Abstract
SUMMARY: We report a case of an incidental nodular calcification of the alar ligament simulating a fracture in the craniovertebral junction of a previously healthy 24-year-old man. Three-dimensional CT and MR imaging revealed a 7.2 × 7.6 × 4.0 mm nodular calcification in the right alar ligament with normal adjacent bony structures. Serial cervical dynamic radiographs and open-mouth views showed that the cervical spine was stable without any change in the calcification.
Calcification in the alar ligament is rare, though some cases with calcification of the transverse or alar ligament have been reported.1,2 It usually develops as a result of traumatic injury or inflammatory disease, especially in the elderly.1,2 In some cases, it is associated with neck pain, relieved by anti-inflammatory drugs and neck immobilization.1 Calcification or ossification of the alar ligament may be an uncommon normal variant and may mimic a fracture of the craniovertebral junction (CVJ).
We present a case of incidentally found nodular alar ligament calcification in a patient with craniocerebral injuries, which was initially considered as a fracture of the odontoid process.
Case Report
A 24-year-old man was involved in a rollover traffic crash. Initially, he was admitted to an outside facility and presented unconscious with a contusion on his left forehead. He underwent radiography and CT of the head, which showed multiplane craniofacial bone fractures to the frontal and sphenoid sinus and left orbital roof, with a bifrontal hemorrhagic contusion. A nodular bony fragment was noted between the right occipital condyle and the odontoid tip in the basal cuts of the brain CT, suggesting a free segment of fractured bone (Fig 1A). The patient was referred to our hospital shortly thereafter. He had no remarkable history. Results of routine laboratory investigations were within normal limits. Initially findings of cervical spine radiographs were also within normal limits.
Fig 1.
A previously healthy 24-year-old man was involved in a traffic crash and presented with severe craniocerebral injuries.
A, Initial axial CT scan shows a nodular calcification between the odontoid tip and the right occipital condyle, suggesting a fractured bone in the craniovertebral junction.
B, 3D volume-rendering image demonstrates a nodular calcification, 7.2 × 7.6 × 4.0 mm, between the occipital condyle and odontoid tip along the course of alar ligament. The bony structures of the craniovertebral junction were normal.
C, Coronal multiplanar reconstruction image shows an attenuated calcific intensity in the region of the right alar ligament, with no remarkable bone marrow component. There is no evidence of fracture in the odontoid process and occipital condyle.
Two days after admission, his consciousness improved, and he complained of severe headache, anosmia, and severe neck pain with limited neck motion. Neurologic examination showed that muscle strength, sensation, and deep tendon reflexes of the upper and lower extremities were normal. Multidetector CT with 3D reconstruction revealed a well-defined 7.2 × 7.6 × 4.0 mm oval nodular calcification in the retro-transverse ligament and supraodontoid tip area along the course of the right alar ligament. The surface of the calcification was smooth without any jagged lines (Fig 1B, -C). A bone marrow component was not present in the calcification. The adjacent occipital condyle, odontoid process, and neural arch of the atlas were apparently normal. Findings of cervical MR imaging also were normal, except for a nodular mass with low signal intensity in the right alar ligament area. In the coronal planes of T1-weighted spin-echo images (TR/TE, 700/14), the left alar ligament was identified with intermediate signal intensity. In contrast, the right alar ligament could not be properly identified because of a nodular calcification with low signal intensity coalescing with the ligament (Fig 2). The calcification was larger than the anatomic boundaries of alar ligament. The medial short segment of the ligament connected the calcification with the odontoid tip.
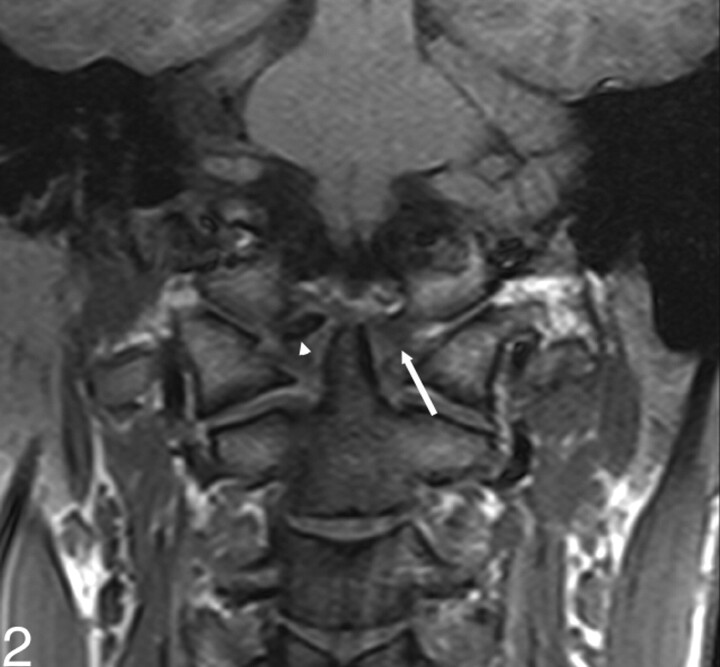
Fig 2.
MR image with coronal T1-weighted sequences shows a nodular calcific attenuation (arrowhead) in the lateral part of the right side alar ligament. It expands in thickness and width beyond the anatomic boundaries of alar ligament. The left alar ligament (white arrow) is a well-defined structure running caudocranially from the apex of odontoid to the occipital condyle, with intermediate signal intensity without any pathologic change.
Fluoroscopic imaging through an open-mouth view showed a calcified nodule in the right side of periodontoid tip area in the CVJ (Fig 3). Serial open-mouth views also denoted the calcification to be consistent, without change of size during 2 months. Serial flexion and extension radiographs of the cervical spine revealed no evidence of instability of the CVJ and upper cervical spine. Technetium-Tc99m methylene dihydroxyphosphonate bone scintigraphy 14 days after trauma showed intense uptake in the fractured area of the frontal and sphenoid sinus but no uptake in the CVJ. The neck pain gradually improved with anti-inflammatory analgesics and physiotherapy, without limitation of neck motion, especially rotatory movement, during 2 months. The patient did not have other ossifications in the other spinal ligaments or upper and lower extremities or any generalized disorders.
Fig 3.
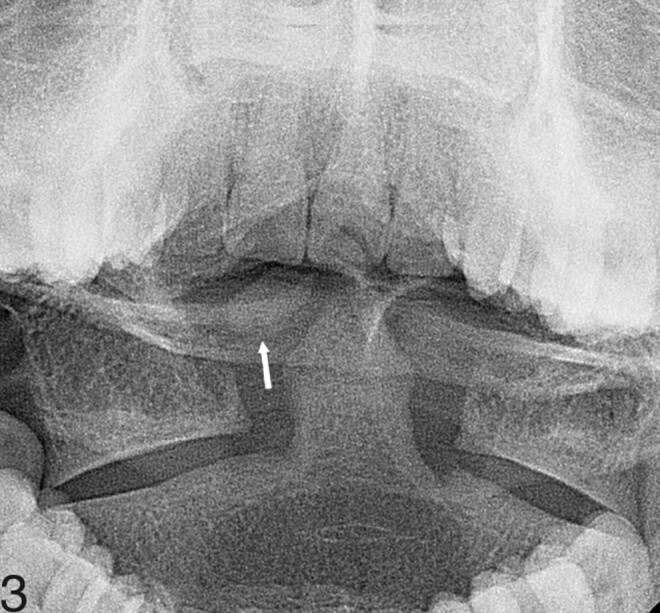
Fluoroscopic image obtained through an open-mouth view. A nodular calcified fragment (white arrow) is present in the right periodontoid tip area with smooth margins.
Discussion
The alar ligaments are strong rounded structures, which arise on both sides of the upper part of the odontoid process and, passing obliquely upward and laterally, are inserted into the medial surface of the condyles of the occipital bone. They play an important role in stabilizing the head during rotatory movements at the CVJ. These ligaments can be assessed well by the use of high-resolution MR imaging, including proton-attenuation weighted sequences. On the basis of these study results, the orientation of the alar ligaments is highly variable, and asymmetry of these ligaments is common in asymptomatic individuals.3 Lesions of the alar ligament with or without associated rotational instability have been discussed as a possible cause of whiplash-associated disorders; however, the structural alteration of the alar ligament related to acute whiplash injury is extremely rare.4,5
Calcification in the alar ligament is very rare, regardless of cause. It usually develops with increasing prevalence after the age of 40 years, especially in the elderly, following minor trauma or as a consequence of inflammatory disease.1,2,6 Kobayashi et al1 reported 2 cases of alar ligament calcification related to neck pain. A 37-year-old man and a 59-year-old woman had pharyngodynia and prior nuchal pain without previous trauma history, which improved gradually with an anti-inflammatory drug therapy and neck immobilization. CT revealed a nodular calcification in 1 patient and a poorly delineated calcified lesion surrounding the odontoid process in the other patient. Serial CT demonstrated that the calcifications shrank and disappeared with time. The authors assumed that pharyngodynia and nuchal pain could be related to an inflammatory reaction induced by deposition of calcium because secondary arthritis was not observed and the symptoms resolved as lesions decreased in size. We thought that their cases could be categorized as a crowned dens syndrome (CDS). CDS is a clinical radiologic entity consisting of periodic acute cervico-occipital pain with fever, neck stiffness, and biologic inflammatory syndrome and a radiologic calcium crystal deposition surrounding the top and sides of the odontoid process in a crown- or halolike distribution.6,7
In the present case, a nodular high attenuation in the periodontoid area was found on the emergent axial brain CT performed after severe head injury. There was lack of information about the patient because he was found unconscious without any witnesses after the trauma. Initially, we considered the possibility of a fracture involving the odontoid process (type I fracture), occipital condyle (type III fracture), or neural arch of the atlas in the CVJ. In the clinical setting, 3D CT was very useful in defining the location and characteristics of the high attenuation and in demonstrating the normal adjacent bone. Although the patient had neck pain with diminished neck motion, we ruled out CDS because our patient was too young and healthy, without previous experience of any neck pain. His neck pain and limited neck motion were interpreted as symptoms of mild neck trauma, and the symptoms resolved gradually by 2 months with anti-inflammatory drugs and physiotherapy. Cervical MR imaging including a proton-attenuation weighted sequence was useful for finding any bone marrow signal intensity within the lesion and for defining the anatomic location and alar ligament. Serial open-mouth views and dynamic radiographs of the cervical spine demonstrated a persistent calcification without reduction of its size and a stable cervical spine.
On the basis of this series of examinations, we concluded that the nodular calcification occurred in the right alar ligament and was unrelated to trauma or inflammation and, therefore, was an incidental finding. This under-recognized entity must be considered in a differential diagnosis of a craniovertebral injury, such as fractures of odontoid process (type I) and occipital condyle (type III) and CDS.
References
- 1.Kobayashi Y, Mochida J, Saito I, et al. Calcification of the alar ligament of the cervical spine: imaging findings and clinical course. Skeletal Radiol 2001;30:295–97 [DOI] [PubMed] [Google Scholar]
- 2.Krakenes J, Kaale BR, Rorvik J, et al. MRI assessment of normal ligamentous structures in the craniovertebral junction. Neuroradiology 2001;43:1089–97 [DOI] [PubMed] [Google Scholar]
- 3.Pfirrmann CW, Binkert CA, Zanetti M, et al. MR morphology of alar ligaments and occipitoatlantoaxial joints: study in 50 asymptomatic subjects. Radiology 2001;218:133–37 [DOI] [PubMed] [Google Scholar]
- 4.Ronnen HR, de Korte PJ, Brink PR, et al. Acute whiplash injury: is there a role for MR imaging?—a prospective study of 100 patients. Radiology 1996;201:93–96 [DOI] [PubMed] [Google Scholar]
- 5.Krakenes J, Kaale BR, Moen G, et al. MRI assessment of the alar ligaments in the late stage of whiplash injury: a study of structural abnormalities and observer agreement. Neuroradiology 2002;44:617–24 [DOI] [PubMed] [Google Scholar]
- 6.Wu DW, Reginato AJ, Torriani M, et al. The crowned dens syndrome as a cause of neck pain: report of two new cases and review of the literature. Arthritis Rheum 2005;15:53:133–37 [DOI] [PubMed] [Google Scholar]
- 7.Bouvet JP, le Parc JM, Michalski B, et al. Acute neck pain due to calcifications surrounding the odontoid process: the crowned dens syndrome. Arthritis Rheum 1985;28:1417–20 [DOI] [PubMed] [Google Scholar]