Abstract
BACKGROUND AND PURPOSE: There exists significant variability in the volume of polymethylmethacrylate cement injected during percutaneous vertebroplasty. Larger cement volumes injected may be associated with better clinical outcomes, but larger volumes may also be associated with greater risk of complications related to cement leakage. We describe an analysis of the association between clinical and procedural variables, including cement volume injected, and the clinical outcomes of patients treated with single-level vertebroplasty.
METHODS: Retrospective analysis of 158 patients treated with single-level vertebroplasty was performed. Relationships among patient and procedural variables and relationships between these variables and ordinal clinical outcome scores of pain and medication use at postprocedure time points from 1 week to 2 years were evaluated with bivariate and multivariable analyses.
RESULTS: There was no significant association between the volume of cement injected and the clinical outcomes of postprocedure pain (P = .159–.871) and medication use (P = .223–.875).
CONCLUSION: Vertebroplasty operators need not feel compelled to achieve particular cement volumes injected in the pursuit of better clinical outcomes but should strive to achieve the maximal safe filling of individual vertebral bodies.
Use of percutaneous vertebroplasty is increasing as a treatment for painful vertebral compression fractures. The procedure has been shown to provide rapid and durable pain relief.1–3 However, a review of the literature and discussions with various operators reveal that despite general adherence to guidelines outlined by Jensen et al4 or Mathis and Wong,5 a large point of procedural variability lies in the volume of cement that is injected into a compressed vertebral body. Even among a given operator’s patients, there is often significant variability in the cement volumes used in treatment. This is likely related to variability in vertebral body size and composition, ease of filling, and the practice of injecting cement until a defined minimal amount of filling is achieved or until there is leakage of cement.
This common but variable methodology is based on the perception that larger volumes of cement generally lead to better outcomes through increased filling of the vertebral body, increased strength and stiffness, and improved internal casting and immobilization of the fracture. Support for this rationale is derived from modeling literature, which describes a positive relationship between cement volume/percentage fill, and vertebral body strength and stiffness in ex vivo studies and finite element models.6–10 Unfortunately, larger volumes of cement may also increase the risk for complications related to leakage, such as disk-space injection, epidural or neural foraminal extension of cement, and pulmonary embolism.11
There have been few clinical studies that have specifically explored the variables that relate to the volume of cement injected during vertebroplasty and how cement volumes relate to vertebroplasty outcomes. We report an analysis of these variables and the impact of cement volume on the clinical outcomes of pain relief and medication requirements after vertebroplasty. Additionally, the relationships between other patient and procedural variables and these clinical outcomes as well as relationships among these patient and procedural variables are explored.
Materials and Methods
We performed a retrospective chart review of all patients who received percutaneous vertebroplasty at our tertiary/quaternary institution between August 1999 and September 2004. The dataset was then limited to those 158 patients who had received vertebroplasty at only a single vertebral level, to reduce the confounding of outcome measures that would be introduced by including patients with multiple treated vertebral compression fractures. The institutional review board for human studies approval was obtained for this study.
Patient Population
Vertebroplasty is typically offered to patients at our institution who have radiologic evidence of subacute or acute vertebral compression fractures of the thoracic or lumbar vertebrae. Nearly all patients undergo preprocedure spine MR imaging, and the presence of edema signal intensity within a compressed vertebra is considered to be suggestive of an acute or subacute fracture. Exclusion criteria include pain that does not localize to a known fracture, improvement with conservative measures such as anesthetic and bracing, and technical contraindications. Over 90% of treated patients had compression fractures that were osteoporotic in origin.
Vertebroplasty Procedure
Vertebroplasties were performed by approximately 5 experienced neuroradiologists in a manner similar to the methods described by Jensen et al.4 Patients were treated by using intravenous conscious sedation, and biplane fluoroscopy was used in all cases. Local anesthetic was administered from the skin to the periosteum of the targeted pedicle. Transpedicular or parapedicular trajectories were used in all cases. Eleven- or 13-gauge bone-biopsy needles were advanced into the central aspect of the vertebral bodies for unipediculate approaches, whereas placement of the needle was made into the midportion of the ipsilateral hemivertebra for bipediculate approaches.
Cement was prepared as has been previously described.4 Briefly, the cement material was prepared by combining polymethylmethacrylate powder with sterile barium sulfate for opacification and with gentamicin powder for infection control, followed by the addition of liquid monomer to make a thin “cake-glaze” consistency material. Cement injection was performed with either 1-mL syringes or a screw-syringe Cook Osteo-Force High Pressure Injector set (HPI 100; Cook Medical, Bloomington, Ind) and was generally considered complete when the cement reached approximately the posterior one fourth of the vertebral body on lateral fluoroscopy. Injection was also terminated if and when epidural, venous, or trans-endplate leakage was noted. Practice patterns among the operators were considered to be similar. Following needle removal, patients were left on strict bed rest for 1 hour and, barring any complicating factor, were then discharged.
Clinical Outcome Measures
Clinical outcomes before and after vertebroplasty were measured with ordinal verbal pain scales scored 0–10 for “pain at rest” and for “pain with activity” (0 = no pain, 10 = worst pain of patient’s life), as well as with changes in medication use (increased, same, decreased, or none) relative to the preceding follow-up time point. Outcomes were measured at baseline preprocedure and at 1 week, 1 month, 6 months, 1 year, and 2 years following vertebroplasty. These measures were obtained prospectively as part of routine clinical care but were reviewed retrospectively for this study.
Percentage of Compression/Cement Volume
Percentage compression was either measured at the time of the procedure from fluoroscopy or was measured after the procedure from preprocedural radiographs. This value was determined by dividing the height of the compressed vertebra by the height of the first nonfractured vertebra immediately cephalad.
The volume of cement injected during vertebroplasty was determined by the operator at the time of the procedure and was recorded in the medical record. We accounted for the volume of cement within the tubing when computing cement volume injected.
Intravertebral Cleft/Cement Leakage
Presence or absence of an intravertebral cleft was determined either from preoperative imaging or from fluoroscopic findings on cement injection during vertebroplasty. Cement leakage data were gathered from procedural reports and were based on identification of leakage during real-time fluoroscopy and from spot fluoroscopic radiographs.
Statistical Analysis
Relationships between the cement volume injected and the binary variables of patient sex, presence or absence of an intravertebral cleft, unipediculate or bipediculate approach, and presence or absence of cement leakage were examined by using the Wilcoxon rank sum test. Simple linear regression was used to explore the bivariate relationships between the outcome variable of cement volume injected and the predictor variables of age, percentage of vertebral compression, vertebral level treated (treated as a continuous variable), and clinical outcomes. The relationships of the presence or absence of cement leakage (including intradiskal, perivertebral, epidural, and pulmonary embolic) with the other variables of patient sex, age, presence or absence of intravertebral cleft, uni- or bipediculate approach, cement volume injected, percentage of vertebral compression, and vertebral level treated were examined by using the Pearson chi-square analysis or the Student t test. The associations between the presence or absence of the intravertebral cleft and the variables of patient age and percentage of vertebral compression were also tested by using the Wilcoxon rank sum test. Analysis of improvement in outcomes across time was performed by using a paired t test comparison to the preceding time point for pain scales and the Wilcoxon signed rank test for medication changes. Bivariate analysis was performed with SAS, Version 8 (SAS Institute, Cary, NC) and with JMP, Version 5.1 (SAS Institute Inc).
A standard least squares multiple linear regression model was constructed with cement volume injected as the outcome variable and with patient sex, age, vertebral level treated (as a continuous variable and which also controls for size of vertebra injected), presence or absence of an intravertebral cleft, unipediculate or bipediculate approach, percentage of vertebral compression, and presence or absence of leakage as the 7 predictor variables. This modeling allows analysis of cement volume injected while controlling individually for each of the previously mentioned predictor variables, including vertebral level treated, which is directly related to vertebral body size.
A nominal logistic regression model was constructed with cement leakage as the binary outcome variable and with patient sex, age, vertebral level treated (as a continuous variable), presence or absence of an intravertebral cleft, uni- or bipediculate approach, percentage of vertebral compression, and cement volume injected as the 7 predictor variables. This modeling allows for analysis of cement leakage while controlling individually for each of the previously mentioned predictor variables, including cement volume injected and vertebral level treated.
Ordinal logistic regression models were constructed for each of the following outcome variables: pain at rest, pain with activity, and medication use, at each of the follow-up time points of 1 week, 1 month, 6 months, 1 year, and 2 years. Each of these 15 ordinal logistic regression models included the following predictor variables: patient sex, age, cement volume injected, vertebral level (as a continuous variable), presence or absence of an intravertebral cleft, unipediculate or bipediculate approach, and percentage of vertebral compression. This modeling allows for analysis of the clinical outcomes of pain and medication use while controlling individually for the previously mentioned predictor variables, including cement volume injected and vertebral level treated. Multivariable analysis was performed with JMP, Version 5.1 (SAS Institute).
Results
We identified 158 patients who received single-level vertebroplasty, with a median age of 76 years (range, 28–95 years). One hundred nine (69%) patients were women. Vertebroplasty was performed at all levels between T4 and L5 (Table 1). A unipediculate approach was used in 100 patients (63%), and intravertebral clefts were described in 53 patients (34%). Asymptomatic extraosseous leakage of cement was observed and recorded in procedural notes in 33/158 patients (21%), with 4 patients with asymptomatic cement pulmonary embolism (2.5%), 4 patients with epidural venous spread (2.5%), 7 patients with nonepidural perivertebral venous spread (4.4%), and 18 cases of disk-space leakage (11%).
Table 1:
Number of patients treated by vertebral level
| Vertebral Level Treated | n |
|---|---|
| T4 | 1 |
| T5 | 1 |
| T6 | 6 |
| T7 | 10 |
| T8 | 9 |
| T9 | 12 |
| T10 | 7 |
| T11 | 8 |
| T12 | 27 |
| L1 | 28 |
| L2 | 23 |
| L3 | 3 |
| L4 | 18 |
| L5 | 5 |
| Total | 158 |
Median and mean cement volumes injected were 3.0 and 3.4 mL (SD, 1.8), respectively, with a range of 0.5–10.3 mL, over all patients. Median cement volumes were 3.0 mL (range, 0.5–7.0 mL) and 3.3 mL (range, 1.5–10.3 mL) for uni- and bipediculate approaches, respectively, and were 2.5 mL (range, 0.8–6.1 mL) and 3.5 mL (range, 0.5–10.3 mL) for thoracic and lumbar vertebrae, respectively.
Of the 158 patients enrolled, we obtained 1-week follow-up for 158, 1-month follow-up for 150, 6-month follow-up for 114, 1-year follow-up for 88, and 2-year follow-up for 53. Pain scores were available on 157/158 patients (99%) at baseline, 146/158 (92%) at 1 week, 138/158 (87%) at 1 month, 104/158 (66%) at 6 months, 80/158 (51%) at 1 year, and 50/158 (32%) at 2 years. Medication use data were available on similar numbers at the various time points.
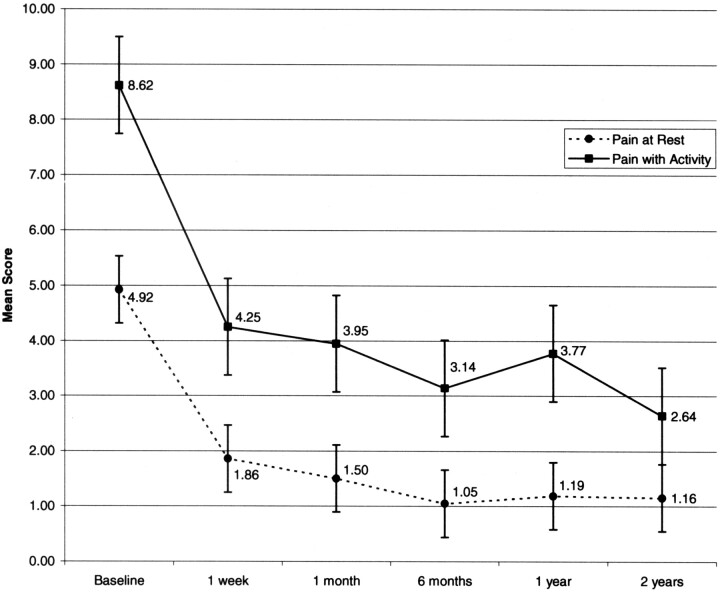
The median and mean preprocedure pain scores were 5/10 and 4.9/10 at rest, respectively, and 9/10 and 8.6/10 with activity, respectively. The range of the median and mean pain scores after the procedure was 0–0/10 and 1.0–1.9/10 at rest, respectively, and 1.5–4/10 and 2.6–4.3/10 with activity, respectively, for the follow-up time points of 1 week to 2 years. Scores for pain at rest and pain with activity improved significantly by 1 week (P < .0001) and remained improved through maximal follow-up (Fig 1). Absolute scores continued to improve after 1 week, though not statistically significantly relative to each preceding time point (Fig 1). Medication use declined significantly at all time points relative to the prior time point (Table 2).
Fig 1.
Graph shows mean pain scores throughout follow-up. Values shown are mean pain scores for each of the time points. Error bars indicate standard error of the mean.
Table 2:
Change in medication use throughout follow-up
| Baseline | 1 wk | 1 mo | 6 mo | 1 y | 2 y | |
|---|---|---|---|---|---|---|
| Medication use | 0 | −0.73 | −0.85 | −1.06 | −1.19 | −1.22 |
| P | <.0001 | <.0001 | <.0001 | <.0001 | <.0001 | <.0001 |
Note:—For medication use, 1 indicates increased medication; 0, same; 1, decreased medication; −2, no medication. P values are relative to the preceding follow-up time point.
Bivariate Analysis
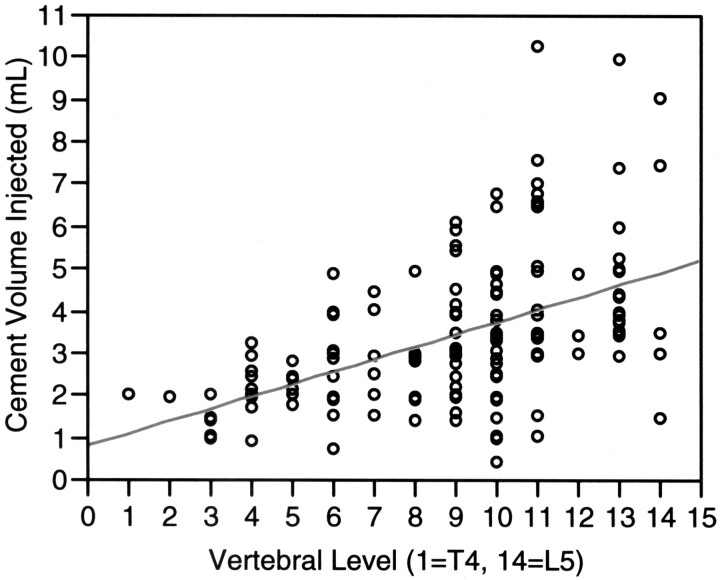
Cement volume injected did not significantly correlate with improvement in the clinical outcome measures of pain and medication use. Volume of cement injected significantly correlated with a uni- versus bipedicular approach (P = .018), with bipedicular injection resulting in placement of an additional 0.3 mL of cement, on average. Men were treated with 0.96 mL more cement on average than were women (P = .032). Lumbar vertebrae were treated with 1.43 mL more cement on average than were thoracic vertebrae (P < .0001). There was a significant relationship (P < .0001) between vertebral level treated (as a continuous variable) and the volume of cement injected (Fig 2), with more caudal levels receiving greater volume of cement, on average. Degree of vertebral body compression (expressed as a percentage of estimated prefracture vertebral body height) (P = .050) and patient age (P = .042) were both found to be significantly and positively associated with cement volume injected—that is, less compressed vertebrae and older patient age were associated with greater cement volume injected. There was no statistically significant association between cement volume injected and leakage (P = .194), though on average, cement volume injected was slightly less in cases of leakage (mean, 3.06 mL; SD, 1.51, with leakage; mean, 3.51 mL; SD, 1.81, without leakage).
Fig 2.
Graph shows cement volume injected as a function of vertebral level treated. Volume of cement increases with treatment of more caudal vertebrae.
Presence or absence of an intravertebral cleft did not significantly correlate with cement volumes injected in the bivariate analysis but was significantly related to percentage of vertebral compression and age at the time of vertebroplasty (P = .0014 and P = .0195, respectively). Specifically, intravertebral clefts were more likely to be found in older patients and within less-compressed vertebrae.
There was a significantly greater proportion of cement leakage with bipediculate (17/58, [29%]) than with unipediculate injection (16/100, [16%]; P = .0473). On average, leakage tended to occur in more compressed vertebral bodies (percentage of normal vertebral height in cases of leakage: mean, 63.6%; SD, 17.3%; without leakage: mean, 70.1%; SD, 14.9%; P = .031).
Multivariable Analysis
In multiple logistic regression, 5 of 7 variables had independent association with volume of cement injected: vertebral level treated (F ratio, 52.81; P < .0001), uni- or bipediculate approach (F ratio, 24.92; P < .0001), presence or absence of intravertebral cleft (F ratio, 18.83; P < .0001), patient sex (F ratio, 9.89; P = .002), and percentage of vertebral compression (F ratio, 6.57; P = .011). Greater cement volume injected was associated with more caudal levels treated, a bipediculate approach, presence of intravertebral cleft, male gender, and lesser degrees of vertebral compression. Patient age was not significantly associated with volume of cement injected when controlling for other variables in multivariable analysis (F ratio, 1.23; P = .270). Cement leakage was also not significantly associated with volume of cement injected (F ratio, 2.25; P = .135).
In multivariable analysis, uni- versus bipediculate injection remained significantly associated with presence or absence of cement leakage (P = .017)—that is, leakage tended to occur more frequently with a bipediculate approach. No other variable had a significant association with cement leakage.
When controlling for the contribution of other predictor variables through ordinal logistic regression modeling, there was no consistent predictor variable that had independent correlation with the outcome variables of pain at different time points. The only significant association found was that of vertebral level injected, treated as a continuous variable, with pain with activity at 1 month following vertebroplasty (Wald chi-square, 4.39; P = .036; more caudal levels treated were associated with greater pain with activity at 1 month)—that is, 1 of 80 associations with pain after vertebroplasty that were tested was significant at the P = .05 level. Specifically, there was no statistically significant relationship between pain at rest or with activity, at any time point in follow-up, with cement volume injected (Table 3; P values for the models ranging from .159 to .871 for the 5 time points of follow-up; mean P value of .579; SD, 0.223) or with the presence or absence of extravasation (P values for the models ranging from .147 to .877 for the 5 time points of follow-up; mean P value of .480; SD, 0.257).
Table 3:
Effect test results for the predictor variable of cement volume injected, from multivariable analysis with pain at each point in follow-up as the outcome variable in the models
| Outcome Variable | For Predictor Variable of Cement Volume Injected |
||
|---|---|---|---|
| Coefficient Estimate | Standard Error | P value | |
| Pain at rest, 1 wk | −0.1337 | 0.1213 | .2702 |
| Pain at rest, 1 mo | −0.0504 | 0.1275 | .6928 |
| Pain at rest, 6 mo | 0.0723 | 0.1580 | .6474 |
| Pain at rest, 1 y | 0.0500 | 0.1924 | .7950 |
| Pain at rest, 2 y | 0.3970 | 0.2820 | .1591 |
| Pain with activity, 1 wk | −0.0183 | 0.1127 | .8711 |
| Pain with activity, 1 mo | −0.0410 | 0.1140 | .7192 |
| Pain with activity, 6 mo | 0.0720 | 0.1340 | .5907 |
| Pain with activity, 1 y | 0.1051 | 0.1532 | .4928 |
| Pain with activity, 2 y | 0.1302 | 0.2195 | .5531 |
In the ordinal logistic regression models with medication use as the outcome variable, the only 2 significant associations, out of 40 tested, were that of age with medication use at 1 week (Wald chi-square, 4.36; P = .037; increasing medication use at 1 week with increasing age) and of uni/bipediculate injection with medication use at 2 years (Wald chi-square, 4.11; P = .043; decreased medication use with bipediculate approach). There was no statistically significant relationship between medication use at any time point in follow-up with cement volume injected (P values for the models ranging from .223 to .875 for the 5 time points of follow-up; mean P value of .603, SD, 0.300) or with presence or absence of leakage (P values for the models ranging from .626 to .947 for the 5 time points of follow-up; mean P value of .846; SD, 0.126).
Discussion
In a retrospective, multivariate analysis of single-level vertebroplasty, we have examined the relationships between several patient- and procedural-related variables and the volume of cement injected during vertebroplasty, and we have specifically described these relationships. From multivariable analysis, treatment of more caudal vertebral levels, a bipediculate approach, the presence of an intravertebral cleft, male gender, and decreased severity of vertebral compression were all independently associated with increased amounts of cement injected. However, there was no significant association between the volume of cement injected during vertebroplasty and the clinical outcomes of pain and medication use at any time point in follow-up, from 1 week to 2 years following the procedure. Across the distribution of cement volumes injected in our practice, the volume of cement injected had no significant bearing on clinical outcomes.
One possible conclusion that can be made is that the clinical efficacy of vertebroplasty is not affected by differences in cement volume injected or at least once a certain threshold amount of cement has been injected—that is, once a volume of cement has been injected that is considered to adequately and safely fill the compressed vertebral body, as determined by the clinical judgment of the operator during the procedure, there may be little or no gain, in terms of pain and medication-use reduction, from injecting additional cement. In fact, efforts to maximize vertebral filling with cement, beyond a reasonable threshold amount, may lead to higher rates of cement leakage. Additionally, asymmetric overfilling of a vertebral body can promote single-sided load transfer and toggle, which is a biomechanically suboptimal result.8
However, speaking against this theory is that we could not appreciate from inspection of our data any particular threshold cement volume needed to achieve pain relief. Unfortunately, predetermination of optimal cement volume is difficult given that it is likely that the minimal amount of cement needed varies with vertebral body volume, percentage compression, and degree of osteoporosis. However, we conclude that practitioners should not feel compelled to increase injected cement volumes beyond that which is reasonable and safe to achieve good clinical outcomes.
We found no statistically significant correlation between cement leakage and the volume of cement injected, and in fact, less cement was injected on average in cases of leakage in our series. This is likely explained by our operators’ immediate cessation of cement injection on detecting any leakage, which may lead to lower total cement volumes injected. Asymptomatic leakage was detected fluoroscopically and noted in 21% of patients, and its presence had no bearing on clinical outcomes.
Although several previous studies have commented on cement volume used in vertebroplasty, we are unaware of any previous multivariable analysis of the effect of cement volumes injected on clinical outcomes in patients who have had only single vertebral levels treated. Other investigations that have commented on cement volumes have been based on populations that were not controlled for the number of vertebral levels treated.12 However, each vertebral fracture can play a separate role in the symptoms of the patient. Failure of pain relief in patients who were treated with vertebroplasty at multiple different levels may potentially represent failure of treatment at 1 or at 2 or at all of these levels.
Therefore, we believe that we cannot adequately control for treatment at multiple levels when studying specific patient and procedural factors that vary among levels treated. To accurately comment on the role of cement volume in outcomes following vertebroplasty, we should best limit analysis to those patients who were treated at a single vertebral level.
Our failure to find an association between cement volume injected and clinical outcomes in this study restricted to single vertebral levels treated is, however, concordant with results previously published by Hodler et al.12 In this study of 152 patients, there was no significant association between cement volume injected per vertebra and immediate postprocedural and midterm clinical outcomes.12
It has been suggested from ex vivo studies of vertebral body strength and stiffness6 that the amount of cement needed to relieve pain clinically may approximate the amount of cement needed to restore the vertebral body’s prefracture mechanical properties.5 Our findings suggest that this may not necessarily be the case and that fracture stabilization and, presumably, associated improvement in clinical outcomes can occur without full restoration of the prefracture properties of strength and stiffness of the vertebral body.
Discordant with prior results,11 our data indicate that volume of cement injected is not significantly associated with the frequency of cement leakage. However, this does not necessarily contradict such previous findings. In our practice, cement injection is always terminated at the first suggestion of leakage. Consequently, the total volume used to treat patients who had leakage was often similar to or even lower than that in patients without leakage.
Our failure to find a significant association between leakage and postprocedural pain was concordant with the findings of Hodler et al,12 Mousavi et al,13 and the midterm follow-up findings of Ryu et al,11 though discordant with the immediate postprocedure findings of Ryu et al and with the intradiskal leakage reported by Alvarez et al.14 We believe, however, that our limitation of study cases to those with single vertebral levels treated produces a better estimate of the effect of leakage on postprocedure clinical outcomes.
We found a significantly lower reported incidence of cement leakage than that in previous studies (21%, compared with the 88% and 72% of Mousavi et al13 and Alavarez et al,14 respectively). This is most likely explained by our identification of leakage from fluoroscopy rather than CT and by our reliance on the dictated procedural notes rather than on images from the procedure themselves.
A significant limitation of our study is that cement volume administered was determined at the discretion of the operator during the procedure rather than being strictly controlled. A randomized trial would be the best way to answer the question of whether, within a certain range, volume of cement injected is associated with clinical outcome. Such a trial, however, may be impossible to carry out because many factors determine the volume of cement injected, not the least of which include safety factors such as leakage during the procedure. Therefore, our conclusions are necessarily based on the results of vertebroplasties performed by a few select operators at our institution, with their individual “senses” of what constitutes an adequate vertebral cement fill. This creates the risk that our results may be peculiar to our institution and, therefore, limited in generalizability. Therefore, we would recommend that our results be confirmed or denied through studies performed at other institutions.
Conclusion
We have failed to demonstrate a significant relationship between volume of cement injected in a compressed vertebral body and clinical outcomes of percutaneous vertebroplasty. Positive clinical outcomes are achieved in our practice with vertebral body filling that is considered adequate and safe by our individual operators, who do not feel compelled to achieve a particular volume of injectant. Vertebroplasty operators need not feel compelled to achieve particular volumes of cement injected but should be guided by their clinical sense of what constitutes an adequate and safe fill of a compressed vertebral body.
References
- 1.Evans AJ, Jensen ME, Kip KE, et al. Vertebral compression fractures: pain reduction and improvement in functional mobility after percutaneous polymethylmethacrylate vertebroplasty retrospective report of 245 cases. Radiology 2003;226:366–72 [DOI] [PubMed] [Google Scholar]
- 2.McGraw JK, Lippert JA, Minkus KD, et al. Prospective evaluation of pain relief in 100 patients undergoing percutaneous vertebroplasty: results and follow-up. J Vasc Interv Radiol 2002;13:883–86 [DOI] [PubMed] [Google Scholar]
- 3.Diamond TH, Champion B, Clark WA. Management of acute osteoporotic vertebral fractures: a nonrandomized trial comparing percutaneous vertebroplasty with conservative therapy. Am J Med 2003;114:257–65 [DOI] [PubMed] [Google Scholar]
- 4.Jensen ME, Evans AJ, Mathis JM, et al. Percutaneous polymethylmethacrylate vertebroplasty in the treatment of osteoporotic vertebral body compression fractures: technical aspects. AJNR Am J Neuroradiol 1997;18:1897–904 [PMC free article] [PubMed] [Google Scholar]
- 5.Mathis JM, Wong W. Percutaneous vertebroplasty: technical considerations. J Vasc Interv Radiol 2003;14:953–60 [DOI] [PubMed] [Google Scholar]
- 6.Belkoff SM, Mathis JM, Jasper LE, et al. The biomechanics of vertebroplasty: the effect of cement volume on mechanical behavior. Spine 2001;26:1537–41 [DOI] [PubMed] [Google Scholar]
- 7.Molloy S, Mathis JM, Belkoff SM. The effect of vertebral body percentage fill on mechanical behavior during percutaneous vertebroplasty. Spine 2003;28:1549–54 [PubMed] [Google Scholar]
- 8.Liebschner MA, Rosenberg WS, Keaveny TM. Effects of bone cement volume and distribution on vertebral stiffness after vertebroplasty. Spine 2001;26:1547–54 [DOI] [PubMed] [Google Scholar]
- 9.Molloy S, Riley LH 3rd, Belkoff SM. Effect of cement volume and placement on mechanical-property restoration resulting from vertebroplasty. AJNR Am J Neuroradiol 2005;26:401–04 [PMC free article] [PubMed] [Google Scholar]
- 10.Wilcox RK. The biomechanics of vertebroplasty: a review. Proc Inst Mech Eng [H] 2004;218:1–10 [DOI] [PubMed] [Google Scholar]
- 11.Ryu KS, Park CK, Kim MC, et al. Dose-dependent epidural leakage of polymethylmethacrylate after percutaneous vertebroplasty in patients with osteoporotic vertebral compression fractures. J Neurosurg 2002;96:56–61 [DOI] [PubMed] [Google Scholar]
- 12.Hodler J, Peck D, Gilula LA. Midterm outcome after vertebroplasty: predictive value of technical and patient-related factors. Radiology 2003;227:662–68 [DOI] [PubMed] [Google Scholar]
- 13.Mousavi P, Roth S, Finkelstein J, et al. Volumetric quantification of cement leakage following percutaneous vertebroplasty in metastatic and osteoporotic vertebrae. J Neurosurg 2003;99:56–59 [DOI] [PubMed] [Google Scholar]
- 14.Alvarez L, Perez-Higueras A, Granizo JJ, et al. Predictors of outcomes of percutaneous vertebroplasty for osteoporotic vertebral fractures. Spine 2005;30:87–92 [DOI] [PubMed] [Google Scholar]