 30-day all-cause mortality in sepsis [26], as well as murine experiments demonstrating the important role of Gal-3 in sepsis pathogenesis and mortality [27, 30]. Our findings suggest that serum Gal-3 may serve as a prognostic indicator in sepsis.
We also found that serum Gal-3 levels obtained at ICU admission were associated with subsequent AKI, as were two previously studied biomarkers of kidney injury, CysC and PCT [50–52]. Further, Gal-3 levels predicted subsequent development of S-AKI after controlling for age and APACHE II score. This is the first report of such a finding in patients with sepsis. It is consistent with previous findings that preoperative serum Gal-3 predicts AKI after cardiac surgery [27], and that Gal-3 at the time of ICU discharge is associated with severity of AKI [28]. Our findings are also consistent with various murine experiments, which demonstrate that Gal-3 plays a role in the pathophysiology of AKI secondary to various insults [28, 33–36]. In our patient study, 6 of the 8 observed deaths were in patients who had developed S-AKI, suggesting that the increased mortality seen in those with high Gal-3 levels may be mediated, at least in part, by impaired renal function [53]. While there was an association between Gal-3 and AKI, the predictive ability of Gal-3 in the detection of AKI was lower than that of mortality. Notably, the patient study was limited by its observational nature, small sample size, and low mortality rate. The findings demonstrate an association of Gal-3 with both mortality and AKI, and warrant further evaluation of the role of Gal-3 in S-AKI and sepsis mortality.
In a CLP rat model, we found that administration of a Gal-3 inhibitor prior to CLP significantly reduced mortality and S-AKI rate in both P-MCP-treated groups. Inhibition of Gal-3 also resulted in a significant reduction in Gal-3 and IL-6 levels. The difference between IL-6 levels in the control and P-MCP-treated groups increased over time, reaching the greatest difference at 24 h post-CLP. Prior studies have also reported attenuation of IL-6 levels with Gal-3 knock out or Gal-3 inhibition [28, 29, 35, 37].
In the control group, serum Gal-3 levels peaked earlier than serum IL-6: Gal-3 levels peaked at 2 h post-CLP and fell to near-baseline by 8 h, while IL-6 continued to rise throughout the entire 24 h post-procedure period. Comparatively, in the Gal-3 inhibitor groups, IL-6 levels decreased between 8 and 24 h post-procedure. Compared to controls, the decrease in IL-6 between 8 and 24 h was statistically significant in the 1200 mg P-MCP group only. Together, these findings suggest that serum Gal-3 release may precede the rise of IL-6 in the inflammatory cascade. Additionally, P-MCP-mediated Gal-3 inhibition may exert its effect in a dose dependent manner. At higher doses, Gal-3 inhibition may cause IL-6 levels to drop at an earlier time point.
Given the important role of IL-6 in the inflammatory cascade, these preliminary findings suggest that Gal-3 may serve as an upstream mediator of the “cytokine storm” in sepsis and S-AKI [54]. Study limitations included small sample sizes, as well as limited follow-up time to monitor Cr rise. Additionally, given our aim to compare mortality among CLP groups, histological evaluation of renal tissue was not possible.
In humans, elevations in serum Gal-3 may persist for longer durations. In a study by Prud’homme et al., 645 patients with AKI during their ICU stay demonstrated elevated serum Gal-3 levels at discharge [28]. Further, Gal-3 levels at discharge were increasingly elevated with increased severity of AKI [28]. Given these findings, Gal-3 may continue to play a role in the progression of AKI past the 2 to 8 h range detected in our rat model. Our findings warrant further investigation of the potential therapeutic utility of Gal-3 inhibition or removal in the prevention and treatment of S-AKI.
Conclusion
This translational study demonstrates the important role of Gal-3 in the pathogenesis of S-AKI, as well as its potential utility as a therapeutic target. Further studies, including randomized trials, are warranted to examine the role of Gal-3 as a therapeutic target in the treatment of sepsis and S-AKI.
Acknowledgements
The authors would like to thank Anat Stern, John Trepanowski, Dale Cumming, and Barry Wilk for their help in preparing the manuscript.
Abbreviations
- AKI
Acute kidney injury
- APACHE II
Acute physiology and chronic health evaluation
- AUC-ROC
Area under the receiver operating characteristic
- CLP
Cecal ligation and puncture
- CKD
Chronic kidney disease
- Cr
Creatinine
- CysC
Cystatin C
- ELFA
Enzyme-linked fluorescent assay
- ELISA
Enzyme-linked immunosorbent assay
- Gal-3
Galectin-3
- IL-6
Interleukin-6
- ICU
Intensive care unit
- KDIGO
Kidney disease: improving global outcomes
- P-MCP
Pectasol modified citrus pectin
- NGAL
Neutrophil gelatinase-associated lipocalin
- PCT
Procalcitonin
- RIFLE
Risk, injury, failure, loss of kidney function, and end-stage kidney disease
- S-AKI
Sepsis-associated AKI
Authors' contributions
IE, ZP, and JK were responsible for study concept and design. HS and HJ performed the experiment. ZP, AE, and HS analyzed and interpreted the data. AE and IE wrote the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (Grant 81772046, 81971816).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This prospective observational clinical study was conducted with the approval of the Ethics Committee of Zhongnan Hospital of Wuhan University, at the general ICU of Zhongnan Hospital of Wuhan University, Hubei Province, China. All performed procedures on animals were previously reviewed and approved by the Animal Care and Use Committee of Wuhan University.
Consent for publication
Not applicable.
Competing interest
IE is the developer of P-MCP. The other authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Haibing Sun and Huiping Jiang have contributed equally to this manuscript and share the first authorship
Contributor Information
Zhiyong Peng, Email: pengzy5@hotmail.com.
Isaac Eliaz, Email: isaac.eliaz@gmail.com.
References
- 1.Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S, et al. Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA. 2005;294:813–818. doi: 10.1001/jama.294.7.813. [DOI] [PubMed] [Google Scholar]
- 2.Bagshaw SM, Uchino S, Bellomo R, Morimatsu H, Morgera S, et al. Septic acute kidney injury in critically ill patients: clinical characteristics and outcomes. CJASN. 2007;2:431–439. doi: 10.2215/CJN.03681106. [DOI] [PubMed] [Google Scholar]
- 3.Bouchard J, Acharya A, Cerda J, Maccariello ER, Madarasu RC, Tolwani AJ, et al. A prospective international multicenter study of AKI in the intensive care unit. CJASN. 2015;10:1324–1331. doi: 10.2215/CJN.04360514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hoste EA, Bagshaw SM, Bellomo R, Cely CM, Colman R, et al. Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive Care Med. 2015;41:1411–1423. doi: 10.1007/s00134-015-3934-7. [DOI] [PubMed] [Google Scholar]
- 5.Rudd KE, Johnson SC, Agesa KM, Shackelford KA, Tsoi D, Kievlan DR, et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the Global Burden of Disease Study. Lancet. 2020;395:200–201. doi: 10.1016/S0140-6736(19)32989-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bagshaw SM, George C, Bellomo R, Committee ADM. Early acute kidney injury and sepsis: a multicentre evaluation. Crit Care. 2008;12:R47. doi: 10.1186/cc6863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mehta RL, Bouchard J, Soroko SB, Ikizler TA, Paganini EP, Chertow GM, et al. Sepsis as a cause and consequence of acute kidney injury: program to improve care in acute renal disease. Intensive Care Med. 2011;37:241–248. doi: 10.1007/s00134-010-2089-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tandukar S, Palevsky PM. Continuous renal replacement therapy: who, when, why, and how. Chest. 2019;155(3):626–638. doi: 10.1016/j.chest.2018.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Singbartl K, Formeck CL, Kellum JA. Kidney-immune system crosstalk in AKI. Semin Nephrol. 2019;39:96–106. doi: 10.1016/j.semnephrol.2018.10.007. [DOI] [PubMed] [Google Scholar]
- 10.Tanaka T, Narazaki M. Kishimoto T immunotherapeutic implications of IL-6 blockade for cytokine storm. Immunotherapy. 2016;8:959–970. doi: 10.2217/imt-2016-0020. [DOI] [PubMed] [Google Scholar]
- 11.Bozza FA, Salluh JI, Japiassu AM, Soares M, Assis EF, Gomes RN, et al. Cytokine profiles as markers of disease severity in sepsis: a multiplex analysis. Crit Care. 2007;11:R49. doi: 10.1186/cc5783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kellum JA, Kon L, Fink MP, Weissfeld LA, Yealy DM, Pinsky MR, et al. Understanding the inflammatory cytokine response in pneumonia and sepsis: results of the Genetic and Inflammatory Markers of Sepsis (GenIMS) Study. Arch Intern Med. 2007;167(15):1655–1663. doi: 10.1001/archinte.167.15.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wu HP, Chen CK, Chung K, Tseng JC, Hua CC, Liu YC, et al. Serial cytokine levels in patients with severe sepsis. Inflamm Res. 2009;58:385–393. doi: 10.1007/s00011-009-0003-0. [DOI] [PubMed] [Google Scholar]
- 14.Mera S, Tatulescu D, Cismaru C, Bondor C, Slavcovici A, Zanc V, et al. Multiplex cytokine profiling in patients with sepsis. APMIS. 2011;119:155–163. doi: 10.1111/j.1600-0463.2010.02705.x. [DOI] [PubMed] [Google Scholar]
- 15.Kellum JA, Pike F, Yealy DM, Huang DT, Shapiro NI, Angus DC, et al. Relationship between alternative resuscitation strategies, host response and injury biomarkers, and outcome in septic shock. Critical Care Med. 2017;45(3):438–445. doi: 10.1097/CCM.0000000000002206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hashizume M. Outlook of IL-6 signaling blockade for COVID-19 pneumonia. Inflamm Regen. 2020;40:24–31. doi: 10.1186/s41232-020-00134-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buckley LF, Wohlford GF, Ting C, Alahmed A, Van Tassell BW, Abbate A, et al. Role for anti-cytokine therapies in severe coronavirus disease 2019. Critical Care Explor. 2020;2:e0178. doi: 10.1097/CCE.0000000000000178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dumic J, Dabelic S, Flögel M. Galectin-3: an open-ended story. Biochim Biophys Acta. 2006;1760:616–635. doi: 10.1016/j.bbagen.2005.12.020. [DOI] [PubMed] [Google Scholar]
- 19.Henderson NC, Sethi T. The regulation of inflammation by galectin-3. Immunol Rev. 2009;230:160–171. doi: 10.1111/j.1600-065X.2009.00794.x. [DOI] [PubMed] [Google Scholar]
- 20.ten Oever J, Giamarellos-Bourboulis E, Van De Veerdonk F, Stelma F, Simon A, Janssen M, et al. Circulating galectin-3 in infections and non-infectious inflammatory diseases. Eur J Clin Microbiol Infect Dis. 2013;32:1605–1610. doi: 10.1007/s10096-013-1919-4. [DOI] [PubMed] [Google Scholar]
- 21.Mueller T, Leitner I, Egger M, Haltmayer M, Dieplinger B. Association of the biomarkers soluble ST2, galectin-3 and growth-differentiation factor-15 with heart failure and other non-cardiac diseases. Clin Chim Acta. 2015;445:155–160. doi: 10.1016/j.cca.2015.03.033. [DOI] [PubMed] [Google Scholar]
- 22.Dieplinger B, Egger M, Leitner I, Firlinger F, Poelz W, Lenz K, et al. Interleukin 6, galectin 3, growth differentiation factor 15, and soluble ST2 for mortality prediction in critically ill patients. J Crit Care. 2016;34:38–45. doi: 10.1016/j.jcrc.2016.03.020. [DOI] [PubMed] [Google Scholar]
- 23.O’Seaghdha CM, Hwang SJ, Ho JE, Vasan RS, Levy D, Fox CS. Elevated galectin-3 precedes the development of CKD. JASN. 2013;24:1470–1477. doi: 10.1681/ASN.2012090909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Drechsler C, Delgado G, Wanner C, Blouin K, Pilz S, Tomaschitz A, et al. Galectin-3, renal function, and clinical outcomes: results from the LURIC and 4D studies. JASN. 2015;26:2213–2221. doi: 10.1681/ASN.2014010093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rebholz CM, Selvin E, Liang M, Ballantyne CM, Hoogeveen RC, Aguilar D, et al. Plasma galectin-3 levels are associated with the risk of incident chronic kidney disease. Kidney Int. 2018;93:252–259. doi: 10.1016/j.kint.2017.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim H, Hur M, Moon HW, Yun YM, Di Somma S. Multi-marker approach using procalcitonin, presepsin, galectin-3, and soluble suppression of tumorigenicity 2 for the prediction of mortality in sepsis. Ann Intensive Care. 2017;7:27. doi: 10.1186/s13613-017-0252-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.von Ballmoos MW, Likosky DS, Rezaee M, Lobdell K, Alam S, Parker D, et al. Elevated preoperative galectin-3 is associated with acute kidney injury after cardiac surgery. BMC Nephrol. 2018;19:280. doi: 10.1186/s12882-018-1093-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Prud’homme M, Coutrot M, Michel T, Boutin L, Genest M, Poirier F, et al. Acute kidney injury induces remote cardiac damage and dysfunction through the galectin-3 pathway. JACC Basic Transl Sci. 2019;4:717–732. doi: 10.1016/j.jacbts.2019.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mishra BB, Li Q, Steichen AL, Binstock BJ, Metzger DW, Teale JM, et al. Galectin-3 functions as an alarmin: pathogenic role for sepsis development in murine respiratory tularemia. PLoS ONE. 2013;8:e59616. doi: 10.1371/journal.pone.0059616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ferreira RG, Rodrigues LC, Nascimento DC, Kanashiro A, Melo PH, Borges VF, et al. Galectin-3 aggravates experimental polymicrobial sepsis by impairing neutrophil recruitment to the infectious focus. J Infect. 2018;77:391–397. doi: 10.1016/j.jinf.2018.06.010. [DOI] [PubMed] [Google Scholar]
- 31.Henderson NC, Mackinnon AC, Farnworth SL, Kipari T, Haslett C, Iredale JP, et al. Galectin-3 expression and secretion links macrophages to the promotion of renal fibrosis. Am J Pathol. 2008;172:288–298. doi: 10.2353/ajpath.2008.070726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sasaki S, Bao Q, Hughes RC. Galectin-3 modulates rat mesangial cell proliferation and matrix synthesis during experimental glomerulonephritis induced by anti-Thy11 antibodies. J Pathol. 1999;187:481–489. doi: 10.1002/(SICI)1096-9896(199903)187:4<481::AID-PATH263>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 33.Nishiyama J, Kobayashi S, Ishida A, Nakabayashi I, Tajima O, Miura S, et al. Up-regulation of galectin-3 in acute renal failure of the rat. Am J Pathol. 2000;157:815–823. doi: 10.1016/S0002-9440(10)64595-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dang Z, MacKinnon A, Marson LP, Sethi T. Tubular atrophy and interstitial fibrosis after renal transplantation is dependent on galectin-3. Transplantation. 2012;93:477–484. doi: 10.1097/TP.0b013e318242f40a. [DOI] [PubMed] [Google Scholar]
- 35.Fernandes Bertocchi AP, Campanhole G, Wang PHM, Gonçalves GM, Damião MJ, Cenedeze MA, et al. A role for galectin-3 in renal tissue damage triggered by ischemia and reperfusion injury. Transpl Int. 2008;21:999–1007. doi: 10.1111/j.1432-2277.2008.00705.x. [DOI] [PubMed] [Google Scholar]
- 36.Kolatsi-Joannou M, Price KL. Winyard, PJ Long, DA Modified citrus pectin reduces galectin-3 expression and disease severity in experimental acute kidney injury. PLoS ONE. 2011;6(e1868):3. doi: 10.1371/journal.pone.0018683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Frenay A-RS, Yu L, van der Velde AR, Vreeswijk-Baudoin I, López-Andrés N, van Goor H, et al. Pharmacological inhibition of galectin-3 protects against hypertensive nephropathy. Am J Physiol Renal Physiol. 2015;308:F500-F509. [DOI] [PubMed]
- 38.Martínez-Martínez E, Ibarrola J, Fernández-Celis A, Calvier L, Leroy C, Cachofeiro V, et al. Galectin-3 pharmacological inhibition attenuates early renal damage in spontaneously hypertensive rats. J Hypertens. 2018;36:368–376. doi: 10.1097/HJH.0000000000001545. [DOI] [PubMed] [Google Scholar]
- 39.Calvier L, Martinez-Martinez E, Miana M, Cachofeiro V, Rousseau E, Sádaba JR, et al. The impact of galectin-3 inhibition on aldosterone-induced cardiac and renal injuries. JACC Heart Fail. 2015;3:59–67. doi: 10.1016/j.jchf.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 40.Zhang M, Gu Y, Wang H, Zhu P, Liu X, Wu J. Valsartan attenuates cardiac and renal hypertrophy in rats with experimental cardiorenal syndrome possibly through down-regulating galectin-3 signaling. Eur Rev Med Pharmacol Sci. 2016;20:345–354. [PubMed] [Google Scholar]
- 41.Martinez-Martinez E, Ibarrola J, Calvier L, Fernandez-Celis A, Leroy C, Cachofeiro V, et al. Galectin-3 blockade reduces renal fibrosis in two normotensive experimental models of renal damage. PLoS ONE. 2016;11:e0166272. doi: 10.1371/journal.pone.0166272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li HY, Yang S, Li JC, Fen, JX. Galectin 3 inhibition attenuates renal injury progression in cisplatin-induced nephrotoxicity. Biosci Rep. 2018;38:BSR20181803. [DOI] [PMC free article] [PubMed]
- 43.Shankar-Hari M, Phillips GS, Levy ML, Seymour CW, Liu VX, Deutschman CS, et al. Developing a new definition and assessing new clinical criteria for septic shock: for the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016;315:775–787. doi: 10.1001/jama.2016.0289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–829. [PubMed] [Google Scholar]
- 45.Kellum JA, Lameire N, Aspelin P, Barsoum RS, Burdman EA, Goldstein SL, et al. Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012;2:1–138. [Google Scholar]
- 46.Eliaz I, Raz A. Pleiotropic effects of modified citrus pectin. Nutrients. 2019;11(11):2619. doi: 10.3390/nu11112619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Peng ZY, Wang HZ, Srisawat N, Wen X, Rimmelé T, Bishop J, et al. Bactericidal antibiotics temporarily increase inflammation and worsen acute kidney injury in experimental sepsis. Crit Care Med. 2012;40:538–543. doi: 10.1097/CCM.0b013e31822f0d2e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhou F, Peng ZY, Bishop JV, Cove ME, Singbartl K, Kellum JA. Effects of fluid resuscitation with 09% saline versus a balanced electrolyte solution on acute kidney injury in a rat model of sepsis. Crit Care Med. 2014;42:e270–e278. doi: 10.1097/CCM.0000000000000145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zou KH, O'Malley AJ, Mauri L. Receiver-operating characteristic analysis for evaluating diagnostic tests and predictive models. Circulation. 2007;115:654–657. doi: 10.1161/CIRCULATIONAHA.105.594929. [DOI] [PubMed] [Google Scholar]
- 50.Huang YT, Lai MY, Kan WC, Shiao CC. Independent Predictive Ability of Procalcitonin of Acute Kidney Injury among Critically Ill Patients. J Clin Med. 2020;9(6):1939. doi: 10.3390/jcm9061939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chun K, Chung W, Kim AJ, Hyunsook K, Han R, Jae HC, et al. Association between acute kidney injury and serum procalcitonin levels and their diagnostic usefulness in critically ill patients. Sci Rep. 2019;9:4777. doi: 10.1038/s41598-019-41291-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dai X, Zeng Z, Fu C, Zhang S, Cai Y, Chen Z. Diagnostic value of neutrophil gelatinase-associated lipocalin, cystatin C, and soluble triggering receptor expressed on myeloid cells-1 in critically ill patients with sepsis-associated acute kidney injury. Crit Care. 2015;19(1):223. doi: 10.1186/s13054-015-0941-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Desmedt V, Desmedt S, Delanghe JR, Speeckaert R, Speeckaert MM. Galectin-3 in renal pathology: more than just an innocent bystander? Am J Nephrol. 2016;43:305–317. doi: 10.1159/000446376. [DOI] [PubMed] [Google Scholar]
- 54.Garcia-Revilla J, Deierborg T, Venero JL, Boza-Serrano A. Hyperinflammation and fibrosis in severe COVID-19 patients: Galectin-3, a target molecule to consider. Front Immunol. 2020;11:2069. doi: 10.3389/fimmu.2020.02069. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.