Abstract
The Centers for Disease Control and Prevention, the U.S. Food and Drug Administration, and state and local health departments have begun an investigation into the lung injury attributed to the use of electronic cigarette (e-cigarette) or vaping products. A clinical case of a 24-year-old man who used e-cigarette products regularly and presented with shortness of breath, productive cough, chest pain, and fever for 1 week was discussed. Radiographic and CT findings in that patient were reviewed. Recent cases of e-cigarette–associated lung injury from the literature were summarized to continue the dialogue and encourage radiologists to research this relatively new and specific type of lung injury.
© RSNA, 2019
Summary
Radiologists will continue to play an important role in understanding and interpreting radiologic findings of lung injury in those with a history of using e-cigarette or vaping products.
Key Points
■ The diagnosis of lung injury due to e-cigarette use should be a differential possibility in patients presenting with bilateral lung opacities on radiographs or ground-glass opacities on chest CT images and exposure to e-cigarette products within 90 days of the presentation.
■ It is crucial that radiologists drive some of the research initiatives to better understand the mechanisms of disease presentation, facilitating the diagnosis and management of patients with a history of vaping.
Introduction
Several authorities, including the Centers for Disease Control and Prevention (CDC), the U.S. Food and Drug Administration, and state and local health departments, have started an investigation into the perceived widespread outbreak of lung injury attributed to the use of electronic cigarette (e-cigarette) or vaping products, or EVALI. The CDC has been monitoring the number of cases reported since March 2019. As of October 15, 2019, 1479 cases have been reported to the CDC from 49 states, the District of Columbia, and one U.S. territory, of which 33 have resulted in death (1). However, these numbers likely underestimate the true incidence and prevalence of disease due to lack of recognition and reporting of vaping-associated lung injury.
E-cigarettes act by delivering nicotine, flavorings, and other additives in aerosol form (2). They were introduced in the United States around 2007 and since 2017 are the most commonly used form of tobacco among U.S. youths (2). In fact, some vaping products are so popular among teenagers that they have resulted in the coining of new words. For example, JUULing refers to the use of the e-cigarette brand JUUL, which looks like a USB memory stick and is easily concealed. Another new verb used by teenagers for the use of electronic nicotine delivery systems is ripping.
Since 2012, several cases reported in the literature have raised the awareness of the potential link between e-cigarette use and lung injury (3–9). A recently published case series of lung injury associated with e-cigarette use in the states of Illinois and Wisconsin (10) identified 53 individuals meeting case criteria. There was one death among the cases. Most of the patients in this series were male (n = 44, 83%), with an overall median age of 19 years (age range, 16–53 years). Fifty-two patients (98%) presented with respiratory symptoms, which were present for a median duration of 6 days before hospitalization. Common respiratory symptoms included shortness of breath (n = 46, 87%), cough (n = 44, 83%), and chest pain (n = 29, 55%). Fever was noted in 29% of the cases (n = 15) at presentation. Tachycardia and tachypnea were also commonly noted (n = 34 and 22, 64% and 43%, respectively). Elevated white cell count was seen in 45 cases (87%), with an interquartile range of values between 12.30 and 18.10 × 109/L. About 45% of the patients (n = 24) were given empirical antibiotic therapy for presumed respiratory infection. Prevalence of imaging findings is confounded by the epidemiologic definition of a case; notwithstanding, opacities were noted to involve both lungs in all cases. Forty-eight of the 53 patients also underwent chest CT; ground-glass opacities with subpleural sparing were characteristically found. Complications such as pleural effusions, pneumothorax, and pneumomediastinum occurred in eight of the 48 patients who underwent CT. Basilar predominance also seems to be a frequent feature (11).
However, these cases are by no means comprehensive, and the publicly available data may represent only the tip of the iceberg. Additionally, the long-term effect of decades’ worth of use of electronic nicotine delivery systems on the lungs and other organ systems is unknown. This special report aims to raise awareness of the presentation of vaping-associated lung disease. We illustrate some of the radiographic and CT findings of lung injury with a clinical case of a 24-year-old male patient with past medical history of asthma, who presented with shortness of breath, productive cough, chest pain, and fever for 1 week. He reported current everyday use of e-cigarettes (with tobacco) and marijuana, without substantial change in recent vaping habits. He had a white cell count of 18.1 × 109/L (normal reference [NR], 4.2–10.3 × 109/L) and a platelet count of 464 × 109/L (NR, 160–383 × 109/L). His chest radiograph on admission is shown in Figure 1.
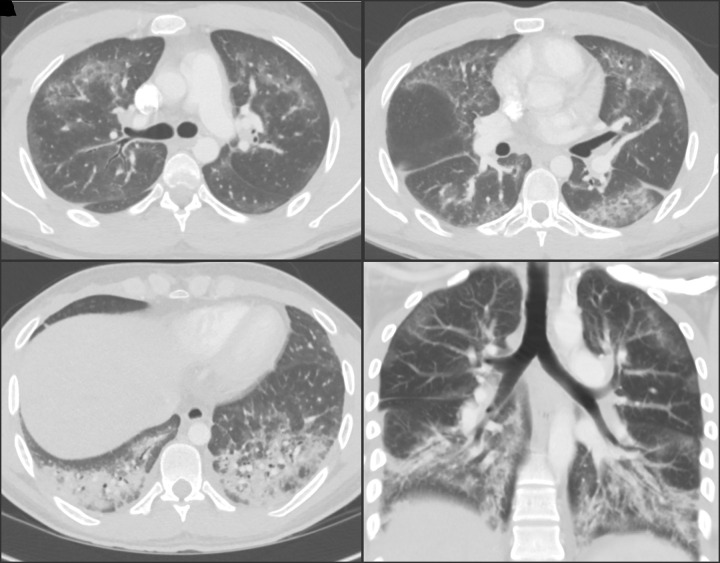
Figure 1:
Posteroanterior chest radiograph in a 24-year-old man with a history of e-cigarette use shows bilateral reticular and predominantly ground-glass and airspace opacities distributed throughout both lower lungs and absence of pleural effusions.
The radiologic findings included bilateral basilar predominant ground-glass and reticular opacities with smaller areas of consolidation. The patient was given empirical antibiotic therapy with standard dose of azithromycin for a presumptive diagnosis of pneumonia. Test results for human immunodeficiency virus and respiratory viruses were negative. Chest CT angiography was performed on the following day for exclusion of pulmonary embolism given the lack of clinical improvement with the empirical treatment and elevated d-dimer level (0.54 μ/mL, NR ≤ 0.50 μ/mL) (Fig 2).
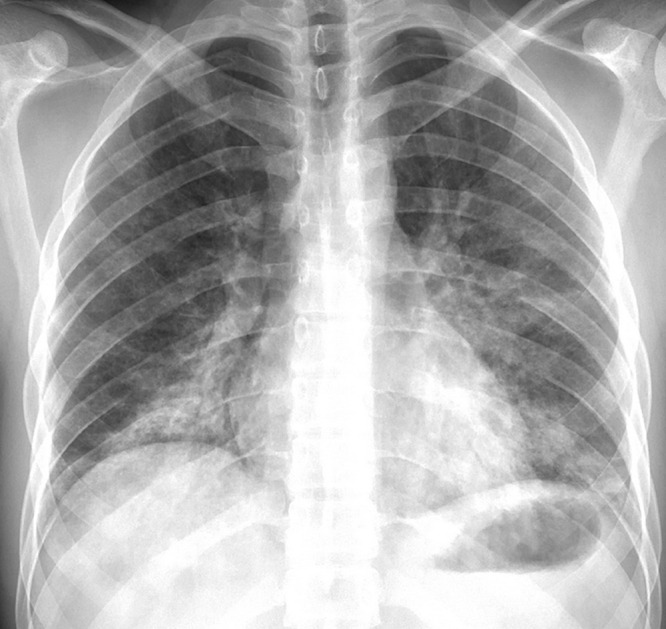
Figure 2:
Chest CT angiographic images in a 24-year-old man with a history of e-cigarette use. A–C, Selected axial sections of the lung presented on lung windows reveal patchy ground-glass opacities distributed bilaterally with some, A, B, subpleural sparing and, C, consolidation in the lung bases. D, Coronal oblique thick-slab average intensity reconstruction shows the predominance of the findings in the basal lungs and demonstrates the peripheral subpleural sparing.
The study was negative for pulmonary embolism; pulmonary findings included several differential diagnoses, such as acute interstitial pneumonia and diffuse alveolar damage. Sputum and blood cultures were negative. The rheumatologic panel result was unrevealing. Histologic specimens obtained from the right lower lobe at transbronchial biopsy revealed positive staining for lipid by Oil Red O, suggestive of lipoid pneumonia. The patient was given steroids with a presumptive diagnosis of lung injury associated with e-cigarette use.
Currently, the epidemiologic case definition of lung injury associated with e-cigarette use for surveillance purposes includes the presence of all of the following criteria: (a) use of e-cigarette or dabbing (butane hash oils) within 90 days before symptom onset; (b) presence of pulmonary opacities on chest radiographs or ground-glass opacities on chest CT images; (c) absence of pulmonary infection at initial workup; and (d) no evidence of alternative plausible diagnoses (1). The case report exemplified in this article shares many of the clinical and radiologic features found in the Wisconsin and Illinois cases series (10,11). The combination of acute respiratory symptoms with fever and leukocytosis initially raised the suspicion for infection, which was subsequently excluded on further examination. Imaging findings on the chest radiograph were nonspecific, consisting of bilateral and basilar predominant opacities, which were further confirmed to represent a combination of ground-glass opacities and consolidation at CT. Interestingly, we also observed relative preservation of the subpleural regions of the lungs, a feature identified by Henry et al in the Wisconsin and Illinois series (11). It is plausible to hypothesize that such a phenomenon could be related to the main involvement of the central aspect of the secondary pulmonary lobule, as this is believed to represent a response to an inhaled agent.
The pathophysiology of vaping-associated lung injury remains unknown. According to data collected by the CDC, most cases reported exposure to cannabinoid products (tetrahydrocannabinol and cannabidiol), although some cases have reported nicotine exposure alone (1). Prior reports have directly linked the inhalation of derivatives of marijuana to acute lung injury (5,12,13). These cases clinically manifested with acute respiratory distress and hemoptysis. At least in one case, bronchoscopy results revealed diffuse alveolar hemorrhage and organizing pneumonia (5). Many other elements found in e-cigarette products have also been found to pose potential health risks (14). Lipids present in aerosols derived from e-cigarettes could play a role in the development of lipoid pneumonia (15,16). On September 5, 2019, the New York State Department of Health announced the discovery of high vitamin E acetate concentrations in cannabis-containing samples of vape products submitted for testing, which is a nonapproved additive according to state regulations (17). In a recent series of six patients from the state of Utah, Maddock et al (16) underscored the consistent finding of lipid-laden macrophages stained by Oil Red O in the bronchoalveolar lavage, with numbers ranging from 25% to more than 75% of the sample. In another study, Butt et al (18) reviewed the pathologic slides of a series of 17 patients from the Mayo Clinic Network meeting epidemiologic criteria for vaping-related lung injury according to the CDC. Although accumulation of foamy macrophages centered in the airways with vacuolization of type 2 pneumocytes was an omnipresent finding, diverse patterns were seen at histology, including acute fibrinous pneumonitis, diffuse alveolar damage, organizing pneumonia, interstitial edema, intra-alveolar fibrin, and reactive type 2 pneumocyte hyperplasia. In contrast to prior articles, the authors did not find direct histopathologic evidence of exogenous lipoid pneumonia in the specimens, raising question about the potential causative role of lipids. Radiologically, cases of vaping-related lung injury resemble lipoid pneumonia, consisting of bilateral ground-glass opacities or consolidations in a segmental or lobar distribution, predominantly distributed in the middle and lower lobes (19). Although classic cases are expected to show low CT numbers within the opacities (eg, −30 HU), this appearance can be confounded by the presence of inflammation and differences in the amount of exogenous lipoid material. Current CDC recommendations state that, when obtained, bronchoalveolar lavage and fresh biopsy specimens should be subject to lipid staining (1).
Radiologists will continue to play an important role in recognizing this emerging entity. This diagnosis should be listed as a differential possibility in patients presenting with bilateral lung opacities on radiographs or ground-glass opacities on chest CT images and exposure to e-cigarette products within 90 days of the presentation. Subpleural sparring and basilar consolidation appear to be common features. It is crucial that radiologists drive some of the research initiatives to better understand the mechanisms of disease presentation, facilitating the diagnosis and management of these patients. These efforts should be done as a team effort with other specialties, including pathologists, epidemiologists, pulmonologists, and emergency physicians. We encourage the medical imaging community to produce scientific evidence and medical knowledge to help us understand the value of clinical, laboratory, and imaging criteria for the diagnosis and treatment of the disease, to help advance our collective knowledge about the effects of e-cigarette use on the lungs and other organ systems.
Disclosures of Conflicts of Interest: S.A. Activities related to the present article: disclosed no relevant relationships. Activities not related to the present article: institution receives grant from CIPRIT; author receives royalties from Elsevier for authoring textbooks. Other relationships: disclosed no relevant relationships. F.U.K. disclosed no relevant relationships.
Abbreviations:
- CDC
- Centers for Disease Control and Prevention
- NR
- normal reference
References
- 1.U.S. Centers for Disease Control and Prevention . Outbreak of Lung Injury Associated with E-Cigarette Use, or Vaping. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html. Published 2019. Accessed October 2019.
- 2.U.S. Department of Health and Human Services, Office of the Surgeon General . E-Cigarette Use Among Youth and Young Adults: A Report of the Surgeon General. https://www.cdc.gov/tobacco/data_statistics/sgr/e-cigarettes/pdfs/2016_sgr_entire_report_508.pdf. Published 2016. Accessed October 2019.
- 3.McCauley L, Markin C, Hosmer D. An unexpected consequence of electronic cigarette use. Chest 2012;141(4):1110–1113. [DOI] [PubMed] [Google Scholar]
- 4.Thota D, Latham E. Case report of electronic cigarettes possibly associated with eosinophilic pneumonitis in a previously healthy active-duty sailor. J Emerg Med 2014;47(1):15–17. [DOI] [PubMed] [Google Scholar]
- 5.He T, Oks M, Esposito M, Steinberg H, Makaryus M. “Tree-in-Bloom”: Severe Acute Lung Injury Induced by Vaping Cannabis Oil. Ann Am Thorac Soc 2017;14(3):468–470. [DOI] [PubMed] [Google Scholar]
- 6.Khan MS, Khateeb F, Akhtar J, et al. Organizing pneumonia related to electronic cigarette use: A case report and review of literature. Clin Respir J 2018;12(3):1295–1299. [DOI] [PubMed] [Google Scholar]
- 7.Sommerfeld CG, Weiner DJ, Nowalk A, Larkin A. Hypersensitivity Pneumonitis and Acute Respiratory Distress Syndrome From E-Cigarette Use. Pediatrics 2018;141(6):e20163927. [DOI] [PubMed] [Google Scholar]
- 8.Arter ZL, Wiggins A, Hudspath C, Kisling A, Hostler DC, Hostler JM. Acute eosinophilic pneumonia following electronic cigarette use. Respir Med Case Rep 2019;27:100825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anderson RP, Zechar K. Lung injury from inhaling butane hash oil mimics pneumonia. Respir Med Case Rep 2019;26:171–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Layden JE, Ghinai I, Pray I, et al. Pulmonary Illness Related to E-Cigarette Use in Illinois and Wisconsin - Preliminary Report. N Engl J Med 2019 Sep 6 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 11.Henry TS, Kanne JP, Kligerman SJ. Imaging of Vaping-Associated Lung Disease. N Engl J Med 2019;381(15):1486–1487. [DOI] [PubMed] [Google Scholar]
- 12.Gilbert CR, Baram M, Cavarocchi NC. “Smoking wet”: respiratory failure related to smoking tainted marijuana cigarettes. Tex Heart Inst J 2013;40(1):64–67. [PMC free article] [PubMed] [Google Scholar]
- 13.Hashmi HR, Duncalf R, Khaja M. A Case Report of Cannabis Induced Hemoptysis. Medicine (Baltimore) 2016;95(13):e3232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burstyn I. Peering through the mist: systematic review of what the chemistry of contaminants in electronic cigarettes tells us about health risks. BMC Public Health 2014;14(1):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davidson K, Brancato A, Heetderks P, et al. Outbreak of Electronic-Cigarette-Associated Acute Lipoid Pneumonia - North Carolina, July-August 2019. MMWR Morb Mortal Wkly Rep 2019;68(36):784–786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maddock SD, Cirulis MM, Callahan SJ, et al. Pulmonary Lipid-Laden Macrophages and Vaping. N Engl J Med 2019;381(15):1488–1489. [DOI] [PubMed] [Google Scholar]
- 17.New York State Department of Health . New York State Department of Health Announces Update on Investigation into Vaping-Associated Pulmonary Illnesses. https://www.health.ny.gov/press/releases/2019/2019-09-05_vaping.htm. Published September 5, 2019. Accessed October 10, 2019.
- 18.Butt YM, Smith ML, Tazelaar HD, et al. Pathology of Vaping-Associated Lung Injury. N Engl J Med 2019 Oct 2 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 19.Betancourt SL, Martinez-Jimenez S, Rossi SE, Truong MT, Carrillo J, Erasmus JJ. Lipoid pneumonia: spectrum of clinical and radiologic manifestations. AJR Am J Roentgenol 2010;194(1):103–109. [DOI] [PubMed] [Google Scholar]