Abstract
Cardiovascular computed tomography (CCT) is a well-validated noninvasive imaging tool with an ever-expanding array of applications beyond the assessment of coronary artery disease. These include the evaluation of structural heart diseases, congenital heart diseases, peri-procedural electrophysiology applications, and the functional evaluation of ischemia. This breadth requires a robust and diverse training curriculum to ensure graduates of CCT training programs meet minimum competency standards for independent CCT interpretation. This statement from the Society of Cardiovascular Computed Tomography aims to supplement existing societal training guidelines by providing a curriculum and competency framework to inform the development of a comprehensive, integrated training experience for cardiology and radiology trainees in CCT.
This article is being published synchronously in Radiology: Cardiothoracic Imaging, Journal of Cardiovascular Computed Tomography, and JACC: Cardiovascular Imaging.
© 2020 Society of Cardiovascular Computed Tomography. Published by RSNA with permission.
Background and Scope
The field of cardiovascular computed tomography (CCT) has seen considerable growth over the past decade. Driven in large part by a growing body of evidence and significant advancements in scanner technology, societal guidelines internationally now strongly recommend CCT, as the preferred first-line test in patients without known coronary artery disease (1–3). The recently updated National Institute for Health and Care Excellence (NICE) guidelines in the United Kingdom (UK) recommend CCT as the preferred testing strategy for stable chest pain patients without known CAD, citing accuracy of diagnosis, as well as economic and prognostic advantages (4,5). One challenge facing this increased utilization of CCT in the UK is the need for more independent CCT practitioners and/or advanced practitioners capable of leading a CCT laboratory (6). In the US, data from recent clinical trials, and an increased emphasis on value based care are contributing to a similar shift toward increased utilization of CCT, and thus a similar need for a higher number of independent CCT readers (7–9). This is expected to drive a similar need for more independent and advanced CCT practitioners.
In addition to the evaluation of CAD, the role for CCT in the evaluation of structural cardiac disease continues to expand rapidly, is now a prerequisite imaging study for the optimal planning of transcatheter, surgical and congenital therapies, and is expected to further evolve in the future (10,11). The modern cardiology and radiology trainee pursuing CCT training should be comfortable with the scope and fundamentals of these various non-coronary applications. In the United States, societal training guidelines from the American College of Cardiology (ACC) and American College of Radiology (ACR) inform the case volume and clinical skills that are required to become accredited as an independent reader or as a laboratory director (12,13).
Internationally, several training statements incorporate CCT training. The 2014 Royal College of Radiologists/British Society of Cardiovascular Imaging document addresses the safe practice of CT coronary angiography (14). The European Association of Cardiovascular Imaging developed a CCT Core Syllabus in 2015 that gives a broad overview to educational topics that constitute competency for CCT practice (15). Recently, the Royal College of Radiology Clinical Radiology Specialty Training Curriculum 2020 has incorporated CCT training (16). The Society of Cardiovascular Computed Tomography (SCCT) published a statement in 2015 outlining a comprehensive curriculum for cardiology and radiology program directors to design an educational experience in the basic, foundational (level I) aspects of CCT (17). To complement these statements, there is a need to assist program directors in designing a comprehensive academic curriculum to address advanced level trainees capable of performing and interpreting complex studies, lead a research program, direct a CCT laboratory and/or train others in CCT.
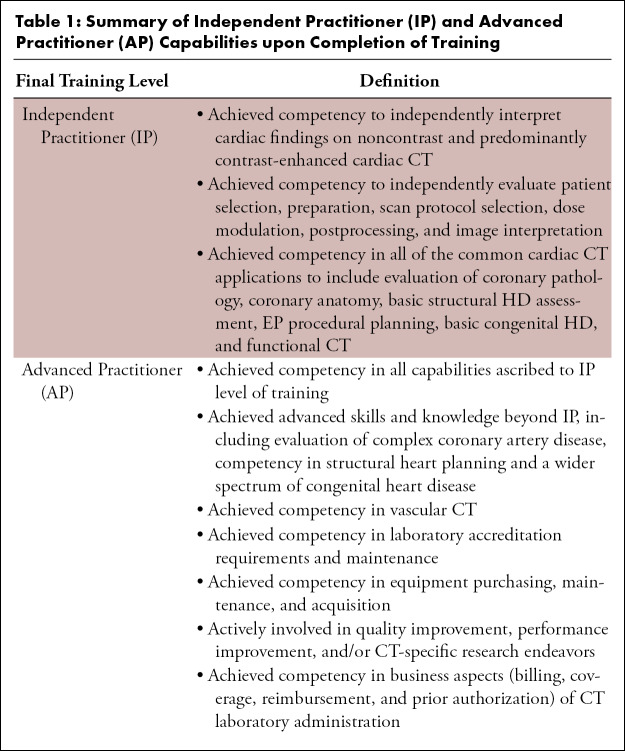
This document strives to provide guidance for program directors (PD) charged with designing a curriculum for the training of Independent Practitioner (IP; Level II) and/or Advanced Practitioner (AP; Level III) (Table 1). In the U.S., the Accreditation Council for Graduate Medical Education (ACGME) adopted a set of 6 core competencies that make up the cornerstone trainee education and assessment: 1) medical knowledge; 2) practice-based learning and improvement (PBLI); 3) patient care and procedural skills; 4) systems-based practice; 5) interpersonal and communication skills; and 6) professionalism.
Table 1:
Summary of Independent Practitioner (IP) and Advanced Practitioner (AP) Capabilities upon Completion of Training
Furthermore, this document uses the framework of the ACGME core competencies as a global document to enable the assessment and education of trainees across these core competencies to reproducibly train graduating fellows and residents fully qualified to care for patients utilizing CCT. Thus, this document aims to reinforce learning competencies utilized regularly in clinical practice through daily case volume. It also aims to provide a guide for necessary medical knowledge and online case volume supplementation needed to expose the trainee to less frequently encountered CCT applications.
CCT trainees emerge from two principle training backgrounds: radiology or cardiology. Importantly, it is not so much what specialty a prospective CCT reader originates from, but rather the quality of dedicated training that they obtain that ultimately defines competency level and expertise in the advanced field of CCT. Indeed, the strong collaboration between radiologists and cardiologists-in clinical practice, research, and in training-has fueled many of the advances in the field of CCT (18). The challenge for radiology and cardiology PDs is to identify training gaps in their respective curriculum and augment the training experience to incorporate all necessary learning objectives, regardless of local expertise, case diversity, or case volume.
Additionally, consideration should be given to tailoring a training curriculum based specifically on augmenting known knowledge gaps. Cardiology fellows, as an example, may require a training curriculum weighted more heavily in CT physics, protocol optimization, and extra-cardiac anatomy, and pathology. Conversely, radiology residents may benefit from a training curriculum focused more on cardiac anatomy, clinical outcomes data, clinical practice guidelines, management of cardiovascular disease, and cardiac pathophysiology. Figure 1 outlines potential CCT training pathways for both cardiology fellows and radiology residents. Given local variations in case volume, diversity, and supervisor expertise, training duration for IP/Level II trainees may vary.
Figure 1:
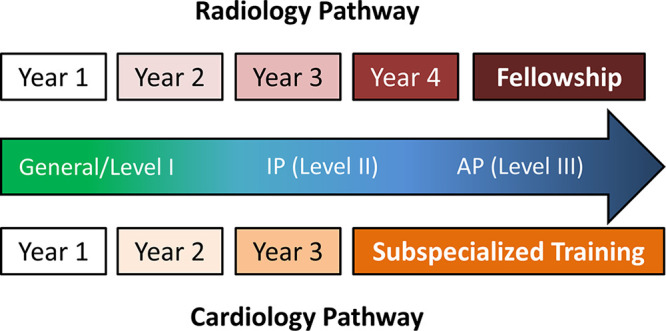
Recommended Pathways to Independent Practitioner & Advanced Practitioner from Cardiology or Radiology Training Backgrounds Local variations in case volume, diversity, and supervisor expertise may allow for completion of IP case volume and requirements as early as the second year of cardiology fellowship. Less variability typically exists with respect to IP training for radiology residents. General curriculum requirements are completed during the first 3 years of training and IP requirements are accomplished during focused cardiac imaging training, typically during the fourth year of training. AP training requires additional fellowship training in advanced cardiac imaging.
Current Requirements for Radiology Trainees
Less variability typically exists with respect to IP training for radiology residents. General curriculum requirements are completed during the first 3 years of training and IP requirements are accomplished during focused cardiac imaging training, typically during the fourth year of training. For radiology and nuclear medicine residents, the American College of Radiology (ACR) released an update to CT accreditation program requirements in July 2015 (19). The ACR statement lays out minimum initial requirements with respect to CCT case volume, board certification and/or training, and additional education in cardiac structure and function in order to interpret and supervise CCT examinations.
More recently in 2016, a joint practice parameter collaboratively revised by ACR in concert with the North American Society of Cardiovascular Imaging (NASCI) and the Society of Pediatric Radiology (SPR) was published that differs slightly from the 2015 ACR statement (13). The joint 2016 practice parameter lowered the number of dedicated cardiac CT examinations performed to 50 studies over a 36 month period (compared with 75 in the 2015 ACR CT accreditation requirements statement) while also lowering the required continuing medical education (CME) hours to 30 (from 40 hours); while maintaining board certification and training program accreditation standards established in the 2015 ACR statement. Importantly, the 2016 joint practice parameter also outlined qualifications required to assume responsibility of a cardiac CT imaging program or laboratory. In addition to the previously discussed requirements, an additional 450 supervised thoracic CT or CT angiography cases, excluding CAC scoring, are required and an additional 200 hours of CT-specific CME.
Nuclear medicine training is much more variable as trainees can emerge from both internal medicine and radiology. Thus, these trainees should follow guidance found in the ACR statement (19). In brief, radiology trainees are required to successfully complete board certification through a recognized governing body (ie, American Board of Radiology, Royal College of Physicians and Surgeons of Canada, etc). Importantly, no distinction is made between IP and AP levels of competency.
Current Requirements for Cardiology Trainees
Independent Practitioner (Level II).—Cardiology fellows training at high volume centers may complete IP case volume requirements within a shorter period of time when compared with cardiology fellows at lower volume centers. CCT training may be incorporated into multimodality imaging rotations to complete IP requirements. Adding to the variability is the fact that general cardiology fellowship training can vary in duration (as short as 24 months of clinical rotations up to 36 months), thus potentially shortening the time available to train IP-level trainees (20). While the 2015 ACR statement mentions training recommendations for IPs originating from a cardiology background, training requirements for various levels of competency for cardiology fellows are governed by the Core Cardiovascular Training Statement (COCATS) published by the American College of Cardiology (12). COCATS 4 provides a case-volume recommendations, in addition to general ACGME core competency-based training objectives (“milestones”) for both Level I and Level II general cardiology fellows (12). Training requirements highlighted in COCATS 4 call for significant hands-on time spent with contrast-enhanced CCT dataset acquisition and patient preparation with a focus on mentored case review at a 3-dimensional (3D) workstation. In general, level I concepts should be met within the first 2 years of fellowship training with more focused case exposure and didactic training required in the 3 year of training to achieve Level II competency during a standard general cardiology fellowship.
Advanced Practitioner (Level III).—AP learners requires additional training in hybrid imaging modalities, participation in the various aspects of laboratory administration, education of cardiology and/or radiology trainees, and participation in CCT-specific research. In addition to devoted training in CCT, an AP trainee is required to achieve advanced training in at least 1 additional imaging modality. Given these extensive requirements, COCATS recommends additional training beyond the standard 3-year fellowship, though this is not explicitly required. In the U.S. multiple cardiovascular imaging fellowships are available that enable trainees to acquired advanced knowledge and skills that enable trainees to achieve level II or level III in multiple imaging modalities. Around the world CCT is an important component of standard cardiology curriculum. For example in the UK, the Joint Royal Colleges of Physicians Training Board incorporates CCT in its specialty training curriculum for cardiology trainees (21). In addition, the length of cardiology training varies widely, and additional training in CCT may be required to achieve AP level.
Statement of Purpose
Taking this background into account, the purpose of this statement is threefold. First, we seek to expand upon the SCCT general (Level I) curriculum guideline statement by providing knowledge and skills required for IP and AP trainees. Second, we seek to provide enhanced granularity and standardization across advanced imaging fellowship curricula and across a broad range of training backgrounds (radiology and cardiology). Finally, we seek to fill in identified gaps in currently published training recommendation statements and emphasize that background knowledge and procedural skill are important requirements delineated in the COCATS and ACR statements. Specifically, this document delineates a suggested minimum threshold for AP case volumes to achieve the milestones outlined. This guideline is not meant to supersede the existing COCATS and ACR statements, but rather complement those documents to encompass the most recent advancements in the field of CCT.
Training Components
Identification of General Training Gaps
As this document builds upon the curriculum previously outlined in the 2015 SCCT Level I curriculum guideline (17), a comprehensive training curriculum with a goal of producing competent IP and AP imagers should be tailored to the specific strengths and limitations of training background (cardiology, radiology, or nuclear medicine), total laboratory case volume, and case diversity. Building an initial curriculum or revamping an existing curriculum for IP and AP trainees is a complex undertaking. Radiology residents/trainees may have a stronger foundation in CT scanner strengths, limitations, protocol selection, postprocessing, and image manipulation. Cardiology fellows/trainees may have a deeper understanding of cardiac anatomy, physiology, pathologic disease states, and the clinical applicability of these various findings, but minimal exposure to CT as an imaging modality. A team-based approach to the hands-on scanner training experience, which could involve technologist, medical physics, and the laboratory director, could also increase the level of understanding and depth of knowledge. In addition, AP trainees may require exposure to multiple scanner platforms and to a diverse case volume that should involve multidisciplinary image interpretation and clinical correlation of findings.
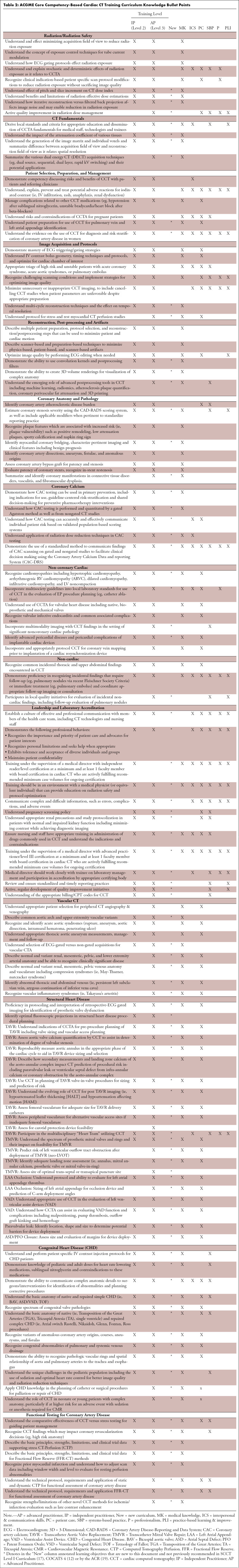
Understanding that a critical review and potential revision of a CCT training curriculum can be time consuming, this document seeks to ease this transition in several ways. First, recommended learning objectives are found in Table 2 and are arranged by ACGME core competency and further broken down by core CCT domain for both IP and AP trainees. The ACGME core competencies were used to allow for PDs to more easily develop trainee evaluations to ensure learners are meeting specific milestones and to identify knowledge gaps earlier in training where they can more easily be addressed.
Table 2:
ACGME Core Competency-Based Cardiac CT Training Curriculum Knowledge Bullet Points
Case Volume and Case Diversity
Case volume and diversity are important aspects for potential IP & AP trainees, as there is data linking increasing case volumes with successful completion of board certification examinations (22). Of greater importance, the case volumes discussed within this document serve as a starting point for competency that must be assessed and verified by CCT advanced practitioners. This can be learned and evaluated during live case manipulation at a dedicated 3D workstation. It is important that IP & AP trainees be directly mentored by a supervising faculty with routine involvement in image acquisition and protocol selection at the scanner. In many institutions, though, there is limited case volume and diversity that is reliably available for all trainees and thus alternative training resources are needed. Supplementation with electronic teaching files and/or online resources with emphasis on maximal exposure to 3D workstation functionality may assist with bridging this gap.
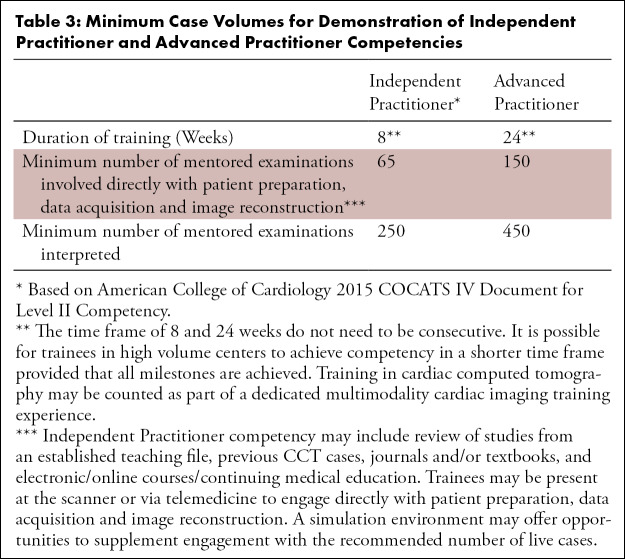
Integration and leveraging of expertise from cardiology and radiology resources within a training center can significantly augment an IP and AP training curriculum (18). PDs are strongly encouraged to coordinate with these other departments to arrange for multidisciplinary conferences, multimodality imaging correlations, and joint live interpretation at the 3D workstation. With regard to minimum case volumes for IP and AP competency (Tables 3–5), the writing group arrived at these recommendations through unanimous consensus.
Table 3:
Minimum Case Volumes for Demonstration of Independent Practitioner and Advanced Practitioner Competencies
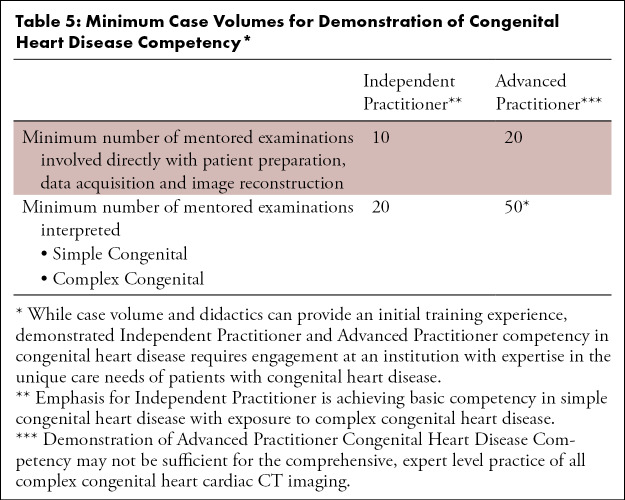
Table 5:
Minimum Case Volumes for Demonstration of Congenital Heart Disease Competency*
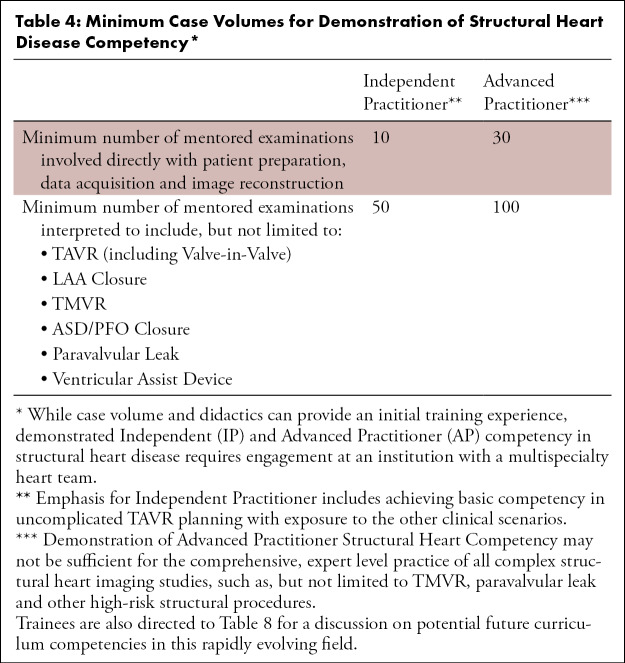
Table 4:
Minimum Case Volumes for Demonstration of Structural Heart Disease Competency*
Structural Heart Disease (SHD)
The widespread adoption of transcatheter aortic valve replacement (TAVR) has driven a strong interest in the field of structural heart disease. During the development of TAVR, CCT has become integral to the preprocedural planning of these procedures which has increased the need for competent IPs and APs with specific expertise and dedicated training in SHD (10,23–27). Furthermore, the role of CCT in newer technologies such as left atrial appendage (LAA) occlusion device implantation and the systematic evaluation of left ventricular assist devices (LVADs) continues to expand due to the distinct advantages from a spatial resolution perspective (28–31). Within the realm of transcatheter mitral valve replacement (TMVR), pre procedural CCT is a requirement in device selection, left ventricular outflow tract obstruction prediction risk, and intraprocedural fusion road mapping (27,32,33).
The application of CCT in structural heart disease is not significantly addressed in any prior societal training guidelines (26). However, it is important that all IP and AP trainees receive at least introductory exposure to this field with didactic content incorporating learning objectives from Table 2 including an understanding of vascular access. While case volume and didactics can provide an initial training experience to structural heart disease, more advanced training requires dedicated time with regular attendance at multi-specialty heart team conferences to fully understand the procedure, potential complications/pitfalls, and minimum equipment requirements as part of a 360-degree learning experience. Multi-specialty “heart team” conferences typically include an expert in CCT imaging, interventional cardiology, cardiothoracic (CT) surgery, interventional imagers, cardiac anesthesia, and other members of the cardiovascular team.
Congenital Heart Disease (CHD)
CCT provides detailed information on the anatomy of the entire thorax and, in contrast to other modalities, is superior for evaluating vascular/soft tissue structures in the setting of CHD (34). While true expertise in the nuances of congenital heart disease require specific training and time dedicated to this area, all IP and AP trainees should have a robust understanding of the distinct advantages/limitations of CCT, as well as other imaging technologies, as part of a multimodality approach to CHD. IP trainees, and more importantly AP trainees, should spend significant time with protocol development and image acquisition as part of the CHD curriculum as standardized coronary protocols may not adequately answer the clinical question (35,36). Additionally, a robust didactic curriculum utilizing learning objectives from Table 2 provide a needed knowledge foundation of simple and complex congenital lesions and repairs. It is strongly encouraged to further solidify these learning objectives in a multispecialty setting involving case review with adult CHD specialist or pediatric cardiologist, other noninvasive imaging specialists (particularly echocardiography and cardiac MR), and a congenital heart disease surgeon, when available. In addition to increasing medical knowledge and improving patient care among trainees, multispecialty learning opportunities teach effective communication skills among members of the CHD team.
Functional Testing of Ischemic Heart Disease
In addition to CCT’s ability to diagnose coronary atherosclerosis anatomically, there are emerging CCT applications that allow for functional assessment of ischemia, most notably CT perfusion (CTP) and CT-based fractional flow reserve (FFR-CT) (37). Ideally, a multidisciplinary heart team conference will leverage local expertise among CCT, nuclear cardiology, cardiac MR, echocardiography, and interventional cardiology to provide a valuable forum for open discussion on strengths, weaknesses, and appropriate use of the respective modalities (38). Table 2 outlines important learning objectives pertaining to functional assessment by CCT. In general, both IP and AP trainees should demonstrate understanding of the current clinical role, supporting data, techniques, strengths, and weaknesses of CT-based techniques for functional assessment of CAD lesions, and how these tests may compare with other imaging techniques. As many training centers may not have readily available access to specific functional CT techniques, including CTP or FFR-CT, hands-on experience during training is not required to meet competency objectives for IP or AP trainees.
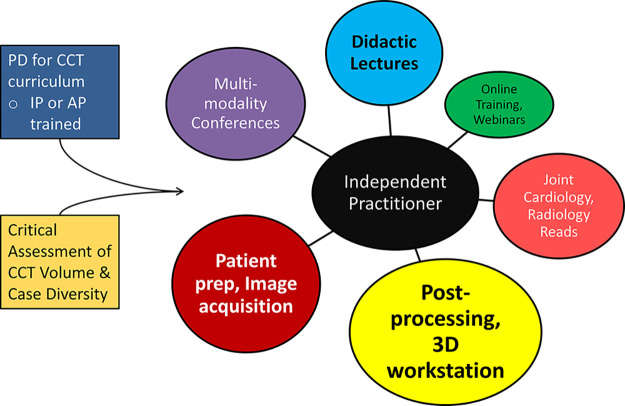
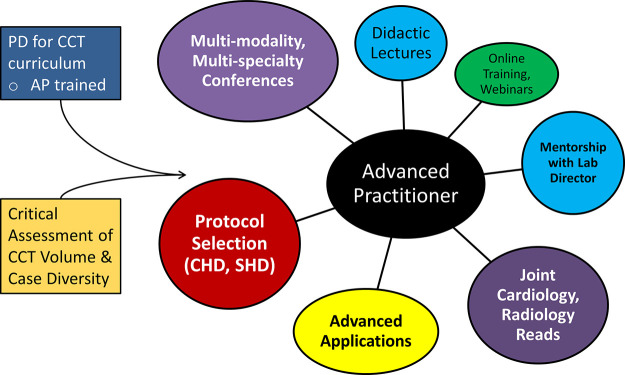
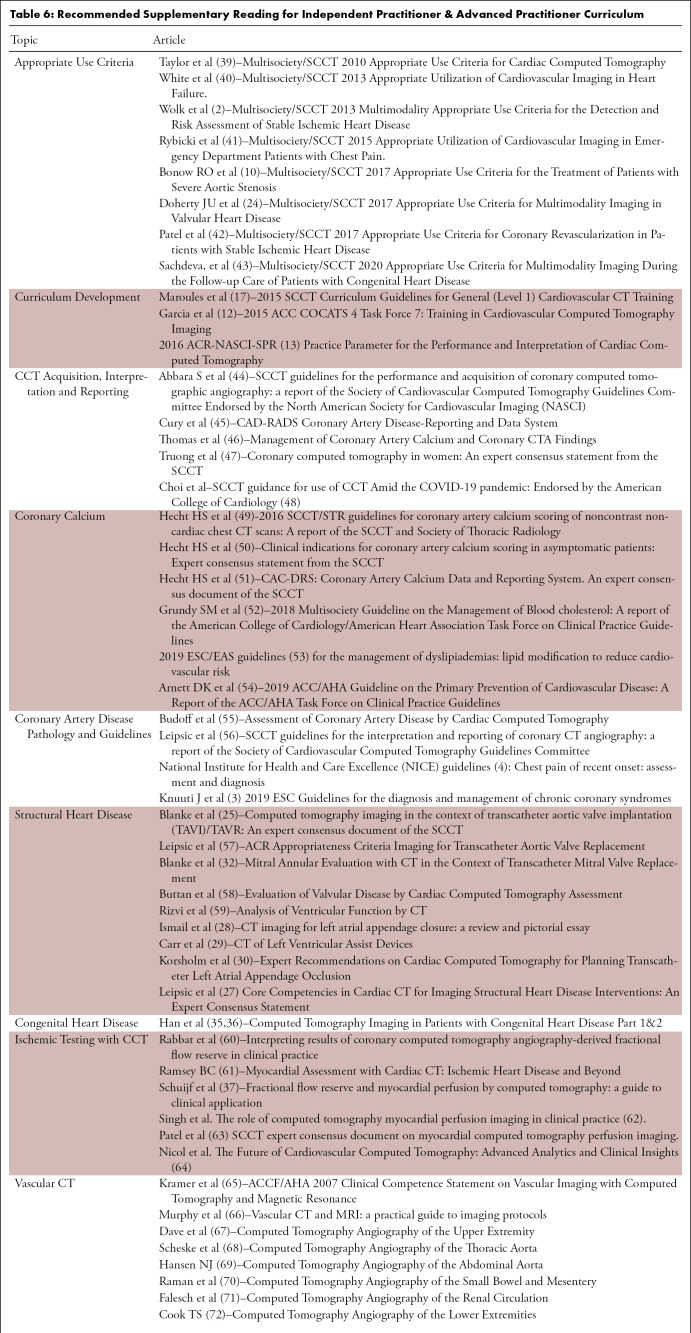
Didactic Curriculum
While a large proportion of the IP & AP training curriculum can be administered in conjunction with live case review, a full didactic curriculum is vital to supplement where gaps in training supervisor or case diversity exist. A didactic curriculum should incorporate multispecialty lectures from local experts complimented with webinars, societal educational offerings, and attendance at annual scientific meetings. Figures 2 and 3 highlight the comprehensive, multifaceted approach that is needed to meet the needs of an IP and AP learner in the current era of CCT. Table 6 lists supplemental reading of societal guidelines, appropriate use criteria and key articles germane to an understanding of CCT for IP and AP trainees. Online training, webinars and simulation environments may be a useful learning adjunct in lower volume or smaller programs to supplement lower volume centers and less common CCT applications.
Figure 2:
Comprehensive Independent Practitioner Training Curriculum in CCT The CCT PD must have attained IP status and critically evaluated individual institution case volume, case diversity, supervisor expertise, and trainee needs prior to curriculum planning. Key components of IP training are highlighted in various shading: postprocessing, 3D workstation image manipulation, patient preparation, image acquisition, and didactics. Online training and webinars may be needed to supplement local resources, particularly in low volume institutions.
Figure 3:
Comprehensive Advanced Practitioner Training Curriculum in CCT. AP training builds on IP skills, but pivots toward more complex applications of CCT and more complex cardiac disease. Integration of multidisciplinary resources into training by leveraging the advanced skills of both cardiology and radiology is needed. Direct trainee mentorship by the laboratory director or other AP supervisor is also imperative.
Table 6:
Recommended Supplementary Reading for Independent Practitioner & Advanced Practitioner Curriculum
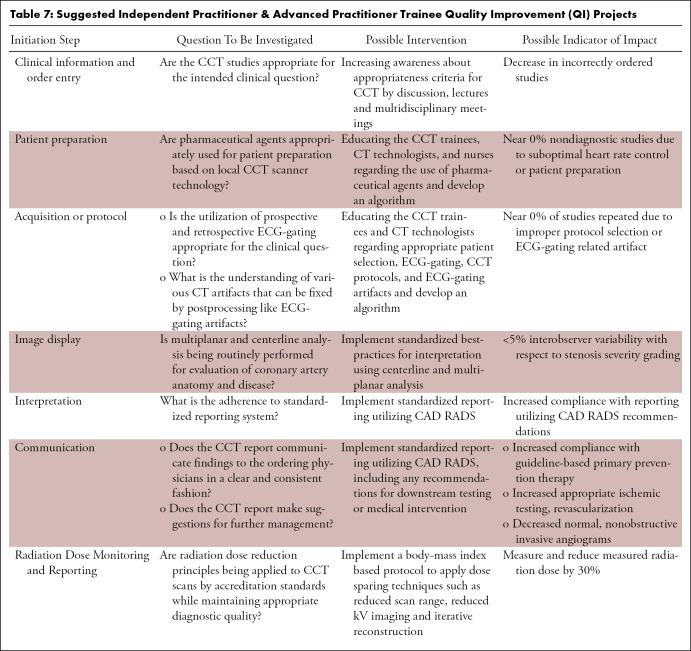
Advanced Practitioner Training
With respect to the AP trainee curriculum (Fig 3), the didactic training focus should pivot toward more complex applications of CCT and complex cardiac disease. Additionally, a broader focus on integrating into a multidisciplinary team and leveraging the advanced skills of both cardiology and radiology is needed. Finally, a comprehensive AP curriculum should involve direct mentorship by the laboratory director or other AP supervisors so that education in the business and administrative aspects of leading a CCT laboratory are incorporated. AP trainees, in addition to a comprehensive understanding of the learning objectives, require a curriculum incorporating mentorship opportunities with the laboratory director. This could include involvement with new equipment purchases, personnel management, protocol development, and performance improvement (PI)/quality assessment (QA). Particularly with the changing landscape of medical reimbursement and payer structures, a strong foundation in quality and appropriate use is vital to a future laboratory director or PD. Specific to the ACGME, requirements have been put in place for residencies and fellowships to actively participate in PI or QA projects as part of graduation requirements. Table 7 lists several recommendations for CCT-specific QA/PI projects.
Table 7:
Suggested Independent Practitioner & Advanced Practitioner Trainee Quality Improvement (QI) Projects
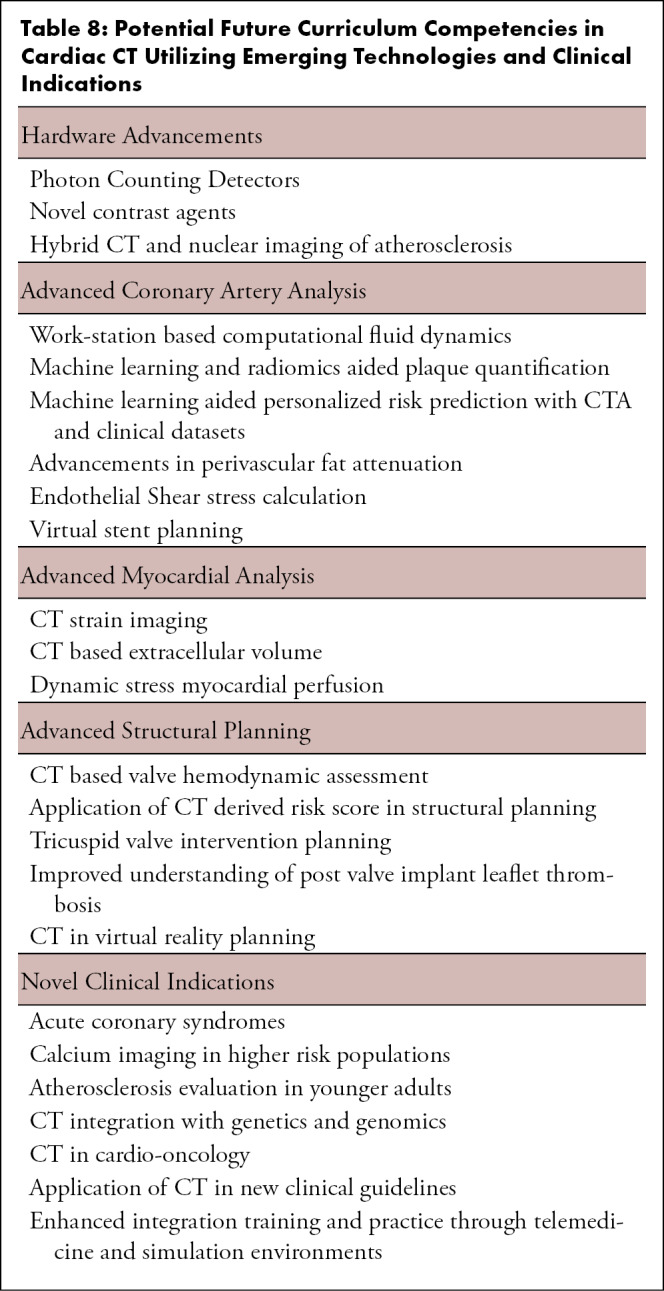
Summary
The rapid growth and expansion of CCT requires training programs to adopt a comprehensive training curriculum in order to meet the growing need for IP and AP that possess a minimum experience and core understanding of all aspects of CCT. As new technologies continue to emerge (Table 8) with sufficient evidence for efficacy and meaningful impact on clinical management, it is expected that the curricular needs of trainees will evolve. The core elements of this document are expected to remain foundational for IP and AP competency, while future updates to this training curriculum may be issued through both traditional and emerging digital publication formats. A curriculum based solely on case volume is insufficient to bridge the substantial knowledge gap, particularly among IP graduates given the diversity of training backgrounds, local volume, and supervisor expertise and so the recommended case volumes serve as a minimum floor to assess competency. To build from the 2015 SCCT Level I Curriculum Guideline, we encourage adoption of these training curriculum recommendations as a supplement to the current societal statements that include ACR, COCATS 4 and other global documents, to develop a training experience that produces a more uniform level of competence for both cardiology and radiology trainees. Additionally, better baseline training in CCT may promote more appropriate implementation of CCT into clinical practice after graduation and/or encourage more trainees to pursue advanced fellowships in CCT.
Table 8:
Potential Future Curriculum Competencies in Cardiac CT Utilizing Emerging Technologies and Clinical Indications
Footnotes
Guideline Co-Chairs
Relationships with Industry/Conflicts of Interest-Authors: Dr. Choi reports equity in Cleerly, Inc and grant support from the GW Heart and Vascular Institute. Dr. Abbara reports royalties for authoring/editing from Elsevier/Amirsys, research funding from CPRIT and stipends for editorial work from RSNA. Dr. Cury reports consultancy from Covera, equity in Cleerly and personal research funding from GE Healthcare. Dr. Leipsic reports consultancy from Heartflow and Circle CVI, serving on the Speakers Bureau of Philips and GE Healthcare, personal research funding from Edwards and GE Healthcare and institutional research support (Core Laboratory) from Edwards, Medtronic, Abbott, Pi Cardia and Boston Scientific. Dr. Maroules reports serving as co-founder and shareholder of Innovation Health Services/Cardioinnovations. Dr. Nagpal reports grant support from the National Institutes of Health. Dr. Steigner reports consultancy with Canon Medical (Vital Images). Dr. Wang reports consultancy with Edwards Life Sciences, Boston Scientific. She reports institutional research support from Boston Scientific (assigned to employer Henry Ford Health System) and LVOT prediction modeling software (assigned to employer Henry Ford Health System; patent). Dr. Blankstein reports research funding from Astellas Inc and Amgen Inc. Drs. Lee, Williams, Zeb, Thomas and Villines report no disclosures.
Relationships with Industry/Conflicts of Interest–Reviewers: Dr. Marcio Bittencourt reports being on the Speaker Bureau for General Electric. Dr. Sarah Cudde reports grant and research support from Pfizer. Dr. John Lesser and Dr. Armin Zadeh report no disclosures.
References
- 1.Al-Mallah MH, Aljizeeri A, Villines TC, Srichai MB, Alsaileek A. Cardiac computed tomography in current cardiology guidelines. J Cardiovasc Comput Tomogr 2015;9(6):514–523. [DOI] [PubMed] [Google Scholar]
- 2.Wolk MJ, Bailey SR, Doherty JU, et al. ACCF/AHA/ASE/ASNC/HFSA/HRS/SCAI/SCCT/SCMR/STS 2013 multimodality appropriate use criteria for the detection and risk assessment of stable ischemic heart disease: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons. J Am Coll Cardiol 2014;63(4):380–406. [DOI] [PubMed] [Google Scholar]
- 3.Knuuti J, Wijns W, Saraste A, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J 2020;41(3):407–477. [DOI] [PubMed] [Google Scholar]
- 4.National Institute for Health and Care Excellence . Chest pain of recent onset: assessment and diagnosis. London, England: National Institute for Health and Care Excellence, 2016. [Google Scholar]
- 5.Kelion AD, Nicol ED. The rationale for the primacy of coronary CT angiography in the National Institute for Health and Care Excellence (NICE) guideline (CG95) for the investigation of chest pain of recent onset. J Cardiovasc Comput Tomogr 2018;12(6):516–522. [DOI] [PubMed] [Google Scholar]
- 6.Dreisbach JG, Nicol ED, Roobottom CA, Padley S, Roditi G. Challenges in delivering computed tomography coronary angiography as the first-line test for stable chest pain. Heart 2018;104(11):921–927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shaw LJ, Blankstein R, Jacobs JE, et al. Defining Quality in Cardiovascular Imaging: A Scientific Statement From the American Heart Association. Circ Cardiovasc Imaging 2017;10(12):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Spilberg G, Scholtz JE, Hoffman U, et al. Availability and Location of Cardiac CT and MR Services in Massachusetts. J Am Coll Radiol 2018;15(4):618–621. [DOI] [PubMed] [Google Scholar]
- 9.Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019;74(10):e177–e232 [Published corrections appear in J Am Coll Cardiol 2019;74(10):1429–1430 and J Am Coll Cardiol 2020;75(7):840.]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bonow RO, Brown AS, Gillam LD, et al. ACC/AATS/AHA/ASE/EACTS/HVS/SCA/SCAI/SCCT/SCMR/STS 2017 Appropriate Use Criteria for the Treatment of Patients With Severe Aortic Stenosis: A Report of the American College of Cardiology Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, European Association for Cardio-Thoracic Surgery, Heart Valve Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons. J Am Coll Cardiol 2017;70(20):2566–2598. [DOI] [PubMed] [Google Scholar]
- 11.Blanke P, Weir-McCall JR, Achenbach S, et al. Computed tomography imaging in the context of transcatheter aortic valve implantation (TAVI) / transcatheter aortic valve replacement (TAVR): An expert consensus document of the Society of Cardiovascular Computed Tomography. J Cardiovasc Comput Tomogr 2019;13(1):1–20. [DOI] [PubMed] [Google Scholar]
- 12.Garcia MJ, Blankstein R, Budoff MJ, et al. COCATS 4 Task Force 7: Training in Cardiovascular Computed Tomographic Imaging. J Am Coll Cardiol 2015;65(17):1810–1821. [DOI] [PubMed] [Google Scholar]
- 13.American College of Radiology . North American Society of Cardiovascular Imaging (NASCI), and the Society of Pediatric Radiology (SPR) Practice Parameter for the Performance and Interpretation of Cardiac Computed Tomography (CT) - Resolution 21 (2016). Reston, Va: American College of Radiology, 2016. [Google Scholar]
- 14.Royal College of Radiologists, Royal College of Physicians, British Society of Cardiovascular Imaging . Standards of practice of computed tomography coronary angiography (CTCA) in adult patients. 2014. [Google Scholar]
- 15.Nieman K, Achenbach S, Pugliese F, Cosyns B, Lancellotti P, Kitsiou A. Cardiac computed tomography core syllabus of the European Association of Cardiovascular Imaging (EACVI). Eur Heart J Cardiovasc Imaging 2015;16(4):351–352. [DOI] [PubMed] [Google Scholar]
- 16.Royal College of Radiologists . Clinical Radiology: 2020 Specialty Training Curriculum. London, England: Royal College of Radiologists, 2020. [Google Scholar]
- 17.Maroules CD, Cheezum MK, Joshi PH, et al. SCCT curriculum guidelines for general (level 1) cardiovascular CT training. J Cardiovasc Comput Tomogr 2015;9(2):81–88. [DOI] [PubMed] [Google Scholar]
- 18.Parwani P, Lopez-Mattei J, Choi AD. Building Bridges in Cardiology and Radiology: Why Collaboration Is the Future of Cardiovascular Imaging. J Am Coll Cardiol 2018;72(20):2534–2538. [DOI] [PubMed] [Google Scholar]
- 19.American College of Radiology . ACR CT Accreditation Program Requirements. Reston, Va: American College of Radiology, 2015. [Google Scholar]
- 20.Fuster V, Halperin JL, Williams ES, et al. COCATS 4 Task Force 1: Training in Ambulatory, Consultative, and Longitudinal Cardiovascular Care. J Am Coll Cardiol 2015;65(17):1734–1753. [DOI] [PubMed] [Google Scholar]
- 21.Joint Royal College of Physicians Training Board . Specialty Training Curriculum for Cardiology.
- 22.Taylor AJ, Patrick J, Abbara S, et al. Relationship between previous training and experience and results of the certification examination in cardiovascular computed tomography. JACC Cardiovasc Imaging 2010;3(9):976–980. [DOI] [PubMed] [Google Scholar]
- 23.Achenbach S, Delgado V, Hausleiter J, Schoenhagen P, Min JK, Leipsic JA. SCCT expert consensus document on computed tomography imaging before transcatheter aortic valve implantation (TAVI)/transcatheter aortic valve replacement (TAVR). J Cardiovasc Comput Tomogr 2012;6(6):366–380. [DOI] [PubMed] [Google Scholar]
- 24.Doherty JU, Kort S, Mehran R, Schoenhagen P, Soman P. ACC/AATS/AHA/ASE/ASNC/HRS/SCAI/SCCT/SCMR/STS 2017 Appropriate Use Criteria for Multimodality Imaging in Valvular Heart Disease: A Report of the American College of Cardiology Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons. J Am Coll Cardiol 2017;70(13):1647–1672. [DOI] [PubMed] [Google Scholar]
- 25.Blanke P, Weir-McCall JR, Achenbach S, et al. Computed Tomography Imaging in the Context of Transcatheter Aortic Valve Implantation (TAVI)/Transcatheter Aortic Valve Replacement (TAVR): An Expert Consensus Document of the Society of Cardiovascular Computed Tomography. JACC Cardiovasc Imaging 2019;12(1):1–24. [DOI] [PubMed] [Google Scholar]
- 26.Wang DD, Geske J, Choi AD, et al. Navigating a Career in Structural Heart Disease Interventional Imaging. JACC Cardiovasc Imaging 2018;11(12):1928–1930. [DOI] [PubMed] [Google Scholar]
- 27.Leipsic J, Nørgaard BL, Khalique O, et al. Core Competencies in Cardiac CT for Imaging Structural Heart Disease Interventions: An Expert Consensus Statement. JACC Cardiovasc Imaging 2019;12(12):2555–2559. [DOI] [PubMed] [Google Scholar]
- 28.Ismail TF, Panikker S, Markides V, et al. CT imaging for left atrial appendage closure: a review and pictorial essay. J Cardiovasc Comput Tomogr 2015;9(2):89–102. [DOI] [PubMed] [Google Scholar]
- 29.Carr CM, Jacob J, Park SJ, Karon BL, Williamson EE, Araoz PA. CT of left ventricular assist devices. RadioGraphics 2010;30(2):429–444. [DOI] [PubMed] [Google Scholar]
- 30.Korsholm K, Berti S, Iriart X, et al. Expert Recommendations on Cardiac Computed Tomography for Planning Transcatheter Left Atrial Appendage Occlusion. JACC Cardiovasc Interv 2020;13(3):277–292. [DOI] [PubMed] [Google Scholar]
- 31.Wang DD, Eng M, Kupsky D, et al. Application of 3-Dimensional Computed Tomographic Image Guidance to WATCHMAN Implantation and Impact on Early Operator Learning Curve: Single-Center Experience. JACC Cardiovasc Interv 2016;9(22):2329–2340. [DOI] [PubMed] [Google Scholar]
- 32.Blanke P, Dvir D, Cheung A, et al. Mitral Annular Evaluation With CT in the Context of Transcatheter Mitral Valve Replacement. JACC Cardiovasc Imaging 2015;8(5):612–615. [DOI] [PubMed] [Google Scholar]
- 33.Wang DD, Eng MH, Greenbaum AB, et al. Validating a prediction modeling tool for left ventricular outflow tract (LVOT) obstruction after transcatheter mitral valve replacement (TMVR). Catheter Cardiovasc Interv 2018;92(2):379–387. [DOI] [PubMed] [Google Scholar]
- 34.Han BK, Casey S, Witt D, et al. Development of a congenital cardiovascular computed tomography imaging registry: Rationale and implementation. J Cardiovasc Comput Tomogr 2018;12(3):263–266. [DOI] [PubMed] [Google Scholar]
- 35.Han BK, Rigsby CK, Hlavacek A, et al. Computed Tomography Imaging in Patients with Congenital Heart Disease Part I: Rationale and Utility. An Expert Consensus Document of the Society of Cardiovascular Computed Tomography (SCCT): Endorsed by the Society of Pediatric Radiology (SPR) and the North American Society of Cardiac Imaging (NASCI). J Cardiovasc Comput Tomogr 2015;9(6):475–492. [DOI] [PubMed] [Google Scholar]
- 36.Han BK, Rigsby CK, Leipsic J, et al. Computed Tomography Imaging in Patients with Congenital Heart Disease, Part 2: Technical Recommendations. An Expert Consensus Document of the Society of Cardiovascular Computed Tomography (SCCT): Endorsed by the Society of Pediatric Radiology (SPR) and the North American Society of Cardiac Imaging (NASCI). J Cardiovasc Comput Tomogr 2015;9(6):493–513. [DOI] [PubMed] [Google Scholar]
- 37.Schuijf JD, Ko BS, Di Carli MF, et al. Fractional flow reserve and myocardial perfusion by computed tomography: a guide to clinical application. Eur Heart J Cardiovasc Imaging 2018;19(2):127–135. [DOI] [PubMed] [Google Scholar]
- 38.Cavalcante R, Onuma Y, Sotomi Y, et al. Non-invasive Heart Team assessment of multivessel coronary disease with coronary computed tomography angiography based on SYNTAX score II treatment recommendations: design and rationale of the randomised SYNTAX III Revolution trial. EuroIntervention 2017;12(16):2001–2008. [DOI] [PubMed] [Google Scholar]
- 39.Taylor AJ, Cerqueira M, Hodgson JM, et al. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 Appropriate Use Criteria for Cardiac Computed Tomography. A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. J Cardiovasc Comput Tomogr 2010;4(6):407.e1–407.e33, e1–e33. [DOI] [PubMed] [Google Scholar]
- 40.White RD, Patel MR, Abbara S, et al. 2013 ACCF/ACR/ASE/ASNC/SCCT/SCMR appropriate utilization of cardiovascular imaging in heart failure: an executive summary: a joint report of the ACR Appropriateness Criteria ® Committee and the ACCF Appropriate Use Criteria Task Force. J Am Coll Radiol 2013;10(7):493–500. [DOI] [PubMed] [Google Scholar]
- 41.Emergency Department Patients With Chest Pain Writing Panel ; Rybicki FJ, Udelson JE, et al. 2015 ACR/ACC/AHA/AATS/ACEP/ASNC/NASCI/SAEM/SCCT/SCMR/SCPC/SNMMI/STR/STS Appropriate Utilization of Cardiovascular Imaging in Emergency Department Patients With Chest Pain: A Joint Document of the American College of Radiology Appropriateness Criteria Committee and the American College of Cardiology Appropriate Use Criteria Task Force. J Am Coll Radiol 2016;13(2):e1–e29. [DOI] [PubMed] [Google Scholar]
- 42.Patel MR, Calhoon JH, Dehmer GJ, et al. ACC/AATS/AHA/ASE/ASNC/SCAI/SCCT/STS 2017 Appropriate Use Criteria for Coronary Revascularization in Patients With Stable Ischemic Heart Disease: A Report of the American College of Cardiology Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and Society of Thoracic Surgeons. J Am Coll Cardiol 2017;69(17):2212–2241 [Published correction appears in J Am Coll Cardiol 2018;71(19):2279–2280.]. [DOI] [PubMed] [Google Scholar]
- 43.Sachdeva R, Valente AM, Armstrong AK, et al. ACC/AHA/ASE/HRS/ISACHD/SCAI/SCCT/SCMR/SOPE 2020 Appropriate Use Criteria for Multimodality Imaging During the Follow-Up Care of Patients With Congenital Heart Disease: A Report of the American College of Cardiology Solution Set Oversight Committee and Appropriate Use Criteria Task Force, American Heart Association, American Society of Echocardiography, Heart Rhythm Society, International Society for Adult Congenital Heart Disease, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Pediatric Echocardiography. J Am Coll Cardiol 2020;75(6):657–703. [DOI] [PubMed] [Google Scholar]
- 44.Abbara S, Blanke P, Maroules CD, et al. SCCT guidelines for the performance and acquisition of coronary computed tomographic angiography: A report of the society of Cardiovascular Computed Tomography Guidelines Committee: Endorsed by the North American Society for Cardiovascular Imaging (NASCI). J Cardiovasc Comput Tomogr 2016;10(6):435–449. [DOI] [PubMed] [Google Scholar]
- 45.Cury RC, Abbara S, Achenbach S, et al. CAD-RADS(TM) Coronary Artery Disease - Reporting and Data System. An expert consensus document of the Society of Cardiovascular Computed Tomography (SCCT), the American College of Radiology (ACR) and the North American Society for Cardiovascular Imaging (NASCI). Endorsed by the American College of Cardiology. J Cardiovasc Comput Tomogr 2016;10(4):269–281. [DOI] [PubMed] [Google Scholar]
- 46.Thomas DM, Divakaran S, Villines TC, et al. Management of Coronary Artery Calcium and Coronary CTA Findings. Curr Cardiovasc Imaging Rep 2015;8(6):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Truong QA, Rinehart S, Abbara S, et al. Coronary computed tomographic imaging in women: An expert consensus statement from the Society of Cardiovascular Computed Tomography. J Cardiovasc Comput Tomogr 2018;12(6):451–466. [DOI] [PubMed] [Google Scholar]
- 48.Choi AD, Abbara S, Branch KR, et al. Society of Cardiovascular Computed Tomography guidance for use of cardiac computed tomography amidst the COVID-19 pandemic. Endorsed by the American College of Cardiology. J Cardiovasc Comput Tomogr 2020;14(2):101–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hecht HS, Cronin P, Blaha MJ, et al. 2016 SCCT/STR guidelines for coronary artery calcium scoring of noncontrast noncardiac chest CT scans: A report of the Society of Cardiovascular Computed Tomography and Society of Thoracic Radiology. J Cardiovasc Comput Tomogr 2017;11(1):74–84 [Published correction appears in J Cardiovasc Comput Tomogr 2017;11(2):170.]. [DOI] [PubMed] [Google Scholar]
- 50.Hecht H, Blaha MJ, Berman DS, et al. Clinical indications for coronary artery calcium scoring in asymptomatic patients: Expert consensus statement from the Society of Cardiovascular Computed Tomography. J Cardiovasc Comput Tomogr 2017;11(2):157–168. [DOI] [PubMed] [Google Scholar]
- 51.Hecht HS, Blaha MJ, Kazerooni EA, et al. CAC-DRS: Coronary Artery Calcium Data and Reporting System. An expert consensus document of the Society of Cardiovascular Computed Tomography (SCCT). J Cardiovasc Comput Tomogr 2018;12(3):185–191. [DOI] [PubMed] [Google Scholar]
- 52.Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019;73(24):3168–3209. [DOI] [PubMed] [Google Scholar]
- 53.Authors/Task Force Members; ESC Committee for Practice Guidelines (CPG); ESC National Cardiac Societies. 2019 ESC/EAS guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Atherosclerosis 2019;290:140–205 [Published corrections appear in Atherosclerosis 2020;292:160–162 and Atherosclerosis 2020;294:80–82.]. [DOI] [PubMed] [Google Scholar]
- 54.Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019;140(11):e596–e646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Budoff MJ, Achenbach S, Blumenthal RS, et al. Assessment of coronary artery disease by cardiac computed tomography: a scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention, Council on Cardiovascular Radiology and Intervention, and Committee on Cardiac Imaging, Council on Clinical Cardiology. Circulation 2006;114(16):1761–1791. [DOI] [PubMed] [Google Scholar]
- 56.Leipsic J, Abbara S, Achenbach S, et al. SCCT guidelines for the interpretation and reporting of coronary CT angiography: a report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovasc Comput Tomogr 2014;8(5):342–358. [DOI] [PubMed] [Google Scholar]
- 57.Expert Panel on Cardiac Imaging and Vascular Imaging; Leipsic JA, Blanke P, et al. ACR Appropriateness Criteria® Imaging for Transcatheter Aortic Valve Replacement. J Am Coll Radiol 2017;14(11S):S449–S455. [DOI] [PubMed] [Google Scholar]
- 58.Buttan AK, Yang EH, Budoff MJ, Vorobiof G. Evaluation of valvular disease by cardiac computed tomography assessment. J Cardiovasc Comput Tomogr 2012;6(6):381–392. [DOI] [PubMed] [Google Scholar]
- 59.Rizvi A, Deaño RC, Bachman DP, Xiong G, Min JK, Truong QA. Analysis of ventricular function by CT. J Cardiovasc Comput Tomogr 2015;9(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rabbat MG, Berman DS, Kern M, et al. Interpreting results of coronary computed tomography angiography-derived fractional flow reserve in clinical practice. J Cardiovasc Comput Tomogr 2017;11(5):383–388. [DOI] [PubMed] [Google Scholar]
- 61.Ramsey BC, Fentanes E, Choi AD, Branch KR, Thomas DM. Myocardial Assessment with Cardiac CT: Ischemic Heart Disease and Beyond. Curr Cardiovasc Imaging Rep 2018;11(7):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Singh A, Mor-Avi V, Patel AR. The role of computed tomography myocardial perfusion imaging in clinical practice. J Cardiovasc Comput Tomogr 2020;14(2):185–194. [DOI] [PubMed] [Google Scholar]
- 63.Patel AR, Bamberg F, Branch K, et al. Society of cardiovascular computed tomography expert consensus document on myocardial computed tomography perfusion imaging. J Cardiovasc Comput Tomogr 2020;14(1):87–100. [DOI] [PubMed] [Google Scholar]
- 64.Nicol ED, Norgaard BL, Blanke P, et al. The Future of Cardiovascular Computed Tomography: Advanced Analytics and Clinical Insights. JACC Cardiovasc Imaging 2019;12(6):1058–1072. [DOI] [PubMed] [Google Scholar]
- 65.Kramer CM, Budoff MJ, Fayad ZA, et al. ACCF/AHA 2007 clinical competence statement on vascular imaging with computed tomography and magnetic resonance. A report of the American College of Cardiology Foundation/American Heart Association/American College of Physicians Task Force on Clinical Competence and Training. J Am Coll Cardiol 2007;50(11):1097–1114. [DOI] [PubMed] [Google Scholar]
- 66.Murphy DJ, Aghayev A, Steigner ML. Vascular CT and MRI: a practical guide to imaging protocols. Insights Imaging 2018;9(2):215–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Dave RB, Fleischmann D. Computed Tomography Angiography of the Upper Extremities. Radiol Clin North Am 2016;54(1):101–114. [DOI] [PubMed] [Google Scholar]
- 68.Scheske JA, Chung JH, Abbara S, Ghoshhajra BB. Computed Tomography Angiography of the Thoracic Aorta. Radiol Clin North Am 2016;54(1):13–33. [DOI] [PubMed] [Google Scholar]
- 69.Hansen NJ. Computed Tomographic Angiography of the Abdominal Aorta. Radiol Clin North Am 2016;54(1):35–54. [DOI] [PubMed] [Google Scholar]
- 70.Raman SP, Fishman EK. Computed Tomography Angiography of the Small Bowel and Mesentery. Radiol Clin North Am 2016;54(1):87–100. [DOI] [PubMed] [Google Scholar]
- 71.Falesch LA, Foley WD. Computed Tomograpy Angiography of the Renal Circulation. Radiol Clin North Am 2016;54(1):71–86. [DOI] [PubMed] [Google Scholar]
- 72.Cook TS. Computed Tomography Angiography of the Lower Extremities. Radiol Clin North Am 2016;54(1):115–130. [DOI] [PubMed] [Google Scholar]