Abstract
BACKGROUND AND PURPOSE: Large-vessel intracranial atherosclerotic stenosis carries a proved stroke risk of 8%–22% per year with “best medical therapy.” The long-term clinical neurologic and angiographic outcomes of angioplasty and/or stent placement for intracranial atherosclerosis in a consecutive series of patients are presented.
METHODS: The demographics, procedural details, procedural outcome, and long-term neurologic follow-up in 60 consecutive patients with 71 lesions, undergoing a total of 84 procedures, were analyzed.
RESULTS: Angioplasty alone was performed in 62 procedures; 22 procedures involved stent placement. The periprocedural stroke+death rate was 4.8%. The overall complication-free success rate was 90.5%. Restenosis occurred in 23 lesions at a mean of 4.6 months; 13 were re-treated without complication. There were 4 strokes and 4 non-neurologic deaths during 224 patient-years of follow-up. The annualized stroke rate was 1.8%, and the annualized stroke+all-cause death rate was 3.0%.
CONCLUSIONS: The stroke and death rates in this consecutive series of patients with severe intracranial atherosclerotic stenosis treated with optimal endovascular therapy are considerably less than those associated with the natural history of intracranial atherosclerosis treated with maximal medical therapy. Intracranial angioplasty with conditional stent placement is technically feasible and clinically effective with a substantial reduction in long-term stroke and death.
Intracranial atherosclerosis carries a risk of stroke of 8%–22% per annum1–4 and may have varying degrees of risk based on the location and severity of stenoses.1–4 Although this condition has received little clinical attention, it has been estimated that it is the cause of approximately 5%–10% of all strokes.1,5,6 Until recently, optimal therapy has been thought to be oral warfarin. With the results from the completed Warfarin Versus Aspirin for Recurrent Stroke Study (WARSS)2 and from the prematurely halted Warfarin Versus Aspirin for Symptomatic Intracranial Disease Study (WASID),7 it is now known that medical therapy is poorly effective for large vessel atherostenosis and that aspirin alone is as good or better than warfarin for all cerebrovascular atherosclerotic conditions.
The current study reports the authors’ long-term clinical outcomes with independent neurologic examinations in 60 patients who underwent percutaneous transluminal angioplasty (PTA) with and without stents for intracranial atherosclerotic disease and who had complete preprocedure and postprocedure neurologic examinations by external observers. The procedural details and short-term results of the initial subset of these patients have been reported previously.8 Those patients treated by the first author between 1996 and 1998 were included in the previous article and represented 14 patients with 16 lesions who underwent a total of 18 procedures (2 for re-stenosis) and are also included in the series presented here.
Methods
Patient Selection
All patients were evaluated and treated at Our Lady of Lourdes Regional Medical Center (Lafayette, La), beginning in August 1996. All patients undergoing intracranial angioplasty or stent placement at this institution between August 1996 and May 2004 were included in this analysis. Neurologists referred most patients for treatment; other referring physicians included neurosurgeons, internists, vascular surgeons, and cardiologists. Before referral, all patients had catheter angiographic or MR angiographic (MRA) imaging as well as cross-sectional imaging of the brain and were specifically referred for possible endovascular therapy. Functional imaging (eg, perfusion CT) data were not readily available until near the end of the series and were, therefore, not collected. After clinical and neuroimaging evaluation by the neurointerventionist (J.C.W.), management options were discussed by the referring clinician and the neurointerventionist.
All patients in the study had measured initial stenoses of at least 70% by the North American Symptomatic Carotid Endarterectomy Trial (NASCET) criteria, which are comparable to WASID methodology. Most patients with an asymptomatic stenosis or a newly diagnosed symptomatic stenosis were initially managed with maximal medical therapy, including dual antiplatelet therapy (aspirin and clopidogrel [Plavix] or aspirin/dipyridamole [Aggrenox]) and cholesterol-lowering agents (statins). Treatment of related conditions such as diabetes or hypertension was optimized. More recently, because of potential beneficial vascular effects, patients were also placed on an angiotensin-converting enzyme (ACE) inhibitor. Even patients with blood pressure in a normal range were placed on low-dose ACE inhibitor therapy unless they could not tolerate it. Blood pressure was preferentially kept at the upper limits of normal to maximize cerebral perfusion past the stenotic vessel. Patients who developed symptoms or continued to have symptoms on maximal medical therapy were then considered for endovascular therapy.
An additional subset of patients with asymptomatic lesions was considered for endovascular therapy if they were already being treated for a symptomatic lesion, had a high-grade stenosis (>70% or <1 mm residual lumen) and required major surgery such as coronary artery bypass grafting, or had angiographically proved rapidly progressive stenosis.
Preprocedural Management
This retrospective analysis received institutional review board approval. Treatment options and timing were discussed with the patient and family. The potential use of off-label devices and the fact that data were being collected were explained. Informed consent was obtained from the patient.
In general, patients continued to receive all medications until endovascular treatment, except when contraindicated. Those on warfarin were switched to another anti-thrombotic therapy 5 days in advance of the procedure. Initially, these patients were placed on a weight-based intravenous (IV) heparin protocol; however, more recently, patients received low-molecular-weight heparinoid therapy at home (administered by a visiting nurse).
Procedure
General
All procedures were performed with the assistance of anesthesiology (an anesthesiologist and/or nurse anesthetist), regardless of whether the procedure was performed with the patient under local anesthetic plus monitored anesthesia care or general anesthesia.
Most procedures were performed via a common femoral artery approach. However, several distal vertebral and/or basilar artery angioplasties/stents were performed via an ipsilateral brachial artery approach because of access difficulty from a femoral approach.
A cervicocerebral interventional guide catheter (eg, Lumax, Cook, Bloomington, Ind) was positioned in the cervical internal carotid artery (ICA) for anterior circulation lesions and in the vertebral artery for posterior circulation lesions. If necessary, the guide catheter was positioned in the subclavian artery adjacent to the vertebral artery origin.9
Intraprocedural and Periprocedural Medication
All patients received a bolus dose of IV abciximab (ReoPro) after placement of the neuroguide catheter. Initially, the standard weight-based cardiac bolus dose (0.25 mg/kg) was given, followed by the standard 12-hour infusion (0.125 μg/kg per minute). Beginning in 2003, in low-risk patients (eg, smooth lesions, no dissection), this bolus was decreased to one half of the standard dose, with no additional infusion. All patients also received an IV antithrombotic agent at this time. Initially, heparin was given (5000-U bolus dose IV with initial doses given to maintain activated clotting time at 250–300 seconds). Beginning in 2003, bivalirudin (Angiomax) was administered in a standard fashion (bolus of 0.75 mg/kg followed by an infusion at 1.75 mg/kg per hour for the duration of the procedure and then 0.25 mg/kg per hour for a total of 12 hours).
Choice of Balloon and/or Stent
Angioplasty alone was performed in most patients. Primary stent placement was reserved for specific circumstances: eccentric stenotic lesions in the ICA below the ophthalmic artery or in the distal vertebral artery or proximal basilar artery. Secondary stent placement was performed if the lesion did not respond to angioplasty or if there was unacceptable rebound stenosis (return to the preangioplasty degree of stenosis or worse). Figures 1 and 2 illustrate typical lesions treated by angioplasty alone versus primary stent placement and the long-term angiographic results.
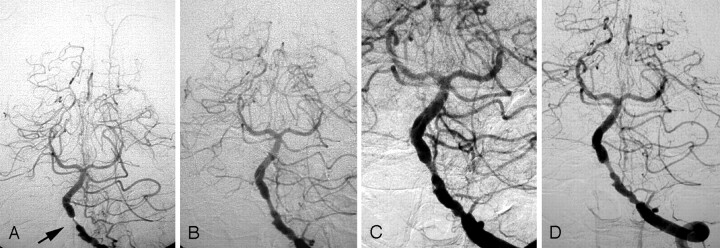
Fig 1.
A, 71-year-old woman who initially presented with a cerebellar infarct. Posteroanterior (PA) left vertebral arteriogram reveals a high-grade stenosis of the proximal basilar artery, supplied only by this vessel (arrow). This lesion is concentric and measures <10 mm in length and is typical of lesions responding well to angioplasty alone. B, Appearance immediately after angioplasty, illustrating that safe suboptimal improvement is satisfactory. There is residual stenosis but flow is improved. C, Appearance 6 months. The patient is still asymptomatic; no repeat angioplasty was performed. D, Appearance 7 years after angioplasty shows that the lesion is stable. The patient remains asymptomatic.
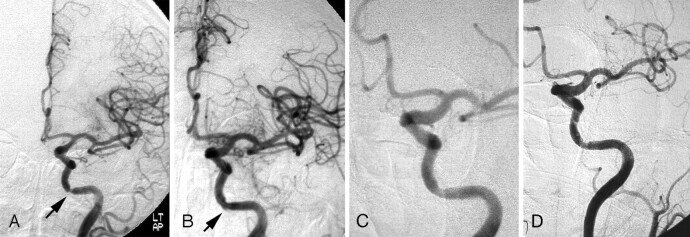
Fig 2.
A, 81-year-old man who presented with recurrent left carotid artery TIAs (right-sided weakness and expressive aphasia). PA left carotid arteriogram reveals a focal but eccentric stenosis at the petrocavernous junction (arrow). The lesion is short, eccentric, and along a curve in the vessel; the vessel is >3 mm in diameter and proximal and is typical of the lesions treated with stent placement. B, Appearance immediately after stent placement. Note a small dissection (arrow). C, Appearance 6 weeks later demonstrates healing of the dissection. D, Appearance 4 years after stent placement. The mild residual stenosis remains and the patient remains asymptomatic.
With the exception of a few early cases in which the Stealth (Boston Scientific-Neurovascular, Fremont, Calif) or the Stratus (MicroInterventional Systems) balloon systems were used (neither is currently available), all of the balloons and stents used were marketed for coronary artery use. If a balloon alone was used, the shortest balloon that covered the length of the stenotic segment was chosen, typically 9–10 mm. The balloon diameter was undersized relative to the vessel diameter by 0.25–0.5 mm if at all possible.8,9 Because of technical and device limitations, lesions in a vessel of primary diameter ≤2.0 mm rendered balloon undersizing impossible until balloons with inflated diameters of 1.5 mm recently became available. If a stent was to be used primarily, the shortest stent providing adequate coverage of the stenotic segment was chosen, and the stent diameter was matched to the vessel diameter or undersized rather than oversized.8
Procedural Technique
In 50 of the 84 procedures, a low-profile microcatheter and neuro-microguidewire (Transcend 14 EX, Boston Scientific, Natick, Mass) were advanced across the stenosis. The guidewire was then replaced with a neuro-microexchange wire, over which the balloon or stent was advanced. In the remaining 34 instances, it was possible to advance the stent or balloon directly across the stenosis by using a selective microguidewire without exchange. Digital subtraction road-mapping was used to accurately position the balloon. If angioplasty alone was performed, the balloon was inflated gradually (at a rate of 1 atm every 30 seconds) to the desired pressure. It was held at this pressure for 30 seconds and then deflated. This technique of extremely slow inflation has been previously described in detail by the authors.8 If a stent was deployed, the rate of inflation was 1 atm every 15 seconds to the desired pressure; the pressure was held at the desired level for 15 seconds, and the balloon was then deflated. All balloon inflations and stent deployments were performed under fluoroscopic surveillance.
Observation and Postprocedure Management
Intraprocedural observation of the angioplastied site was performed to observe for 2 possible sequelae: rebound stenosis and acute/subacute clot (platelet) deposition. With the use of abciximab, the latter has been essentially nonexistent as opposed to early experience when subacute clot appearance was not infrequently observed. If the initial appearance was unsatisfactory or if there was evidence of rebound stenosis at any time during a 1-hour observation period during which angiographic images were obtained every 15 minutes, the authors took 1 of 3 actions: 1) repeat angioplasty with the same balloon to a higher pressure, 2) repeat angioplasty with a larger balloon, or 3) stent placement (Fig 3). Once a satisfactory appearance was achieved, observation resumed for 1 hour.
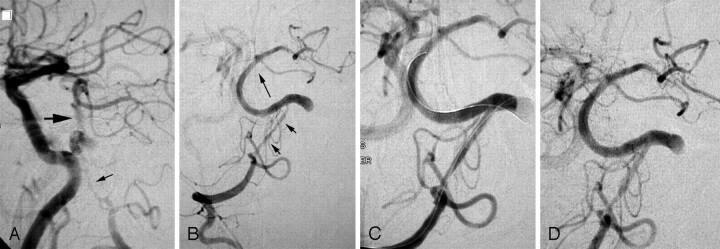
Fig 3.
A, 66-year-old man with recurrent episodes of dizziness, nausea, and diplopia. Lateral view of arteriogram performed with the catheter in the innominate artery. The right vertebral artery has a hairlike residual lumen beyond the posterior inferior cerebellar artery (small arrow); the basilar artery is supplied in large part from the anterior circulation via the posterior communicating artery (larger arrow). The dominant left vertebral is occluded just above the posterior inferior cerebellar artery. B, After initial angioplasty with a 1.5-mm balloon, distal perfusion is improved (long arrow indicating antegrade flow in the basilar artery), but a severely stenotic lumen persists (short arrows). C, After placement of overlapping stents in the distal vertebral artery, there is antegrade filling of both posterior cerebral arteries indicating increased perfusion. D, Initial follow-up examination at 6 weeks reveals continued patency. The patient was followed up with CT angiography, and the stents remain patent 2 and a half years later.
Patients treated in the first 2 years of this series underwent a noncontrast CT at the completion of the procedure; more recently, CT was only performed if there was angiographic concern or a change in neurologic status was suggestive of procedural complication.
Postprocedure, to prevent reperfusion/hyperperfusion hemorrhage, strict attention was paid to blood pressure control with the goal of keeping the systolic pressure within a specified normal range (110–130 mm Hg) using IV labetalol. If there was inadequate response, a nitroprusside infusion was used. All patients were initially managed in the intensive care unit. Strict attention was paid to blood pressure control with the goal of keeping the systolic pressure within the specified normal range. Once stable, they were transferred to the neurology/neurosurgery floor. Most patients were ready for hospital discharge (or transfer to rehabilitation in the case of patients presenting with an acute stroke) within 48 hours after the procedure. All patients were discharged on dual antiplatelet therapy unless warfarin therapy was required for another condition such as atrial fibrillation (these patients were discharged on warfarin and aspirin [81 mg/day]).
Follow-Up
Early in the series, patients were scheduled for follow-up angiography after 2–3 months but more recently have been re-imaged 6 weeks after the procedure. All patients were evaluated with cerebral angiography. If the follow-up appearance remained satisfactory, imaging was repeated at 3 months, 6 months, 1 year, and then at yearly intervals. Initially, this was achieved by cerebral angiography. Recently, MR imaging and MRA were performed at the time of initial follow-up along with angiography if possible. If there was good correlation, then MRA was alternated with conventional angiography.
If a significant restenosis was demonstrated at the time of follow-up, the patient underwent repeat prophylactic angioplasty (or stent placement if necessary) even without recurrent symptoms and was then followed up as described previously. The rationale for treating asymptomatic restenoses was the authors’ observation (later confirmed by WASID) that a certain percentage of patients would not have recurrent symptoms manifested by transient ischemic attack (TIA) but rather by stroke or death.2,3 Asymptomatic restenoses of lesser severity were observed with repeat angiography and only treated if they became symptomatic or progressed to >70% or <1 mm residual lumen. Any time a patient experienced symptoms possibly related to the treated stenosis, an MR imaging (or a CT if MR imaging was not possible because of contra-indications such as pacemaker) and an angiography were performed. Repeat angioplasty or stent placement was performed if indicated. Conventional angiography was also performed if the need arose for major surgery with a significant chance of hypotension/hypoperfusion (eg, coronary artery bypass surgery).
All patients were followed up clinically by the referring physician, a neurologist (if the referring physician was not a neurologist), and the neurointerventionist. The referring physician (and neurologist if necessary) performed a neurologic examination 1–2 weeks after discharge and at the time of each imaging evaluation.
Clinical Outcome Measures
Treatment success was defined as a reduction of stenosis by at least 20% with no intraprocedural or periprocedural complications.
Data Analysis
Data were collected on patient vascular risk characteristics, degree of intracranial stenosis, stenosis locations, initial or repeat angioplasty, and the sizes and types of balloons and stents used for each procedure. Immediate angiographic and clinical neurologic outcomes, periprocedural clinical events and their outcomes, and information on whether the residual stenosis was >50% were also collected. Long-term clinical and angiographic outcomes included restenosis, time to restenosis, information on whether the restenosis was symptomatic and/or required retreatment, duration of follow-up, long-term management, subsequent stroke, other adverse events, and death. In most cases, percentages, means, and ranges for each of these outcomes were calculated to summarize the patient-level data. The time-to-death and time-to-stroke analyses were performed on the patient level.
The time-to-restenosis analysis was performed on the basis of unique specific procedure dates and follow-up times. If a patient had more than 1 unique procedure date, time was calculated as time from 1 procedure to the next or until restenosis. For the patient’s final procedure, time was calculated from time of that procedure until restenosis or end of follow-up.
Results
Sixty consecutive patients with 71 lesions requiring a total of 84 procedures were included in the analyses. There were a total of 224 patient-years of follow-up, and no patients were lost to follow-up. At some time in the period under observation (≤88 months), 6 patients had a stroke and 5 patients died. These deaths included 1 periprocedural death and 4 long-term non-neurologic deaths. There was no long-term neurologic death.
The mean age of the patient population was 62.5 years. Most patients were men (76.7%) and white (86.7%). The mean length of follow-up was 45.7 months; the longest follow-up was 88 months. The only patient with no follow-up was the 1 periprocedural death. One patient died at 3 months from complications following coronary artery bypass surgery. Two patients had <6 months of follow-up (2 and 3 months) at the time of analysis but had undergone follow-up angiography. All of the remaining patients were followed up for at least 6 months. The only patients lost to follow-up were those patients who died; they were followed up until death from any cause.
The distribution of lesions and lesion characteristics are given in Table 1. The most common lesion location was the ICA (42.3%). About half of the lesions were on the left side, 35% were on the right, and approximately 16% were midline basilar arteries (Table 1). A total of 40.8% of the lesions were recurrently or repeatedly symptomatic while the patient was on maximal medical therapy. A total of 46% of the cases presented with a TIA, 39% presented with stroke, and 14% of lesions were asymptomatic at presentation. Of the 12 asymptomatic lesions, only 4 were de novo “new” lesions. Two were additional lesions in patients with symptomatic lesions, 2 (in 1 patient) were treated before planned coronary artery bypass surgery, and 8 were rapidly progressing restenoses of previously treated symptomatic lesions (and were thus treated as part of the planned therapeutic strategy).
Table 1:
Lesion characteristics
| Characteristic | Lesions (%) (n = 71) |
|---|---|
| Lesion location | |
| ICA | 42.3 |
| Vertebral artery | 29.6 |
| Basilar artery | 14.1 |
| MCA | 11.3 |
| ACA | 1.4 |
| PCA | 1.4 |
| Lesion side | |
| Left | 49.3 |
| Right | 35.2 |
| Midline (basilar artery) | 15.5 |
| Presentation* | |
| TIA | 46.4 |
| Stroke | 39.3 |
| Asymptomatic | 14.3 |
| Persistent/recurrent symptoms on medical therapy | 40.8 |
Note:—ICA indicates internal carotid artery; MCA, middle cerebral artery; ACA, anterior cerebral artery; PCA, posterior cerebral artery; TIA, transient ischemic attack.
Presentation of original lesions (n = 71), as well as restenosis, for a total of 84 lesion presentations.
Angioplasty alone was performed in 62/84 procedures. A total of 22 procedures (26.2%) involved stent placement, either primarily (14 procedures) or because of inadequate response to angioplasty (8 procedures). Most stenoses treated with stent placement, either primary or secondary, were located in the distal vertebral arteries and in the petrocavernous carotid artery. Table 2 presents the outcomes for all 84 procedures as well as the outcomes stratified by lesion location.
Table 2:
Procedure outcomes by lesion location*
| Procedures |
|||||
|---|---|---|---|---|---|
| Overall (n = 84) | Basilar (n = 12) | Vertebral (Non ostial) (n = 28) | ICA (n = 32) | MCA (n = 10) | |
| Outcome | |||||
| Treatment success (%)† | 76 (90.5) | 12 (100) | 25 (89.3) | 30 (93.8) | 9 (90.0) |
| Periprocedural complications during initial treatment (not including death) (%) | 7 (8.3) | 0 (0) | 3 (10.7) | 2 (6.3) | 1 (10.0) |
| Periprocedural deaths (%))‡ | 1 (1.2) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Residual >50% (%) | 11 (13.1) | 1 (8.3) | 6 (21.4) | 3 (9.4) | 1 (10.0) |
| Time to restenosis, mo mean (range) | 4.59 (1–16) | 6.25 (1–16) | 4.50 (1.5–16) | 2.88 (2–4) | 3.5 (3–4) |
| Restenosis (%) | 23 (27.4) | 6 (50.0) | 11 (39.3) | 4 (12.5) | 2 (20.0) |
| Restenosis with symptoms (%) | 5 (6.0) | 2 (16.7) | 2 (7.1) | 1 (3.1) | 0 (0) |
| Retreatment for restenosis (with or without symptoms) | 13 (15.5) | 2 (16.7) | 7 (25.0) | 2 (6.3) | 2 (20.0) |
| Retreatment success†§ | 13/13 (100) | 2/2 (100) | 7/7 (100) | 2/2 (100) | 2/2 (100) |
Note:—ICA indicates internal carotid artery; MCA, middle cerebral artery.
Vertebrobasilar junction is included with vertebral artery; anterior cerebral artery and posterior cerebral artery data are included in the overall column, but not in the breakdown by lesion location. The posterior cerebral artery case resulted in a periprocedural death and the anterior cerebral artery case resulted in a periprocedural complication (wire perforation).
Reduction of stenosis by at least 20% and lack of periprocedural complications.
The death was in the PCA case and is not included in the breakdown by location.
Based on the 13 repeat procedures.
The total periprocedural stroke+death rate was 4.8%. The overall complication-free procedural success rate was 90.5%. TIAs accounted for 3/7 (43%) of all nonfatal procedural events. Nonfatal periprocedural complications, including TIA (3), wire perforation (1), hyperperfusion bleed (1), and stroke in the opposite hemisphere (2), occurred in 8.3% of all procedures. The 1 periprocedural death (1.2%) was due to vessel rupture. Both opposite hemisphere strokes, the hyperperfusion bleed, and the wire perforation eventually resulted in good clinical outcomes (patients independent and functioning at previous level). Ten of the 84 procedures resulted in radiographically detectable dissection without symptoms, and none of these required treatment. Although all of the successful procedures reduced stenoses by at least 20%, 13% of the procedures still resulted in arteries with residual stenoses >50%. None of these were associated with persistent symptoms.
Twenty-three of the lesions (27.4%) developed restenosis, but only 5 were symptomatic (Table 2). The average time to restenosis, when it occurred, was <5 months. More than 90% of restenoses occurred by 7 months. By 16 months, all restenoses had occurred (Table 2). The time-to-restenosis curve is presented in Fig 4A. Thirteen of these 23 recurrent lesions were re-treated, but only 2 were for symptoms. Three of the 5 symptomatic restenoses were not treated because in 1 case, the patient was too sick to treat (procedurally unrelated multisystem failure and eventual death) and in the other 2 cases, the lesion could not be re-accessed endovascularly. All completed pre-emptive retreatment procedures for restenosis were successful, and no re-treatment attempt was detrimental.
Fig 4.
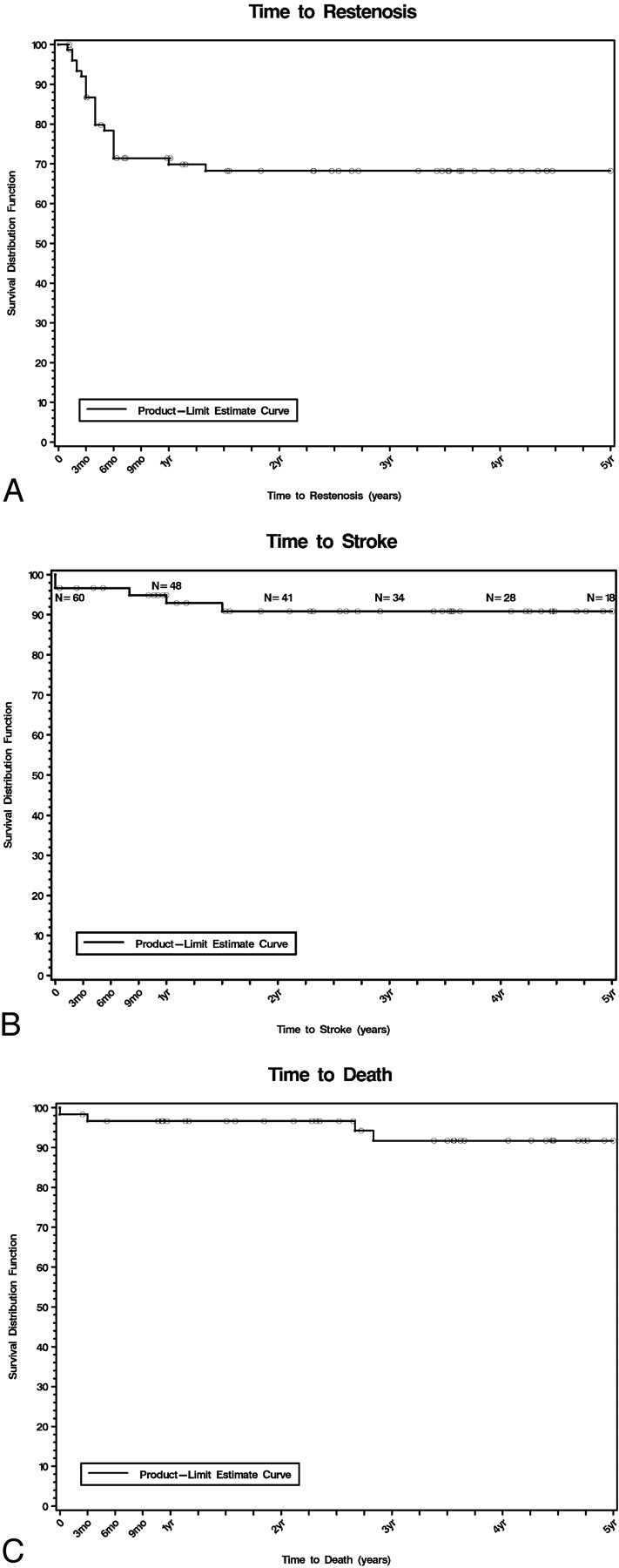
Graphs indicate (A) time to restenosis, (B) time to stroke, and (C) time to death.
The time-to-stroke curve is presented in Fig 4B. Long-term stability of revascularization is shown by the fact that no restenosis occurred later than 16 months and only 1 stroke occurred later than 18 months after the angioplasty/stent. Figure 4C presents the time-to-death curve.
A total of 5 (8.3% of all patients in the study) died during the study. There were 4 deaths from proved non-neurologic causes (6.7% of all patients). Four patients overall (2 with basilar lesions, 1 with a vertebral lesion, and 1 with an ICA lesion) had strokes in the distribution of the treated vessel. There were no late long-term deaths from neurologic cause. The annualized stroke rate was 1.8%. The total annualized stroke+all-cause death rate was 3.0% (1 patient had a stroke and later died of another non-neurologic cause). Table 3 summarizes the pertinent data on each of the individual patients in the series.
Table 3:
Summary of data on individual patients in the series
| Patient No./Age (y) at Initial Procedure/Sex | Race | Comment | Lesion Location | Referred/Followed by | Type of Physician | Procedure Performed | Outcome | Periprocedural Neurological Event (Outcome) | Restenosis (mo) | Management | Follow-up (mo as of May 10, 2004) | Late Event |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1/56/M | W | Basilar | R.M. | Neurologist | A | 61 | Died (abdominal sepsis) | |||||
| 2/65/F | W | Basilar | R.M./D.D. | Neurologist | A | 88 | ||||||
| 3/39/M | W | ICA | D.D. | A | Residual stenosis >50% | 85 | ||||||
| 2nd lesion | MCA | A | 85 | |||||||||
| 4/74/M | W | Vertebral | R.M./E.N./K.M. | Neurologist/CV surgeon/internist | A | TIA (resolved) | 84 | Lacunar stroke 69 mo | ||||
| 5/59/F | W | MCA | R.M./D.D./J.B. | Neurologist/vascular surgeon | A | 4 | Retreated: stable | 83 | ||||
| Repeat at 10 mo | ||||||||||||
| 6/53/M | B | ICA | R.M./J.B. | Neurologist/vascular surgeon | A | 2 | Retreated: stable | 83 | ||||
| Repeat at 2 mo | A | |||||||||||
| 7/70/F | W | Vertebral | D.D./E.N. | Neurologist/CV surgeon | A | Hyperperfusion bleed (good) | 3 | Died (post–coronary artery bypass) | ||||
| 8/71/F | W | Vertebral | D.D. | Neurologist | A | Residual stenosis >50% | 6 | Followed: stable | 78 | |||
| 9/54/M | W | ICA | L.D./J.B. | Neurologist/vascular surgeon | A | 77 | ||||||
| 10/68/M | W | Basilar | R.M./J.L. | Neurologist/ cardiologist | A | 76 | ||||||
| 11/60/F | W | ICA | R.M./J.B. | Neurologist/vascular surgeon | A | Stroke opposite hemisphere (good) | 76 | |||||
| 12/73/M | W | ICA | D.D. | Neurologist | A | 74 | ||||||
| 13/45/M | W | ICA | R.M. | Neurologist | A | 72 | ||||||
| 2nd lesion | MCA | A | 72 | |||||||||
| 14/46/M | W | Vertebral | D.D. | Neurologist | A | Residual stenosis >50% | 6* | Retreated: stable | 68 | |||
| Repeat at 6 mo | Vertebral | A | ||||||||||
| 2nd lesion | Vertebral | A | 62 | |||||||||
| 3rd lesion | ICA | A | Asymptomatic dissection | 61 | ||||||||
| 15/72/M | W | ICA | D.D./J.B. | Neurologist/vascular surgeon | 63 | |||||||
| 2nd lesion | ICA | A | 63 | |||||||||
| 16/81/M | W | ICA | D.D. | Neurologist | A/S | Asymptomatic dissection | 62 | |||||
| 17/71/M | W | Vertebral | R.M. | Neurologist | A | 62 | ||||||
| 18/74/F | W | ICA | R.M./R.D. | Neurologist/CV surgeon | S | Asymptomatic dissection | 61 | |||||
| 19/70/M | W | ICA | R.R./L.D. | Internist/neurologist | A | Residual stenosis >50% | 61 | |||||
| 20/55/M | W | ACA | R.L. | Neurosurgeon | A | Wire perforation (craniotomy, good) | 60 | |||||
| 21/49/M | W | Vertebral | D.D. | Neurologist | A | 4 | Retreated: recurred | 58 | ||||
| Repeat at 12 mo | A/S | 6 | Occluded: stable | |||||||||
| 22/78/M | W | ICA | L.D. | Neurologist | A | 57 | ||||||
| 2nd lesion | MCA | A | 51 | |||||||||
| 23/72/M | W | Basilar | D.D. | Neurologist | A | 12* | Followed: unable to access | 56 | Stroke 12 mo | |||
| 24/76/M | W | ICA | D.D. | Neurologist | A | Residual stenosis >50% | 2.5 | Retreated: stable | 56 | |||
| Repeat at 3 mo | S | |||||||||||
| 25/75/M | W | Basilar | D.D. | Neurologist | A | 16 | Followed: stable | 53 | ||||
| 26/39/M | B | ICA | R.M./Lu.D. | Neurologist/ neurosurgeon | A | Asymptomatic dissection | 53 | |||||
| 2nd lesion | ICA | A | 50 | |||||||||
| 27/42/M | W | ICA | D.D. | Neurologist | A | 52 | ||||||
| 28/66/M | W | Vertebral | P.T. | Internist | A | Asymptomatic dissection | 6* | Retreated: stable | 34 | Died (cardiovascular) | ||
| Repeat at 5 mo | A/S | |||||||||||
| 29/70/M | B | ICA | S.S. | Neurologist | A | 53 | ||||||
| 30/55/M | W | Vertebral | J.D./R.M. | Neurologist | A | Asymptomatic dissection, >50% residual stenosis | 5 | Retreated: stable | 50 | |||
| Repeat at 5 mo | A | |||||||||||
| 31/67/F | B | MCA | D.D. | Neurologist | A | Residual stenosis >50% | TIA (resolved) | 3 | Retreated: stable | 50 | ||
| Repeat at 3 mo | A | |||||||||||
| 32/69/M | W | Vertebral | D.D. | Neurologist | A | 48 | ||||||
| 33/75/M | W | Basilar | R.M. | Neurologist | A | 4 | Retreated: recurred | 32 | ||||
| Repeat at 5 mo | A | 1* | Too sick to treat | Stroke 18 mo, died (multisystem failure) | ||||||||
| 34/59/M | W | ICA | R.M./D.D. | Neurologist | A | 43 | Hemorrhagic stroke 8 mo | |||||
| 2nd lesion | MCA | A | 43 | |||||||||
| 35/74/M | W | Vertebral | L.D. | Neurologist | S | 43 | ||||||
| 2nd lesion | VB junction | A | 43 | |||||||||
| 36/51/M | W | Vertebral | R.M./D.D. | Neurologist | A | Asymptomatic dissection, >50% residual stenosis | 3 | Retreated: stable | 42 | |||
| Repeat at 3 mo | A | |||||||||||
| 37/70/M | W | ICA | E.N. | CV surgeon | A/S | 42 | ||||||
| 2nd lesion | ICA | A/S | Asymptomatic dissection | 42 | ||||||||
| 38/57/M | W | ICA | L.D. | Neurologist | S | 42 | ||||||
| 39/74/M | W | Vertebral | L.D. | Neurologist | A | 41 | ||||||
| 40/52/F | W | PCA | S.S. | Neurologist | A | Vessel rupture (fatal) | 0 | |||||
| 41/79/M | W | ICA | R.M. | Neurologist | A | Asymptomatic dissection | 40 | |||||
| 42/46/M | W | ICA | N.B./D.D. | Neurologist | S | 32 | ||||||
| 43/70/M | W | Vertebral | N.B. | Neurologist | S | 31 | ||||||
| 44/41/F | W | Vertebral | F.L. | Neurologist | S | 30 | ||||||
| 45/61/M | W | Vertebral | J.D. | Neurologist | A/S | Asymptomatic dissection, >50% residual stenosis | 1.5 | Retreated: recurred | 27 | |||
| Repeat at 2 mo | S | Residual stenosis >50% | 2 | Retreated: stable | ||||||||
| Repeat at 3 mo | S | 4 | Followed: stable | |||||||||
| 46/70/M | W | MCA | L.D. | Neurologist | A | 27 | ||||||
| 47/65/M | W | Vertebral | L.D. | Neurologist | A(1)/S(2) | Stroke opposite cerebellar hemisphere (good) | 27 | |||||
| 48/54/M | W | Vertebral | N.B./D.D. | Neurologist | S | 6 | Followed: stable | 25 | ||||
| 49/48/M | W | ICA | J.B. | Vascular surgeon | S | 21 | ||||||
| 50/71/F | W | Vertebral | E.B. | Cardiologist | S | 18 | ||||||
| 51/48/M | O | MCA | F.L. | Neurologist | A | 18 | ||||||
| 52/59/F | B | Vertebral | C.T./D.D. | CV Surgeon/neurologist | A | 13 | ||||||
| 53/78/M | W | Basilar | K.M. | Internist | A | 13 | ||||||
| 54/75/M | W | Basilar | L.Du. | Cardiologist | A | 11 | ||||||
| 55/48/F | W | ICA | H.C. | Neurologist | A | 3* | Followed: unable to access | 11 | ||||
| 56/68/M | W | ICA | J.B. | Vascular surgeon | S | TIA (resolved) | 11 | |||||
| 57/36/M | B | ICA | D.D. | Neurologist | S | 4 | Followed: stable | 10 | ||||
| 2nd lesion | ICA | A | 6 | |||||||||
| 58/72/M | B | Basilar | K.H. | Neurologist | A | 3 | Retreated: stable | 10 | ||||
| Repeat at 3 mo | Basilar | A/S | ||||||||||
| 59/53/F | W | ICA | H.C. | Neurologist | A | 4 | ||||||
| 60/80/F | W | Basilar | E.A. | Internist | A | Residual stenosis >50% | 1.5 | Followed | 2 |
Note:—W indicates white; B, black; O, oriental; ICA, internal carotid artery; MCA, middle cerebral artery; ACA, anterior cerebral artery; PCA, posterior cerebral artery; A, angioplasty; S, stent; TIA, transient ischemic attack;
, with symptoms.
Updated Results
Since the original data analysis and manuscript preparation, an additional 18 months of clinical and angiographic follow-up data have been accumulated. There have been no additional strokes, but 1 patient developed TIAs (possibly due to a second new lesion). The mean follow-up is now 62.5 months, with a maximal follow-up of 106 months (>8.5 years).
Two patients have been lost to follow-up (at 56 and 60 months because we were unable to contact them after Hurricane Rita), and 1 patient died from complications of a spinal cord injury sustained in a motor vehicle crash. These 3 patients were stable at the time of their last clinical and imaging follow-up with no new neurologic symptoms.
Two patients developed additional intracranial atherostenotic lesions. One patient had previously been treated for a distal vertebral artery stenosis that recurred and was treated and eventually asymptomatically occluded. The patient later developed a new asymptomatic basilar artery stenosis at 76 months, detected during routine follow-up. Another patient who was treated for a supraclinoid ICA stenosis developed a symptomatic restenosis (TIAs), which could not be crossed to perform repeat angioplasty, and then an additional stenosis at the carotid apex at 29 months. This second lesion was threatening the collateral supply to the middle cerebral artery distribution via the anterior cerebral artery. In light of the article by Kwon et al,10 both patients were started on cilostazol. The patient with the carotid apex lesion is also being evaluated for extracranial-intracranial (ECIC) bypass surgery.
Discussion
Intracranial atherosclerotic stenosis is a condition estimated to account for 5%–10% of all ischemic strokes.1,5,6 With decreasing routine angiographic evaluation of intracranial vasculature during routine stroke and TIA evaluation, intracranial atherostenosis might be less frequently identified than more easily evaluable sources such as carotid stenosis. Specific evaluation for intracranial sources for stroke/TIA might also be underperformed because of the belief that there are limited options for therapy. Unfortunately, however, a high percentage of patients with intracranial atherosclerotic stenoses fail “best medical therapy.”1,2,11
WASID was a blinded, randomized, and controlled National Institutes of Health trial designed to evaluate outcomes with best medical therapy for intracranial atherosclerotic stenosis. Because of the extremely small vessels and the resultant difficulty with measurement, most trials and series, including WASID, have included patients with as little as 50% or greater stenoses but have still uniformly had high rates of stroke/death. WASID confirmed previous trial data4 and series1,11 and demonstrated that warfarin is no better than aspirin as a medical treatment. WASID was prematurely halted because of the high end point event rate with both aspirin and warfarin and the increased major hemorrhage rate associated with warfarin.
Surgical endarterectomy is not an option for intracranial atherosclerotic stenosis as it is with cervical carotid stenosis, and as opposed to coronary atherostenosis, surgical bypass (ECIC) has been shown to be ineffective or even counterproductive for intracranial atherosclerotic stenosis.4 During the total course of follow-up (a mean of 55.8 months), the relative risk of stroke was 14% higher for the ECIC bypass surgery group.4 Therefore, for intracranial atherosclerotic stenosis, there is no surgical option of any kind for this extremely high-risk condition.
Widespread availability of intracranial angioplasty and/or stent placement may be limited because of the technically demanding nature of the procedure and/or patient inaccessibility as a result of medical-financial restrictions. Retrospective case series have, however, been published investigating short- and medium-term procedural and clinical outcomes of PTA with and without stents for intracranial atherosclerosis, typically for patients with symptomatic intracranial atherosclerosis who failed best medical therapy.8,12–19 A prospective trial of intracranial stent placement (SSYLVIA) resulted in the Humanitarian Device Exemption approval by the Food and Drug Administration of a stent specifically designed for this therapy.20
The procedural complication rates reported in these series varied widely. This variation may be due to a combination of factors, including choice of procedure (angioplasty versus primary stent placement), operator experience, patient selection, and/or timing of the procedure. In some series, primary balloon-expandable stent placement was the chosen procedure but might introduce additional risks.15,17,20 In the series of patients undergoing angioplasty without stent placement reported by Marks et al,19 the periprocedural complication rate was 8.3% and is similar to the results presented here. In other series, a significant number of patients were treated acutely following stroke, and this might be associated with an increased risk of reperfusion/hyperperfusion hemorrhage.
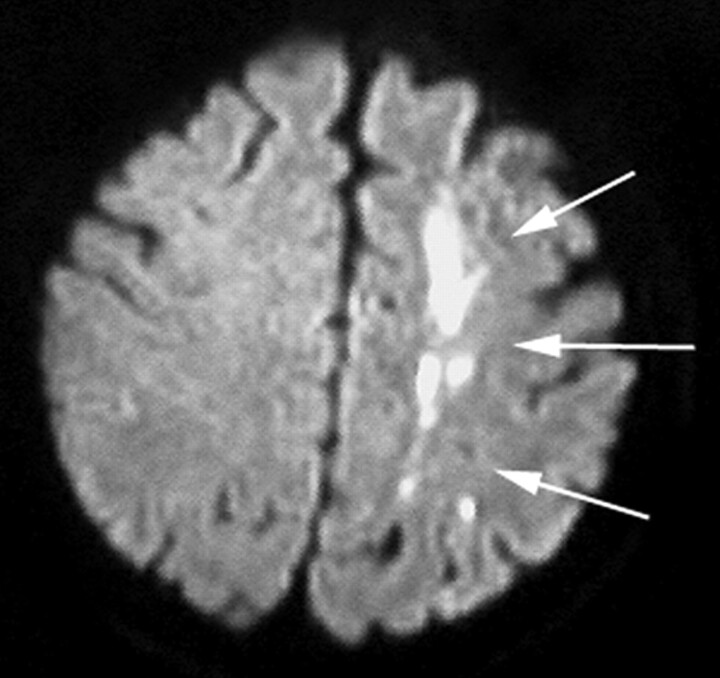
There are at least 4 proposed mechanisms of stroke caused by intracranial stenosis: hypoperfusion, distal embolization, local perforator thrombotic occlusion, and primary vessel thrombotic occlusion. Intracranial stenosis as a cause for stroke/TIA is suggested by a history of recurrent symptoms or infarcts in the same vascular territory or infarcts in the classic watershed distribution (Fig 5). Although assessment in the past has been conventional angiography, recent evaluation has also comprised MRA, CT angiography, and transcranial Doppler sonography.21,22
Fig 5.
Diffusion-weighted MR image demonstrating acute infarct (arrows) produced by intracranial stenosis of the left ICA.
Not all intracranial stenoses represent the same risk or the same therapeutic challenge. Mori et al23 have described an angiographic classification system for the prognosis of angioplasty results and procedural durability: Short concentric or minimally eccentric lesions are classified as type A; type B lesion are 5–10 mm in length, extremely eccentric, and/or moderately angulated; and type C lesions are longer than 10 mm, extremely angulated (>90°), or have a very tortuous proximal segment. Only 5/71 (7%) of lesions reported here were type C. The authors have found these types of lesions to be more technically challenging and to require stent placement more frequently, as has been described with coronary lesions.24
Typical locations for intracranial atherosclerotic stenosis are the petrous and cavernous siphon segments of the ICA, the middle cerebral artery, the paracranial and intracranial vertebral arteries, and the basilar artery. In NASCET, the infraclinoid portion of the ICA was affected 7 times more often than the supraclinoid portion.25 Most lesions in this current series were in the intracranial ICA. Typical presenting symptoms included defined acute neurologic deficits (stroke/TIA) as well as ongoing/recurrent “soft” findings of vertebrobasilar insufficiency. The authors have observed similar soft neurologic findings such as word-finding difficulties that were functionally related to anterior circulation hypoperfusion and that improved after revascularization.26
Improvement in symptoms as well as the decrease in stroke rate compared with natural history is thought to be due to multiple factors. Increase in vessel lumen gives increased flow related to the vessel radius to the fourth power (Poiseuille’s Law). Therefore, a preprocedure lumen of 0.5 mm increased to 1.5 mm results in flow improvement of 34 = 8100%. This law of physics applies even if the original vessel is 3 mm and angioplasty results in a 1.5 mm lumen, leaving a residual stenosis of 50%. An additional mechanism of stroke reduction could be remodeling of the endothelial surface to a smoother surface that could theoretically be less thrombogenic.
Follow-up angiography at defined times after angioplasty has revealed the following: 1) no change, 2) restenosis, or 3) positive outward remodeling with further enlargement in vessel size and thus reduction in stenosis. The latter was an unexpected finding and was not systematically examined but has been repeatedly observed by the authors (J.C.W., J.J.C.). This increase in luminal diameter after angioplasty is thought to be secondary to vascular remodeling after damage to fibrous structures either in the plaque or in the vessel wall (this phenomenon has not been rigorously investigated). This positive remodeling has typically been observed at first follow-up and has been stable with time.
Conclusion
Intracranial atherostenosis is one of the most high-risk neurovascular conditions and is associated with higher stroke and death rates than intracranial aneurysms or arteriovenous malformations, has long-term stroke and death rates greater than those of extracranial carotid stenosis, and has no surgical treatment option. Intracranial angioplasty with or without stent placement has previously been shown to be technically feasible and possibly beneficial for stroke reduction.8,12–20 This retrospective consecutive series with long-term independent clinical neurologic follow-up has shown that intracranial angioplasty with conditional stent placement is both technically feasible and clinically effective. The total periprocedural stroke+death rate was 4.8%. Treatment by angioplasty with conditional stent placement resulted in a considerable reduction in total long-term stroke and neurologic death (from 8% to 22% 1-year stroke/death down to 3% long-term stroke/death rate)1–4 and may currently represent the only effective treatment for this condition. The substantial and durable benefit of endovascular revascularization establishes the appropriateness of this therapeutic approach for primary treatment of symptomatic intracranial atherosclerotic stenosis. Further study is warranted.
Dedication
This article is dedicated to the memory of Robert D. Martinez, MD, a pioneering neurologist in the treatment of intracranial atherosclerosis.
Acknowledgments
The authors wish to acknowledge Kathleen Villa, Susan D. Mathias, and Dave Miller of Ovation Research Group for their contributions in the data analysis and preparation of the manuscript.
References
- 1.Chimowitz MI, Kokkinos J, Strong J, et al. The warfarin-aspirin symptomatic intracranial disease study. Neurology 1995;45:1488–93 [DOI] [PubMed] [Google Scholar]
- 2.Chimowitz M, Lynn M, Howlett-Smith H, et al. Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. N Engl J Med 2005;352:1305–16 [DOI] [PubMed] [Google Scholar]
- 3.Bose A. The Wingspan Study. Paper presented at: the 43rd Annual Meeting of the American Society of Neuroradiology; May2005; Toronto, ON, Canada
- 4.[No authors listed] Failure of extracranial-intracranial arterial bypass to reduce the risk of ischemic stroke: results of an international randomized trial—The EC/IC Bypass Study Group. N Engl J Med 1985;313:1191–200 [DOI] [PubMed] [Google Scholar]
- 5.Sacco RL, Kargman DE, Gu Q, et al. Race-ethnicity and determinants of intracranial atherosclerotic cerebral infarction: The Northern Manhattan Stroke Study. Stroke 1995;26:14–20 [DOI] [PubMed] [Google Scholar]
- 6.Wityk RJ, Lehman D, Klag M, et al. Race and sex differences in the distribution of cerebral atherosclerosis. Stroke 1996;27:1974–80 [DOI] [PubMed] [Google Scholar]
- 7.Mohr JP, Thompson JL, Lazar RM, et al. A comparison of warfarin and aspirin for the prevention of recurrent ischemic stroke. N Engl J Med 2001;345:1444–51 [DOI] [PubMed] [Google Scholar]
- 8.Connors JJ III, Wojak JC. Percutaneous transluminal angioplasty for intracranial atherosclerotic lesions: evolution of technique and short-term results. J Neurosurg 1999;91:415–23 [DOI] [PubMed] [Google Scholar]
- 9.Connors JJ III. Intracranial angioplasty. In: Connors JJ III, Wojak JC, eds. Interventional Neuroradiology: Strategies and Practical Techniques. Philadelphia: WB Saunders Company;1999. :500–55
- 10.Kwon SU, Cho YJ, Koo JS, et al. Cilostazol prevents the progression of the symptomatic intracranial arterial stenosis: the multicenter double-blind placebo-controlled trial of cilostazol in symptomatic intracranial arterial stenosis. Stroke 2005;36:782–86. Epub 2005 Mar 3 [DOI] [PubMed] [Google Scholar]
- 11.Thijs VN, Albers GW. Symptomatic intracranial atherosclerosis. outcome of patients who fail antithrombotic therapy. Neurology 2000;55:490–97 [DOI] [PubMed] [Google Scholar]
- 12.Alazzaz A, Thornton J, Aletich VA, et al. Intracranial percutaneous transluminal angioplasty for arteriosclerotic stenosis. Arch Neurol 2000;57:1625–30 [DOI] [PubMed] [Google Scholar]
- 13.Eckard DA, Zarnow DM, McPherson CM, et al. Intracranial internal carotid artery angioplasty: technique with clinical and radiographic results and follow-up. AJR Am J Roentgenol 1999;172:703–07 [DOI] [PubMed] [Google Scholar]
- 14.Gress DR, Smith WS, Dowd CF, et al. Angioplasty for intracranial symptomatic vertebrobasilar ischemia. Neurosurgery 2002;51:23–27 [DOI] [PubMed] [Google Scholar]
- 15.Lylyk P, Cohen JE, Ceratto R, et al. Angioplasty and stent placement in intracranial atherosclerotic stenoses and dissections. AJNR Am J Neuroradiol 2002;23:430–36 [PMC free article] [PubMed] [Google Scholar]
- 16.Marks MP, Marcellus M, Norbash AM, et al. Outcome of angioplasty for atherosclerotic intracranial stenosis. Stroke 1999;30:1065–69 [DOI] [PubMed] [Google Scholar]
- 17.Mori T, Kazita K, Chokyu K, et al. Short-term arteriographic and clinical outcome after cerebral angioplasty and stenting for intracranial vertebrobasilar and carotid atherosclerotic occlusive disease. AJNR Am J Neuroradiol 2000;21:249–54 [PMC free article] [PubMed] [Google Scholar]
- 18.Nahser HC, Henkes H, Weber W, et al. Intracranial vertebrobasilar stenosis: angioplasty and follow-up. AJNR Am J Neuroradiol 2000;21:1293–301 [PMC free article] [PubMed] [Google Scholar]
- 19.Marks MP, Marcellus ML, Do HM, et al. Intracranial angioplasty without stenting for symptomatic atherosclerotic stenosis: long-term follow-up. ANJR Am J Neuroradiol 2005;26:525–30 [PMC free article] [PubMed] [Google Scholar]
- 20.SSYLVIA Study Investigators. Stenting of Symptomatic Atherosclerotic Lesions in the Vertebral or Intracranial Arteries (SSYLVIA): study results. Stroke 2004;35:1388–92. Epub 2004 Apr 22 [DOI] [PubMed] [Google Scholar]
- 21.Wong KS, Gao S, Chan YL, et al. Mechanisms of acute cerebral infarctions in patients with middle cerebral artery stenosis: a diffusion-weighted imaging and microemboli monitoring study. Ann Neurol 2002;52:74–81 [DOI] [PubMed] [Google Scholar]
- 22.Segura T, Serena J, Castellanos M, et al. Embolism in acute middle cerebral artery stenosis. Neurology 2001;56:497–501 [DOI] [PubMed] [Google Scholar]
- 23.Mori T, Mori K, Fukuoka M, et al. Percutaneous transluminal cerebral angioplasty: serial angiographic follow-up after successful dilatation. Neuroradiology 1997;39:111–16 [DOI] [PubMed] [Google Scholar]
- 24.Iliadis EA, Zaacks SM, Calvin JE, et al. The relative influence of lesion length and other stenosis morphologies on procedural success of coronary intervention. Angiology 2000;51:39–52 [DOI] [PubMed] [Google Scholar]
- 25.Kappelle LJ, Eliasziw M, Fox AJ, et al. Importance of intracranial atherosclerotic disease in patients with symptomatic stenosis of the internal carotid artery. Stroke 1999;30:282–86 [DOI] [PubMed] [Google Scholar]
- 26.Moftakhar R, Turk AS, Niemann DB, et al. Effects of carotid or vertebrobasilar stent placement on cerebral perfusion and cognition. AJNR Am J Neuroradiol 2005;26:1772–80 [PMC free article] [PubMed] [Google Scholar]