Abstract
Noninvasive fractional flow reserve derived from coronary CT angiography (FFRCT) is increasingly used in patients with coronary artery disease as a gatekeeper to the catheterization laboratory. While there is emerging evidence of the clinical benefit of FFRCT in patients with moderate coronary disease as determined with coronary CT angiography, there has been less focus on interpretation, reporting, and integration of FFRCT results into routine clinical practice. Because FFRCT analysis provides a plethora of information regarding pressure and flow across the entire coronary tree, standardized criteria on interpretation and reporting of the FFRCT analysis result are of crucial importance both in context of the clinical adoption and in future research. This report represents expert opinion and recommendation on a standardized FFRCT interpretation and reporting approach.
Published under a CC BY 4.0 license.
Summary
Expert opinion and recommendation was given by an independent group of physicians on a standardized interpretation and reporting approach for CT-derived fractional flow reserve testing supported by years of clinical experience.
Key Points
■ Standardized criteria on interpretation and reporting of CT-derived fractional flow reserve (FFRCT) analysis results are of importance both in context of their clinical adoption and in future research.
■ Use of the FFRCT value 10–20 mm distal to the lower border of the stenosis for decision making is recommended.
■ We recommend for clinical decision making a dichotomous interpretation strategy to be considered only in lesions with FFRCT greater than 0.80 or lower than or equal to 0.75, whereas, in patients with FFRCT ranging between 0.76 and 0.80, additional risk stratification information is needed.
■ The results of FFRCT must be evaluated in their clinical context, taking into account patient symptoms, the coronary anatomy, and suitability of revascularization.
Introduction
Since the first study on coronary CT angiography–derived fractional flow reserve (CT FFR) diagnostic performance by Koo and colleagues in 2011 (1), an abundance of data pertaining to this modality has been published. Several tools have been introduced for the calculation of CT FFR (1–3); however, the majority of existing evidence and clinical experience is based on the HeartFlow FFRCT method (HeartFlow, Redwood City, Calif), which is the only CT FFR cleared by the United States Food and Drug Administration (4) and endorsed by the National Institute for Health and Care Excellence in the United Kingdom (5). Comprehensive reviews of the principle of FFRCT have been described previously (6–8). FFRCT assessment is increasingly used in mainstream clinical practice (9–14) and is likely to further expand with the increased utilization of coronary CT angiography as a first-line test in patients suspected of having coronary artery disease (CAD). While there has been much focus on the diagnostic performance and potential clinical utility of FFRCT in patients with moderate CAD (9–18), there has been less focus on interpretation, reporting, and integration of FFRCT results into routine clinical practice (19). A broadly adopted standardized FFRCT interpretation and reporting approach providing rich and consistent information may facilitate more appropriate clinical implementation and stimulate further high-quality research. Thus, this report, which was written by an independent group of physicians with years of clinical experience with FFRCT, proposes standardized criteria for FFRCT interpretation and reporting for application in clinical practice and for clinical research.
FFR versus FFRCT
FFRCT provides simultaneous calculation of pressure and flow across the entire coronary tree (Fig 1). In contrast, information pertaining to invasively measured FFR is only available in vessels that have been interrogated with the pressure wire, which is typically decided during invasive coronary angiography at the discretion of the interventionists (20). While anatomic percentage of stenosis is evaluated at the location of the lesion, invasive FFR is typically measured by positioning the pressure sensor in the distal part of the vessel and then manually pulling the pressure sensor back to the ostium to assess the distribution of abnormal epicardial resistance along the course of the vessel (20). In both invasive FFR and FFRCT, the distal values in any given vessel reflect the cumulative pressure loss and impact of all disease proximal to the measurement location. Values obtained by both techniques may vary depending on the measurement location within a vessel. Accordingly, in vessels that have been assessed using both techniques, if the measurement locations of invasive FFR and FFRCT are not matched, their values can be different and may not closely correlate.
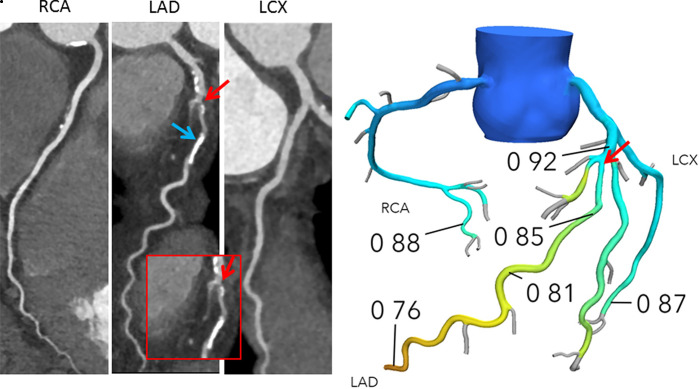
Figure 1a:
(a) Interpretation of FFRCT results in a 65-year-old woman with typical angina. Agatston score, 333. Left: Coronary CT angiography curved multiplanar reconstructions demonstrate a 50%–69% proximal left anterior descending artery (LAD) stenosis (red arrow) and in the mid-LAD, nonobstructive diffuse disease. The blue arrow indicates where the lesion-specific FFRCT value was assessed. Right: In the FFRCT three-dimensional model, the FFRCT value 16 mm distal to the stenosis was 0.85, indicating that the lesion did not cause significant pressure loss. However, FFRCT was significantly low (0.76) in the terminal vessel segments. (b) Interpretation of FFRCT results in a 63-year-old man with atypical angina. Agatston score, 245. Left: Coronary CT angiographic images demonstrate a 50%–69% proximal LAD stenosis (red arrow). The blue arrow indicates where the lesion-specific FFRCT value was assessed. Right: In the FFRCT three-dimensional model, the FFRCT value 14 mm distal to the stenosis indicated that the lesion was hemodynamically significant with a value of 0.69. Coronary CT angiography and FFRCT reporting are demonstrated in Figure 4. LCX = left circumflex coronary artery, RCA = right coronary artery.
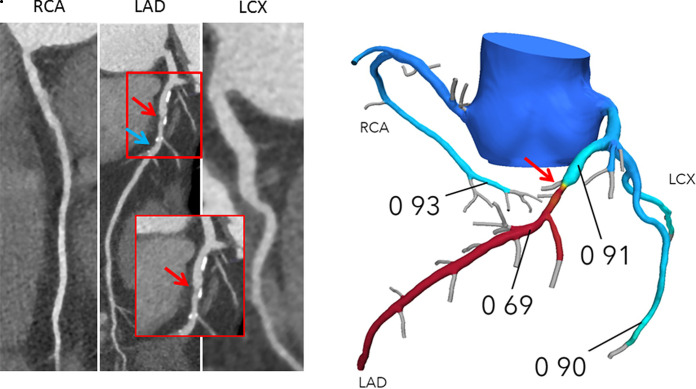
Figure 1b:
(a) Interpretation of FFRCT results in a 65-year-old woman with typical angina. Agatston score, 333. Left: Coronary CT angiography curved multiplanar reconstructions demonstrate a 50%–69% proximal left anterior descending artery (LAD) stenosis (red arrow) and in the mid-LAD, nonobstructive diffuse disease. The blue arrow indicates where the lesion-specific FFRCT value was assessed. Right: In the FFRCT three-dimensional model, the FFRCT value 16 mm distal to the stenosis was 0.85, indicating that the lesion did not cause significant pressure loss. However, FFRCT was significantly low (0.76) in the terminal vessel segments. (b) Interpretation of FFRCT results in a 63-year-old man with atypical angina. Agatston score, 245. Left: Coronary CT angiographic images demonstrate a 50%–69% proximal LAD stenosis (red arrow). The blue arrow indicates where the lesion-specific FFRCT value was assessed. Right: In the FFRCT three-dimensional model, the FFRCT value 14 mm distal to the stenosis indicated that the lesion was hemodynamically significant with a value of 0.69. Coronary CT angiography and FFRCT reporting are demonstrated in Figure 4. LCX = left circumflex coronary artery, RCA = right coronary artery.
FFRCT Interpretation
As for CT angiography, FFRCT interpretation should be performed by the local imaging experts determined by level of clinical knowledge and practical experience with the technique. This may include cardiologists and/or radiologists. It is recommended that downstream management decision making beyond FFRCT takes into account both the clinical scenario (symptoms, risk profile, and/or comorbid conditions) and the coronary anatomy.
Evaluation of CT Angiography and Lesion Location
The first step in the interpretation of FFRCT is to re-examine the original coronary CT angiography study with particular focus on the location and severity of detailed anatomic lesions (Table). Because FFRCT declines along the length of the vessel with serial focal lesions or areas of diffuse disease, it is important to correlate the pressure loss to specific lesions, which can only be established by direct comparison between the CT angiography lesion location and the FFRCT three-dimensional coronary tree model in relation to identifiable vessel landmarks, such as origin, branches, and segments. It is recommended that this first step be performed by using the Society of Cardiovascular Computed Tomography (SCCT) coronary segmentation model (21).
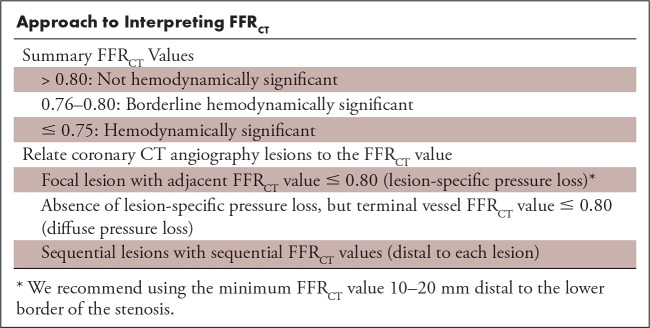
Approach to Interpreting FFRCT
FFRCT Threshold
There is high per-patient and per-vessel agreement between FFRCT and invasive FFR using the threshold of 0.80 for both techniques (1,15–18). An FFRCT value greater than 0.80 indicates that the lesion is unlikely to be hemodynamically significant and that the patient can be safely treated with optimal medical treatment without further downstream testing (1,12–18,22,23). A poststenotic FFRCT value less than or equal to 0.80 indicates the possibility of hemodynamic significance (1,15–18). The use of this dichotomous FFRCT threshold to guide treatment decisions, namely to avoid further downstream testing or consider invasive angiography and revascularization, remains controversial, as it is well known from the invasive literature that the greatest benefit of revascularization is obtained in patients with the most severe pressure loss (24,25). We recommend a dichotomous interpretation strategy to be considered in lesions with FFRCT greater than 0.80 or less than or equal to 0.75 (ie, values >0.80 are “normal” and values ≤0.75 are associated with high likelihood of hemodynamic significance) (Table, Figure 2). Several factors support this strategy. First, FFRCT values are lower than measured FFR (with a bias ranging between 0.03 and 0.05) (16,18). Second, among patients with FFRCT values less than or equal to 0.80, there is a graded correlation between FFRCT and invasive FFR, with the highest FFRCT uncertainty in the range between 0.76 and 0.80 and the highest agreement when FFRCT is less than or equal to 0.75 (12,18). Third, FFRCT, similar to FFR, exhibits a continuous relationship between its numerical value and clinical outcomes, with the worst outcome at lower FFRCT values (14,22,23). Finally, symptomatic patients with moderate CAD determined at CT angiography and FFRCT values greater than 0.80 and in whom invasive angiography is deferred have a favorable prognosis (12,14,22,23).
Figure 2:
FFRCT appropriateness and interpretation recommendation. * = Low risk: patients either without coronary disease or with maximum stenosis less than 30%. Intermediate risk: patients with one or more intermediate range stenosis (30%–69%). High risk: patients with left main, three-vessel disease or stenosis 70% or greater. Anatomic characteristics beyond stenosis severity, patient symptoms, and suitability of revascularization may influence decisions on management after coronary CT angiography (CTA). ** = Posttest risk stratification: Test results must always be evaluated in their clinical context, taking into account patient symptoms and preferences as well as high-risk anatomic features and likelihood of revascularization.
Clinical decision making in patients with FFRCT ranging between 0.76 and 0.80 is nuanced and may benefit from consideration of additional risk stratification information (Fig 2). Identifying patients at incrementally higher cardiovascular risk, who may benefit from an early coronary angiography approach, can be done by assessing several factors: high-risk plaque features (low attenuation, positive remodeling, napkin-ring sign) (26–28), plaque burden (27,28), stenosis location (proximal vs distal; main vessel vs side branch) (25,29,30), vessel territory (left anterior descending artery [LAD] vs non-LAD) (29), ratio of coronary vessel volume to myocardial mass (31), and/or the translesional FFRCT gradient (ΔFFRCT) (32). It is the opinion of the present author group that in certain instances with FFRCT values less than or equal to 0.75 (eg, small vessels, distal lesions, side branches), patients may be treated with optimal medical therapy without referral to invasive angiography as a first-line strategy (14,33).
In a recent retrospective study, a large pressure drop (ΔFFRCT ≥ 0.06) was a stronger predictor of culprit lesions for future acute coronary syndromes than FFRCT measured distal to the lesion alone (32). Ongoing studies are assessing the potential diagnostic value of ΔFFRCT in clinical practice. Overall, the results of FFRCT, as for invasive FFR, must always be evaluated in their clinical context, taking into account patient symptoms and comorbid conditions, which inform the goals of coronary intervention, in combination with the coronary anatomy and suitability of revascularization.
Standardized Interpretation of Hemodynamically Significant Lesions
In patients with CAD, as for measured FFR, FFRCT values decline from the ostium to the distal vessel irrespective of the vessel territory, stenosis severity, and location (14,19,34–36). In FFR practice, it is advised that the FFR value within the throat of the lesion (which may correspond to the minimum FFRCT value) is not used clinically and that the pressure is assessed at least 2–3 cm distal to the stenosis of interest (20). Likewise, for clinical decision making, we recommend using the FFRCT value distal to the lesion. With the interactive three-dimensional coronary model tool (HeartFlow), it is possible to obtain multiple values across the vessel. Hence, after localizing the stenosis, the vessel should be serially interrogated downstream from the lesion. Notably, the FFRCT value may transiently rise immediately after the stenosis because of poststenotic vessel dilatation, resulting in reduced flow velocity and pressure recovery (Fig 3). In a recent study, it was suggested that a reliable location at which to assess FFRCT was 1 cm distal to the end of a stenosis (36). For clinical decision making, we recommend using the FFRCT value 1–2 cm distal to the lower border of the stenosis, avoiding the pressure recovery phenomenon.
Figure 3:
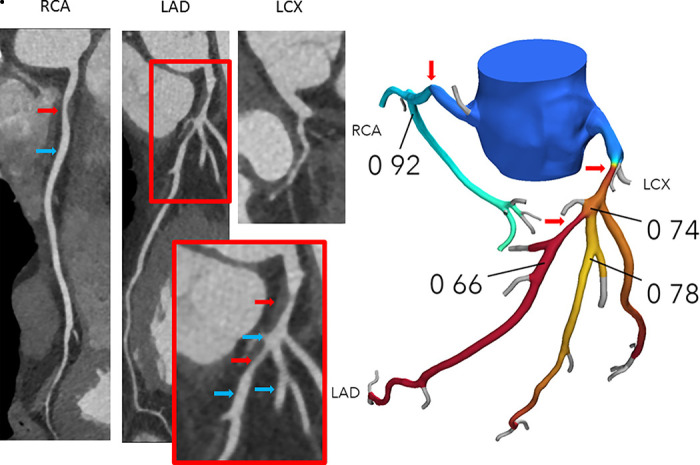
FFRCT assessment in vessels with serial lesions in a 53-year-old man with typical angina. Agatston score, 0. Left: Coronary CT angiography curved multiplanar reconstructions demonstrate a proximal 60% right coronary artery (RCA) stenosis (red arrow) and two serial stenoses in the left anterior descending artery (LAD) (one lesion in the proximal segment with 70% or greater diameter stenosis, and a 50%–69% diameter stenosis lesion distal to the takeoff of the second diagonal [red arrows]). Blue arrows indicate where the FFRCT values were assessed. Right: In the FFRCT three-dimensional model, the FFRCT value 10 mm distal to the proximal LAD stenosis was 0.74 and thus had hemodynamic significance, whereas FFRCT 15 mm distal to the second LAD stenosis was 0.66. FFRCT 10 mm distal to the lower border of the proximal RCA stenosis was 0.92, thus this lesion had low likelihood of being hemodynamically significant. Of note, pressure recovery was observed in the proximal part of the second diagonal with a step-up in FFRCT from 0.74 in the LAD to 0.78 when moving downstream the diagonal branch. LCX = left circumflex coronary artery.
Distal Vessel FFRCT Values
FFRCT provides simultaneous computation of pressure and flow in the entire coronary tree, thus exposing both lesion-specific pressure as well as nadir FFRCT values across the coronary system, which in various settings may drop less than or equal to 0.80 (14,19,34–36) (Fig 1). Low terminal vessel FFRCT values (rather than a value distal to stenosis) may include effects unrelated to the stenosis (19,35–37). These low values remote from a focal lesion may be due to diffuse CAD or reflect the sum of serial flow-limiting lesions (35–37). In recent studies, 35%–44% of patients with stable CAD and terminal vessel FFRCT values less than or equal to 0.80 were reclassified as negative when the FFRCT point of reading was 1–2 cm distal to stenosis (14,35). In one observational single-center study, the intermediate follow-up clinical outcome was favorable in patients with terminal FFRCT values less than or equal to 0.80 who were treated with optimal medical treatment (14). In vessels without a significant pressure loss within 2 cm distal to the lesion of interest, but with FFRCT values less than or equal to 0.80 in nearby (eg, mid coronary) segments, we recommend assessment for extent of upstream disease including both CT angiography and FFRCT. FFRCT values less than or equal to 0.80 in such circumstances may be clinically relevant (especially when present distal to a lesion in a proximal segment supplying a large myocardial territory). The group recognizes that more research is needed, particularly in large vessels that have discordance between lesion-specific FFRCT and values taken 2 cm beyond an upstream lesion.
Serial Lesions
The individual contribution of a given lesion in the event of serial stenosis cannot be assessed with FFRCT, similar to measured FFR, in any straightforward way because of the complex physiologic interplay between stenoses (Fig 3). At present, there is no accepted way to identify the lesion that contributes most to this cumulative pressure loss. Intuitively, the intrinsic impact of a given lesion should relate to ΔFFRCT of that individual lesion, and previous data have in fact demonstrated excellent correlation between ΔFFRCT and invasive ΔFFR (38). However, in a recent study, it was demonstrated that ΔFFRCT (as well as ΔFFR) may underestimate the physiologic contribution of stenosis in vessels with serial lesions (39). An interactive revascularization FFRCT-based planner tool (HeartFlow) may more accurately predict the invasive FFR contribution of each stenosis in serial CAD (39). The ongoing Precise Percutaneous Coronary Intervention plan (P3) study (ClinicalTrials.gov: NCT03782688) investigates the diagnostic value of the FFRCT revascularization planner tool.
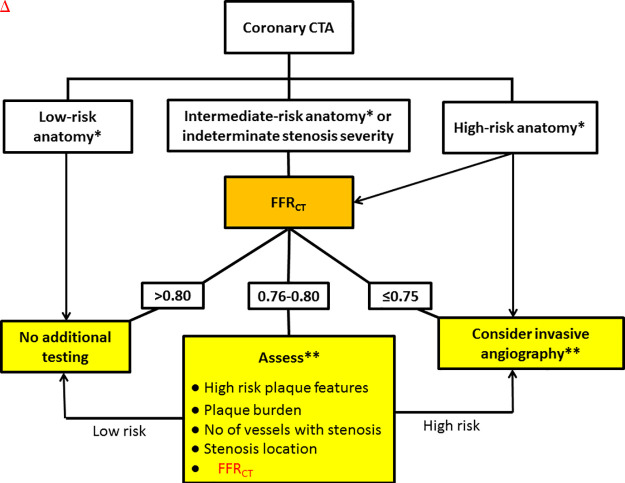
FFRCT Reporting
Coronary CT angiography and FFRCT uniquely provide simultaneous anatomic and functional information in a noninvasive fashion. To provide useful, actionable guidance for medical or invasive management, the FFRCT report must relate the observed anatomic coronary CT angiography findings with lesion-specific FFRCT values. The principal purpose of the report is to communicate these findings and their clinical implications (Fig 4).
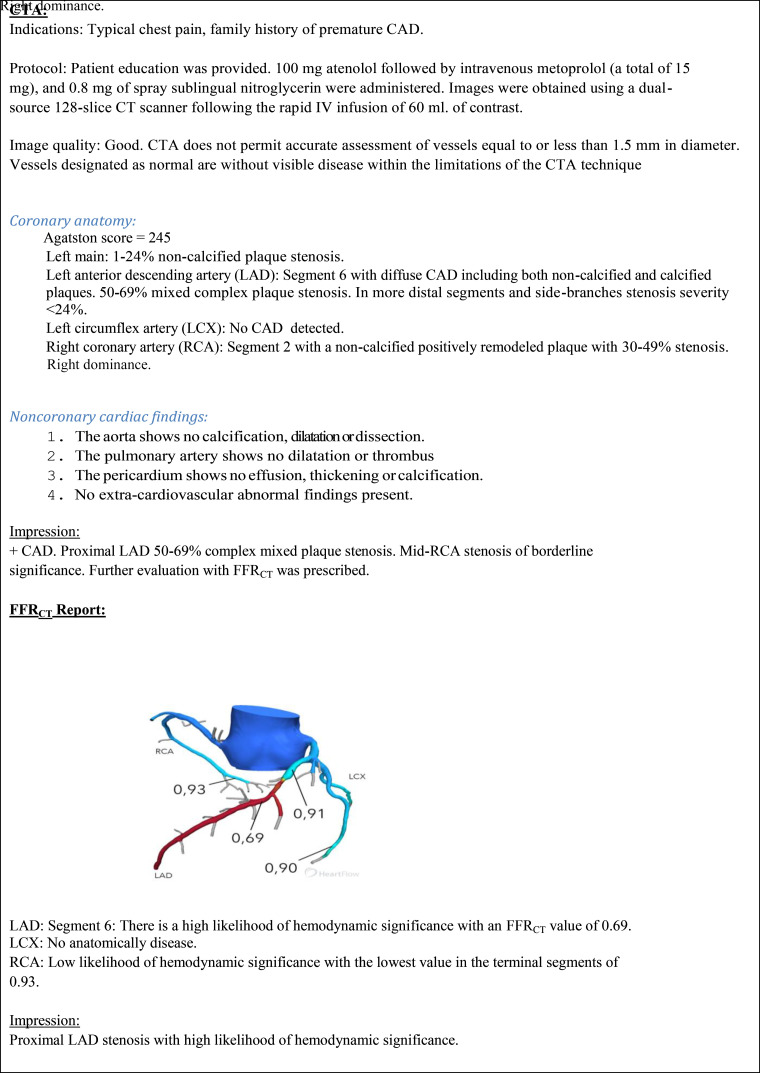
Figure 4:
Example of a coronary CT angiography–FFRCT report (patient case, Fig 1b). CAD = coronary artery disease, CTA = coronary CT angiography.
Indications
The indications for the FFRCT analysis should include clinical information from the original coronary CT angiography report, as well as specific anatomic details from the impression of the report that motivated the performance of FFRCT analysis. Mention should be made of factors pertinent to the FFRCT indication and suitability for analysis, such as angiographic degree of stenosis, extent of calcifications, and overall image quality (signal-to-noise ratio, motion artifacts, luminal contrast opacification). The indications should specify the anatomic lesions from the original coronary CT angiography report that were of particular concern in ordering the FFRCT analysis. The present author group finds FFRCT testing appropriate in patients with intermediate anatomic stenosis. FFRCT values may be less than or equal to 0.80 in lesions of less than 50% diameter stenosis. Physiologic characterization with FFRCT may be relevant in a small proportion of such lesions when located in proximal coronary segments supplying a large myocardial territory because they may have prognostic implications (40). On the other hand, even high-grade anatomic lesions with stenosis severity greater than 70% or even greater than 90%, which are generally considered flow limiting, may overestimate the physiologic significance (41,42). Therefore, we commonly use FFRCT testing in the setting of more severe anatomic disease and multivessel disease to help guide decision making on downstream catheterization and potential revascularization planning (Fig 2). As with any test, the appropriateness is often determined on a case-by-case basis and commonly related to many factors beyond stenosis severity (Fig 2). Finally, because the impact of coronary occlusion on the diagnostic performance of FFRCT is unknown, we do not recommend FFRCT analysis to be prescribed in such circumstances.
Results
We recommend FFRCT values to be reported for each major coronary branch by specific coronary segments (diameter greater than 1.8 mm) using the standardized SCCT guidelines for coronary segmentation classification (21), and that the values be related to specific lesions within a given segment.
Any lesion identified in the original coronary CT angiography report as a potential source of pressure loss should be specifically reported in the FFRCT report and its standard SCCT coronary segment identified. A given FFRCT value may have different therapeutic implications if located in a proximal segment as opposed to either a distal location or within a minor side branch (25,29,30). If no FFRCT value of 0.80 or less was reported in a given artery territory, we recommend the lowest value for that territory be reported. It is not necessary to provide FFRCT values greater than 0.80 for minimal (1%–24% stenosis) or mild (25%–49%) lesions unless located in the left main or proximal LAD or when containing high-risk plaque features, in which case FFRCT values should be provided. Any lesion with an abnormal FFRCT value should be reported even if not considered as a likely source of significant pressure loss in the original coronary CT angiography report. We recommend that an FFRCT value be provided for all moderate (50%–69%) and all severe (>70% to 99%) stenoses.
FFRCT values 0.80 or lower that are measured more than 2 cm beyond a lesion not causing a significant focal pressure loss (FFRCT > 0.80) should be reported when present in large vessels. The clinical significance of FFRCT values 0.80 or lower in the distal coronary tree remote from any focal lesion is unknown. These may be reported; however, it should be stated that the values are remote from angiographic stenosis and are of uncertain clinical significance.
In the event of serial lesions, we recommend that the value of FFRCT 10–20 mm distal to each lesion should be reported. If this is not possible, FFRCT values between lesions should be reported, including information on the distance between stenosis and the FFRCT value.
Occlusion of small vessels that were overlooked in the primary CT angiography assessment (typically involving distal segments or small side branches) may be revealed by the FFRCT analysis process. While this may or may not be clinically relevant, an occluded branch may have some slight impact on FFRCT in the parent vessel. The impact will depend on the size of the branch relative to other vessels. Occluded segments should be identified and referenced.
In recognition of the fact that FFRCT is a mathematically derived analysis rather than an actual measurement of flow and pressure, it is recommended that results be described as demonstrating low, borderline, or high likelihood of hemodynamic significance rather than ischemia (Table).
Impression
The report summary should focus on the presence of a low, borderline, or high likelihood of hemodynamic significance of the lesions identified in the impression section of the original coronary CT angiography report. In addition, any other lesion that has a borderline or high likelihood of hemodynamic significance should be reported even if it was not identified in the original coronary CT angiography interpretation. In particular, areas of diffuse coronary disease that produce low FFRCT values distal to the affected segments should be described.
Format
It is recognized that institutional requirements may dictate the specific reporting format required. Ideally, the coronary CT angiography and FFRCT reports can be combined into a single uniform report that will most clearly relate anatomic and functional information. However, it is important to interrogate the anatomy to assess the extent and severity of CAD to determine the need for FFRCT analysis. Given the time gap between the coronary CT angiography and FFRCT results, either a preliminary CT angiography report may be finalized after the FFRCT results are available or an FFRCT report may subsequently be added to the original coronary CT angiography report. Both of these formats closely incorporate the most detailed description of anatomy and functional significance with minimal repetition. If institutions require a separate free-standing report, additional details in the indications should be provided to emphasize the severity, morphology, and location of lesions suspected of causing flow limitation.
FFRCT Images
It is recommended that relevant images from the FFRCT report should be included if technically possible to more accurately convey the location of FFRCT values at a specific anatomic location. This will help other physicians understand the location and extent of the pressure loss and the location for potential confirmatory invasive FFR measurement and will facilitate medical or invasive treatment planning. Providing images combining FFRCT values and their specific location can rapidly and succinctly convey the extent of pressure loss and facilitate therapeutic decision making more easily than if textual description was offered alone.
Management Recommendations
The decision of whether FFRCT interpretation reports should contain management recommendations (ie, consideration for invasive coronary angiography or optimal medical therapy alone) will be determined by local institutional practices. If management recommendations are typically included in reports, note should be made that FFRCT values should not be considered in isolation but are integrated with clinical and other imaging factors such as symptoms, plaque morphology, and lesion location. This is particularly important in cases of borderline FFRCT values between 0.76 and 0.80 (Fig 2).
Limitations
The diagnostic performance and utility of FFRCT has been studied only in patients suspected of having stable CAD. At present, the use of FFRCT in patients with stents or bypass grafts, microvascular dysfunction, prior myocardial infarction, or suspected or known acute coronary syndromes cannot be recommended. FFRCT analysis cannot be performed in all patients. Coronary CT angiography–related artifacts, such as motion, misalignment, low contrast, or blooming from coronary calcification, may impair the diagnostic reliability of CT angiography and FFRCT (43–45). It is our experience that FFRCT has high diagnostic performance in patients with coronary calcification. However, our experience with FFRCT testing in patients with severe calcification (Agatston score > 1000) is limited, and in two previous studies demonstrating high diagnostic performance of FFRCT in vessels and patients with high calcium scores, the number of such patients were low (44,45). In previous multicenter studies of FFRCT diagnostic performance, CT angiographic images were not of sufficient quality for FFRCT analysis in 11%–13% of patients (15,16), whereas in more recent single-center studies that assessed the clinical utility of FFRCT, less than 4% of the patients did not meet the image quality requirements (10–12,14).
Conclusion
By virtue of the complexity of the FFRCT analysis providing information on pressure and flow across the entire coronary tree, standardized criteria on interpretation and reporting of the FFRCT analysis results are of crucial importance both in context of clinical adoption of the test and in future research. For assessment of the hemodynamic significance of lesions, we recommend using the FFRCT value 10–20 mm distal to the lower border of the stenosis. For clinical decision making, we recommend a dichotomous interpretation strategy be considered only in lesions with FFRCT greater than 0.80 or less than or equal to 0.75, whereas in patients with FFRCT ranging between 0.76 and 0.80, additional risk stratification information is needed. The results of FFRCT must always be evaluated in their clinical context, taking into account patient symptoms, the coronary anatomy, and suitability of revascularization.
Disclosures of Conflicts of Interest: B.L.N. Activities related to the present article: disclosed no relevant relationships. Activities not related to the present article: has received unrestricted institutional research grants from Siemens and HeartFlow; travel expenses covered at TCT 2017 by HeartFlow (no personal payment). Other relationships: disclosed no relevant relationships. T.A.F. Activities related to the present article: disclosed no relevant relationships. Activities not related to the present article: has been an invited speaker sponsored by HeartFlow. Other relationships: disclosed no relevant relationships. R.D.S. disclosed no relevant relationships. M.G.R. Activities related to the present article: disclosed no relevant relationships. Activities not related to the present article: author is consultant for HeartFlow. Other relationships: disclosed no relevant relationships. B.K. Activities related to the present article: has been an invited speaker at symposiums sponsored by Canon Medical, Medtronic, and St Jude, and has received research funding from Canon Medical. Activities not related to the present article: disclosed no relevant relationships. Other relationships: disclosed no relevant relationships. J.M.J. disclosed no relevant relationships. K.N. Activities related to the present article: disclosed no relevant relationships. Activities not related to the present article: unrestricted institutional research support from HeartFlow, Siemens, GE, and Bayer; coverage of travel expenses to the present study results at the TCT in 2018 by HeartFlow; Steering committee ADVANCE registry for HeartFlow (unpaid). Other relationships: disclosed no relevant relationships. K.M.C. Activities related to the present article: institution receives grant from HeartFlow. Activities not related to the present article: Medical Advisory Board for HeartFlow (no personal compensation); institution receives grants from HeartFlow. Other relationships: disclosed no relevant relationships. N.P.S. disclosed no relevant relationships. H.M. disclosed no relevant relationships. J.L. Activities related to the present article: disclosed no relevant relationships. Activities not related to the present article: has received speaker honoraria from GE Healthcare, served as a consultant for Edwards Lifesciences, and served as a consultant and has stock options in Circle CVI and HeartFlow; has core laboratory contracts with Edwards Lifesciences, Medtronic, Abbott, Noevasc; research support from Edwards. Other relationships: disclosed no relevant relationships. G.R. disclosed no relevant relationships.
Abbreviations:
- CAD
- coronary artery disease
- FFR
- fractional flow reserve
- FFRCT
- CT angiography–derived FFR
- LAD
- left anterior descending artery
- SCCT
- Society of Cardiovascular Computed Tomography
References
- 1.Koo BK, Erglis A, Doh JH, et al. Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve computed from coronary computed tomographic angiograms. Results from the prospective multicenter DISCOVER-FLOW (Diagnosis of Ischemia-Causing Stenoses Obtained Via Noninvasive Fractional Flow Reserve) study. J Am Coll Cardiol 2011;58(19):1989–1997. [DOI] [PubMed] [Google Scholar]
- 2.Coenen A, Lubbers MM, Kurata A, et al. Fractional flow reserve computed from noninvasive CT angiography data: diagnostic performance of an on-site clinician-operated computational fluid dynamics algorithm. Radiology 2015;274(3):674–683. [DOI] [PubMed] [Google Scholar]
- 3.Ko BS, Cameron JD, Munnur RK, et al. Noninvasive CT-derived FFR based on structural and fluid analysis: a comparison with invasive FFR for detection of functionally significant stenosis. JACC Cardiovasc Imaging 2017;10(6):663–673. [DOI] [PubMed] [Google Scholar]
- 4.U.S. Food and Drug Administration. 510(k) Premarket Notification. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpmn/pmn.cfm. Accessed November 12, 2019.
- 5.National Institute for Health and Care Excellence. Chest pain of recent onset: assessment and diagnosis of recent onset chest pain or discomfort of suspected cardiac origin. Clinical guideline CG95. London: NICE, 2016. https://www.nice.org.uk/guidance/CG95. Accessed November 12, 2019. [PubMed]
- 6.Zarins CK, Taylor CA, Min JK. Computed fractional flow reserve (FFTCT) derived from coronary CT angiography. J Cardiovasc Transl Res 2013;6(5):708–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Taylor CA, Fonte TA, Min JK. Computational fluid dynamics applied to cardiac computed tomography for noninvasive quantification of fractional flow reserve: scientific basis. J Am Coll Cardiol 2013;61(22):2233–2241. [DOI] [PubMed] [Google Scholar]
- 8.Min JK, Taylor CA, Achenbach S, et al. Noninvasive fractional flow reserve derived from coronary CT angiography: Clinical data and scientific principles. JACC Cardiovasc Imaging 2015;8(10):1209–1222. [DOI] [PubMed] [Google Scholar]
- 9.Douglas PS, Pontone G, Hlatky MA, et al. Clinical outcomes of fractional flow reserve by computed tomographic angiography-guided diagnostic strategies vs. usual care in patients with suspected coronary artery disease: the prospective longitudinal trial of FFR(CT): outcome and resource impacts study. Eur Heart J 2015;36(47):3359–3367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nørgaard BL, Gormsen LC, Bøtker HE, et al. Myocardial perfusion imaging versus computed tomography angiography-derived fractional flow reserve testing in stable patients with intermediate-range coronary lesions: influence on downstream diagnostic workflows and invasive angiography findings. J Am Heart Assoc 2017;6(8):e005587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jensen JM, Bøtker HE, Mathiassen ON, et al. Computed tomography derived fractional flow reserve testing in stable patients with typical angina pectoris: influence on downstream rate of invasive coronary angiography. Eur Heart J Cardiovasc Imaging 2018;19(4):405–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nørgaard BL, Hjort J, Gaur S, et al. Clinical use of coronary CTA-derived FFR for decision-making in stable CAD. JACC Cardiovasc Imaging 2017;10(5):541–550. [DOI] [PubMed] [Google Scholar]
- 13.Fairbairn TA, Nieman K, Akasaka T, et al. Real-world clinical utility and impact on clinical decision-making of coronary computed tomography angiography-derived fractional flow reserve: lessons from the ADVANCE Registry. Eur Heart J 2018;39(41):3701–3711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nørgaard BL, Terkelsen CJ, Mathiassen ON, et al. Coronary CT angiographic and flow reserve-guided management of patients with stable ischemic heart disease. J Am Coll Cardiol 2018;72(18):2123–2134. [DOI] [PubMed] [Google Scholar]
- 15.Min JK, Leipsic J, Pencina MJ, et al. Diagnostic accuracy of fractional flow reserve from anatomic CT angiography. JAMA 2012;308(12):1237–1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nørgaard BL, Leipsic J, Gaur S, et al. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: the NXT trial (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps). J Am Coll Cardiol 2014;63(12):1145–1155. [DOI] [PubMed] [Google Scholar]
- 17.Sand NPR, Veien KT, Nielsen SS, et al. Prospective comparison of FFR derived from coronary CT angiography with SPECT perfusion imaging in stable coronary artery disease: the ReASSESS study. JACC Cardiovasc Imaging 2018;11(11):1640–1650. [DOI] [PubMed] [Google Scholar]
- 18.Driessen RS, Danad I, Stuijfzand WJ, et al. Comparison of coronary computed tomography angiography, fractional flow reserve, and perfusion imaging for ischemia diagnosis. J Am Coll Cardiol 2019;73(2):161–173. [DOI] [PubMed] [Google Scholar]
- 19.Rabbat MG, Berman DS, Kern M, et al. Interpreting results of coronary computed tomography angiography-derived fractional flow reserve in clinical practice. J Cardiovasc Comput Tomogr 2017;11(5):383–388. [DOI] [PubMed] [Google Scholar]
- 20.Toth GG, Johnson NP, Jeremias A, et al. Standardization of Fractional Flow Reserve Measurements. J Am Coll Cardiol 2016;68(7):742–753. [DOI] [PubMed] [Google Scholar]
- 21.Leipsic J, Abbara S, Achenbach S, et al. SCCT guidelines for the interpretation and reporting of coronary CT angiography: a report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovasc Comput Tomogr 2014;8(5):342–358. [DOI] [PubMed] [Google Scholar]
- 22.Patel MR, Nørgaard BL, Fairbairn TA, et al. 1-Year Impact on Medical Practice and Clinical Outcomes of FFRCT: The ADVANCE Registry. JACC Cardiovasc Imaging 2019 Mar 17 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 23.Ihdayhid AR, Norgaard BL, Gaur S, et al. Prognostic value and risk continuum of noninvasive fractional flow reserve derived from coronary CT angiography. Radiology 2019;292(2):343–351. [DOI] [PubMed] [Google Scholar]
- 24.Johnson NP, Tóth GG, Lai D, et al. Prognostic value of fractional flow reserve: linking physiologic severity to clinical outcomes. J Am Coll Cardiol 2014;64(16):1641–1654. [DOI] [PubMed] [Google Scholar]
- 25.Adjedj J, De Bruyne B, Floré V, et al. Significance of intermediate values of fractional flow reserve in patients with coronary artery disease. Circulation 2016;133(5):502–508. [DOI] [PubMed] [Google Scholar]
- 26.Motoyama S, Ito H, Sarai M, et al. Plaque characterization by coronary computed tomography angiography and the likelihood of acute coronary events in mid-term follow-up. J Am Coll Cardiol 2015;66(4):337–346. [DOI] [PubMed] [Google Scholar]
- 27.Park HB, Heo R, Ó Hartaigh B, et al. Atherosclerotic plaque characteristics by CT angiography identify coronary lesions that cause ischemia: a direct comparison to fractional flow reserve. JACC Cardiovasc Imaging 2015;8(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gaur S, Øvrehus KA, Dey D, et al. Coronary plaque quantification and fractional flow reserve by coronary computed tomography angiography identify ischaemia-causing lesions. Eur Heart J 2016;37(15):1220–1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kim HY, Lim HS, Doh JH, et al. Physiological severity of coronary artery stenosis depends on the amount of myocardial mass subtended by the coronary artery. JACC Cardiovasc Interv 2016;9(15):1548–1560. [DOI] [PubMed] [Google Scholar]
- 30.Kim HY, Doh JH, Lim HS, et al. Identification of coronary artery side branch supplying myocardial mass that may benefit from revascularization. JACC Cardiovasc Interv 2017;10(6):571–581. [DOI] [PubMed] [Google Scholar]
- 31.Taylor CA, Gaur S, Leipsic J, et al. Effect of the ratio of coronary arterial lumen volume to left ventricle myocardial mass derived from coronary CT angiography on fractional flow reserve. J Cardiovasc Comput Tomogr 2017;11(6):429–436. [DOI] [PubMed] [Google Scholar]
- 32.Lee JM, Choi G, Koo BK, et al. Identification of high-risk plaques destined to cause acute coronary syndrome using coronary computed tomographic angiography and computational fluid dynamics. JACC Cardiovasc Imaging 2019;12(6):1032–1043. [DOI] [PubMed] [Google Scholar]
- 33.Nørgaard BL, Jensen JM, Blanke P, Sand NP, Rabbat M, Leipsic J. Coronary CT angiography derived fractional flow reserve: the game changer in noninvasive testing. Curr Cardiol Rep 2017;19(11):112. [DOI] [PubMed] [Google Scholar]
- 34.Takagi H, Ishikawa Y, Orii M, et al. Optimized interpretation of fractional flow reserve derived from computed tomography: Comparison of three interpretation methods. J Cardiovasc Comput Tomogr 2019;13(2):134–141. [DOI] [PubMed] [Google Scholar]
- 35.Kueh SH, Mooney J, Ohana M, et al. Fractional flow reserve derived from coronary computed tomography angiography reclassification rate using value distal to lesion compared to lowest value. J Cardiovasc Comput Tomogr 2017;11(6):462–467. [DOI] [PubMed] [Google Scholar]
- 36.Cami E, Tagami T, Raff G, et al. Assessment of lesion-specific ischemia using fractional flow reserve (FFR) profiles derived from coronary computed tomography angiography (FFRCT) and invasive pressure measurements (FFRINV): importance of the site of measurement and implications for patient referral for invasive coronary angiography and percutaneous coronary intervention. J Cardiovasc Comput Tomogr 2018;12(6):480–492. [DOI] [PubMed] [Google Scholar]
- 37.De Bruyne B, Hersbach F, Pijls NH, et al. Abnormal epicardial coronary resistance in patients with diffuse atherosclerosis but “Normal” coronary angiography. Circulation 2001;104(20):2401–2406. [DOI] [PubMed] [Google Scholar]
- 38.Tanaka K, Bezerra HG, Gaur S, et al. Comparison between non-invasive (coronary computed tomography angiography derived) and invasive-fractional flow reserve in patients with serial stenoses within one coronary artery: a NXT Trial substudy. Ann Biomed Eng 2016;44(2):580–589. [DOI] [PubMed] [Google Scholar]
- 39.Modi BN, Sankaran S, Kim HJ, et al. Predicting the physiological effect of revascularization in serially diseased coronary arteries. Circ Cardiovasc Interv 2019;12(2):e007577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Toth G, Hamilos M, Pyxaras S, et al. Evolving concepts of angiogram: fractional flow reserve discordances in 4000 coronary stenoses. Eur Heart J 2014;35(40):2831–2838. [DOI] [PubMed] [Google Scholar]
- 41.Layland J, Oldroyd KG, Curzen N, et al. Fractional flow reserve vs. angiography in guiding management to optimize outcomes in non-ST-segment elevation myocardial infarction: the British Heart Foundation FAMOUS-NSTEMI randomized trial. Eur Heart J 2015;36(2):100–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Curzen N, Rana O, Nicholas Z, et al. Does routine pressure wire assessment influence management strategy at coronary angiography for diagnosis of chest pain?: the RIPCORD study. Circ Cardiovasc Interv 2014;7(2):248–255. [DOI] [PubMed] [Google Scholar]
- 43.Leipsic J, Yang TH, Thompson A, et al. CT angiography (CTA) and diagnostic performance of noninvasive fractional flow reserve: results from the Determination of Fractional Flow Reserve by Anatomic CTA (DeFACTO) study. AJR Am J Roentgenol 2014;202(5):989–994. [DOI] [PubMed] [Google Scholar]
- 44.Min JK, Koo BK, Erglis A, et al. Effect of image quality on diagnostic accuracy of noninvasive fractional flow reserve: results from the prospective multicenter international DISCOVER-FLOW study. J Cardiovasc Comput Tomogr 2012;6(3):191–199. [DOI] [PubMed] [Google Scholar]
- 45.Nørgaard BL, Gaur S, Leipsic J, et al. Influence of coronary calcification on the diagnostic performance of CT angiography derived FFR in coronary artery disease: A substudy of the NXT trial. JACC Cardiovasc Imaging 2015;8(9):1045–1055. [DOI] [PubMed] [Google Scholar]