Abstract
PURPOSE: To prospectively assess the short-term clinical outcome of patients with subacute or chronic painful osteoporotic vertebral compression fractures (VCF) treated with percutaneous vertebroplasty (PV) compared with optimal pain medication (OPM).
METHODS: Randomization of patients in 2 groups: treatment by PV or OPM. After 2 weeks, patients from the OPM arm could change therapy to PV. Patients were evaluated 1 day and 2 weeks after treatment. Visual analog score (VAS) for pain and analgesic use were assessed before, and 1 day and 2 weeks after start of treatment. Quality of Life Questionnaire of the European Foundation for Osteoporosis (QUALEFFO) and Roland-Morris Disability (RMD) questionnaire scores were assessed before and 2 weeks after start of treatment. Follow-up scores in patients requesting PV treatment after 2 weeks OPM treatment were compared with scores during their OPM period.
RESULTS: Eighteen patients treated with PV compared with 16 patients treated with OPM had significantly better VAS and used less analgesics 1 day after treatment. Two weeks after treatment, the mean VAS was less but not significantly different in patients treated with OPM, whereas these patients used significantly less analgesics and had better QUALEFFO and RMD scores. Scores in the PV arm were influenced by occurrence of new VCF in 2 patients. After 2 weeks OPM, 14 patients requested PV treatment. All scores, 1 day and 2 weeks after PV, were significantly better compared with scores during conservative treatment.
CONCLUSION: Pain relief and improvement of mobility, function, and stature after PV is immediate and significantly better in the short term compared with OPM treatment.
Percutaneous vertebroplasty (PV) consists of the percutaneous injection of bone cement, usually polymethylmethacrylate (PMMA), in a vertebral compression fracture (VCF). PV stabilizes the fractured vertebral body and provides nearly immediate reduction or relief of pain caused by the VCF. Initially patients with symptomatic primary or secondary osteolytic vertebral tumors were treated with PV. Nowadays, the main target population of PV are patients with painful, therapy-resistant osteoporotic VCF not responding to analgesics, rest, bracing, or other conservative therapies.
Studies have shown that PV is effective and safe in patients with painful osteoporotic VCF with a reported pain relief in more than 90% of patients.1–5 Although this innovative treatment exists for over 20 years, no randomized controlled trial (RCT) has been performed to assess the differences in clinical outcome between patients treated with PV and those treated with the “gold standard”: optimal pain medication (OPM).
In this prospective RCT, we assessed the short-term clinical outcome in patients with painful osteoporotic VCF treated with PV compared with patients treated with OPM.
Patients and Methods
Patients
Between July 2003 and June 2005, all patients with painful osteoporotic VCF refractive to medical therapy for at least 6 weeks and no longer than 6 months were approached to participate in the study. After informed consent, patients were randomized in 2 groups. Three hospitals took part in the study. All patients were discussed in a multidisciplinary team consisting of internists, orthopedic surgeons, and radiologists. The inclusion criteria were: 1) VCF with height loss of the vertebral body (minimal 15%) on x-ray of the spine, 2) invalidating back pain related to the VCF refractive to medical therapy for at least 6 weeks and no longer than 6 months, 3) focal tenderness on physical examination related to the level of the VCF, 4) bone attenuation T-scores less than −2.0, 5) bone marrow edema of the affected VCF on MR imaging scan of the spine, and 6) patient age 50 years or older. The patient exclusion criteria were: 1) poor cardiopulmonary condition, 2) untreatable coagulopathy, 3) ongoing systemic infection or local infection of the spine (osteomyelitis, spondylodiscitis), 4) radicular and/or myelum compression syndrome, 5) indication of other underlying disease than osteoporosis, and 6) no informed consent.
Study Protocol
The patients had had at least 1 day to consider their involvement in the study before participating. After informed consent, the patients were randomized in 2 groups by an independent central operator. One arm consisted of patients to be treated by PV and the other arm of those to be treated by OPM. The intention of the study was to follow the patients from both groups for 1 year with MR imaging scans and standardized questionnaires at serial intervals in time: 1 day, 2 weeks, and 3, 6, and 12 months after start of the study. The patients randomized in the OPM arm, who still had severe pain 2 weeks after initiating optimized analgesic treatment, could undergo PV if they wanted to (“crossover”). The OPM treatment was optimized during follow-up by the internist and/or orthopedic surgeon. Any patient could leave the study at any moment without explanation of their motivation. Institutional Review Board approval was obtained in each participating hospital.
Our original study design was changed during our trial. Because nearly all of the patients randomized in the OPM arm requested to be treated by PV 2 weeks after start of OPM treatment, we stopped the study early. Our interest was to compare the outcomes between the treatment arms. Consequently, the follow-up data from 2 weeks after the start of treatment were not analyzed in this study. The results from the patients who requested subsequent PV were analyzed 2 weeks after PV to compare these results with the results from the period during OPM treatment.
Preprocedural Imaging Protocol
Upon the detection of a VCF on the x-rays of the spine, a total spine MR imaging was performed on a 1T or 1.5T MR imaging scanner. The MR imaging sequences consisted of sagittal T1-weighted (TR, 400 ms; TE, 13 ms), T2-weighted turbo spin-echo (TSE) (TR, 3500 ms; TE, 120 ms), and short τ inversion recovery (STIR) images (TR, 2500 ms; TE, 70 ms) of the entire spinal column and transverse T2 TSE weighted images (TR, 2500 ms; TE, 120 ms) at the level of the VCF with bone marrow edema (BME). BME in the collapsed vertebral body was defined as a decreased signal intensity on T1-weighted images and an increased signal intensity on STIR images.6,7 The shape and grade of every treated VCF was scored by 2 radiologists in consensus using the semiquantitative visual grading scale of vertebral deformities according to Genant.8 The shape of VCF was classified on the basis of the reduction in anterior height (wedged), middle height (biconcave), and posterior height (crush). The grade of VCF was classified as a percentage of the height reduction in mild (15%–25%), moderate (26%–40%), and severe (>40%).
Study Population
Of approximately 1 in 4 potential study candidates, a total of 46 patients consented initially to participate in the study. Despite informed consent, 12 patients refrained from the study shortly after inclusion: 6 patients randomized for OPM actually wanted to be treated by PV, 2 patients randomized for PV actually wanted to be treated by conservative treatment, and 4 patients refused to fill out questionnaires 2 weeks after their treatment. In the end, 34 patients were enrolled in the study. Eighteen patients were randomized to be treated by PV and 16 patients by OPM.
PV Procedure
The patients were treated within 1 week after study inclusion. PV was performed under local anesthesia on a biplane (n = 2 hospital departments) or monoplane (n = 1 hospital department) angiographic unit. In most cases, a bilateral transpedicular approach was used. Under continuous fluoroscopy, PMMA bone cement (Osteopal V; Biomet Merck, Ried b. Kerzers, Switzerland) was injected manually using 1.0-mL syringes and 11- or 13-gauge bone biopsy needles (Cook Europe, Bjaeverskov, Denmark). Immediately after the PV, a CT scan with multiplanar reconstructions of the treated levels was performed to assess the cement deposition and to identify possible extra cement leakage or other local complications that might not have been noted under fluoroscopy.
Pain Medication Protocol
The pain medication was optimized according to the individual need of patients. In ascending order of anesthesia, the patients were treated with paracetamol (acetaminophen), nonsteroidal anti-inflammatory drugs (NSAIDs), or opiate derivatives. To optimize analgesic use, at first the dose per day of prescribed analgesics was regulated. Second, the class of pain medication was adjusted. Corrections were made on a daily basis by the endocrinologists on an as-needed basis.
Clinical Follow-Up
All 34 patients filled out pain questionnaires before and both 1 day and 2 weeks after PV or after initiation of OPM. All questionnaires consisted of a visual analog score (VAS) for back pain and recording of analgesic use.9 VAS was indicated on a 10-point scale ranging from 0 (no pain) to 10 (worst pain in the patient's life). The prescribed analgesic use was classified into no medication (0), use of paracetamol (1), use of NSAIDs (2), and use of opiate derivatives (3).
In addition to the scores of VAS and analgesic use, both before and 2 weeks after starting the treatment, 2 more extensive standardized questionnaires were filled out: the Quality of Life Questionnaire of the European Foundation for Osteoporosis (QUALEFFO) and the Roland-Morris Disability (RMD) questionnaire.10,11 QUALEFFO is specifically developed for patients with osteoporosis and vertebral fractures.10 QUALEFFO consists of 41 multiple choice questions in the domains pain, physical function, social function, general health perception, and mental function. The RMD questionnaire measures functional status in patients with (low) back pain.11
Statistical Analysis
The data were analyzed according to the “intention-to-treat” principle. The differences in baseline characteristics in the patients from both groups were compared using the χ2 test for categoric variables and the unpaired t test for continuous variables.
The following patient and imaging characteristics were compared in the patients from both treatment arms: patient age, sex, interval of pain related to VCF, number and spinal distribution of treated and pre-existing VCF, shape and grade of treated VCF, percentage of height loss of treated VCF, VAS for pain, and analgesic use. In addition, QUALEFFO and RMD questionnaire scores were compared. The percentage height loss of VCF was calculated by dividing the minimal vertebral height through the dorsal wall height on lateral midspinal MR imaging T1-weighted images.
The differences in VAS score, type of analgesics used, QUALEFFO total and subscores, and RMD score at the follow-up intervals in patients from each group were evaluated by linear regression analysis. Regression coefficients were calculated with corresponding 95% confidence limits.12 The changes in VAS at different points in time were assessed by subtraction of scores at both follow-up intervals. The differences in the type of analgesic use at every follow-up period were quantified by defining analgesic use as an ordinal variable from 0 (no analgesic use) to 3 (use of opiate derivatives). The paired t test was used to compare the changes in VAS and the Wilcoxon paired-sample test to compare the changes in the use of type of analgesics.
The changes in scores of QUALEFFO total scores were calculated by subtraction of the scores at 2 weeks from the initial scores. The changes in RMD scores at 2-week follow-up were calculated by subtraction of the scores at 2 weeks from the initial scores and divided by the initial score times 100 (percentage).
All scores from the standardized questionnaires 1 day and 2 weeks after PV in the patients who requested a PV treatment 2 weeks after initiating OPM (“crossover ”arm) were compared with their scores from the standardized questionnaires at 1 day and 2 weeks during their OPM period. The differences in scores in these patients were compared by the paired t test with corresponding 95% confidence limits.
Results
Clinical Outcome Treatment by PV versus Pain Medication
Of the 34 included patients, 18 were randomized for PV and 16 for OPM. Characteristics of the patients before randomization are summarized in Table 1. The randomization was successful: except for the number and shape of the treated VCF, all patient characteristics that influenced the outcome were equally distributed, including the subscores of QUALEFFO (Table 4).
Table 1:
Characteristics of the total group of patients and categorized by treatment arm: PV and OPM, before initiating therapy; P value for differences in PV versus OPM
| Total | PV | OPM | P | |
|---|---|---|---|---|
| Number of patients | 34 | 18 | 16 | |
| Age (years) | 73 (55–88) | 72 (59–84) | 74 (55–88) | .4 |
| Female sex (%) | 28 (82) | 14 (78) | 14 (88) | .5 |
| Duration of back pain | 81 (46–141) | 85 (47–138) | 76 (46–141) | .4 |
| Total number of pre-existing VCF | 108 | 59 | 48 | .5 |
| Mean (range) | 3.2 (1–8) | 3.3 (1–8) | 3.1 (1–8) | |
| Distribution of pre-existing VCF | T5–L5 | T5–L5 | T5–L5 | .5 |
| Total number of treated VCF | 49 | 28 | 21 | .04 |
| Mean (range) | 1.4 (1–3) | 1.6 (1–3) | 1.2 (1–2) | |
| Distribution of treated VCF | T6–L5 | T6–L5 | T6–L5 | .5 |
| Shape-treated VCF (%) | .02 | |||
| Wedge | 38 (78) | 25 (89) | 13 (62) | |
| Biconcave | 11 (22) | 3 (11) | 8 (38) | |
| Grade-treated VCF (%) | .1 | |||
| Mild | 6 (12) | 3 (11) | 3 (14) | |
| Moderate | 11 (22) | 6 (21) | 5 (24) | |
| Severe | 32 (65) | 19 (68) | 13 (62) | |
| Compression of treated VCF (%) | 45 (15–72) | 47 (23–72) | 42 (15–68) | .3 |
| Initial VAS for pain | 7.3 (5–10) | 7.1 (5–9) | 7.6 (5–10) | .3 |
| Initial pain medication (%) | .5 | |||
| None | 3 (9) | 2 (11) | 1 (6) | |
| Paracetamol | 11 (32) | 4 (22) | 7 (44) | |
| NSAIDs | 9 (27) | 6 (33) | 3 (19) | |
| Opiate derivative | 11 (32) | 6 (33) | 5 (31) | |
| QUALEFFO | 63 (37–86) | 60 (37–86) | 67 (38–86) | .1 |
| RMD | 16.7 (8–24) | 15.7 (8–22) | 17.8 (9–24) | .2 |
Note:—PV indicates percutaneous vertebroplasty; OPM, optimal pain medication; VCF, vertebral compression fracture; VAS, visual analog scale; NSAID, nonsteroidal anti-inflammatory drug; QUALEFFO, Quality of Life Questionnaire of the European Foundation for Osteoporosis; RMD, Roland-Morris Disability questionnaire. Numbers are mean (range) or absolute number (percentage) if indicated by (%).
Table 4:
Mean scores of the subgroups of the QUALEFFO before and 2 weeks after therapy in 18 patients treated by PV and 16 patients treated by OPM; absolute differences and 95% CI of the differences between patients after PV and patients treated by OPM
| QUALEFFO | PV (n = 18) | OPM (n = 16) | Difference PV–OPM | 95% CI Difference |
|---|---|---|---|---|
| Initial scores | ||||
| Pain | 19 | 21 | −2 | −3.6–0.4 |
| Function | 10 | 12 | −2 | −5.3–0.6 |
| Mobility | 18 | 20 | −2 | −5.9–1.4 |
| Stature | 23 | 27 | −4 | −9.6–1.5 |
| Social | 26 | 27 | −1 | −4.7–2.9 |
| Quality of life | 11 | 12 | −1 | −2.3–0.9 |
| Emotion | 31 | 33 | −2 | −4.0–0.6 |
| 2 Weeks after therapy | ||||
| Pain | 14 | 20 | −6 | −8.5–−2.5 |
| Function | 8 | 13 | −5 | −7.5–−2.0 |
| Mobility | 16 | 20 | −4 | −8.3–−0.3 |
| Stature | 21 | 27 | −6 | −11.8–−1.0 |
| Social | 25 | 26 | −1 | −4.6–3.5 |
| Quality of life | 11 | 12 | −1 | −2.9–0.3 |
| Emotion | 31 | 32 | −1 | −3.2–1.2 |
Note:—QUALEFFO, Quality of Life Questionnaire of the European Foundation for Osteoporosis; PV, percutaneous vertebroplasty; OPM, optimal pain medication; CI, confidence interval.
In patients who underwent PV, the mean amount of injected cement in each vertebral body was 3.2 mL, median was 3.0 mL, and the range was 1.0–5.0 mL. One PV procedure-related complication occurred in a patient initially randomized in the OPM arm but who requested to be treated by PV after 2 weeks of OPM treatment. An intrapedicular cement spur that broke upon manipulation by the bone biopsy needle caused a small cortical chip fracture at the medial border of the pedicle. No neurologic sequelae evolved.
One day after initiation of the treatment, the mean VAS and analgesic use differed significantly in both groups (Table 2). The mean VAS scores compared with the scores before treatment decreased 2.3 points in the patients treated by PV and 0.5 point in the patients treated by OPM. Analgesic use compared with pretreatment decreased nearly 1 point in patients treated by PV and increased nearly 1 point in patients treated with pain medication. The patient with the previously described procedure-related pedicle chip fracture showed an increase in pain scores. The pain was relieved with the use of analgesics and by local anesthetic infiltration of the involved pedicle.
Table 2:
Mean VAS for pain and analgesic use scores before start of treatment and at 1 day after start of the treatment and the mean changes in both scores in 18 patients treated by PV and 16 patients treated by OPM; P value and 95% CI of the differences between patients after PV and patients treated by OPM
| PV (n = 18) | OPM (n = 16) | Difference PV–OPM | 95% CI Difference | |
|---|---|---|---|---|
| Initial scores | ||||
| VAS for pain (range) | 7.1 (5–9) | 7.6 (5–10) | ||
| Analgesic use (range) | 1.9 (0–3) | 1.7 (0–3) | ||
| Scores after 1 day | ||||
| VAS for pain (range) | 4.7 (1–8) | 7.1 (5–10) | −2.4 | −3.7–−1.0 |
| Change | −2.3 | −0.5 | −1.8 | −2.9–−0.8 |
| Analgesic use (range) | 1.1 (0–3) | 2.5 (1–3) | −1.4 | −2.1–−0.8 |
| Change | −0.8 | +0.8 | −1.6 | −2.3–−0.8 |
Note:—VAS indicates visual analog scale; PV, percutaneous vertebroplasty; OPM, optimal pain medication; CI, confidence interval.
Two weeks after the start of the treatment, the mean VAS scores differed between the groups but the difference was not significant (Table 3). Compared with 1 day after the start of the treatment, the mean VAS increased 0.2 points in the patients after PV and decreased 0.6 points in patients treated by OPM. The patients needed significantly less pain medication compared with the situation before PV, but their analgesic use did not decrease compared with 1 day after PV. Both mean scores and changes in the scores of QUALEFFO and RMD questionnaires compared with the situation before the start of treatment were significant (Table 3). The subscores of QUALEFFO demonstrated significant relief in pain and progress in function, mobility, and stature (Table 4). However, the subscores of social, quality of life, and emotional functioning were comparable with the levels before treatment in both groups. The RMD scores showed a clear improvement in the functional status of the patients after PV and a slight worsening in the patients from the OPM arm.
Table 3:
Mean VAS for pain and analgesic use scores at 2 weeks after initiation of treatment and the mean changes in scores compared with initial scores and scores 1 day after treatment in 18 patients treated by PV and 16 patients treated by OPM
| PV (n = 18) | OPM (n = 16) | Difference PV–OPM | 95% CI Difference | |
|---|---|---|---|---|
| Initial scores | ||||
| VAS for pain (range) | 7.1 (5–9) | 7.6 (5–10) | ||
| Analgesic use (range) | 1.9 (0–3) | 1.7 (0–3) | ||
| QUALEFFO (range) | 60 (37–86) | 67 (38–86) | ||
| RMD (range) | 15.7 (8–22) | 17.8 (9–24) | ||
| Scores after 2 weeks | ||||
| VAS for pain (range) | 4.9 (0–10) | 6.4 (3–9) | −1.5 | −3.2–0.2 |
| Change vs initial score | −2.1 | −1.1 | −1.0 | −0.5–2.5 |
| Change vs 1 day | +0.2 | −0.6 | 0.8 | −2.4–0.7 |
| Analgesic use | 1.2 (0–3) | 2.6 (2–3) | −1.4 | −2.0–−0.8 |
| Change vs initial score | −0.7 | +0.9 | −1.5 | −2.3–−0.8 |
| Change vs 1 day | −0.2 | −0.1 | −0.1 | −0.4–0.5 |
| QUALEFFO (range) | 53 (28–79) | 67 (40–88) | −14 | −24.7–−3.4 |
| Change | −6.8 | −0.7 | −6.1 | −10.7–−1.6 |
| RMD (range) | 13 (3–22) | 18 (9–23) | −5 | −8.4–−1.2 |
| Change (%) | +19 | −2 | 21 | 0.07–0.35 |
Note:—VAS indicates visual analog scale; PV, percutaneous vertebroplasty; OPM, optimal pain medication; CI, confidence interval; QUALEFFO, Quality of Life Questionnaire of the European Foundation for Osteoporosis; RMD, Roland-Morris Disability questionnaire.
Two patients treated by PV with initially improved pain scores 1 day after PV had maximal pain scores 2 weeks after PV. Both patients indicated pain at a vertebral level adjacent to the treated levels. The spine x-rays and subsequent MR imaging scans showed a new VCF in adjacent vertebral bodies. After several weeks of conservative treatment, these new VCFs were treated by PV with subsequent improvement of pain during follow-up. The mean VAS score in 16 patients after PV (with the scores from the 2 patients with new VCF eliminated) was 4.4 (range, 0–8) with a decrease of 2.9 compared with VAS before PV. Comparing the mean VAS in these patients with the 16 patients in the OPM arm showed a significant difference (95% confidence interval difference, −3.6–−0.5).
Clinical Outcome Crossover from Pain Medication to PV
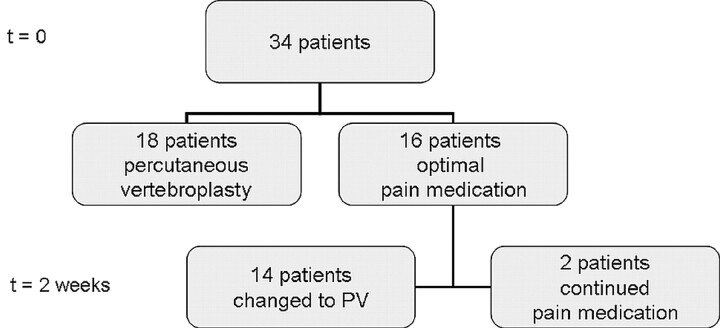
Fourteen (88%) of the 16 patients in the OPM arm requested treatment by PV, 2 weeks after initiation of OPM. The scores of these patients 1 day and 2 weeks after PV were compared with the scores during their OPM study period. Figure 1 illustrates the outcomes of the randomization scheme.
Fig 1.
Randomization scheme in 34 patients randomized in either the percutaneous vertebroplasty (PV) treatment arm (n = 18 patients) or the optimal pain medication (OPM) treatment arm (n = 16 patients). After 2 weeks of treatment, 14 patients treated by OPM requested treatment by PV and 2 patients continued the OPM treatment.
One day after PV, the mean VAS and analgesic use were significantly better compared with 1 day after the start of OPM (Table 5). Two weeks after PV, the mean VAS, analgesic use, QUALEFFO, and RMD questionnaire scores showed significant improvement (Table 5). The subscores of QUALEFFO demonstrated significant relief in pain and progress in function, mobility, stature, and social functioning. Quality of life and emotional status were almost comparable with the scores 2 weeks after optimizing pain medication.
Table 5:
Mean scores in 14 patients randomized for OPM who requested crossover to treatment by PV 2 weeks after start of the study
| OPM Treatment (n = 14) | After Crossover to PV (n = 14) | Difference OPM–PV | 95% CI Difference | |
|---|---|---|---|---|
| 1 Day | ||||
| VAS for pain (range) | 7.4 (5–10) | 3.9 (0–10) | −3.5 | −4.8–−2.1 |
| Analgesic use (range) | 2.5 (1–3) | 0.9 (0–3) | −1.6 | −2.4–−0.9 |
| 2 Weeks | ||||
| VAS for pain (range) | 6.8 (4–9) | 3.3 (0–7) | −3.5 | −4.9–−2.1 |
| Analgesic use (range) | 2.6 (2–3) | 0.9 (0–3) | −1.7 | −2.5–−1.0 |
| QUALEFFO | 67 | 53 | 14 | 8.5–19 |
| RMD | 18 | 11 | 7 | 2.4–11.4 |
| QUALEFFO subsections | ||||
| Pain | 20 | 13 | −7 | −10.6–−2.6 |
| Function | 13 | 9 | −4 | −5.6–−2.5 |
| Mobility | 20 | 16 | −4 | −6.7–−1.6 |
| Stature | 27 | 22 | −5 | −8.3–−1.6 |
| Social | 26 | 25 | −1 | −3.1–−0.1 |
| Quality of life | 12 | 11 | −1 | −2.1–0.1 |
| Emotion | 32 | 31 | −1 | −2.3–0.2 |
Note:—OPM, optimal pain medication; PV, percutaneous vertebroplasty; CI, confidence interval; VAS, visual analog scale; QUALEFFO, Quality of Life Questionnaire of the European Foundation for Osteoporosis; RMD, Roland-Morris Disability questionnaire.
One patient indicated worsening of pain immediately after PV (maximal VAS). This patient had the previously described pedicle chip fracture and was treated conservatively. Two weeks after PV, VAS decreased to 5.
Discussion
One day and 2 weeks after initiating the treatment, the pain relief was significantly better in the patients treated by PV compared with the patients treated by OPM. Two weeks after initiating treatment, the differences were less significant, but this was caused by the occurrence of new VCFs in adjacent vertebral bodies in 2 patients treated by PV. The progress in mobility, function, and stature of the patients after PV was significant compared with OPM treatment. The outcomes of quality of life and social and emotional status were comparable in both treatment arms. Fourteen of 16 patients randomized in the OPM arm requested treatment by PV 2 weeks after starting OPM. The pain outcome scores 1 day and 2 weeks after PV treatment were better compared with the short-term results after OPM.
Decrease in VAS 1 day after treatment in the patients treated with PV was largest, whereas VAS after 2 weeks was almost comparable with 1-day VAS. Consequently, the effect on pain caused by the VCF is immediate after PV. One day and 2 weeks after treatment, a gradual decrease in VAS is observed in the patients treated by OPM. Besides its lesser impact on back pain, pain medication seems to have a slower effect on pain relief compared with the instant response after PV.
Shortly after treatment, the only comparable outcomes in the study groups were quality of life and social as well as emotional status (subsections of QUALEFFO). Moreover, the scores after treatment were equal to the scores before treatment in nearly all cases. Apparently, pain and physical impairment of painful osteoporotic VCF have not that much short-term influence on mental status of patients after PV.
In studies with small populations, the results can be influenced by 1 or 2 extreme measurements. The present study showed that the pain scores of 2 patients who developed new VCFs within 2 weeks after PV influenced the pain scores such that exclusion of these patients’ scores resulted in significantly improved VAS scores after PV compared with patients treated by OPM. The occurrence of new VCFs is a well-known phenomenon in patients with osteoporosis, after both PV treatment and conservative treatment. New VCFs are observed in approximately a quarter of patients within the first year after the initial VCF.13 Within 3 months after PV, most new VCFs occur in the vertebral bodies adjacent to treated levels.13
The present management of patients with pain and functional impairment of osteoporotic VCF consists of conservative therapy: analgesics, (bed) rest, and, in some cases, bracing. However, these palliative treatments are not directed toward the cause of complaints: the VCF. To the contrary, the aim of PV is immediate alleviation of the pain and improvement of the disability through cement stabilization of the VCF. Since the first PV treatment of an aggressive cervical vertebral body hemangioma by Galibert and Deramond14 in 1987 and the first published case of PV in an osteoporotic VCF in 1989 by Lapras and Dusquenel,15 numerous clinical studies have been performed. In a recent literature review on clinical studies in patients with osteoporotic VCF treated by PV, we found that these studies indicated that PV is a safe minimal invasive treatment of painful osteoporotic VCF with immediate and long-lasting good clinical outcome.3 However, most of these studies were retrospectively conducted and nearly all had 1 or more methodologic shortcomings.3 Most studies included small patient groups. Often there was lack of data on exclusion criteria, severity of fractures, duration of pain, and duration and type of the preprocedural therapy. Only a few studies assessed the clinical outcome with the use of standardized pain, functional status, or quality of life questionnaires. No prospective randomized intervention study was published. The present study is, to our knowledge, the first randomized prospective comparative clinical trial in patients with painful osteoporotic VCF comparing PV to the present “gold standard” therapy: pain medication.
Until now, common practice in most centers has been to treat patients with osteoporotic VCF conservatively for at least 6 to 8 weeks after initial VCF, because most osteoporotic VCFs heal within this period with subsequent pain relief.16,17 As a consequence, potential candidates for our study were already treated with various conservative therapies, including (bed) rest, bracing, and analgesics. Most of these patients were referred to 1 of our hospitals to be treated by PV because conservative treatment failed. The mean duration of back pain from the VCF in our patient population was nearly 3 months. These patients were not motivated to participate in our study and wanted to be treated with an alternative therapy. During almost 2 years of inclusion, 46 patients consented to participate, but in the end, only 34 could be included in the study. Twelve patients who initially consented to take part left the study in an early phase because they refused to fill out the extensive questionnaires or to be observed so intensively. The patients who did consent to participate in the study and were randomized in the OPM arm were probably prejudiced against continued medical therapy, albeit the individual optimization, because most had been treated for an average of 3 months without success. This explains the high number of crossovers to PV after 2 weeks of OPM.
Another limitation of our study was the short-term follow-up to compare patients in both randomization arms. The initial objective was to follow the patients for 1 year. We incorporated in the study the possibility of PV for those patients who did not benefit from 2 weeks of OPM. The crossover possibility to PV was never encouraged by the physicians but in all cases was requested by the patients. Despite some improvement of pain relief during 2 weeks of OPM, only 2 patients continued their OPM treatment.
Further research is needed with larger groups of patients and longer follow-up. To enroll more patients in a RCT, these patients have to be included in an early stage after initial fracture of the vertebral body. This way, participants will more readily accept possible randomization to conservative treatment. To have less influence on the clinical outcome by patients in whom natural VCF healing takes place within 6 to 8 weeks, such a study needs to be performed in a larger population. Even more important, there must be no acceptance of a “crossover” from 1 study arm to the other in a future prospective RCT. To evaluate the effect of the injected cement on pain and to exclude the influence of other factors such as a placebo effect or local anesthetic effect, another RCT could be a sham trial, in which the 1 arm has a cementation after percutaneous needle placement and in the other arm no cement is injected. For the time being, PV should be reserved for carefully selected patients in whom conservative therapy has not been effective to treat their pain.
Conclusion
The pain relief and improvement of mobility, function, and stature after PV is immediate and significantly better in the short term compared with OPM treatment.
References
- 1.Mathis JM, Barr JD, Belkoff SM, et al. Percutaneous vertebroplasty: a developing standard of care for vertebral compression fractures. AJNR Am J Neuroradiol 2001;22:373–81 [PMC free article] [PubMed] [Google Scholar]
- 2.Kallmes DF, Jensen ME. Percutaneous vertebroplasty. Radiology 2003;229:27–36 [DOI] [PubMed] [Google Scholar]
- 3.Hendrikse CA, Kalmijn S, Voormolen MH, et al. [Percutaneous vertebroplasty in the treatment of osteoporotic vertebral compression fractures: review of the literature]. NTvG Ned Tijdschr Geneeskd 2003;147:1553–59 [PubMed] [Google Scholar]
- 4.Diamond TH, Champion B, Clark WA. Management of acute osteoporotic vertebral fractures: a nonrandomized trial comparing percutaneous vertebroplasty with conservative therapy. Am J Med 2003;114:326–28 [DOI] [PubMed] [Google Scholar]
- 5.Do HM, Kim BS, Marcellus ML, et al. Prospective analysis of clinical outcomes after percutaneous vertebroplasty for painful osteoporotic vertebral body fractures. AJNR Am J Neuroradiol 2005;26:1623–28 [PMC free article] [PubMed] [Google Scholar]
- 6.Baker LL, Goodman SB, Perkash I, et al. Benign versus pathologic compression fractures of vertebral bodies: assessment with conventional spin-echo, chemical-shift, and STIR MR imaging. Radiology 1996;199:541–49 [DOI] [PubMed] [Google Scholar]
- 7.Do HM. Magnetic resonance imaging in the evaluation of patients for percutaneous vertebroplasty. Top Magn Reson Imaging 2000;11:235–44 [DOI] [PubMed] [Google Scholar]
- 8.Genant HK, Wu CY, van Kuyk C, et al. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 1993;8:1137–48 [DOI] [PubMed] [Google Scholar]
- 9.Huskisson EC. Measurement of pain. Lancet 1974;2(7889):1127–31 [DOI] [PubMed] [Google Scholar]
- 10.Lips P, Cooper C, Agnusdei D, et al. Quality of life in patients with vertebral fractures: validation of the Quality of Life Questionnaire of the European Foundation for Osteoporosis (QUALEFFO). Working Party for Quality of Life of the European Foundation for Osteoporosis. Osteoporosis Int 1999;10:150–60 [DOI] [PubMed] [Google Scholar]
- 11.Roland M, Morris R. A study of the natural history of back pain, part I: development of a reliable and sensitive measure of disability in low back pain. Spine 1983;8:141–44 [DOI] [PubMed] [Google Scholar]
- 12.Gardner MJ, Altman DG. Confidence Interval Analysis. London: British Medical Journal;1989
- 13.Voormolen MHJ, Lohle PNM, Juttmann JR, et al. The risk of new osteoporotic vertebral compression fractures in the year after percutaneous vertebroplasty. J Vasc Interv Radiol 2006;17:71–76 [DOI] [PubMed] [Google Scholar]
- 14.Galibert P, Deramond H, Rosat P, et al. [Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty]. Neurochirurgie 1987;33:166–68 [PubMed] [Google Scholar]
- 15.Lapras C, Dusquenel J. [Percutaneous injection of methylmetacrylate in osteoporosis and severe vertebral osteolysis (Galibert's technique)]. Ann Chir 1989;43:371–76 [PubMed] [Google Scholar]
- 16.de Laet C, van Hout BA, Pols HA. Osteoporosis in the Netherlands: A Burden of Illness Study. Rotterdam: Institute for Medical Technology Assessment;1996
- 17.Nevitt MC, Ettinger B, Black DM, et al. The association of radiographically detected vertebral fractures with back pain and function: a prospective study. Ann Intern Med 1998;128:793–800 [DOI] [PubMed] [Google Scholar]