Abstract
Purpose
To assess the characteristics and trends of cardiovascular MRI and CT practitioners and practice in the United States.
Materials and Methods
A retrospective cross-sectional analysis of 2012–2017 Medicare Part B physician payments from the Provider Utilization and Payment Data Physician and Other Supplier Public Use Files (POSPUF) was performed. Characteristics of cardiovascular MRI and CT, including the number of providers and examinations, provider sex and location, and physician reimbursement were analyzed. Variable means, standard deviations, and changes per year were reported and compared.
Results
In 2017, 582 physicians provided cardiovascular MRI services in 45 states, a 16.6% increase from 2016 and an 84.8% increase from 2012. A total of 1645 physicians provided cardiovascular CT services in 49 states, a 14.2% increase from 2016 and a 77.3% increase from 2012. Of the providers, 18.0% and 13.3% of cardiovascular MRI and CT providers were women, respectively, similar to providers’ respective medical specialties. Only 1.0% of radiologists and 0.2% of cardiologists provided cardiovascular MRI services. A total of 3.2% of radiologists and 0.5% of cardiologists provided cardiovascular CT services. Both cardiovascular MRI use (+75.5%) and cardiovascular CT use (+97.4%) increased markedly over the 6-year study period.
Conclusion
Although the availability of cardiovascular MRI and CT is increasing, both are used less frequently in comparison with other cardiovascular imaging modalities.
See also the commentary by Bierhals in this issue.
Supplemental material is available for this article.
© RSNA, 2021
Summary
Although the availability of cardiovascular MRI and CT is increasing, both are used less frequently in comparison with other cardiovascular imaging modalities.
Key Points
■ In 2017, 582 physicians provided cardiovascular MRI services in 45 states, a 16.6% increase from 2016 and an 84.8% increase from 2012.
■ In 2017, 1645 physicians provided cardiovascular CT services in 49 states, a 14.2% increase from 2016 and a 77.3% increase from 2012.
■ Both cardiovascular MRI use (+75.5%) and cardiovascular CT use (+97.4%) increased markedly over the 6-year study period.
Introduction
Technical advances (1), in conjunction with encouraging clinical trials showing improved and comparable outcomes (2–6), have spurred enthusiasm for routine clinical use of cardiovascular MRI and CT in a wide range of cardiovascular disease indications for clinical practice and research trials. In addition, training for these modalities is more widely available than in the past. Available noninvasive cardiovascular MRI diagnostic imaging tools include morphologic, functional, blood flow, and oncologic imaging as well as myocardial tissue characterization, stress testing, and angiography (7). For cardiovascular CT, imaging tools include coronary calcium scoring and coronary angiography in addition to evaluation of cardiovascular structure and function (8). Training requirements (7,9–15), standardized protocols (16), board certification (17,18), and appropriateness criteria (8,19–24) are currently well documented. Nevertheless, outside of professional society memberships, surveys (25–27), and voluntary registries (28,29), little information has been published about the practitioners, practice, and trends of cardiovascular MRI and CT in the United States.
Health care spending in the United States is a major concern and is higher than in other high-income countries (30). Advances in medical technology are one of the primary drivers of increasing health care costs. If health care spending increases continue in the United States, the estimated unfunded Medicare debt will become unsustainable (31). Rapid advances in cardiovascular MRI and CT technology are undeniable, but statewide or national trends in use and cost are unknown. Inappropriate use of imaging is a current concern as an economic issue (32), whereas underuse of appropriate imaging is also a health policy issue. Lower incidence of use of these modalities can be the result of a lack of practitioners with appropriate training as well as the availability of suitable imaging equipment or inadequate financial incentives. Modality use could also be geographically biased in the United States for a variety of factors. Another concern is gender representation in cardiovascular MRI and CT; currently, several efforts are under way to support and increase the number of women in cardiovascular MRI and CT practice. A clear understanding of the current state of cardiovascular MRI and CT in the United States would guide training recommendations and reimbursement and, in the future, affect clinical practice and use.
The purpose of this study was to describe the practice and practitioners of cardiovascular MRI and CT in the Medicare population of the United States and to determine Medicare cardiovascular MRI and CT use, cost, and trends from 2012 to 2017.
Materials and Methods
Part B Medicare Data and Sorting
A retrospective cross-sectional analysis of Medicare physician payments from publicly available information (33) was performed. Direct payments to physicians for fee-for-service Part B Medicare services were analyzed. In the United States, Medicare is a national social insurance program that is administered by the federal government. Medicare provides health insurance for Americans aged 65 years and older who have worked and contributed financially to the Medicare system and others with disabilities. In 2017, 58.4 million people were Medicare enrollees in the United States, approximately 16% of the residence population (34); 49.5 million qualified because of age and 8.9 million because of disability.
The Provider Utilization and Payment Data Physician and Other Supplier Public Use Files (POSPUF) for 2012–2017 each consist of over 9 million lines with 28 data fields. The nine fields listed in Table E1 (supplement) were used in this study and include pertinent demographic, modality usage, and payment information. Eighteen fields including provider name, street address, average charge submitted, and standard deviations of charges submitted were not used for analysis. Data used in this study are publicly available. Hence, use does not require ethics board approval and waives the need for informed consent.
Cardiovascular MRI was identified using the Healthcare Common Procedure Coding System codes (75557–75565; Table E2 [supplement]), and cardiovascular CT was identified using the Healthcare Common Procedure Coding System codes (75571–75574; Table E3 [supplement]). Providers of services were identified by National Provider Identification number. The POSPUF includes data for providers that had a valid National Provider Identification and submitted Medicare Part B noninstitutional claims during the calendar year. To protect the privacy of Medicare beneficiaries, any aggregated records that are derived from 10 or fewer beneficiaries are excluded from the POSPUF.
In addition, all services for cardiovascular MRI and CT providers were extracted from the POSPUF database. The complete Medicare Part B services performed by the specialties with the highest cardiovascular MRI use (cardiology and radiology) were also extracted to compare cardiovascular MRI and CT physicians’ sex, modality use, and payments with those of physicians with similar medical specialty training. Last, echocardiography and nuclear cardiovascular imaging use and payments were analyzed for comparison with cardiovascular MRI and CT.
For services delivered in a nonfacility (ie, office, which is typically nonhospital outpatient) place of service, such as a physician’s office or independent imaging facility, the POSPUF represents the complete payment for the service or the global payment. For services delivered in a facility (typically a hospital) place of service, the data in the POSPUF only represent the physician’s professional fee and does not include any payments to the facility (so-called technical fees). Therefore, payments were analyzed separately for place of service because of the different nature of the payments.
Analysis
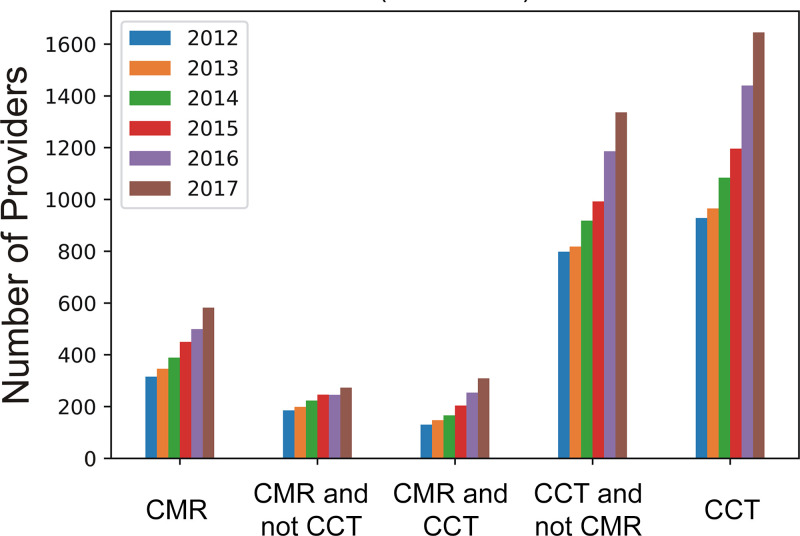
Cardiovascular MRI and CT number of providers, services, and payments were summarized annually. These data were analyzed and visualized as a map to determine the state availability of providers and modality usage. The latest data available from 2017 were detailed in tabular form, and trends were studied. Average change per year (examination count, physician payment, and total payments) in the United States was estimated using:
 |
In addition, generalized estimating equations (35) were used to estimate the average provider change per year (2012–2017) in examinations and payments, taking into account the within-subject effects of including physicians multiple times (yearly and per examination type) as well as possible confounding or interaction with examination type and place of service.
All analyses were performed using the Python programming language, version 3.6.8 (Python Software Foundation, https://www.python.org/), or SAS version 9.4 (SAS Institute, Cary, NC). Maps were generated using RStudio version 1.1.456 (https://www.rstudio.com/).
Results
Cardiovascular MRI and CT Providers
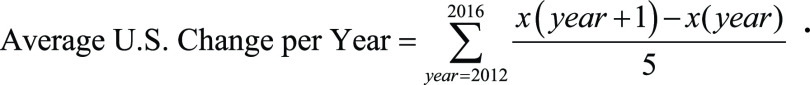
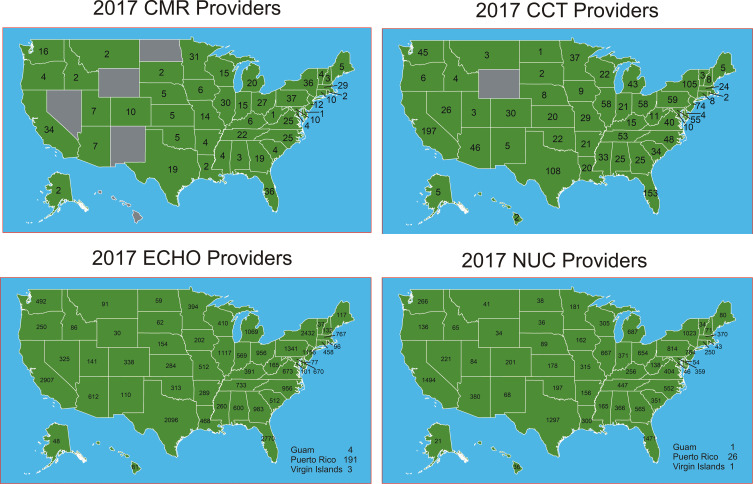
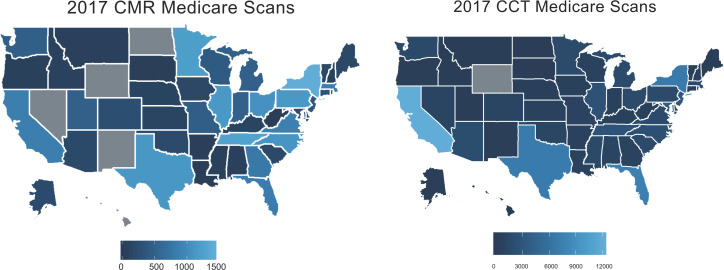
Geographical location.— In 2017, there were 582 physicians providing cardiovascular MRI services in 45 states (Fig 1) for the Medicare Part B population, a 16.6% increase from 2016 and an 84.8% increase from 2012 (Fig 2). From 2012 to 2017, the number of cardiovascular MRI providers increased on average by 53 per year. Five states (Hawaii, North Dakota, New Mexico, Nevada, and Wyoming) did not provide cardiovascular MRI services. Pennsylvania, Florida, New York, California, and Minnesota had the largest number of cardiovascular MRI providers. In 2017, there were 1645 physicians providing cardiovascular CT services in 49 states (Fig 1) for the Medicare Part B population, a 14.2% increase from 2016 and a 77.3% increase from 2012 (Fig 2). From 2012 to 2017, on average, there was an increase of 146 national cardiovascular CT providers per year. Only Wyoming was without cardiovascular CT services. California, Florida, Texas, New York, and New Jersey had the largest number of cardiovascular CT providers. In 2017, of the providers that provided cardiovascular MRI and/or CT, 70% provided CT only, 14% provided MRI only, and the remaining 16% provided both MRI and CT (Fig 2). There were no cardiovascular CT or MRI providers in any U.S. territory, including Puerto Rico and Guam. The number of echocardiography and nuclear cardiac imaging providers exceeded cardiovascular MRI and CT providers in total and in each state.
Figure 1:
Cardiovascular MRI (CMR), CT (CCT), echocardiography (ECHO), and nuclear (NUC) imaging providers per state in 2017.
Figure 2:
Bar graphs show 6-year trends of the number of cardiovascular MRI (CMR) and CT (CCT) providers and the providers that perform both services.
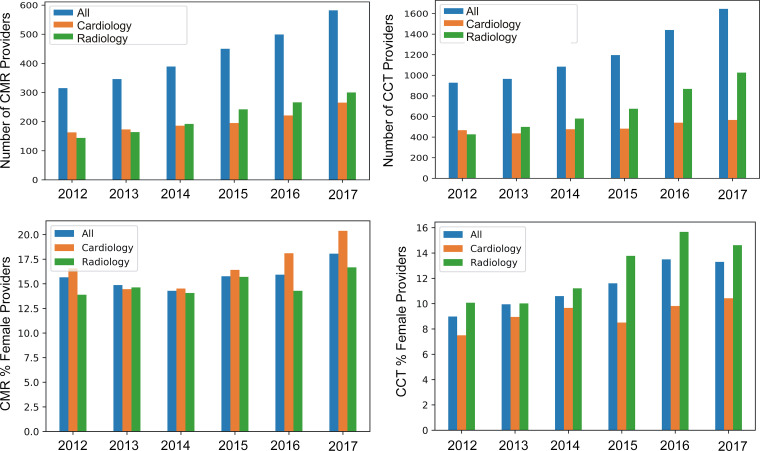
Medical specialty.—Most providers identified as cardiologists or radiologists. In 2012, slightly fewer radiologists than cardiologists provided services for both cardiovascular CT and MRI (Fig 3, top). Over the 6-year time period, the number of cardiovascular MRI and CT radiologists (300 and 1026, respectively) started lower than and then clearly surpassed the number of cardiologists (265 and 566, respectively), especially for cardiovascular CT. Only 1.0% of radiologists and 0.2% of cardiologists provided cardiovascular MRI services, whereas 3.2% of radiologists and 0.5% of cardiologists provided cardiovascular CT services.
Figure 3:
Bar graphs show temporal changes in number (top) and sex (bottom) of cardiovascular MRI (CMR) and CT (CCT) providers in the most common medical specializations (cardiology and radiology).
Sex of provider.—Cardiovascular CT and MRI providers were mostly men (Fig 3, bottom). In 2017, 18.0% and 13.3% of cardiovascular MRI and CT providers were women, respectively. Over the study period, the cardiovascular MRI gender gap remained fairly constant, while the cardiovascular CT gender gap narrowed slightly, with a 4.3% increase in women practitioners. Compared with all Medicare providers (43.3% women), cardiovascular MRI and CT have a wide gender disparity. Conversely, when compared with radiology (22.8% women), cardiology (12.8% women), echocardiography (13.9% women), and nuclear cardiology (11.8% women) providers, the gap could be viewed as similar. Radiology representation of women was below average for cardiovascular MRI and CT, 16.7% and 14.6%, respectively, versus 22.8% for radiologists. The percentage of women cardiology providers was markedly above for cardiovascular MRI, but below for cardiovascular CT, respectively 20.4% and 10.4% versus 12.8% for cardiologists.
Cardiovascular MRI and CT Use and Cost
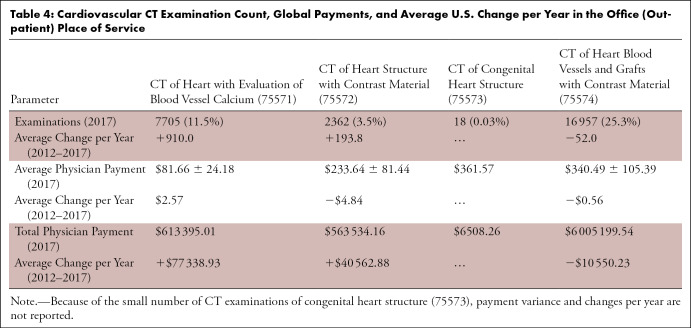
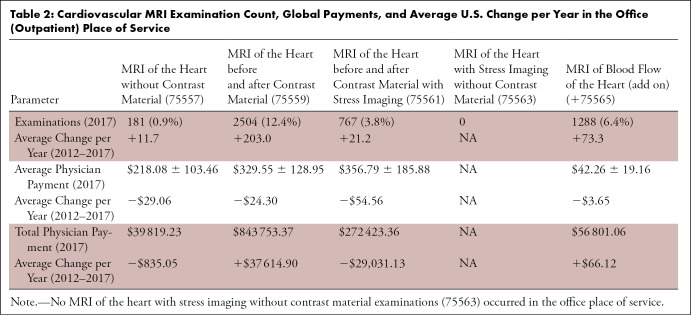
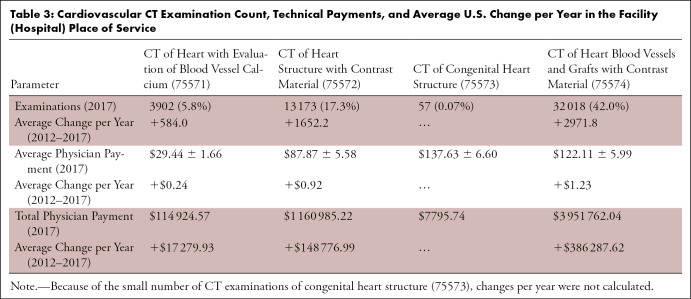
Payments by state.—The total amount paid to these health care providers during the 6-year time period was 16.2 million dollars for 89 494 cardiovascular MRI examinations and 55.8 million dollars for 318 608 cardiovascular CT examinations. In contrast, there were 5.2 million echocardiography examinations with payments of 5.9 billion dollars and 13.7 million nuclear cardiology examinations with payments of 4.2 billion dollars. Both cardiovascular MRI (+75.5%) and CT (+97.4%) use increased markedly over the period (Fig 4 and Tables 1–4) to 20 137 MRI examinations and 76 192 cardiovascular CT examinations. New York, Tennessee, Minnesota, Illinois, and Pennsylvania performed the highest number of cardiovascular MRI examinations (Fig 5). California, Florida, Texas, New York, and Maryland performed the highest number of cardiovascular CT examinations (Fig 5).
Figure 4:
Bar graphs show the 6-year trends in cardiovascular MRI (CMR [left]) and CT (CCT [right]) examination usage.
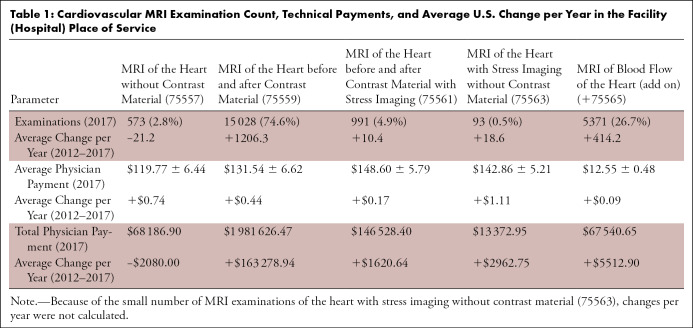
Table 1:
Cardiovascular MRI Examination Count, Technical Payments, and Average U.S. Change per Year in the Facility (Hospital) Place of Service
Table 4:
Cardiovascular CT Examination Count, Global Payments, and Average U.S. Change per Year in the Office (Outpatient) Place of Service
Figure 5:
Cardiovascular MRI (CMR) and CT (CCT) examinations per state in 2017.
Table 2:
Cardiovascular MRI Examination Count, Global Payments, and Average U.S. Change per Year in the Office (Outpatient) Place of Service
Table 3:
Cardiovascular CT Examination Count, Technical Payments, and Average U.S. Change per Year in the Facility (Hospital) Place of Service
Payments by examination subtype.—Rarely were stress cardiovascular MRI without contrast material (code 75557) and cardiovascular CT of the congenital heart (code 75573) performed. In 2017, 58 cardiovascular MRI physicians (10.4% women and 10.0% of all cardiovascular MRI physicians) provided 1851 cardiovascular MRI stress examinations (9.1% of 2017 cardiovascular MRI examinations). Cardiovascular MRI without contrast material did not have the same growth as cardiovascular MRI with contrast material (1419 examinations per year), and only 4.2% of the examinations in 2017 were performed without contrast material. The cardiovascular MRI professional payment did not change over the period (Fig 6), but the global payment was reduced for cardiovascular MRI with contrast material at an average rate of −$30.64 per year in the United States. A total of 83% were performed in the facility (hospital) place of service, and 33% were performed with blood flow measurements (code 75565). Cardiovascular MRI blood flow usage peaked in 2017 at 6659 examinations, a 78.3% increase from 2012, but remained a fraction of the echocardiography Doppler flow use of 8.4 million examinations. The decrease in cardiovascular MRI reimbursements was offset by an increase in usage, yielding a substantial increase in total payments for cardiovascular MRI. In contrast, cardiovascular CT payments changed only slightly over the time period (Fig 6), and a lower percentage of cardiovascular CT examinations (64%) were performed in the facility (hospital) place of service. Except for 66% of calcium scores, most cardiovascular CT examinations were performed in the office or in an outpatient place of service.
Figure 6:
Bar graphs show 6-year trends of cardiovascular MRI (CMR [top]) and CT (CCT [bottom]) professional payments in the office and/or outpatient place of service (left) and global payments (professional and technical) in the facility (hospital) place of service (right). No MRI of the heart without contrast material with stress (75559) examinations were performed in the facility setting (2013–2017).
Payments by geographical location.—When cardiovascular MRI and CT providers and use were normalized to the number of Medicare enrollees in each state, different state usage was observed (Fig E1 and E2 [supplement]). Analysis of Medicare enrollees per provider for each state (Fig E1 [supplement]) showed the availability of providers was best for cardiovascular MRI in Minnesota, the District of Columbia, Vermont, Utah, and Massachusetts and for cardiovascular CT in the District of Columbia, Minnesota, New York, Maryland, and Mississippi. Use per Medicare enrollee (Fig E2 [supplement]) was highest in Minnesota, the District of Columbia, Arkansas, Utah, and Tennessee for cardiovascular MRI and the District of Columbia, Maryland, Minnesota, California, and New York for cardiovascular CT.
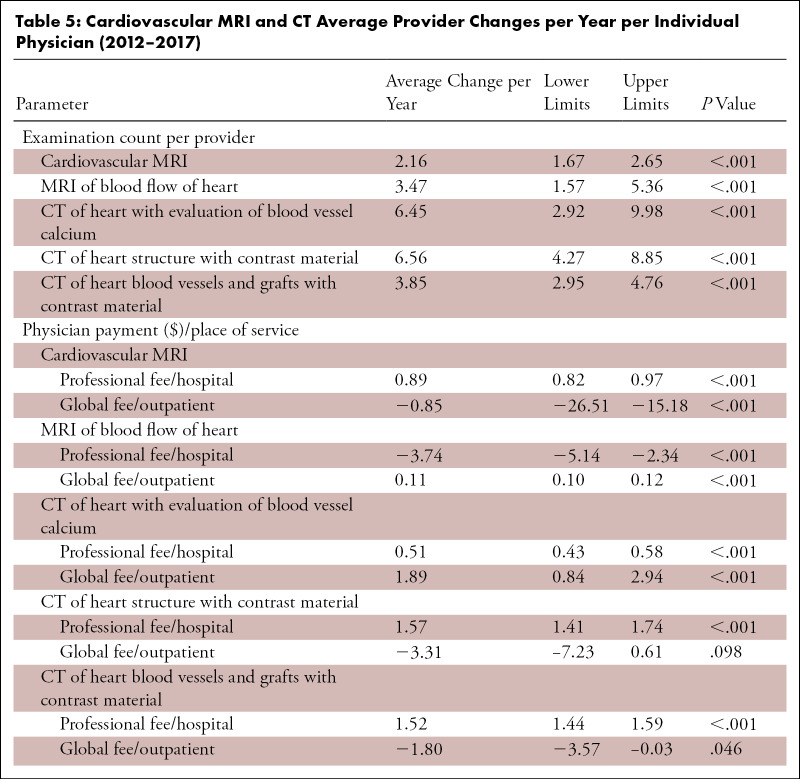
Per provider use and payments.—Individual provider utilization increased significantly over the study time period (Table 5). The cardiovascular MRI average change per year per provider was 2.16 examinations per year, and flow imaging increased at a yearly rate of 3.47 examinations per provider. Cardiovascular CT average change per year per provider also increased significantly at a yearly rate of 3.85–6.56 examinations per provider (Table 5). Examination per provider payments changed significantly on average over the time period by a small amount per year (−$3.74 to +$1.89).
Table 5:
Cardiovascular MRI and CT Average Provider Changes per Year per Individual Physician (2012–2017)
Discussion
As evidenced by the analysis of Part B Medicare payments to physicians (2012–2017), cardiovascular MRI and CT use along with the number practitioners in the United States was robustly increasing but remained a small fraction of overall cardiovascular imaging practice. In 2017, there were 582 physicians providing cardiovascular MRI services (an 84.8% increase from 2012) and 1645 physicians providing cardiovascular CT services (a 77.3% increase from 2012). Less than 1.0% of cardiologists provided cardiovascular MRI and CT services. A total of 3.2% of radiologists provided cardiovascular CT services, and 1.0% provided cardiovascular MRI services. In 2017, an increasing number of examinations continued with performance of 20 137 cardiovascular MRI examinations and 76 192 cardiovascular CT examinations, a 75% and 97% increase from 2012, respectively. Even with the increases in providers and use, a few states did not provide Medicare Part B cardiovascular MRI and CT services. The data of this study supported regional increases in cardiovascular MRI and CT providers, but probably not U.S.-wide increases because of the low volume per reader. Increases in reimbursement may be supported by this study because of the time requirements and expense of cardiovascular MRI and CT. Although the straightforward path for increased acceptance is not certain, availability in terms of trained providers, software, and equipment such that examinations can be performed promptly would be advantageous.
With few exceptions, most providers were radiologists or cardiologists. Cardiovascular MRI services were split between the two specialties over the study time period, but cardiovascular CT services were increasingly provided by radiologists, starting in 2012 with 0.91 radiologists per cardiologist and ending in 2017 with 1.8 radiologists per cardiologist providing cardiovascular CT services. This mirrors trends observed in general CT angiography (36) and a prior study on cardiovascular CT (37). A disparity in gender (10%–20% women) was evident compared with general Medicare physicians, but this disparity was comparable to that of similar medical specialties and cardiovascular imaging physicians. Gender parity (38) is important in advanced subspecialty training not only for patient care bias, but also by providing advancement for academic and leadership positions. Professional fees remained constant ($100–$150) over the study period, but technical fees dropped significantly from 2012 levels. Compared with 2012, 2017 global (professional and technical) payments for cardiovascular MRI with contrast material dropped 30.7% and cardiovascular MRI stress testing reimbursements with contrast material fell by 47.8%.
Cardiovascular MRI is represented in two-thirds of American Heart Association and American College of Cardiology guidelines (39), but when compared with European Society of Cardiology guidelines, cardiovascular MRI is less represented, in particular in the area of coronary artery disease. This supports the common belief that cardiovascular MRI is better implemented outside of the United States. Cardiovascular MRI and CT are routinely practiced in academic or training centers and large medical centers and less commonly in private practice.
Complementary data are available from 2016 to 2020 on cardiovascular MRI Hospital Outpatient Prospective Payment System technical payment trends. Each year, the Centers for Medicaid and Medicare Services updates Medicare payment rates for partial hospitalization program services furnished in hospital outpatient departments and community mental health centers. The Society for Cardiovascular Magnetic Resonance Imaging, American Society of Nuclear Cardiology, and Society of Cardiovascular Computed Tomography monitor and report these Medicare reimbursement changes. In 2017, there were large reductions in payments for cardiovascular MRI in the Hospital Outpatient Prospective Payment System setting (Table E4 [supplement]). In 2019, the Centers for Medicaid and Medicare Services moved both stress cardiovascular MRI codes (75559 and 75563) from the nuclear Ambulatory Payment Classification (APC) group into the general radiology APC groups. Reimbursement rates are affected by several factors. Codes in the same APC groups receive similar reimbursement. This action was followed by a doubling of stress cardiovascular MRI without contrast material examinations (code 75559) in 2019 as a result of another APC change. Note that this cardiovascular MRI examination is rarely used. Conversely, CT calcium scoring saw a large increase (+371%) in reimbursement in 2017 (Table E5 [supplement]). In addition, a 30.5% increase in CT calcium scoring (code 75571) reimbursement was finalized for 2020. From 2018 to 2020, other cardiovascular CT rates were markedly reduced.
The observed trends may guide future imaging-related policies. Several factors should be taken into consideration because they may affect cardiovascular MRI and CT in the United States. Rapid technical developments increase indications and ease of use and reduce cost. Large clinical multicenter prospective trials and registries may further support efficient use of cardiovascular MRI and CT in routine clinical practice. One study showed that cardiovascular MRI with contrast material is possible in the developing world in 18 minutes for $150 and resulted in important changes in patient care (40). Board certification in cardiovascular MRI and CT is recently available (17,18). Also, training requirements have been well documented. All standard 3-year training programs in cardiology must provide cardiovascular MRI and CT Level I training and should provide enough time for Level II training (requirement to perform and interpret cardiovascular MRI examinations as part of the practice of cardiovascular medicine). Last, the Protecting Access to Medicare Act of 2014, Section 218 (b), established a new program to increase the rate of appropriate advanced diagnostic imaging services provided to Medicare beneficiaries (41). It is unknown how this will affect usage in the short- and long-term periods. In the future, cardiovascular MRI and CT practitioners and use in the Medicare population should be routinely monitored to provide clear insight into practice in the United States.
The main assumption in this report was that cardiovascular MRI and CT Part B Medicare payments to physicians were representative of cardiovascular MRI and CT practice in the United States and could be generalized to examinations reimbursed by other health insurances. Medicare is the primary health insurance for disabled and elderly individuals. The use of private insurance is not considered in this report. More than 34% of Medicare beneficiaries have chosen to enroll in Part C private health plans that contract with Medicare to provide Part A and Part B health services (42). The POSPUF database does not include Part C Medicare payments, so it underrepresents the total Medicare examinations but should closely represent the Medicare physicians. Acknowledging the limitations of this study, the exact number of practitioners as well as cardiovascular MRI and CT examinations were not provided in this report. Limitations aside, this report provided clear data on usage of cardiovascular MRI and cardiovascular CT in the population that participates in Medicare Part B. Largely, private insurance companies often follow Medicare reimbursement decisions for coverage and reimbursement.
The results of this study suggested that cardiovascular MRI and CT use in the United States was steadily increasing but remained a small fraction of all cardiovascular imaging. Less than 20% of providers are women, similar to radiology and cardiology gender statistics. Echocardiography and nuclear imaging are still the most used cardiovascular imaging modalities. It remains to be seen if past trends of increasing usage and availability of providers will continue.
SUPPLEMENTAL TABLES
SUPPLEMENTAL FIGURES
Disclosures of Conflicts of Interest: J.W.G. disclosed no relevant relationships. J.W. disclosed no relevant relationships.
Author contributions: Guarantor of integrity of entire study, J.W.G.; study concepts/study design or data acquisition or data analysis/interpretation, J.W.G., J.W.; manuscript drafting or manuscript revision for important intellectual content, J.W.G., J.W.; approval of final version of submitted manuscript, J.W.G., J.W.; agrees to ensure any questions related to the work are appropriately resolved, J.W.G., J.W.; literature research, J.W.G.; statistical analysis, J.W.G., J.W.; and manuscript editing, J.W.G., J.W.
Abbreviations:
- APC
- Ambulatory Payment Classification
- POSPUF
- Provider Utilization and Payment Data Physician and Other Supplier Public Use Files
References
- 1.Chaikriangkrai K, Choi SY, Nabi F, Chang SM. Important advances in technology and unique applications to cardiovascular computed tomography. Methodist DeBakey Cardiovasc J 2014;10(3):152–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jørgensen ME, Andersson C, Nørgaard BL, et al. Functional Testing or Coronary Computed Tomography Angiography in Patients With Stable Coronary Artery Disease. J Am Coll Cardiol 2017;69(14):1761–1770. [DOI] [PubMed] [Google Scholar]
- 3.SCOT-HEART Investigators ; Newby DE, Adamson PD, et al. Coronary CT Angiography and 5-Year Risk of Myocardial Infarction. N Engl J Med 2018;379(10):924–933. [DOI] [PubMed] [Google Scholar]
- 4.Hoffmann U, Ferencik M, Udelson JE, et al. Prognostic Value of Noninvasive Cardiovascular Testing in Patients With Stable Chest Pain: Insights From the PROMISE Trial (Prospective Multicenter Imaging Study for Evaluation of Chest Pain). Circulation 2017;135(24):2320–2332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nagel E, Greenwood JP, McCann GP, et al. Magnetic Resonance Perfusion or Fractional Flow Reserve in Coronary Disease. N Engl J Med 2019;380(25):2418–2428. [DOI] [PubMed] [Google Scholar]
- 6.Greenwood JP, Maredia N, Younger JF, et al. Cardiovascular magnetic resonance and single-photon emission computed tomography for diagnosis of coronary heart disease (CE-MARC): a prospective trial. Lancet 2012;379(9814):453–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kramer CM, Hundley WG, Kwong RY, Martinez MW, Raman SV, Ward RP. COCATS 4 Task Force 8: Training in Cardiovascular Magnetic Resonance Imaging. J Am Coll Cardiol 2015;65(17):1822–1831. [DOI] [PubMed] [Google Scholar]
- 8.Doherty JU, Kort S, Mehran R, et al. ACC/AATS/AHA/ASE/ASNC/HRS/SCAI/SCCT/SCMR/STS 2019 Appropriate Use Criteria for Multimodality Imaging in the Assessment of Cardiac Structure and Function in Nonvalvular Heart Disease: A Report of the American College of Cardiology Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and the Society of Thoracic Surgeons. J Nucl Cardiol 2019;26(4):1392–1413. [DOI] [PubMed] [Google Scholar]
- 9.Garcia MJ, Blankstein R, Budoff MJ, et al. COCATS 4 Task Force 7: Training in Cardiovascular Computed Tomographic Imaging: Endorsed by the American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Atherosclerosis Imaging and Prevention, and the Society of Cardiovascular Computed Tomography. J Nucl Cardiol 2015;22(4):826–839. [DOI] [PubMed] [Google Scholar]
- 10.Garcia MJ, Blankstein R, Budoff MJ, et al. COCATS 4 Task Force 7: Training in Cardiovascular Computed Tomographic Imaging. J Am Coll Cardiol 2015;65(17):1810–1821. [DOI] [PubMed] [Google Scholar]
- 11.Kim RJ, Simonetti OP, Westwood M, et al. Guidelines for training in cardiovascular magnetic resonance (CMR). J Cardiovasc Magn Reson 2018;20(1):57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Narula J, Chandrashekhar YS, Dilsizian V, et al. COCATS 4 Task Force 4: Training in Multimodality Imaging. J Am Coll Cardiol 2015;65(17):1778–1785. [DOI] [PubMed] [Google Scholar]
- 13.Pelberg R, Budoff M, Goraya T, et al. Training, competency, and certification in cardiac CT: a summary statement from the Society of Cardiovascular Computed Tomography. J Cardiovasc Comput Tomogr 2011;5(5):279–285. [DOI] [PubMed] [Google Scholar]
- 14.Petersen SE, Almeida AG, Alpendurada F, et al. Update of the European Association of Cardiovascular Imaging (EACVI) Core Syllabus for the European Cardiovascular Magnetic Resonance Certification Exam. Eur Heart J Cardiovasc Imaging 2014;15(7):728–729. [DOI] [PubMed] [Google Scholar]
- 15.Choi AD, Thomas DM, Lee J, et al. 2020 SCCT Guideline for Training Cardiology and Radiology Trainees as Independent Practitioners (Level II) and Advanced Practitioners (Level III) in Cardiovascular Computed Tomography: A Statement from the Society of Cardiovascular Computed Tomography. JACC Cardiovasc Imaging 2020. 10.1016/j.jcmg.2020.09.004. Published online November 4, 2020. [DOI] [PubMed] [Google Scholar]
- 16.Kramer CM, Barkhausen J, Bucciarelli-Ducci C, Flamm SD, Kim RJ, Nagel E. Standardized cardiovascular magnetic resonance imaging (CMR) protocols: 2020 update. J Cardiovasc Magn Reson 2020;22(1):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Min JK, Abbara S, Berman DS, et al. Blueprint of the certification examination in cardiovascular computed tomography. J Cardiovasc Comput Tomogr 2008;2(4):263–271. [DOI] [PubMed] [Google Scholar]
- 18.Alliance for Physician Certification & Advancement . Certification Board of Cardiovascular Magnetic Resonance (CBCMR). https://www.apca.org/certifications-examinations/cbnc-and-cbcct/certification-board-of-cardiovascular-magnetic-resonance/. Published 2019. Accessed January 2021. [Google Scholar]
- 19.Earls JP, Woodard PK, Abbara S, et al. ACR appropriateness criteria asymptomatic patient at risk for coronary artery disease. J Am Coll Radiol 2014;11(1):12–19. [DOI] [PubMed] [Google Scholar]
- 20.Ho VB. ACR appropriateness criteria on suspected congenital heart disease in adults. J Am Coll Radiol 2008;5(2):97–104. [DOI] [PubMed] [Google Scholar]
- 21.Hoffmann U, Venkatesh V, White RD, et al. ACR Appropriateness Criteria(®) acute nonspecific chest pain: low probability of coronary artery disease. J Am Coll Radiol 2012;9(10):745–750. [DOI] [PubMed] [Google Scholar]
- 22.Garbi M, Habib G, Plein S, et al. Appropriateness criteria for cardiovascular imaging use in clinical practice: a position statement of the ESC/EACVI taskforce. Eur Heart J Cardiovasc Imaging 2014;15(5):477–482. [DOI] [PubMed] [Google Scholar]
- 23.Garbi M, McDonagh T, Cosyns B, et al. Appropriateness criteria for cardiovascular imaging use in heart failure: report of literature review. Eur Heart J Cardiovasc Imaging 2015;16(2):147–153. [DOI] [PubMed] [Google Scholar]
- 24.Leiner T, Bogaert J, Friedrich MG, et al. SCMR Position Paper (2020) on clinical indications for cardiovascular magnetic resonance. J Cardiovasc Magn Reson 2020;22(1):76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roifman I, Paterson DI, Jimenez-Juan L, et al. The State of Cardiovascular Magnetic Resonance Imaging in Canada: Results from the CanSCMR Pan-Canadian Survey. Can J Cardiol 2018;34(3):333–336. [DOI] [PubMed] [Google Scholar]
- 26.Moody WE, Hudsmith LE, Holloway B, et al. Variation in cardiovascular magnetic resonance myocardial contouring: insights from an international survey. J Magn Reson Imaging 2019;50(4):1336–1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu K, Hsieh C, Zhuang N, et al. Current utilization of cardiac computed tomography in mainland China: a national survey. J Cardiovasc Comput Tomogr 2016;10(1):76–81. [DOI] [PubMed] [Google Scholar]
- 28.Global Cardiovascular Magnetic Resonance Registry (GCMR) Investigators ; Kwong RY, Petersen SE, et al. The global cardiovascular magnetic resonance registry (GCMR) of the Society for Cardiovascular Magnetic Resonance (SCMR): its goals, rationale, data infrastructure, and current developments. J Cardiovasc Magn Reson 2017;19(1):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Han BK, Casey S, Witt D, et al. Development of a congenital cardiovascular computed tomography imaging registry: rationale and implementation. J Cardiovasc Comput Tomogr 2018;12(3):263–266. [DOI] [PubMed] [Google Scholar]
- 30.Papanicolas I, Woskie LR, Jha AK. Health Care Spending in the United States and Other High-Income Countries. JAMA 2018;319(10):1024–1039 [Published correction appears in JAMA 2018;319(17):1824.]. [DOI] [PubMed] [Google Scholar]
- 31.Ferrari VA, Whitman B, Blankenship JC, et al. Cardiovascular imaging payment and reimbursement systems: understanding the past and present in order to guide the future. JACC Cardiovasc Imaging 2014;7(3):324–332. [DOI] [PubMed] [Google Scholar]
- 32.Shrank WH, Rogstad TL, Parekh N. Waste in the US Health Care System: Estimated Costs and Potential for Savings. JAMA 2019;322(15):1501–1509. [DOI] [PubMed] [Google Scholar]
- 33.Centers for Medicare & Medicaid Services . Medicare Provider Utilization and Payment Data: Physician and Other Supplier. https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/medicare-provider-charge-data/physician-and-other-supplier.html. Accessed January 2021.
- 34.Centers for Medicare & Medicaid Services . Medicare & Medicaid Statistical Supplement. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/MedicareMedicaidStatSupp/2013.html. Published October 18, 2019. Accessed January 2021.
- 35.Fitzmaurice GM, Laird NM, Ware JH. Applied Longitudinal Analysis. 2nd ed. Hoboken, NJ: Wiley, 2011; 353–394. [Google Scholar]
- 36.Prabhakar AM, Misono AS, Hemingway J, Hughes DR, Duszak R Jr. Medicare Utilization of CT Angiography from 2001 through 2014: Continued Growth by Radiologists. J Vasc Interv Radiol 2016;27(10):1554–1560. [DOI] [PubMed] [Google Scholar]
- 37.Levin DC, Parker L, Halpern EJ, Rao VM. Coronary CT Angiography: Reversal of Earlier Utilization Trends. J Am Coll Radiol 2019;16(2):147–155. [DOI] [PubMed] [Google Scholar]
- 38.Hillman BJ. Gender Bias. J Am Coll Radiol 2018;15(8):1061. [DOI] [PubMed] [Google Scholar]
- 39.von Knobelsdorff-Brenkenhoff F, Pilz G, Schulz-Menger J. Representation of cardiovascular magnetic resonance in the AHA/ACC guidelines. J Cardiovasc Magn Reson 2017;19(1):70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Menacho K, Ramirez S, Segura P, et al. INCA (Peru) Study: Impact of Non-Invasive Cardiac Magnetic Resonance Assessment in the Developing World. J Am Heart Assoc 2018;7(17):e008981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cooke R. Utilization Management and ACR Select. Radiol Manage 2015;37(2):9–12. [PubMed] [Google Scholar]
- 42.Yoon YE, Hong YJ, Kim HK, et al. 2014 Korean Guidelines for Appropriate Utilization of Cardiovascular Magnetic Resonance Imaging: A Joint Report of the Korean Society of Cardiology and the Korean Society of Radiology. Korean Circ J 2014;44(6):359–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.



![Bar graphs show the 6-year trends in cardiovascular MRI (CMR [left]) and CT (CCT [right]) examination usage.](https://cdn.ncbi.nlm.nih.gov/pmc/blobs/245b/7977977/1c23da3a6717/ryct.2021200112.fig4.jpg)
![Bar graphs show 6-year trends of cardiovascular MRI (CMR [top]) and CT (CCT [bottom]) professional payments in the office and/or outpatient place of service (left) and global payments (professional and technical) in the facility (hospital) place of service (right). No MRI of the heart without contrast material with stress (75559) examinations were performed in the facility setting (2013–2017).](https://cdn.ncbi.nlm.nih.gov/pmc/blobs/245b/7977977/23bae640df21/ryct.2021200112.fig6.jpg)