Abstract
Purpose
To evaluate the influence of applying nitroglycerin (NTG) on detecting significant coronary artery disease (CAD) and NTG-induced coronary vasodilation using coronary MR angiography in patients suspected of having CAD.
Materials and Methods
In this prospective study conducted from November 2017 to September 2018, 70 consecutive participants suspected of having CAD were recruited. Of those, 57 patients successfully underwent pre- and post-NTG coronary MR angiography, both of which were performed during the end-systolic phase of the cardiac cycle. Significant coronary stenosis was defined at x-ray coronary angiography as stenosis of 50% or more. Participants were divided into a significant CAD group (significant stenosis) and nonsignificant CAD group (no significant stenosis) based on x-ray coronary angiography. Paired and unpaired Student t, generalized linear mixed model, and McNemar tests were used.
Results
The diagnostic performance of coronary MR angiography was significantly improved after NTG (P < .001). Per-patient for coronary MR angiography, from before to after NTG, respectively, the sensitivity was 97.6% (95% confidence interval [CI]: 85.6%, 99.9%) to 97.6% (95% CI: 85.6%, 99.9%), specificity was 25.0% (95% CI: 8.3%, 52.5%) to 62.5% (95% CI: 35.9%, 83.7%), positive predictive value was 76.9% (95% CI: 62.8%, 87.0%) to 87.0% (95% CI: 73.0%, 94.6%), negative predictive value was 80.0% (95% CI: 29.9%, 98.9%) to 90.9% (95% CI: 57.1%, 99.5%), and accuracy was 77.2% (95% CI: 66.3%, 88.1%) to 87.7% (95% CI: 79.2%, 96.3%). The NTG-induced coronary vasodilation was significantly lower in the significant CAD group compared with the nonsignificant CAD group.
Conclusion
Administration of NTG significantly improved the diagnostic performance of coronary MR angiography for detecting significant CAD; however, NTG-induced coronary vasodilation was impaired in patients with significant CAD.
© RSNA, 2020
See also commentary by François in this issue.
Summary
Sublingual nitroglycerin could improve diagnostic performance of coronary MR angiography for detecting significant coronary artery disease; impaired nitroglycerin-induced coronary vasodilation was also helpful in assessing the severity of coronary artery disease despite the poor effect of nitroglycerin on improving image quality in such patients with impaired coronary vasodilation.
Key Points
■ Sublingual nitroglycerin should be recommended for coronary MR angiography.
■ Nitroglycerin-induced coronary vasodilation was impaired in patients with significant coronary artery disease.
Introduction
MRI is a promising noninvasive technique for evaluating coronary artery disease (CAD) (1). For patients with CAD, coronary arterial function has a key influence on the development, progression, and clinical symptoms of the disease (2). Normal vascular tissue releases nitric oxide, which plays a pivotal role in the vasodilation of vascular smooth muscle (3). Impaired endothelium-dependent vasodilation has been regarded as an early step in the progression of atherosclerosis (4). Exogenous nitroglycerin (NTG) could induce smooth muscle cell–dependent vasodilation by providing endothelium-independent nitric oxide. Nitrate-induced coronary vasodilation could help improve the visibility of the coronary arteries (5,6). For coronary CT angiography, administration of NTG could help improve diagnostic performance and the visibility of the coronary arteries. Moreover, NTG administration has been recommended in some guidelines (7,8). One study reported that sublingual isosorbide dinitrate improved the signal-to-noise ratio and image quality of coronary MR angiography (5). However, the influence of NTG on diagnostic performance of coronary MR angiography for CAD has not been determined in a relatively large number of patients with CAD. Furthermore, coronary vasodilation may be reduced in patients with CAD, which may largely eliminate the effect of NTG on improving image quality.
Historically, x-ray coronary angiography (CAG) and intravascular US have been performed for assessing coronary vasodilation; however, because these methods are invasive, they are not suitable for widespread application (9). Because it does not use radiation or a contrast agent and because it is noninvasive, coronary MR angiography is safe for repetitive acquisition and measurement. The severe calcification evident at CT always results in blooming artifact, which may obscure the relevant vessel lumen. Coronary MR angiography may be helpful in evaluating heavily calcified coronary arteries (10). Although nitrate-induced coronary vasodilation has been assessed with coronary MR angiography in previous studies, most of those studies used volume-targeted coronary MR angiography acquisition confined to the limited coverage of a single coronary artery, a technique that is less commonly used in current clinical practice (6,11–13). In addition, due to the increase in heart rate after applying NTG, previous studies usually performed pre- and post-NTG coronary MR angiography during different phases of the cardiac cycle (6,9,14), which may affect the accurate assessment of coronary vasodilation.
This study was designed to evaluate the influence of NTG on the diagnostic performance of coronary MR angiography for detecting significant CAD using noncontrast whole-heart coronary MR angiography at 1.5 T, with CAG as the reference standard. However, we also wanted to assess the difference in NTG-induced coronary vasodilation between patients with significant CAD and patients with nonsignificant CAD. Taking into consideration the increased heart rate after applying NTG, we took care to perform the coronary MR angiography during the systolic phase both before and after administering NTG.
Materials and Methods
Participants
During November 2017 to September 2018, 70 consecutive participants suspected of having CAD and with referral for CAG were recruited. Our hospital committee on clinical investigation approved our study protocol. Each participant provided written consent before examination. Exclusion criteria were severe arrhythmias, unstable angina, prior myocardial infarction, coronary stents or bypass grafts, and contraindications for MRI examination and NTG, such as claustrophobia and hypotension. Neither β-blockers nor contrast material were used in our study, with the exception of patients who had used a β-blocker before the MRI examination according to clinical needs. All patients were trained to maintain regular breathing during coronary MR angiography acquisition.
Coronary MR Angiography Acquisition
Whole-heart three-dimensional coronary MR angiography was performed using a 1.5-T scanner (Magnetom Aera; Siemens Healthcare, Erlangen, Germany) equipped with quantum gradients (maximum strength, 45 mT/m; slew rate, 200 mT/m/sec) and an 18-channel body phased-array surface coil. All participants were in a supine position during examination. Initially, free-breathing single-slice coronal scout imaging was performed using steady-state free precession to observe the movement of the diaphragm and heart, after which four-chamber cine imaging during free-breathing was performed to monitor the movement of the right coronary artery. To obtain real-time respiratory gating, a cardiac pencil-beam navigator was placed on the right diaphragm to generate a navigator echo with a gating window of 5 mm. The acquisition window and trigger delay time were determined based on a period of minimal right coronary artery motion during systole. Coronary MR angiography acquisition was done during the systolic phase in all participants using steady-state free precession (repetition time msec/echo time msec, 3.3/1.5; 90° flip angle; field of view, 320 × 240 mm; acquisition matrix, 320 × 216; reconstructed matrix, 640 × 432; slice thickness, 1.0 mm). We employed a generalized autocalibrating partially parallel acquisition technique (GRAPPA, Siemens Healthcare) with factor of two.
After performing pre-NTG coronary MR angiography, 0.4 mg sublingual NTG (Nitrolingual; G. Pohl-Boskamp, Itohenlockstedt, Germany) was administered to the participant. The free-breathing coronal scout imaging and four-chamber cine imaging were performed respectively at 4 to 6 minutes after administration of NTG. The acquisition window and trigger delay time were determined as before administration of NTG. We also performed the post-NTG coronary MR angiography during the systolic phase using the same sequence as for the pre-NTG acquisition. Heart rate was monitored throughout the study. Blood pressure was measured by cuff sphygmomanometer before and 2 minutes after the administration of NTG in all participants. To suppress abdominal movement, all patients wore a tight-fitting medical abdominal belt around the rib cage.
X-ray Coronary Angiography
All participants underwent CAG within 5 days after coronary MR angiography. The result of CAG was evaluated using quantitative coronary angiography (QCA; Siemens Healthcare) by the consensus of two experienced cardiologists (C.G.L.) blinded to the result of coronary MR angiography. The 15-segment American Heart Association classification system was used (15). Intracoronary administration of NTG was used routinely for all patients during CAG. Reduction in luminal diameter of 50% or more was defined as significant stenosis of the coronary arteries. Coronary segments with a reference diameter of less than 2 mm were excluded. For occluded vessels, the distal segments were not analyzed at CAG, although collateral flow existed.
Coronary MR Angiography Analysis
The original coronary MR angiographic images were transferred to an independent postprocessing workstation (Leonardo VD10B; Siemens Healthcare). Original images and the relevant postprocessed images were assessed independently by the two experienced radiologists (S.H.Z. and Y.Y.C.) blinded to the patient information. The result of coronary MR angiography was evaluated by visual assessment. A different diagnosis between the two radiologists was solved with consensus reading. The coronary arteries were evaluated according to the 15-segment American Heart Association classification (15). Reduction in luminal diameter of 50% or more was defined as significant stenosis. Coronary segments with luminal diameter of less than 2 mm were excluded. In our study, nonassessable segments at coronary MR angiography were considered to have a significant stenosis, while these segments could be assessed at CAG. For occluded vessels, we analyzed only the adjacent proximal segments; the distal segments were not analyzed at coronary MR angiography, although collateral flow existed. Image quality of every coronary segment was graded visually on a four-point scale (1 = poor [severe artifacts], 2 = moderate [moderate artifacts], 3 = good [mild artifacts], 4 = excellent [no artifact]).
Luminal diameter was measured in the proximal segment with an optimal multiplanar reformatted plane along the long axis of the coronary artery and measured in consensus by the two radiologists blinded to NTG status. The selected position to measure luminal diameter before and after NTG should be corresponding with careful matching of the surrounding structures and the distance from the coronary origin to the selected position. Coronary vasodilation was calculated as: coronary vasodilation = (Dpost − Dpre)/Dpre × 100%, where Dpre and Dpost are the luminal diameter before NTG and after NTG, respectively.
Statistical Analysis
All statistical analysis was performed using statistical software (IBM SPSS Statistics 25.0; Armonk, NY). The results of quantitative variables were presented as mean ± standard deviation. With CAG as the reference standard, the diagnostic performance of coronary MR angiography for detecting significant CAD was calculated on per-patient, per-vessel, and per-segment analysis, including sensitivity, specificity, positive predictive value, negative predictive value, and accuracy with 95% confidence intervals. The McNemar test was used to compare the indexes of diagnostic performance of coronary MR angiography on per-patient, per-vessel, and per-segment analysis. A generalized linear mixed model was also used to compare the indexes of diagnostic performance of coronary MR angiography on per-patient analysis. For performing the model, the coronary segments and participants were regarded as subject variables, in which the coronary segments were nested within per-subject and the subject was set as random effect while the application of NTG and coronary segment were fixed effects. A χ2 test was used to compare the number of failures in which it was not possible to complete coronary MR angiography acquisition between pre- and post-NTG. The interobserver agreement of diagnostic performance of coronary MR angiography was evaluated by κ test on a per-patient basis. The paired Student t test was used to compare heart rate, navigator efficiency, blood pressure, trigger delay time, duration of acquisition window, and acquisition time between pre- and post-NTG coronary MR angiography. The image quality between pre- and post-NTG coronary MR angiography was presented as mean value ± standard deviation and constituent ratio, which were compared using the nonparametric paired Wilcoxon signed rank test and a χ2 test, respectively. The participants were divided into a significant CAD group (significant stenosis) and a nonsignificant CAD group (no significant stenosis) based on CAG. Vessel diameter before NTG and coronary vasodilation between the two groups were compared using an unpaired Student t test. Coronary vasodilation between the participants using β-blockers and the participants not using β-blockers was compared using an unpaired Student t test. A P value of less than .05 was considered a statistically significant difference.
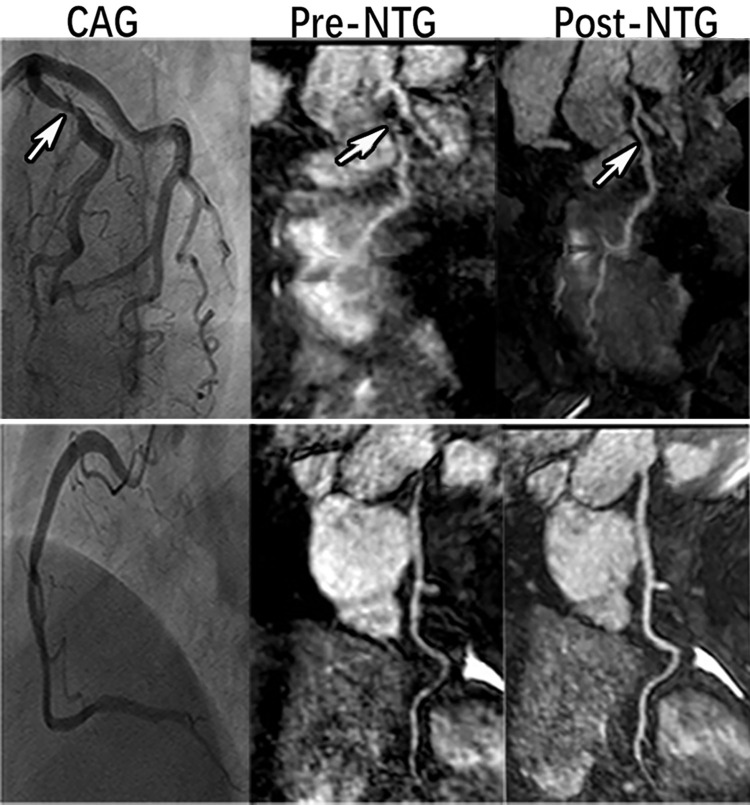
Results
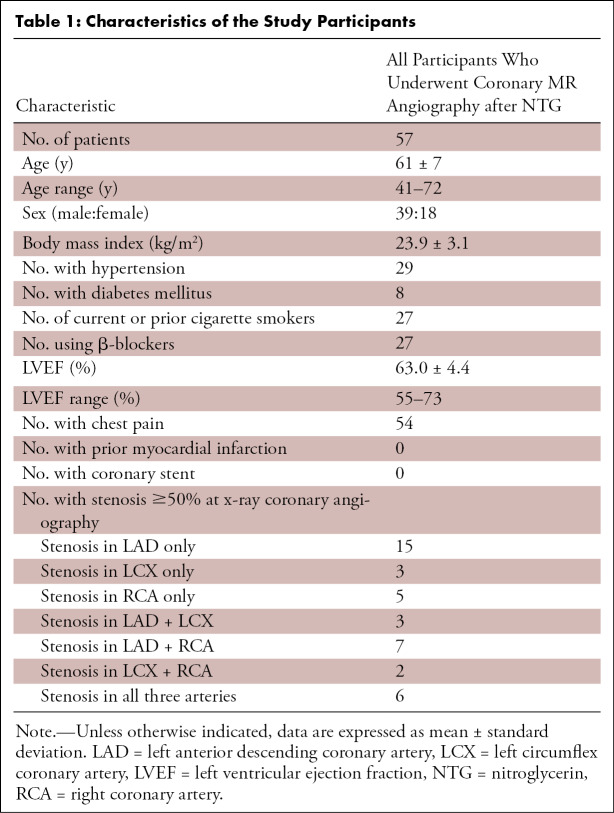
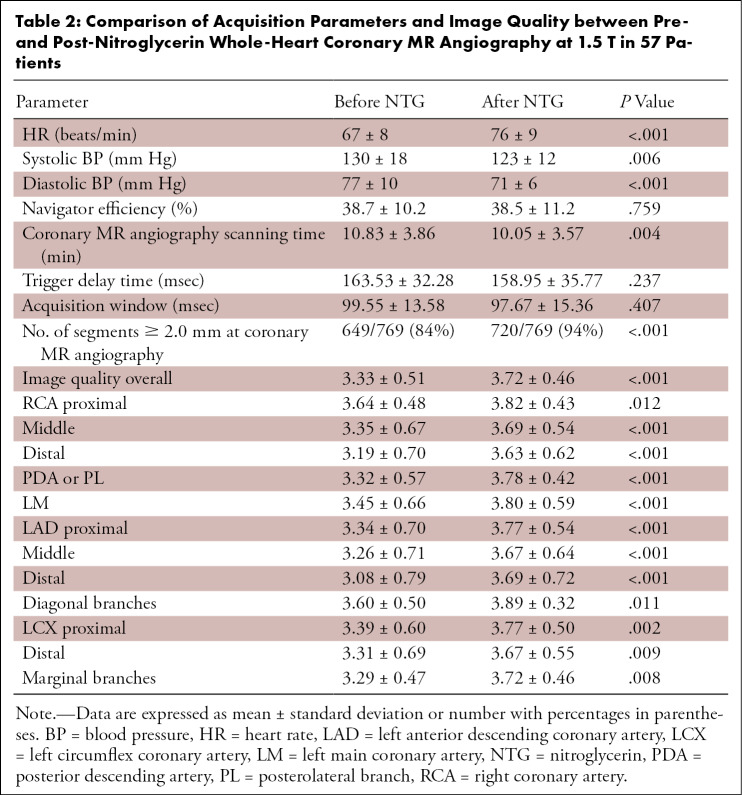
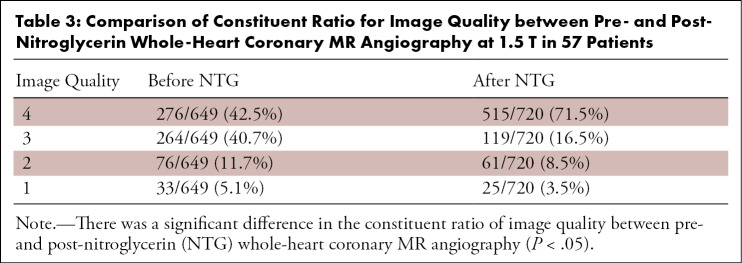
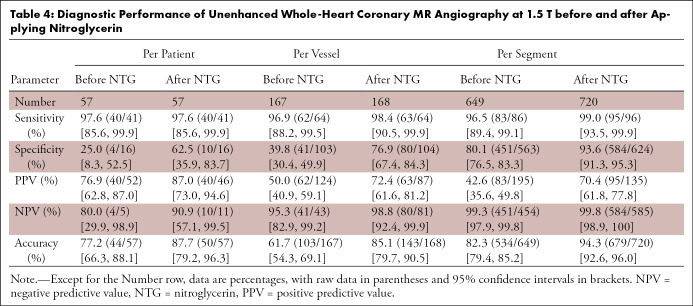
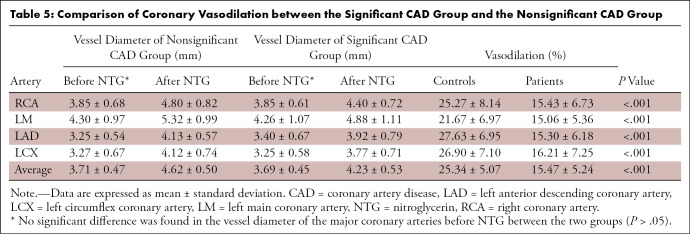
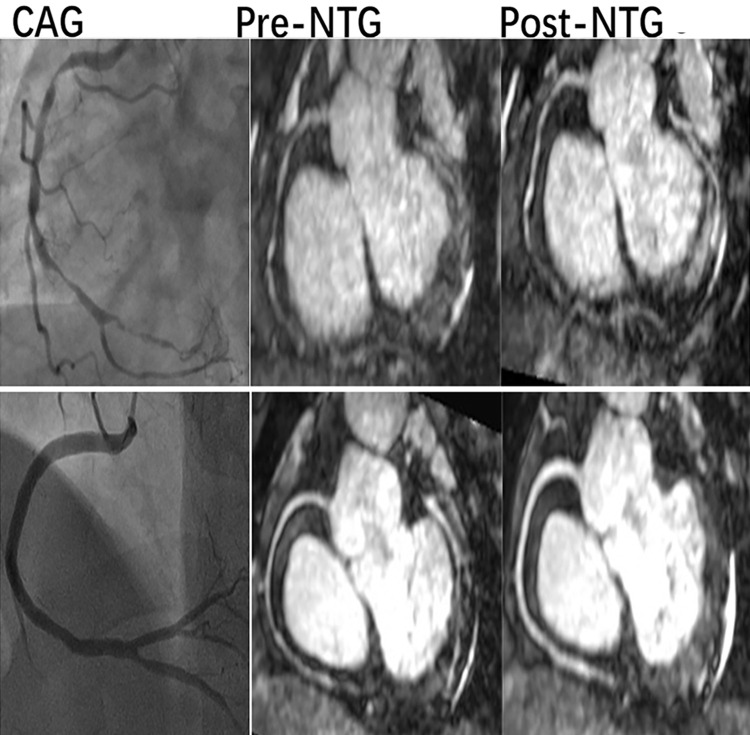
Table 1 summarizes the characteristics of the study participants. Sixty-five (93%) of 70 patients successfully underwent pre-NTG coronary MR angiography, and the post-NTG coronary MR angiography was successfully completed in 57 (88%) of 65 patients. Five participants did not finish pre-NTG coronary MR angiography due to the extremely low navigator efficiency (<20%) resulting from irregular breathing pattern. Two patients had anomalous origin of the right coronary artery, which was validated with CAG. Post-NTG coronary MR angiography was not successfully completed in six participants due to long scanning time. In addition, due to symptoms of dizziness, post-NTG coronary MR angiography was not acquired in two participants whose dizziness was not severe and which subsided spontaneously after resting. The number of failures after NTG was not significantly different from the number of failures before NTG (P > .05). Comparison of acquisition parameters and image quality between pre- and post-NTG coronary MR angiography is shown in Table 2. There was a significant difference in the constituent ratio of image quality between pre- and post-NTG coronary MR angiography (P < .05), as shown in Table 3. There was no significant difference in navigator efficiency, trigger delay time, or acquisition window (P > .05). The image quality scores and heart rate were increased significantly at post-NTG coronary MR angiography (P < .05). The scanning time and blood pressure decreased significantly after the administration of NTG (P < .05). Use of CAG showed 769 segments with a diameter of greater than or equal to 2 mm. There were eight patients, 37 vessels, and 116 segments with different diagnoses after applying NTG. The segments with luminal diameter of greater than or equal to 2 mm at post-NTG coronary MR angiography were significantly increased compared with pre-NTG imaging (P < .05). Using the McNemar test, we found that the indexes of diagnostic performance, including specificity, positive predictive value, negative predictive value, and accuracy, were significantly increased on per-vessel and per-segment analysis after NTG (P < .05) (Table 4), while the diagnostic performance was not significantly different between pre-NTG and post-NTG coronary MR angiography on per-patient analysis for the significant CAD group and the nonsignificant CAD group (P > .05), respectively. However, the diagnostic performance was significantly improved on per-patient analysis after NTG (P < .001), when using generalized linear mixed model. Figure 1 shows that the image quality and diagnostic performance were significantly improved at post-NTG coronary MR angiography compared with pre-NTG coronary MR angiography. The κ value of interobserver agreement for assessing CAD with coronary MR angiography was 0.81 on per-patient analysis. No significant difference was found in the vessel diameter of the major coronary arteries before NTG between the two groups (P > .05). The coronary vasodilation of the significant CAD group is markedly lower than that of the nonsignificant CAD group (P < .05) (Table 5, Fig 2). In addition, no significant difference was found in coronary vasodilation between the participants using β-blockers and the participants not using β-blockers (P > .05).
Table 1:
Characteristics of the Study Participants
Table 2:
Comparison of Acquisition Parameters and Image Quality between Pre- and Post-Nitroglycerin Whole-Heart Coronary MR Angiography at 1.5 T in 57 Patients
Table 3:
Comparison of Constituent Ratio for Image Quality between Pre- and Post-Nitroglycerin Whole-Heart Coronary MR Angiography at 1.5 T in 57 Patients
Table 4:
Diagnostic Performance of Unenhanced Whole-Heart Coronary MR Angiography at 1.5 T before and after Applying Nitroglycerin
Figure 1:
X-ray coronary angiography (CAG) and curved multiplanar reformatted images from coronary MR angiography before and after nitroglycerin (NTG) in a 56-year-old woman. A, CAG (arrow) shows significant stenosis in the proximal left anterior descending coronary artery (LAD). Coronary MR angiography before and after NTG also shows a significant stenosis in the proximal LAD (arrows), whereas coronary MR angiography before NTG overestimates the stenotic degree of LAD compared with CAG and does not clearly depict LAD, which was improved significantly after applying NTG. B, CAG shows no stenosis in the right coronary artery (RCA); however, coronary MR angiography before NTG detects a significant stenosis in the proximal RCA (arrowhead), which is not observed at coronary MR angiography after NTG (arrowhead).
Table 5:
Comparison of Coronary Vasodilation between the Significant CAD Group and the Nonsignificant CAD Group
Figure 2:
X-ray coronary angiography (CAG) and maximum intensity projection images of the right coronary artery (RCA) from coronary MR angiography demonstrate nitroglycerin (NTG)-induced vasodilation. A, The coronary MR angiographic images in a 50-year-old man with multiple significant stenosis in RCA show no significant coronary vasodilation, whereas the, B, coronary MR angiographic images in a 50-year-old male control without significant stenosis in RCA show significant coronary vasodilation. The decreased coronary vasodilation may eliminate the effect of NTG on improving the image quality; however, it also may indicate coronary artery disease and may still play an important role in the diagnosis of multiple significant stenosis.
Discussion
In this study, we found that the diagnostic performance of coronary MR angiography for detecting significant CAD could be significantly improved by administration of sublingual NTG. In addition, although the impaired coronary vasodilation in patients with significant CAD may largely eliminate the effect of NTG on improving image quality, NTG-induced vasodilation may still add extra value for the diagnosis given that NTG-induced vasodilation was evaluated. Much of the literature on coronary CT angiography focuses on the application of NTG during coronary CT angiography acquisition (16). To the best of our knowledge, only one other study has been performed on the diagnostic performance of NTG-coronary MR angiography (6). However, the number of patients in that study was relatively small (n = 17), and the study only recruited patients with significantly stenotic coronary artery identified at CAG before cardiac MR angiographic acquisition; however, healthy volunteers did not undergo CAG. Some indexes of diagnostic performance in that study, such as positive predictive value and specificity, seemed to be lower than those in our study and in several previous reports (17–19). Although coronary CT angiography could produce high-resolution imaging of coronary arteries, the radiation and contrast agents involved remain the major limitation in assessing NTG-induced coronary vasodilation. In part because it does not involve use of a contrast agent, coronary MR angiography is a promising noninvasive method for evaluating NTG-induced coronary vasodilation. Moreover, blooming artifact from calcification makes it difficult to make a correct diagnosis based on coronary CT angiography. A study published in 2007 demonstrated that coronary MR angiography has better diagnostic performance over coronary CT angiography for detecting significant CAD with a heavily calcified coronary lumen (20).
Currently, long acquisition time remains a major reason for limited use of coronary MR angiography in clinical practice. Many factors affect acquisition time, including heart rate, trigger delay time, acquisition window, and respiratory navigator efficiency. In our study, we acquired the coronary MR angiography acquisition during systole for pre- and post-NTG administration, which was different from previous studies (6,14); we did this out of consideration that the evaluation of coronary vasodilation may be not accurate if a different acquisition phase of the cardiac cycle is used for pre-NTG versus post-NTG or vice versa. As a result, in our study no significant difference was found in navigator efficiency, trigger delay time, and acquisition window; however, the acquisition time of coronary MR angiography was found to be slightly shortened after NTG, which was also different from previous studies (6,14). This may be due to the much larger sample size of our study and that previous studies did not strictly maintain the acquisition window in the same phase of the cardiac cycle for pre- and post-NTG coronary MR angiography. In addition, in our study increased heart rate was somewhat helpful in reducing the acquisition time post-NTG.
The coronary artery blood flow mainly occurs in diastole; however, Weissman et al (21) reported that the coronary luminal diameter and luminal area increased during mid- and late systole compared with that during diastole. It is well known that nitrates have an important effect on the luminal diameter of the coronary arteries. To improve the coronary spasm, NTG has been routinely applied in invasive cardiology (6,22). Several studies on the vasodilation effect of nitrates have been published (6,12–14,23). Coronary vasodilation is a reflection of arterial stiffness. Epidemiologic studies show arterial stiffness to be an independent predictor of future cardiovascular events, including stroke and myocardial infarction, and they show that arterial stiffness has been related to heart failure (24). For patients with CAD or relevant risk factors, dysfunction of coronary arterial reaction to the vasodilators may be related to both impaired endothelium-dependent coronary vasodilation and abnormality of endothelium-independent coronary vasodilation reaction to NTG, which is related to vascular smooth muscle cells (25). One study using intravascular US with intracoronary NTG administration suggested that the vascular reactivity to NTG is impaired in the coronary segments with atherosclerosis (26). In our study, we found that the NTG-induced coronary vasodilation of the significant CAD group was significantly lower than that of the nonsignificant CAD group for all major coronary arteries, whereas Heer et al (6) reported a significant difference in coronary vasodilation between volunteers and patients for the left main coronary artery, left anterior descending artery, and left circumflex coronary artery, with no mention of the right coronary artery; additionally, those authors did not provide the detailed percentage of coronary vasodilation for patients and volunteers or detailed comparison of coronary vasodilation. The possible reasons may be that the sample of patients was relatively small (n = 17), and those volunteers did not undergo CAG, which caused the coronary arteries status of volunteers to not be confirmed. Another study found that age may affect coronary vasodilation with NTG, although no significant difference was found in NTG-induced coronary vasodilation between patients and healthy controls (23). We speculate that this may be due to the two-dimensional MRI technique used for coronary MR angiography data acquisition and the small sample of patients with CAD (n = 6). Moreover, those healthy controls were markedly younger than patients in the two previous studies (6,23), which also may affect the evaluation of coronary vasodilation. Jin et al (9) found NTG-induced coronary vasodilator capacity to be significantly correlated with age. In our study, all participants underwent CAG, and mean age was not significantly different between the two groups, which could make us identify the actual situation of coronary arteries for every participant. Although impaired coronary vasodilation to NTG may weaken the effect of NTG on improving the image quality in patients with severe CAD, we believe that it is still helpful because it may add the diagnostic confidence in assessing the severity of CAD. However, the decreased dilation of coronary arteries detected at coronary MR angiography may provide the potential value for identifying or predicting significant CAD.
Our study had some limitations. The number of patients with significant stenosis only in the right coronary artery and left circumflex coronary artery was relatively small. Because we performed coronary MR angiography before and after NTG during the systolic phase, the total scanning time was long for some participants, with a relatively low heart rate and longer rest period during the diastolic phase. Considering the participants were suspected of having CAD, the high prevalence of significant CAD may boost the diagnostic accuracy of the coronary MR angiography. In our study, we used only 0.4 mg of NTG for each participant, whereas many centers use 0.8 mg of NTG. In addition, the results only are applied when coronary MR angiography is successful after NTG. Thus, it is helpful to apply NTG during coronary MR angiography acquisition only if the patient is a candidate for NTG administration.
In conclusion, we show that coronary MR angiography is feasible in patients with regular breathing pattern and absence of arrhythmia. The image quality and diagnostic performance of coronary MR angiography for detecting significant CAD can be significantly improved after NTG. The scanning time during coronary MR angiography acquisition was reduced after applying NTG. The NTG-induced coronary vasodilation was impaired in patients with significant CAD. Therefore, we suggest that coronary MR angiography should be performed after the administration of sublingual NTG.
Work supported by National Natural Science Foundation of China (contract grant no. 81701643) and Zhongshan Hospital Fudan University Science Foundation for Youth (contract grant no. 2017ZSQN24).
Disclosures of Conflicts of Interest: S.H.Z. Activities related to the present article: institution received grant from National Natural Science Foundation of China (grant 81701643). Activities not related to the present article: disclosed no relevant relationships. Other relationships: disclosed no relevant relationships. C.G.L. Activities related to the present article: institution received grant from National Natural Science Foundation of China (grant 81701643). Activities not related to the present article: disclosed no relevant relationships. Other relationships: disclosed no relevant relationships. Y.Y.C. Activities related to the present article: institution received grant from National Natural Science Foundation of China (grant 81701643). Activities not related to the present article: disclosed no relevant relationships. Other relationships: disclosed no relevant relationships. H.Y. Activities related to the present article: institution received grant from National Natural Science Foundation of China (grant 81701643). Activities not related to the present article: disclosed no relevant relationships. Other relationships: disclosed no relevant relationships. M.S.Z. Activities related to the present article: institution received grant from National Natural Science Foundation of China (grant 81701643). Activities not related to the present article: disclosed no relevant relationships. Other relationships: disclosed no relevant relationships. H.J. Activities related to the present article: institution received grant from National Natural Science Foundation of China (grant 81701643). Activities not related to the present article: disclosed no relevant relationships. Other relationships: disclosed no relevant relationships.
S.H.Z. and C.G.L. contributed equally to this work.
Abbreviations:
- CAD
- coronary artery disease
- CAG
- x-ray coronary angiography
- NTG
- nitroglycerin
References
- 1.von Knobelsdorff-Brenkenhoff F, Schulz-Menger J. Role of cardiovascular magnetic resonance in the guidelines of the European Society of Cardiology. J Cardiovasc Magn Reson 2016;18:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ludmer PL, Selwyn AP, Shook TL, et al. Paradoxical vasoconstriction induced by acetylcholine in atherosclerotic coronary arteries. N Engl J Med 1986;315(17):1046–1051. [DOI] [PubMed] [Google Scholar]
- 3.Deanfield JE, Halcox JP, Rabelink TJ. Endothelial function and dysfunction: testing and clinical relevance. Circulation 2007;115(10):1285–1295. [DOI] [PubMed] [Google Scholar]
- 4.Bonetti PO, Lerman LO, Lerman A. Endothelial dysfunction: a marker of atherosclerotic risk. Arterioscler Thromb Vasc Biol 2003;23(2):168–175. [DOI] [PubMed] [Google Scholar]
- 5.Hu P, Chuang ML, Ngo LH, et al. Coronary MR imaging: effect of timing and dose of isosorbide dinitrate administration. Radiology 2010;254(2):401–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heer T, Reiter S, Trißler M, Höfling B, von Knobelsdorff-Brenkenhoff F, Pilz G. Effect of nitroglycerin on the performance of MR coronary angiography. J Magn Reson Imaging 2017;45(5):1419–1428. [DOI] [PubMed] [Google Scholar]
- 7.Scanlon PJ, Faxon DP, Audet AM, et al. ACC/AHA guidelines for coronary angiography: executive summary and recommendations. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Coronary Angiography) developed in collaboration with the Society for Cardiac Angiography and Interventions. Circulation 1999;99(17):2345–2357. [DOI] [PubMed] [Google Scholar]
- 8.Raff GL, Abidov A, Achenbach S, et al. SCCT guidelines for the interpretation and reporting of coronary computed tomographic angiography. J Cardiovasc Comput Tomogr 2009;3(2):122–136. [DOI] [PubMed] [Google Scholar]
- 9.Jin H, Zeng MS, Yun H, Ge MY, Ma JY, Yang S. Noninvasive test of nitrate-induced coronary vasomotion by 1.5-T whole-heart 3D magnetic resonance angiography using a T2-prepared SSFP sequence. Int J Cardiovasc Imaging 2012;28(7):1707–1716. [DOI] [PubMed] [Google Scholar]
- 10.Hundley WG, Bluemke DA, Finn JP, et al. ; American College of Cardiology Foundation Task Force on Expert Consensus Documents. ACCF/ACR/AHA/NASCI/SCMR 2010 expert consensus document on cardiovascular magnetic resonance: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. Circulation 2010;121(22):2462–2508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nguyen PK, Meyer C, Engvall J, Yang P, McConnell MV. Noninvasive assessment of coronary vasodilation using cardiovascular magnetic resonance in patients at high risk for coronary artery disease. J Cardiovasc Magn Reson 2008;10(1):28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pepe A, Lombardi M, Takacs I, Positano V, Panzarella G, Picano E. Nitrate-induced coronary vasodilation by stress-magnetic resonance imaging: a novel noninvasive test of coronary vasomotion. J Magn Reson Imaging 2004;20(3):390–394. [DOI] [PubMed] [Google Scholar]
- 13.Terashima M, Nguyen PK, Rubin GD, et al. Impaired coronary vasodilation by magnetic resonance angiography is associated with advanced coronary artery calcification. JACC Cardiovasc Imaging 2008;1(2):167–173. [DOI] [PubMed] [Google Scholar]
- 14.Jin H, Zeng MS, Ge MY, et al. Influence of applying nitroglycerin in whole-heart free-breathing 3D coronary MR angiography. AJR Am J Roentgenol 2010;194(4):927–932. [DOI] [PubMed] [Google Scholar]
- 15.Austen WG, Edwards JE, Frye RL, et al. A reporting system on patients evaluated for coronary artery disease: report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation 1975;51(suppl 4):5–40. [DOI] [PubMed] [Google Scholar]
- 16.Takx RAP, Suchá D, Park J, Leiner T, Hoffmann U. Sublingual Nitroglycerin Administration in Coronary Computed Tomography Angiography: a Systematic Review. Eur Radiol 2015;25(12):3536–3542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang Q, Li K, Liu X, et al. Contrast-enhanced whole-heart coronary magnetic resonance angiography at 3.0-T: a comparative study with x-ray angiography in a single center. J Am Coll Cardiol 2009;54(1):69–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sakuma H, Ichikawa Y, Chino S, Hirano T, Makino K, Takeda K. Detection of coronary artery stenosis with whole-heart coronary magnetic resonance angiography. J Am Coll Cardiol 2006;48(10):1946–1950. [DOI] [PubMed] [Google Scholar]
- 19.Kato S, Kitagawa K, Ishida N, et al. Assessment of coronary artery disease using magnetic resonance coronary angiography: a national multicenter trial. J Am Coll Cardiol 2010;56(12):983–991. [DOI] [PubMed] [Google Scholar]
- 20.Liu X, Zhao X, Huang J, et al. Comparison of 3D free-breathing coronary MR angiography and 64-MDCT angiography for detection of coronary stenosis in patients with high calcium scores. AJR Am J Roentgenol 2007;189(6):1326–1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Weissman NJ, Palacios IF, Weyman AE. Dynamic expansion of the coronary arteries: implications for intravascular ultrasound measurements. Am Heart J 1995;130(1):46–51. [DOI] [PubMed] [Google Scholar]
- 22.Seo MK, Koo BK, Kim JH, et al. Comparison of hyperemic efficacy between central and peripheral venous adenosine infusion for fractional flow reserve measurement. Circ Cardiovasc Interv 2012;5(3):401–405. [DOI] [PubMed] [Google Scholar]
- 23.Terashima M, Meyer CH, Keeffe BG, et al. Noninvasive assessment of coronary vasodilation using magnetic resonance angiography. J Am Coll Cardiol 2005;45(1):104–110. [DOI] [PubMed] [Google Scholar]
- 24.Kang S, Fan HM, Li J, et al. Relationship of arterial stiffness and early mild diastolic heart failure in general middle and aged population. Eur Heart J 2010;31(22):2799–2807. [DOI] [PubMed] [Google Scholar]
- 25.Schächinger V, Britten MB, Zeiher AM. Prognostic impact of coronary vasodilator dysfunction on adverse long-term outcome of coronary heart disease. Circulation 2000;101(16):1899–1906. [DOI] [PubMed] [Google Scholar]
- 26.Yamagishi M, Nissen SE, Booth DC, et al. Coronary reactivity to nitroglycerin: intravascular ultrasound evidence for the importance of plaque distribution. J Am Coll Cardiol 1995;25(1):224–230. [DOI] [PubMed] [Google Scholar]