Abstract
BACKGROUND AND PURPOSE: Various techniques and materials have been used for the endovascular treatment of craniofacial high-flow arteriovenous vascular malformations, because their rarity precludes standardization of their treatment. The aim of this retrospective review is to assess Onyx as the primary embolic agent in the treatment of these vascular malformations.
MATERIALS AND METHODS: Six patients with arteriovenous fistulas and 3 with arteriovenous malformations (AVMs) of the head and neck region were treated with intra-arterial (IA)/direct percutaneous injections of Onyx. Adjunctive maneuvers used during embolization included external compression of the arterial feeders or venous outflow (6 patients), balloon assist (4 patients), and direct embolization of the draining vein remote to the fistula site (1 patient). n-butyl-2-cyanoacrylate (n-BCA) was used in addition to Onyx for rapid induction of thrombosis in a large venous pouch (1 patient) and for cost containment purposes (1 patient). Four patients were treated surgically after the embolization.
RESULTS: There were no neurologic complications secondary to the embolization procedure. The arteriovenous shunt was eliminated in all of the fistulous lesions and 2 of the 3 AVMs. The embolization was incomplete in 1 patient with a large AVM who declined further endovascular or surgical procedures. Untoward events included 2 instances of catheter entrapment (of 9 IA injections), blackish skin discoloration necessitating surgical revision in 1 patient, and difficulty of balloon deflation/wire withdrawal during a balloon-assisted embolization.
CONCLUSION: Onyx appears to be a safe and effective liquid embolic agent for use in the treatment of craniofacial high-flow vascular malformations with distinct advantages and disadvantages compared with n-BCA.
The physical properties of ethylene-vinyl alcohol copolymer (Onyx; ev3, Irvine, Calif) render it suitable for the treatment of intracranial arteriovenous malformations (AVMs), dural vascular malformations, or direct carotid cavernous fistulas.1-4 The reported use of this embolic agent in extracranial vascular malformations, including those of the head and neck, is currently very limited. We reviewed the results of treatment in our patients with facial high-flow vascular malformations who were treated primarily with this embolic agent.
Materials and Methods
From October 2003 to June 2006, 9 patients (7 male and 2 female) with a mean age of 19.9 years (range, 7–33 years) underwent elective embolization primarily with use of Onyx for the treatment of craniofacial high-flow vascular malformations (CHVMs). CHVM was defined as any vascular malformation of the craniofacial region with arteriovenous shunt surgery, supplied mainly by external carotid artery branches or the ophthalmic artery. Intracranial and dural malformations and carotid cavernous fistulas were excluded. One patient with an extensive intraosseous CHVM treated on an emergency basis for exsanguinating hemorrhage after tooth extraction was also excluded, because the treatment in this case was performed only for purposes of hemostasis. These patients were referred by the plastic/reconstructive service for pain, swelling, multiple varicosities, or thrill. One patient was referred for recurrent low-grade bleeding from the lesion. None of the patients were treated previously with surgery or embolization.
All of the patients underwent diagnostic angiography to include injections of bilateral external and internal carotid and at least 1 of the vertebral arteries via a femoral approach before the treatment to verify the associated shunt surgery and delineate the feeding arteries. Lesions were classified as AVMs if there was a clearly definable nidal component; otherwise they were classified as fistulas.
All of the treatments were performed after obtaining an informed consent through a femoral arterial approach and under systemic heparinization to keep activated clotting time levels at 250–300. All but 1 patient were treated under general anesthesia. Percutaneous injections were performed using the 21-gauge micropuncture needle (Cook, Bloomington, Ind). Percutaneous approach was supplemented with injection of n-butyl-2-cyanoacrylate (n-BCA; Braun, Melsungen, Germany) in 2 patients (for cost containment purposes in 1 patient during the treatment of a large AVM and for induction of a more intense thrombotic reaction in a large venous pouch supplied by innumerous arterial feeders in another patient). For intra-arterial (IA) injections, the UltraFlow microcatheter (ev3) and Onyx 18 (ev3) were used. The injections were performed using the technique as described in previous reports.1 In those cases where a need for limitation of proximal reflux of Onyx was anticipated, a 4- × 4-mm HyperForm balloon (ev3) was navigated as distal as possible, by the side of the microcatheter, and inflated intermittently during Onyx injection under road-mapping. In those cases where angiographic elimination of the malformation was unlikely to be achieved with a single embolization procedure, we arbitrarily aimed to obliterate at least one third of the malformation during the first session. After the procedure, anticoagulation was reversed. In 4 patients, postembolization surgery was performed in 2–4 weeks.
Results
Angiographic studies demonstrated a fistulous lesion in 6 patients. These lesions were supplied by the superficial temporal artery in 4 patients, from the main trunk of the internal maxillary artery in 1 patient, and from the occipital artery in another. The AVMs in the remaining 3 patients were primarily supplied by the ophthalmic (OA), middle meningeal, and superficial temporal arteries in the first patient; OA and internal maxillary artery and inferolateral trunk in the second patient; and the facial arteries bilaterally in the last patient. The locations of these lesions are listed in the Table.
Clinical and angiographic characteristics of patients
| Patient No. (Figure No.) | Age/Sex | Location | Main Symptoms | Type | Access | Reason to Use Onyx | Assist Technique | Outcome | Notes |
|---|---|---|---|---|---|---|---|---|---|
| 1 (Figure 1) | 21/M | L periorbital | Painful pulsatile mass totally obstructing vision | vm | IA × 3 PC | Anticipation of better penetration into the nidus of the malformation with IA injection and direct puncture | Balloon, direct puncture of draining vein remote to fistula | Total removal after 2 series of embolizations and surgeries | Catheter tip retained and removed later during surgery, difficulty in balloon retrieval, supplemented with glue for cost containment purposes and also for direct puncture of draining vein |
| 2 | 24/F | L cheek | Painful mass, cosmetic concerns | vm | IA × 1 | Anticipation of better penetration into the nidus of the malformation with IA injection | Balloon | Residual AVM | Incomplete treatment, patient unwilling to pursue further treatment |
| 3 | 10/M | At mentum of mandible | Mass with intermittent bleeding | vm | IA × 2 | Anticipation of better penetration into the nidus of the malformation with IA injection | Total elimination of malformation | Small AVM, bilateral facial approach, no surgery, catheter tip retained on one side | |
| 4 | 7/M | L preauricular | Enlarging PM | fs | IA × 1 | Plan to use external compression to limit embolization to the exact point of fistula under controlled injection to avoid excessive venous filling & arterial reflux | EC on both arterial and venous side of AVF | Total elimination of shunt | |
| 5 | 9/M | R angle of mandible | Enlarging PM | fs | IA × 1 TV in session 1, PC for 2nd session | Plan to use balloon assist | Balloon for session 1, venous EC for both sessions | Total elimination of shunt after 2 sessions of embolization | Significant filling of lesion through collaterals after session 1, glue used during second session to fill in large venous pouch |
| 6 (Figure 2) | 25/F | R zygoma | Bruit, PM | fs | IA × 1 | Plan to use balloon assist | Balloon | Total elimination of shunt | |
| 7 | 26/M | L temple | fs | PC | Anticipation of retrograde filling of feeders | Venous EC | Total elimination of shunt | Surgical excision of cast | |
| 8 (Figure 3) | 33/M | L occipital | Painful large scalp mass | fs | PC | Anticipation of retrograde filling of feeders | Venous EC | Total elimination of shunt | Surgical excision of cast |
| 9 (Figure 4) | 24/M | L forehead | Cosmetic concerns | fs | PC | Anticipation of retrograde filling of feeders | Venous EC | Total elimination of shunt | Surgical excision of cast, second surgery for blackish discoloration at injection site |
Note:—M indicates male; F, female; L, left; R, right; PM, pulsatile mass; vm or AVM, arteriovenous malformation; AVF, arteriovenous fistula; fs, fistulous lesion; IA, intra-arterial; PC, percutaneous; TV, transvenous; EC, external compression.
The embolization procedures were well tolerated by all of the patients without evidence of a systemic or local toxicity, including cranial nerve palsy. Subcutaneous extravasation was noted in 1 patient. Except for mild pain that was controlled with nonnarcotic analgesics, none of the patients developed symptoms clinically suggestive of an inflammatory response. In 6 patients with arteriovenous fistulas, endovascular treatment alone was sufficient to eradicate the shunt. Five of these patients underwent a single session of embolization, and 1 patient needed a second embolization procedure to fully occlude a very large venous pouch draining innumerable arterial feeders from the external carotid circulation.
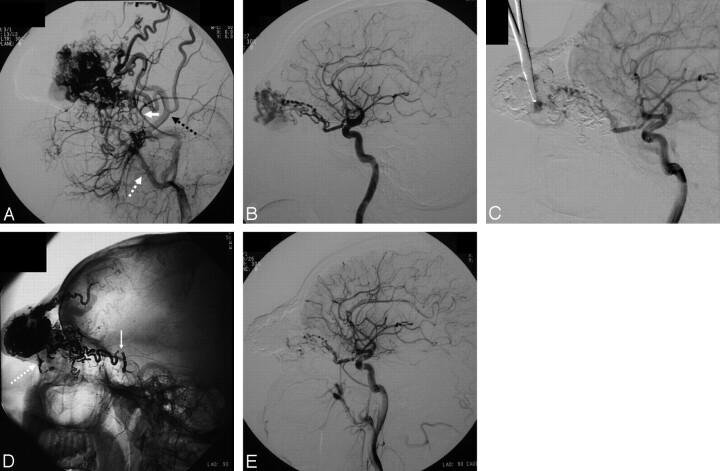
In 1 patient with an AVM, despite efforts to limit reflux by proximal balloon inflation, nidal penetration was less than expected. Otherwise, Onyx penetrated the vascular malformations effectively. The distal segments of 2 catheters were retained after IA injections. Retrograde filling of the arterial feeders with the embolic material was noted in all of the fistulous malformations during both IA and percutaneous injections. Maneuvers used to enhance the effectiveness of embolization during injections included compression of the drainage vein, direct puncture and embolization of the drainage vein remote to the fistula (Fig 1), external compression to trap both inflow and outflow (trapping the catheter tip), and inflation of a balloon proximal to the tip of the catheter (Figs 1 and 2). The latter method was associated with retrograde penetration (reflux) along the inflated balloon eventually in all of the 4 attempts.
Fig 1.
Patient 1.
A, Lateral projection of the left external carotid arteriogram demonstrates a periorbital arteriovenous malformation supplied by the branches of the superficial temporal (black dotted arrow) and internal maxillary arteries (white dotted arrow, middle meningeal branch: white arrow).
B, Lateral projection of the left internal carotid arteriogram showing ophthalmic artery contribution to the supply of the arteriovenous malformation.
C, Lateral projection of the left internal carotid arteriogram during second session embolization, after completion of the embolization of the external carotid supply discloses the drainage of the ophthalmic supply (marked by the tip of the hemostatic clamp). This drainage vein was selectively punctured and embolized.
D, Native image of the venous phase of a postembolization left common carotid arteriogram showing the embolic cast. The defect within the embolic cast denoted with the solid white arrow is the point of balloon inflation. Embolic agent is also noted in the vein draining the ophthalmic supply (white dotted arrow).
E, Left common arteriogram after the final session of embolization shows almost total obliteration of the lesion angiographically.
Fig 2.
Patient 6.
A, Native radiogram of right external carotid arteriogram in lateral projection reveals a fistulous CHVM supplied by the superficial temporal artery and collateral supply by ipsilateral middle meningeal and occipital arteries.
B, The inflated HyperForm balloon is visible (white arrows) on the roadmap capture in lateral projection obtained during embolization; note the retrograde filling of the middle meningeal and occipital collateral supply.
C, Postembolization ipsilateral external carotid arteriogram in the same projection demonstrates no evidence of residual arteriovenous shunt surgery.
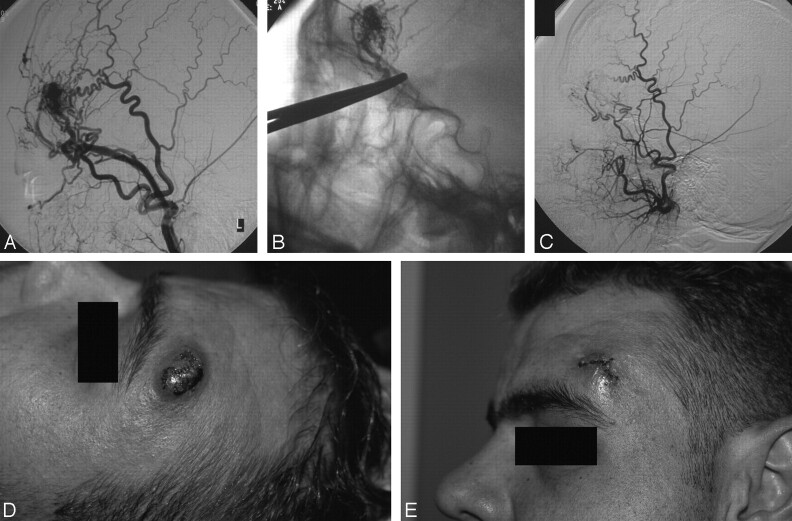
Surgical treatment was performed in 4 patients after the final session of embolization. In 1 patient with a large orbital AVM, the obstruction of the visual field (by the involved upper eyelid) was removed after staged resection of the embolic cast, and a good cosmetic result was also obtained. In 1 patient with a large scalp mass because of venous ectasia secondary to arteriovenous fistula (Fig 3), the cast was removed, because the patient was disturbed by the mass effect, especially when he had to lie on the ipsilateral side. In a young female patient with a fistula of the right zygomatic area, though the contour deformity of the embolic cast was barely noticeable, the patient preferred to have it removed based on the relatively low risk involved in the surgical removal. In a young male patient, there was subcutaneous extravasation of Onyx causing blackish skin discoloration, as well as persistence of the mass lesion of the small fistula. This patient underwent removal of the Onyx cast by simple excision with the expectation that the discoloration at the margins would eventually fade. However, the discoloration was evident even after the removal of the cast, and the patient decided to have a surgical revision for total elimination of the residual discoloration (Fig 4). At the conclusion of the multitechnique treatment by embolization alone or by combined embolization and surgery, 8 of 9 of our patients were asymptomatic and had good cosmetic results. In 1 patient, treatment could not be finalized, because the patient did not come back for admission for further embolization. Transient postprocedure mild-to-moderate pain was noted by the patient treated for the periorbital vascular malformation, and this was responsive to nonsteroidal anti-inflammatory/analgesic medication. The skin discoloration observed in 1 patient was successfully eradicated after surgical revision. Specifically, there were no transient or permanent neurologic deficits after the embolization procedures. The Table summarizes our results in this patient group.
Fig 3.
Patient 8.
A, Anteroposterior projection of a left external carotid arteriogram in Waters projection depicts a fistulous CHVM supplied by the superficial temporal, anterior deep temporal, and middle meningeal arteries.
B, Postembolization external carotid arteriogram in anteroposterior projection reveals total obliteration of the lesion.
Fig 4.
Patient 9.
A, Lateral projection of the left superficial temporal arteriogram demonstrates a fistulous CHVM; there is attenuated opacification of the draining vein, which projects in between the 2 branches of the artery.
B, Floroscopic image captured during percutaneous embolization shows impediment of venous filling by the external compression over the vein with a hemostatic clamp; retrograde filling in numerous arterial pedicles is also noted.
C, Postprocedure external carotid injection in lateral projection demonstrated no evidence of a residual lesion.
D, Postembolization photograph demonstrates blackish discoloration at the injection site.
E, Photograph after resection of the cast on postoperative day 5 shows residual discoloration at the margins of the incision.
Discussion
The experience and related literature regarding the use of Onyx in the treatment of vascular malformations have been growing within recent years. However, the current literature mainly relates to the cerebral and, to some extent, the peripheral (including the extremities and visceral circulations) use of this embolic agent.1,4,5 CHVMs have been studied as a subset of AVMs distinct from those involving the brain, the dura, or the peripheral circulation.6 They include AVMs and arteriovenous fistulas.7 Their rarity limits a systematic study to define a standard treatment; however, treatment is favored if they are symptomatic or located on the lips or scalp.6 The contribution of endovascular treatment to the management of these lesions is not clearly delineated. Some authors have used this approach only as an adjunct to surgery for definitive treatment.6 Others have used it successfully to attain total angiographic devascularization but still advocate surgical excision as the final step of treatment.8 In some patients, endovascular treatment sufficed as the only treatment with durable clinical results.9 We were able to find only 4 patients with CHVMs in the literature10,11 where Onyx was used as a liquid embolic agent for endovascular treatment. Three of these patients were treated as a part of the multicenter preclinical evaluation of this agent for head and neck hypervascular lesions.10 In the concise report on the fourth patient, the authors only briefly mention that Onyx was used as an adjunct to the coil embolization, and a discussion on this embolic agent is not provided.11 As such, the current literature lacks a dedicated analysis of this embolic agent for CHVMs.
For CHVMs, the distinction between a nidal and a fistulous type of malformation is important but sometimes impossible, because the latter may be treated only by endovascular obliteration of the fistulous opening and the adjacent vein.9,12 In our series, all of the malformations classified as fistulous could be treated with the use of Onyx as the primary embolic agent. We ascribe this result to the ability to inject this embolic agent slowly, in a prolonged fashion,1,2 with both IA and direct percutaneous access. We noted that Onyx first forms an embolic cast within the vascular structures, and then, unlike n-BCA, it permeates this cast with each injection, following the path of least resistance. In all of the fistulous lesions treated merely via percutaneous route, this physical property of Onyx1 enabled retrograde embolization of the arterial feeders after direct puncture of the venous outlet.
In the limited number of patients with AVMs in this series, our results were not as favorable. In these patients, Onyx penetrated the nidal compartment effectively. The ability to inject slowly during treatment enabled avoidance of the dangerous collaterals of the craniofacial vasculature, which are known to become more prominent in the presence of a vascular malformation.13 However, even with a good nidal penetration, sufficient preoperative devascularization could not be achieved in 1 patient because of the extensive nature of the malformation and the reflux of Onyx over the microcatheter despite the use of a proximal balloon-assist technique.
No clinical evidence of cranial nerve damage was noted after embolization procedures in our patients. Yet, findings suggestive of such toxicity were reported previously in a patient treated for preoperative embolization of a tumor.10
Proximal reflux of Onyx has been a technical problem.14 We used a balloon-assisted technique with over-the-wire balloon catheters to prevent proximal reflux of Onyx in 4 patients. To our knowledge this technique has not been documented previously. Balloons have been used for flow arrest for n-BCA embolization procedures15; however, the technique that we used is distinct from flow arrest in both the underlying purpose and the materials used. To begin with, the intent in balloon-assisted Onyx injection is to increase proximal resistance in the feeder in an effort to enhance distal penetration, whereas the primary goal of the previously reported flow-arrest is to prevent distal migration of n-BCA. In addition, the over-the-wire nondetachable balloons that we used in our patients are not well suited to assist n-BCA embolization because of the risk for adhesion or balloon rupture with this material. If use of the balloon-assisted technique was to be contemplated with n-BCA and detachable balloons, the detachable balloons would be limited in their navigation to access distal feeders of vascular malformations. In our limited experience with the balloon-assisted technique, the advantage of enhanced penetration of embolic agent was partly offset by some technical difficulties. We experienced difficulty in microwire withdrawal and subsequent balloon deflation on 1 occasion. In this patient (Fig 1), we left a lengthy segment between the tip of the microcatheter and the balloon. This segment was later filled with an attenuated reflux of Onyx promoted by inflation of the balloon proximally. Conceivably, the wire of the balloon was entrapped either within this reflux or at the level of the valve of the balloon by the insinuating Onyx. In the same patient, the tip of the microcatheter was also entrapped within the attenuated and lengthy reflux. In all of the instances where a balloon was used proximally, Onyx eventually penetrated retrogradely along the inflated balloon. Theoretically, increased proximal resistance may increase the likelihood of inadvertent embolization via external carotid-internal carotid or vertebral anastomosis.
Some disadvantages that we noted with the use of Onyx in facial lesions were discoloration of the skin, catheter entrapment, and cost. The extravasation of Onyx during percutaneous injection in 1 patient resulted in a permanent blackish discoloration of the overlying skin. This patient had to undergo 2 surgical treatments after embolization. There is a possibility that direct percutaneous embolization with glue would have prevented at least 1 of these surgeries, thus serving better the aim of embolization. Catheter tip retention occurred in 2 of 9 IA injections. Because a lengthier segment of reflux may be justified in the external carotid circulation compared with the intracranial circulation,1 a denser and lengthier proximal “embolic plug” and enhanced penetration of the embolic agent into the vascular malformation was possible. The higher (2 of 9 attempts) rate of catheter entrapment in this series is possibly secondary to the fact that we allowed for a more liberal reflux of the material at the expense of better penetration. The cost per volume of Onyx far exceeded that of n-BCA, which is diluted by Ethiodol (Andre Guerbet, Melville, NY) for embolization procedures. Another drawback of Onyx is the discomfort during injection in patients not treated under general anesthesia.5
For the purpose of comparison with Onyx, it is important to note that some of the drawbacks of n-BCA classically encountered during embolization of cerebral AVMs are less significant or even advantageous for percutaneous approach, which has been the mainstay8 of the embolization of CHVMs. First, the direct puncture approach eliminates the problem of catheter adhesion. In addition, increased thrombogenicity of n-BCA and subsequent occlusion of the venous outflow may be favorable16 rather than disadvantageous in CHVM treatment. Finally, it has been stated that the intense inflammatory reaction caused by n-BCA17 imposes early surgery in the brain. In contrast to the previous reports,16 delayed surgery (∼2–4 weeks) after embolization leads to the formation of a pseudocapsule around the embolic cast, allowing for easier excision in the head and neck lesions in our experience with n-BCA (currently unreported data).
Based on our preliminary findings, we adopted an approach that targets to make the most of the favorable characteristics of Onyx while avoiding some of its disadvantages for the embolization of superficial high-flow lesions. Our current approach involves IA embolization of the malformation with Onyx if it is easily accessible transarterially and direct percutaneous puncture and embolization of the remaining lesion with n-BCA. If the lesion is not easily accessible via an external carotid transarterial approach, percutaneous embolization with n-BCA is performed. The decision for the surgical excision is based on whether the lesion is totally embolized or the presence of cosmetic concerns. The efficacy of this approach will need to be evaluated.
Conclusion
Unlike the intracranial circulation, craniofacial high-flow malformations are rare, and there is no consensus on their treatment. Embolization has become an integral part of the treatment of these malformations. Cure of these lesions may be attained by embolization alone or embolization followed by surgical removal. Fistulous lesions are more likely to be cured by embolization alone through an IA and/or direct percutaneous approach. The advantages of Onyx seem to hold more for IA rather than a percutaneous approach. With the currently available limited data, the best strategy may be the individualization of the choice of the liquid embolic agent (n-BCA versus Onyx) based on the clinical and angiographic characteristics of each patient, as well as the overall estimated cost of the embolization procedure.
Footnotes
Part of this publication previously presented at: Annual Meeting of the American Society of Neuroradiology, April 29 to May 5, 2006; San Diego, Calif.
References
- 1.Arat A, Inci S. Treatment of a superior sagittal sinus dural arteriovenous fistula with Onyx: technical case report. Neurosurgery 2006;59(1 suppl 1):ONSE169–70 [DOI] [PubMed] [Google Scholar]
- 2.Arat A, Cekirge S, Saatci I, et al. Transvenous injection of Onyx for casting of the cavernous sinus for the treatment of a carotid-cavernous fistula. Neuroradiology 2004;46:1012–15 [DOI] [PubMed] [Google Scholar]
- 3.Suzuki S, Lee DW, Jahan R, et al. Transvenous treatment of spontaneous dural carotid-cavernous fistulas using a combination of detachable coils and Onyx. AJNR Am J Neuroradiol 2006;27:1346–49 [PMC free article] [PubMed] [Google Scholar]
- 4.Pierot L, Januel AC, Herbreteau D, et al. Endovascular treatment of brain arteriovenous malformations using Onyx: preliminary results of a prospective multicenter study. Intervent Neuroradiol 2005;11(suppl 1):159–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Numan F, Omeroglu A, Kara B, et al. Embolization of peripheral vascular malformations with ethylene vinyl alcohol copolymer (Onyx). J Vasc Interv Radiol 2004;15:939–46 [DOI] [PubMed] [Google Scholar]
- 6.Kohout MP, Hansen M, Pribaz JJ, et al. Arteriovenous malformations of the head and neck: natural history and management. Plast Reconstr Surg 1998;102:643–54 [DOI] [PubMed] [Google Scholar]
- 7.Berenguer B, Burrows PE, Zurakowski D, et al. Sclerotherapy of craniofacial venous malformations: complications and results. Plast Reconstr Surg 1999;104:1–11 [PubMed] [Google Scholar]
- 8.Han MH, Seong SO, Kim HD, et al. Craniofacial arteriovenous malformation: preoperative embolization with direct puncture and injection of n-butyl cyanoacrylate. Radiology 1999;211:661–66 [DOI] [PubMed] [Google Scholar]
- 9.Persky MS, Yoo HJ, Berenstein A. Management of vascular malformations of the mandible and maxilla. Laryngoscope 2003;113:1885–92 [DOI] [PubMed] [Google Scholar]
- 10.Gobin YP, Murayama Y, Milanese K, et al. Head and neck hypervascular lesions: embolization with ethylene vinyl alcohol copolymer–laboratory evaluation in swine and clinical evaluation in humans. Radiology 2001;221:309–17 [DOI] [PubMed] [Google Scholar]
- 11.Whiteside OJ, Monksfield P, Steventon NB, et al. Endovascular embolization of a traumatic arteriovenous fistula of the superficial temporal artery. J Laryngol Otol 2005;119:322–24 [DOI] [PubMed] [Google Scholar]
- 12.Berenstein A, Lasjaunias P, terBrugge K. Traumatic Arteriovenous Fistulae. Surgical Neuroangiography. Volume 2: Clinical and Endovascular Treatment Aspects in Adults. 2nd ed. New York: Springer-Verlag;2004. :277–364
- 13.Ahn HS, Kerber CW, Deeb ZL. Extra- to intracranial arterial anastomoses in therapeutic embolization: recognition and role. AJNR Am J Neuroradiol 1980;1:71–75 [PMC free article] [PubMed] [Google Scholar]
- 14.Jahan R, Murayama Y, Gobin YP, et al. Embolization of arteriovenous malformations with Onyx: clinicopathological experience in 23 patients. Neurosurgery 2001;48:984–95 [DOI] [PubMed] [Google Scholar]
- 15.Luo CB, Teng MM, Chang FC, et al. Transarterial balloon-assisted n-butyl-2-cyanoacrylate embolization of direct carotid cavernous fistulas. AJNR Am J Neuroradiol 2006;27:1535–40 [PMC free article] [PubMed] [Google Scholar]
- 16.Firat M, Dincer C, Cerezci I, et al. Treatment of a giant orbitofacial vascular malformation and ophthalmic artery aneurysms with intralesion glue injections: case report. AJNR Am J Neuroradiol 2001;22:1419–23 [PMC free article] [PubMed] [Google Scholar]
- 17.Duffner F, Ritz R, Bornemann A, et al. Combined therapy of cerebral arteriovenous malformations: histological differences between a non-adhesive liquid embolic agent and n-butyl 2-cyanoacrylate (NBCA). Clin Neuropathol 2002;21:13–17 [PubMed] [Google Scholar]