Abstract
Background
In COVID-19 patients with acute respiratory distress syndrome (ARDS), the effectiveness of ventilatory rescue strategies remains uncertain, with controversial efficacy on systemic oxygenation and no data available regarding cerebral oxygenation and hemodynamics.
Methods
This is a prospective observational study conducted at San Martino Policlinico Hospital, Genoa, Italy. We included adult COVID-19 patients who underwent at least one of the following rescue therapies: recruitment maneuvers (RMs), prone positioning (PP), inhaled nitric oxide (iNO), and extracorporeal carbon dioxide (CO2) removal (ECCO2R). Arterial blood gas values (oxygen saturation [SpO2], partial pressure of oxygen [PaO2] and of carbon dioxide [PaCO2]) and cerebral oxygenation (rSO2) were analyzed before (T0) and after (T1) the use of any of the aforementioned rescue therapies. The primary aim was to assess the early effects of different ventilatory rescue therapies on systemic and cerebral oxygenation. The secondary aim was to evaluate the correlation between systemic and cerebral oxygenation in COVID-19 patients.
Results
Forty-five rescue therapies were performed in 22 patients. The median [interquartile range] age of the population was 62 [57–69] years, and 18/22 [82%] were male. After RMs, no significant changes were observed in systemic PaO2 and PaCO2 values, but cerebral oxygenation decreased significantly (52 [51–54]% vs. 49 [47–50]%, p < 0.001). After PP, a significant increase was observed in PaO2 (from 62 [56–71] to 82 [76–87] mmHg, p = 0.005) and rSO2 (from 53 [52–54]% to 60 [59–64]%, p = 0.005). The use of iNO increased PaO2 (from 65 [67–73] to 72 [67–73] mmHg, p = 0.015) and rSO2 (from 53 [51–56]% to 57 [55–59]%, p = 0.007). The use of ECCO2R decreased PaO2 (from 75 [75–79] to 64 [60–70] mmHg, p = 0.009), with reduction of rSO2 values (59 [56–65]% vs. 56 [53–62]%, p = 0.002). In the whole population, a significant relationship was found between SpO2 and rSO2 (R = 0.62, p < 0.001) and between PaO2 and rSO2 (R0 0.54, p < 0.001).
Conclusions
Rescue therapies exert specific pathophysiological mechanisms, resulting in different effects on systemic and cerebral oxygenation in critically ill COVID-19 patients with ARDS. Cerebral and systemic oxygenation are correlated. The choice of rescue strategy to be adopted should take into account both lung and brain needs.
Registration The study protocol was approved by the ethics review board (Comitato Etico Regione Liguria, protocol n. CER Liguria: 23/2020).
Supplementary Information
The online version contains supplementary material available at 10.1186/s13054-021-03537-1.
Keywords: Coronavirus, Cerebral oxygenation, Rescue therapies, Prone position, Recruitment maneuvers, Carbon dioxide removal
Introduction
In late December 2019, an outbreak of respiratory infection caused by a then-unknown virus was detected in Wuhan, China. Since then, severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) has spread worldwide, causing a pandemic of coronavirus disease 2019 (COVID-19) which overwhelmed intensive care units (ICUs) [1]. Although most patients with SARS-CoV-2 experience only mild symptoms such as fever and cough, a substantial number of patients develop severe hypoxemic respiratory failure, requiring intubation and mechanical ventilation [2, 3], with multiorgan failure in the most severe cases [4].
Recent publications have highlighted the specific features of COVID-19-associated acute respiratory distress syndrome (ARDS) [3, 5, 6], which make ventilatory management particularly challenging [7–10].
Patients with COVID-19-associated ARDS have a form of injury which, in many aspects, resembles ARDS unrelated to COVID-19 [11]. Adherence to evidence-based management has been recommended, including lung-protective mechanical ventilation and positive end-expiratory pressure (PEEP), as suggested by international guidelines for ARDS [12]. The value of other respiratory rescue therapies, such as recruitment maneuvers (RM), prone positioning (PP), inhaled nitric oxide (iNO), and carbon dioxide removal by ECCO2R or extracorporeal membrane oxygenation (ECMO), remains uncertain in this cohort of patients [13–16], with controversial efficacy concerning systemic oxygenation.
No data are available regarding the effect of these rescue therapies on cerebral hemodynamics, particularly on cerebral oxygenation. This latter point is of extreme importance, as neurological complications are common in mechanically ventilated critically ill patients with COVID-19 [17, 18] and may lead to impaired cerebral hemodynamics [17, 19]. Furthermore, respiratory rescue therapies may have detrimental effects on brain physiology, especially in the early phases after application, when the major hemodynamic and respiratory changes occur; therefore, their application in brain-injured patients outside of the COVID-19 pandemic is currently debated [20–22].
We hypothesized that each rescue strategy would have different effects on respiratory and cerebral oxygenation. Thus, the choice of ventilatory rescue therapy should take into account both lung and cerebral needs.
A prospective observational study was conducted to assess the early effects of different ventilatory rescue therapies currently used in ICU (RMs, PP, iNO or ECCO2R) on systemic and cerebral oxygenation in mechanically ventilated patients with COVID-19-associated ARDS. For this purpose, arterial blood gases and systemic and cerebral hemodynamics were analyzed. The correlation between systemic and cerebral oxygenation in the whole population was also assessed before and after rescue therapies.
Methods
Study design
This study followed the “Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)” statement guidelines for observational cohort studies (Additional file 1) [23]. This prospective, single-center observational study was conducted in a university-affiliated hospital in Genoa, northern Italy (Ospedale Policlinico San Martino, IRCCS for Oncology and Neuroscience). The study protocol was approved by the local ethics review board (Comitato Etico Regione Liguria, protocol n. CER Liguria: 23/2020). Written consent was obtained from next of kin, as patients were unconscious at the time of inclusion.
Study population
This study included consecutive critically ill patients with COVID-19, as confirmed by SARS-CoV2 polymerase chain reaction on nasopharyngeal swab specimens, admitted to our ICU during the second wave of the SARS-CoV-2 pandemic in Italy (from October 1, 2020, to December 15, 2020).
Further inclusion criteria were adult age (≥ 18 years old), requiring intubation and mechanical ventilation, and acute onset of ARDS, as defined by the Berlin criteria [24], which included new or worsening respiratory symptoms due to SARS-CoV-2 infection with hypoxemia (defined by a ratio between partial pressure of oxygen in arterial blood [PaO2] and fraction of inspired oxygen [PaO2/FiO2] ≤ 300 mmHg on positive end-expiratory pressure [PEEP] ≥ 5 cmH2O, regardless of FiO2; presence of bilateral pulmonary infiltrates on chest imaging [X-ray or computed tomography]; and absence of left atrial hypertension or no clinical signs of left heart failure), who required one or more ventilatory rescue therapies according to clinical needs (RMs, PP, iNO, ECCO2R), and who contemporarily underwent noninvasive multimodal neuromonitoring, including cerebral oxygenation using near-infrared spectroscopy (NIRS) and transcranial Doppler (TCD) as per our local clinical practice.
The exclusion criteria were non-confirmed SARS-CoV-2 infection according to WHO guidance [25], patients with no data at baseline or who did not undergo any type of rescue therapies or neuromonitoring, or those in which TCD or NIRS could not be performed (absence of temporal window or space in the forehead for NIRS sensor positioning).
Data collection
Demographic, epidemiologic, and clinical data were collected from electronic medical records, both at admission to the ICU and on the day when each rescue therapy was performed. Data from patients’ electronic medical records were reviewed and collected by physicians trained in critical care. Patients’ confidentiality was protected by assigning a de-identified patient code.
General monitoring data
Recorded data included admission demographics such as age, gender, Sequential Organ Failure Assessment (SOFA), body mass index (BMI), comorbidities (hypertension, diabetes mellitus, chronic kidney injury, chronic respiratory disease, previous neurological disease, liver failure, chronic cardiac disease), vital signs such as mean arterial pressure (MAP), heart rate (HR), laboratory parameters such as blood test, D-dimer, C-reactive protein (CRP), procalcitonin (PCT), creatinine, hemoglobin (Hb) and ventilatory parameters such as tidal volume (VT), FiO2, respiratory rate (RR), PEEP, plateau pressure (Pplat), respiratory system compliance (Crs), ICU length of stay (LOS), and mortality.
Ventilatory parameters such as PEEP, Pplat, Crs, VT, FiO2, saturation of oxygen (SpO2), pHa, PaO2, partial pressure of carbon dioxide (PaCO2), systemic (MAP, HR) and neuromonitoring parameters (TCD and NIRS-derived indices) were obtained before (T0) and after (T1) the application of any type of rescue therapy.
Ventilator management and rescue therapies
Patients were sedated with propofol (or midazolam) and fentanyl and paralyzed with a continuous infusion of cisatracurium besilate. They were ventilated in pressure-controlled mode (P-CMV), aiming to maintain PPlat < 28 cmH2O, using a VT of 4–8 mL/kg of predicted body weight (PBW); FiO2 and PEEP were titrated in order to achieve SpO2 88–92%, and RR to aim for PaCO2 = 35–45 mmHg or allow permissive hypercapnia as long as pHa was maintained in range.
The decision to start any type of rescue therapy was related to the clinician’s assessment and judgment. In our institution, the use of rescue therapies (RM, PP, iNO) was considered when patients presented severe ARDS with PaO2/FiO2 values < 100 for more than 6 h with worsening clinical trajectory [26].
ECCO2R was considered when pHa was below 7.3 and/or PaCO2 higher than 70 mmHg, with Pplat higher than 27 cmH2O, not responsive to conventional treatment.
As for our local protocol, after optimizing lung protective strategies, we progressively increased the FiO2 to 100% before starting any type of rescue therapy. From T0 and T1, FiO2 was not modified. In case of refractory hypoxemia, RMs and/or iNO and prone positioning were used. Recruitment maneuvers were used when the patients were considered potentially PEEP responders according to respiratory system mechanics and computed tomography (CT) findings. In the presence of posterior atelectasis at the lung CT, prone positioning was the treatment of choice. Finally, iNO was considered in cases of refractory hypoxemia with clinical suspect on echocardiography of pulmonary hypertension and CT findings.
Recruitment maneuvers
Recruitment maneuvers were applied using an escalating PEEP strategy, as is common practice at in our institution. For PEEP titration, VT was kept constant and PEEP was increased up to maximal inspiratory pressure 35–40 cmH2O for 30 s (five breaths at each PEEP level) followed by decremental PEEP titration according to SpO2, respiratory system mechanical properties and hemodynamic parameters. T1 measurements were taken 5–10 min after the RM.
Prone positioning
Patients were carefully turned from the supine to prone position by a team of 4 staff members (3 staff nurses and 1 physicians); 2 on each side and 1 (the anesthetist) controlling head and airways and coordinating the procedure.
In the PP, we limited the shoulder abduction to < 90 degrees to avoid overstretching of the brachial plexus. We placed the forearm in a neutral position to minimize the direct pressure on the ulnar nerve at the elbow and applied soft padding under the elbows, chest, and pelvis. The potential for increased intrathoracic pressure caused by increased abdominal pressure in the prone position was minimized by using foam padding to limit abdominal compression. The head was put in neutral position on an open soft head ring (Horseshoe Head Pad—High—Adult Size) to avoid any direct pressure to the eyes, nose, and mouth. T1 measurements were taken 30 min–1 h after patient positioning.
Inhaled nitric oxide
Nitric oxide gas was provided through the breathing circuit (Maquet-Kinox, Healthcare, Canada 2020) at a test concentration of 20 ppm. After assessing the response of systemic and cerebral oxygenation to iNO (from T0 and T1 after 1 h) [27], iNO was titrated according to patients’ needs and arterial blood gases.
Extracorporeal CO2 removal
ECCO2R was started in case of refractory hypercapnia with decompensated pHa and was provided using two methods using systemic heparin anticoagulation: (1) using a dedicated or pump-driven venovenous (EstorFlow®, Estor, Milan, Italy) ECCO2 removal device. ECCO2R was commenced at a blood flow of 200 mL/min and air flow of 10–12 l/min, and then blood and gas flows were titrated according to patients’ response and arterial blood gases values. (2) a polymethylpentene, hollow-fiber, gas-exchanger membrane (multiECCO2R; Eurosets, Medolla, Italy), a labeled and certified European device to be used in conjunction with multiFiltrate continuous renal replacement therapy (CRRT) platforms (Fresenius Medical Care, Bad Homburg, Germany) for combined respiratory and renal support. ECCO2R + CRRT was commenced at a blood flow of 200–400 mL/min, and continuous venovenous hemodialysis (CVVHD) was delivered with an effluent dose of 25 mL/kg/h; blood flow was increased stepwise according to the patient response. T1 measurements were taken after 20 min from ECCO2R initiation.
Neuromonitoring data
Cerebral oxygenation
Continuous regional cerebral oxygen saturation was obtained using a Masimo Root monitor® (USA) with bilateral sensors applied to the frontotemporal area. Final cerebral oxygenation was calculated as the mean between the right and left frontotemporal sensors. The Masimo tool is able to noninvasively estimate different innovative NIRS-derived parameters (Additional file 1: Fig. S1):
rSO2: total value of regional cerebral oxygen saturation.
Variation of O2Hbi (ΔO2Hbi): an index associated with variation of the oxygenated component of the Hb of the total calculation of rSO2, thus representing changes in the arterial component of rSO2.
Variation of HHbi (ΔHHbi): an index associated with variation of the deoxygenated component of Hb within the total calculation of rSO2, thus representing changes in the venous component of rSO2.
Variation of cHbi (ΔcHbi) is the sum of the values of ΔO2Hbi e ΔHHbi to calculate the value rSO2 (ΔcHbi = ΔHHbi + ΔO2Hbi)
Variation of SpO2–rSO2: difference between the value of SpO2 and rSO2
Noninvasive intracranial pressure assessment
Noninvasive ICP (nICP) was measured using the transcranial color duplex Doppler technique (Philips Bothwell 98021®, USA), with a low-frequency (2 MHz) echo graphic micro-convex probe to investigate intracranial vessels. The temporal window was used to assess bilaterally the proximal part of the mean cerebral artery (MCA) [28, 29]. Systolic, diastolic, and mean flow velocities (FVs, FVd, and FVm, respectively) were obtained bilaterally from the MCA, and nICP is calculated according to the formula [30]:
The final nICP was calculated as the mean of the right and left nICP in both the MCAs.
Statistical analysis
No data on arterial and cerebral oxygenation after rescue therapies are available in COVID-19 patients, and therefore, a formal a priori sample size calculation was not feasible. However, the achieved sample size was comparable to other physiologic studies in the field [31–33]. For the two rescue therapies for which we observed the highest impact on arterial and cerebral oxygenation (RMs and PP), the achieved sample size resulted in a power (1-β) above 90%, assuming an intrasubject correlation of R = 0.5.
The Shapiro–Wilk test was used to test the normality of the distribution of the results. Data are reported as median and interquartile range [IQR = 25th–75th percentiles], if not otherwise specified.
Comparisons between different variables at T0 and T1 were made by repeated measures t test, while non-normally distributed variables were compared by Wilcoxon signed-rank test.
The correlations between cerebral and systemic oxygenation were verified. Correlations with repeated measurements were computed according to the Bland and Altman method [34, 35]. All statistical analyses were performed using SPSS 21® (IBM corp., US) and RStudio software (version 4.0.3). A p < 0.05 was considered statistically significant.
Results
Baseline characteristics
Thirty-eight patients with COVID-19-associated ARDS were admitted to the ICU during the study period. Among these, 22 patients received at least one or more rescue therapies and were included in the final analysis. A total of 45 rescue therapies were used, and measurements before and after rescue therapies (at T0 and T1) were taken from each patient.
Demographic and clinical characteristics of the population included in our study are presented in Additional file 1: Table S1. The median age was 62 years [IQR = 57–69], and 18/22 (82%) were male. On ICU admission, the median PaO2/FiO2 was 81 mmHg [IQR = 65–82.5]. Rescue therapies included 22 RMs, 9 iNO administrations, 10 prone positionings, and 4 ECCO2R or respiratory dialysis applications.
Effect of rescue therapies in the overall population
Considering the overall population, at T0, the median PEEP was 12 (IQR = [11–13]) cmH20, median Pplat 29 [28–30] cmH20, and median VT 5.7 [5.5–6.2] ml/predicted body weight (PBW); the median baseline PaO2 was 66 [62–72] mmHg, PaCO2 54 [48–64] mmHg, pHa 7.37 [7.33–7.41], median MAP 72 [68–76.5] mmHg, and median HR was 75 [65–88.5] beats per minute (Table 1).
Table 1.
Ventilator settings, neuromonitoring values, and hemodynamic data at time points T0 (before rescue therapy) and T1 (after rescue therapy)
| Parameter | All (N = 45) | RM (N = 22)RM (N = 22) | Prone position (N = 10) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| T0 | T1 | p value | T0 | T1 | p value | T0 | T1 | p value | |
| Primary outcome | |||||||||
| rSO2 (%) | 53 [51–55] | 52 [49–59] | 0.692 | 52 [51–54] | 48.5 [47–50] | < 0.0001* | 53 [52–54] | 59.5 [59–64] | 0.005* |
| PaO2 /FiO2 | 66 [62–72] | 71 [67–74] | 0.002* | 66 [62–72] | 67.5 [63–72] | 0.189 | 62 [56–71] | 81.5 [76–87] | 0.005* |
| SpO2 (%) | 88 [87–90] | 91 [89–92] | < 0.0001* | 88 [87–89] | 89 [88–91] | 0.072 | 87 [86–88] | 93 [89–96] | 0.005* |
| Ventilator settings | |||||||||
| PEEP (cmH2O) | 12 [11–13] | 12 [11–13] | 0.169 | 12 [11–13] | 12 [10–13] | 0.157 | 12 [11–13] | 12 [10–13] | 0.317 |
| Pplat (cmH2O) | 29 [28–30] | 29 [28–30] | 0.698 | 29 [28–30] | 29 [28–30] | 1.000 | 29 [28–30] | 29 [28–30] | 1.000 |
| VT/PBW (mL/Kg) | 5.7 [5.5–6.2] | 5.9 [4.9–6.9] | 0.086 | 6.7 [6–7.1] | 6.3 [5.4–6.6] | 0.001* | 5.4 [5.1–6.1] | 6.3 [6–7.1] | 0.005* |
| RR (n/min) | 26 [24.5–27.5] | 26 [24.5–28] | 0.026* | 25 [24–26] | 25 [24–26] | 0.109 | 27.5 [26–28] | 27.5 [26–28] | 1.000 |
| Crs (mL/cmH2O) | 20.1 [18.2–24.7] | 19.8 [17.8–23.5] | 0.615 | 21.6 [19.4–25.2] | 20.1 [19.6–24.5] | 0.200 | 14.9 [13.4–18.6] | 23.4 [19.5–26.4] | 0.005* |
| Neuromonitoring | |||||||||
| ΔcHbi | 4.3 [3–6] | 4.7 [2.6–7.7] | 0.157 | 5 [3.7–6.1] | 3.2 [2.5–4.6] | < 0.0001* | 4.5 [2.4–6.5] | 10.2 [8.9–12.4] | 0.005* |
| ΔO2Hbi | 3.2 [2.7–4.2] | 2.1 [1.4–5.3] | 0.991 | 3.7 [2.9–4.4] | 1.7 [1.3–2.1] | < 0.0001* | 3.5 [2.1–4.6] | 8 [6.3–8.8] | 0.005* |
| ΔHHbi | 0.9 [0.3–1.8] | 2.1 [1.2–2.8] | < 0.0001* | 1.1 [0.8–1.8] | 1.3 [1.1–2.2] | 0.001* | 1 [0.2–1.9] | 2.3 [2.1–3.9] | 0.005* |
| nICP (mmHg) | 17 [15.5–19] | 21 [17–26] | < 0.0001* | 17.5 [15–19] | 26 [24–28] | < 0.0001* | 16 [15–18] | 18 [16–20] | 0.016* |
| nCPP (mmHg) | 55 [51–60] | 50 [39–59] | 0.001* | 54 [50–62] | 39 [35–44] | < 0.0001* | 55.5 [53–58] | 60.5 [59–63] | 0.011* |
| ΔSpO2rSO2 (%) | 36 [37–37 | 38 [33–41] | 0.001* | 36 [35–37] | 41 [38–43] | < 0.0001* | 33.5 [32–35] | 31.5 [30–33.5] | 0.134 |
| Other arterial blood gas values | |||||||||
| pHa | 7.37 [7.33–7.41] | 7.38 [7.35–7.41] | 0.017* | 7.38 [7.34–7.41] | 7.38 [7.35–7.42] | 0.466 | 7.37 [7.34–7.41] | 7.41 [7.38–7.43] | 0.024* |
| PaCO2 (mmHg) | 54 [48–64] | 53 [47–63] | < 0.0001* | 51 [46–56] | 50 [45–56] | 0.108 | 53.5 [47–71] | 53.3 [47–69] | 0.021* |
| Hemodynamics | |||||||||
| Hb (mg/dL) | 8.5 [8.1–8.8] | 8.3 [8.1–8.7] | 0.119 | 8.6 [8.2–8.8] | 8.4 [8.3–8.8] | 0.343 | 8.5 [8.1–8.9] | 8.3 [8.1–8.7] | 0.321 |
| MAP (mmHg) | 72 [68–76.5] | 71 [65–76] | 0.013* | 71.5 [67–76] | 64 [59–68] | < 0.0001* | 72.5 [68–75] | 78.5 [71–84] | 0.005* |
| HR (n/min) | 75 [65–88.5] | 77 [68–94] | 0.015* | 77.5 [68–89] | 79 [69–91] | 0.009* | 77 [75–85] | 78 [72–83] | 0.878 |
| Parameter | iNO (N = 9) | ECCO2R (N = 4) | ||||
|---|---|---|---|---|---|---|
| T0 | T1 | p value | T0 | T1 | p value | |
| Primary outcome | ||||||
| rSO2 (%) | 53 [51–56] | 57 [55–59] | 0.007* | 59 [55.5–64.5] | 56 [52.5–62] | 0.002* |
| PaO2 /FiO2 | 65 [67–73] | 72 [67–73] | 0.015* | 75 [74.5–78.5] | 63.5 [60–69.5] | 0.009* |
| SpO2 (%) | 89 [88–90] | 92 [91–93] | 0.016* | 93 [91.5–94] | 89.5 [87.5–91] | 0.01* |
| Ventilator settings | ||||||
| PEEP (cmH2O) | 12 [11–14] | 12 [10–13] | 0.025* | 12 [1113] | 10.5 [10–11] | 0.103 |
| Pplat (cmH2O) | 29 [28–29] | 29 [28–29] | 1.000 | 29.5 [28–30.5] | 29.5 [28–30.5] | 0.543 |
| VT/PBW (mL/Kg) | 5.7 [5.2–7.4] | 5.9 [5.3–7.2] | 0.441 | 5.7 [3–6.7] | 4.3 [3.8–6] | 0.068 |
| RR (n/min) | 25 [20–26] | 26 [22–26] | 0.102 | 29 [27–30] | 29 [27–30] | 0.225 |
| Crs (mL/cmH2O) | 20.8 [19.3–26.5] | 16.7 [19.6– 26.6] | 0.086 | 17 [15.9–18.9] | 13.5 [11.3–15.7] | 0.465 |
| Neuromonitoring | ||||||
| ΔcHbi | 3.1 [3–4.3] | 7.1 [7–8.1] | 0.008* | 3.6 [2.7–4.2] | 1.3 [0.7–1.9] | 0.002* |
| ΔO2Hbi | 2.8 [2.6–3.7] | 4.7 [4.1–5.2] | 0.008* | 3 [2.3–3.4] | 0.6 [0.2–1.2] | 0.002* |
| ΔHHbi | 0.4 [0.3–1.2] | 2.8 [1.9–2.9] | 0.008* | 0.6 [0.3–0.8] | 0.7 [0.4–0.8] | 0.182 |
| nICP (mmHg) | 18 [17–19] | 17 [16–18] | 0.033* | 22.5 [19–26] | 18.5 [15–23] | 0.006* |
| nCPP (mmHg) | 59 [54–60] | 59 [53–60] | 0.395 | 50.5 [50–52] | 53 [52–54.5] | 0.059 |
| ΔSpO2rSO2 (%) | 36 [34–37] | 35 [33––37] | 0.320 | 34 [29.5–36] | 33.5 [29–35] | 0.058 |
| Other arterial blood gas values | ||||||
| pHa | 7.36 [7.35–7.38] | 7.38 [7.36–7.39] | 0.031* | 7.21 [7.19–7.26] | 7.36 [7.34–7.37] | 0.008* |
| PaCO2 (mmHg) | 54 [48–68] | 55[48–67] | 0.058 | 100 [99–100] | 72 [70–73] | < 0.0001* |
| Hemodynamics | ||||||
| Hb (mg/dL) | 8.1 [7.9–8.3] | 8.3 [7.7–8.3] | 0.432 | 8.1 [7.8–8.5] | 8.2 [7.9–8.5] | 0.314 |
| MAP (mmHg) | 76 [71–76] | 75 [70–77] | 0.248 | 73 [69–78] | 71.5 [67–77.5] | 0.141 |
| HR (n/min) | 69 [64–75] | 67 [65–89] | 0.917 | 65.5 [65–71.5] | 73 [69.5–78] | 0.049* |
Values are presented as median and Interquartile range if not otherwise specified
ECCO2R extracorporeal carbon dioxide removal, RM recruitment maneuvers, iNO inhaled nitric oxide, PaO2 partial pressure of oxygen, FiO2 inspired fraction of oxygen ratio, SpO2 oxygen saturation, PEEP positive end-expiratory pressure, Pplat plateau pressure, VT tidal volume, PBW predicted body weight, RR respiratory rate, Crs respiratory system compliance, rSO2 cerebral oxygenation saturation, nICP noninvasive intracranial pressure, nCPP noninvasive cerebral perfusion pressure
DeltaO2Hbi (ΔO2Hbi), change in the oxygenated component of hemoglobin (Hb); delta HHbi (ΔHHbi), change in the deoxygenated component of Hb; delta cHbi (ΔcHbi), sum of the values of ΔO2Hbi; ΔcHbi = ΔHHbi + ΔO2Hbi; ΔSpO2–rSO2, difference between the value of SpO2 and rSO2; N number
The baseline median rSO2 was 53% [51–55], with ΔcHbi 4.3 [3–6], ΔHHbi 0.9 [0.3–1.8] and ΔO2Hbi 3.2 [2.7–4.2]; the nICP was 17 [15.5–19].
At T1, SpO2, PaO2, and nICP values were significantly increased compared to T0 (88 [87–90] vs. 91% [89–92], p < 0.001; 66 [62–72] vs. 71 [67–74] mmHg; p = 0.002; 17 [15.5–19] vs. 21 [17–26] mmHg, p < 0.001, respectively), whereas PaCO2 was significantly lower compared to T0 (median = 54 [48–64] mmHg vs. 53 [47–63]; p < 0.001). No differences in rSO2 were observed between T0 and T1 (54 [48–64] vs. 53 [47–63] %, p = 0.692) (Table 1). From T0 to T1, nCPP was reduced (55 [51–60] vs. 50 [39–59], p = 0.001). Additional file 1: Table S2 presents the effect of rescue therapies according to subgroups with low or high PaO2, dichotomized according to the median value of PaO2.
Correlations between systemic and cerebral oxygenation in the overall population
Considering the entire data (T0 + T1 = 90 measurements), a statistically significant correlation between SpO2 and rSO2 values was observed overall (r = 0.62, p < 0.001), at T0 (r = 0.64, p < 0.001), and T1 (r = 0.73, p < 0.001) (Fig. 1). PaO2 and rSO2 were also overall correlated (r = 0.54, p < 0.001.), at T0 ((r = 0.52, p = 0.01) and T1 (r = 0.61, p = 0.001) (Fig. 1). We also found a significant correlation between the changes in rSO2 and in SpO2, PaO2, and rSO2 (Additional file 1: Fig. S2). Finally, a statistically significant correlation was found between PaCO2 and rSO2 (T0 r = 0.31, p = 0.038; T1 r = 0.269, p = 0.074; overall values r = 0.315, p = 0.002), and between MAP and rSO2 (T0 r = 0.262, p = 0.082; T1 r = 0.609, p = 0.001; overall values r = 0.357, p = 0.001).
Fig. 1.
Scatterplots showing the linear association and correlation (R) between systemic oxygen saturation (SpO2) (left panel) and partial pressure of oxygen (PaO2) (right panel) versus cerebral oxygenation (rSO2) at different study timepoints. Repeated measurements for each patient are plotted in the same color pattern. Linear regression lines are correspondent to repeated measurements within patients
Specific subgroups
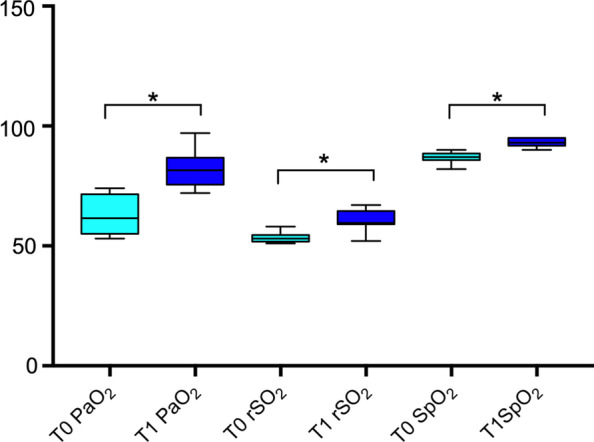
Twenty-two patients underwent RMs, after which no significant changes were observed in PaO2 and PaCO2 values (Table 1). At T1, values of cerebral oxygenation (both arterial and venous components) were decreased (rSO2 52 [51–54] vs. 48.5% [47–50], p < 0.001), whereas nICP increased significantly compared to T0 (17.5 [15–19] vs. 26 [24–28] mmHg, p < 0.001). Furthermore, MAP and nCPP were decreased after RM application (71.5 [67–76] vs. 64 [59–68] mmHg, p < 0.001 and 54 [50–62] vs. 39 [35–44] mmHg, p < 0.001, respectively) (Fig. 2).
Fig. 2.

Boxplots representing the effect of recruitment maneuvers (RMs) on partial pressure of oxygen (PaO2), cerebral oxygenation (rSO2), and oxygen saturation (SpO2) from baseline, T0 (pre), and after RMs, T1 (post). Values are presented as median and interquartile range
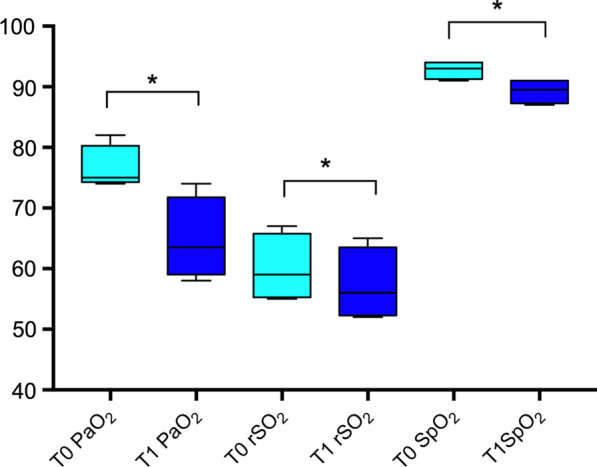
After prone positioning (N = 10), systemic and cerebral oxygenation increased significantly (PaO2 = 62 [56–71] vs. 81.5 [76–87]mmHg, p = 0.005; rSO2 = 53 [52–54]% vs. 59.5 [59–64]%, p = 0.005), with a slight increase in nICP (16 [15–18] vs. 18 [16–20] mmHg, p = 0.016), MAP (72.5 [68–75] vs. 78.5 [71–84]mmHg, p = 0.005), and nCPP (55.5 [53–58] vs. 60.5 [59–63]mmHg, p = 0.011) (Fig. 3).
Fig. 3.
Boxplots representing the effect of prone positioning on partial pressure of oxygen (PaO2), cerebral oxygenation (rSO2), and oxygen saturation (SpO2), from baseline, T0 (pre), and after prone positioning, T1 (post). Values are presented as median and interquartile range
After iNO, both systemic and cerebral oxygenation values increased (65 [67–73] vs. 72 [67–73] mmHg, p = 0.015, and 53 [51–56]% vs. 57 [55–59]%, p = 0.007, respectively), with no effect on MAP and nCPP and a slight reduction of nICP (18 [17–19] vs. 17 [16–18] mmHg, p = 0.033) (Fig. 4).
Fig. 4.

Boxplots representing the effect of inhaled nitric oxide (iNO) on partial pressure of oxygen (PaO2), cerebral oxygenation (rSO2), and oxygen saturation (SpO2) from baseline, T0 (pre), and after iNO, T1 (post). Values are presented as median and Interquartile range
Finally, ECCO2R was used in four patients. The use of CO2 removal resulted in a decrease in PaO2 (75 [74.5–78.5] vs. 63.5 [60–69.5] mmHg, p = 0.009), SpO2 (93 [87.5–91] vs. 89.5 [87.5–91]%), PaCO2 (100 [9–100] vs. 72 [70–73] mmHg, p < 0.001), and rSO2 (59 [55.5–64.5] vs. 56 [52.5–62]%, p = 0.002), and in particular, in the oxygenated component of ΔcHbi (ΔO2Hbi = 3.6 [2.7–4.2] vs. 1.3 [0.7–1.9], p = 0.002) (Table 1; Fig. 5).
Fig. 5.
Boxplots representing the effect of ECCO2R or respiratory dialysis on partial pressure of oxygen (PaO2), cerebral oxygenation (rSO2), and oxygen saturation (SpO2) from baseline, T0 (pre), and after CO2 removal, T1 (post). Values are presented as median and interquartile range
Discussion
In the present study, we investigated the early effects of different types of rescue therapies on systemic and cerebral oxygenation in patients with COVID-19-associated ARDS. We found that iNO and prone positioning improved systemic and cerebral oxygenation; RMs did not improve systemic oxygenation, but worsened rSO2; respiratory dialysis/ECCO2R reduced both systemic and cerebral oxygenation, and in the whole population, a significant correlation was found between SpO2 and rSO2, and between rSO2 and PaO2 .
To our knowledge, this is the first study investigating the early effects of rescue therapies on systemic and cerebral oxygenation and their correlation in critically ill patients with COVID-19-associated ARDS. The use of multimodal neuromonitoring, including new indices such as ΔHHbi + ΔO2Hbi, enabled us to better investigate the specific consequences of each ventilatory rescue strategy for brain and lung function. This is particularly important, especially in the early phases after rescue therapies application, when most of the effects on cerebral physiology are mainly acting.
The lung and brain are important organs to be monitored. COVID-19 patients often present with severe hypoxemia not responsive to conventional treatment and at the same time are at high risk of neurological complications [17, 36]. In this context, the role of rescue therapies generally used to improve oxygenation and outcomes in conventional severe ARDS [37–39] has not been completely elucidated in COVID-19 [14, 40–43].
In a recent prospective physiological study [31] where a two-step positive end-expiratory pressure trial with change of 10 cmH2O was applied, potential for lung recruitment was found to vary widely among patients. Similarly, the efficacy of iNO has not been completely defined in COVID-19 patients; although iNO can significantly improve oxygenation, probably helping in redistribution of pulmonary flow [14], its effect on oxygenation is inconsistent among studies [44]. Prone positioning has been increasingly used during the pandemic [30, 41, 45], and preliminary reports suggest a beneficial effect of this maneuver on the PaO2/FiO2 ratio. Finally, few case reports [13] are available regarding the use of respiratory dialysis/ECCO2R in this population as an adjuvant therapy to limit further ventilator-induced lung injury. The potential harmful effects of these therapies on cerebral hemodynamics have not been investigated. Although COVID-19 patients are not primarily brain-injured, a significant proportion of them experience neurological complications [36, 46, 47]; the pathophysiology of such complications in this cohort of patients is complex and probably multifactorial, including different mechanisms such as viral neurotropism, hypercoagulability, and brain–lung crosstalk [48], with cerebral hypoxemia [17, 19] consequent to severe respiratory failure. The use of rescue therapies can further aggravate the delicate relationship between the brain and the lungs in these patients [49–54]. The use of RM and prone positioning can potentially increase intrathoracic pressure and therefore ICP [28], while extracorporeal systems such as respiratory dialysis/ECCO2 removal or ECMO may potentially increase the risk for intracerebral hemorrhage [55].
The concept of protective ventilation and the use of rescue therapies is slowly gaining interest even in this population, although evidence is still lacking [20, 56, 57]; small studies and a recent expert consensus on mechanical ventilation in acute brain injury suggested considering at least prone position in patients who have concurrent ARDS and acute brain injury but no significant ICP elevation, whereas the role of RMs, CO2 removal systems, and ECMO is still uncertain [20, 52, 53].
Our findings suggest that each rescue therapy has specific effects on systemic and cerebral oxygenation, which reflect specific pathophysiological effects of each strategy on systemic and cerebral dynamics.
RMs and respiratory dialysis/ECCO2R seem to have no beneficial effect on systemic and cerebral oxygenation, whereas prone positioning and iNO can improve both systemic and cerebral oxygenation. Both RMs and prone positioning may increase ICP, but RMs seem to have a major effect on the hemodynamic system, causing an important reduction of MAP and thus reducing CPP. Prone positioning led to an increase in both the arterial and venous components of rSO2, suggesting an increase in CPP and a reduction of jugular venous return, causing only slightly increased nICP, whereas after RMs the arterial component was reduced (consequent to arterial hypotension) and the venous component was slightly increased (consequent to impairment of venous return), causing a substantial increase in ICP. iNO had no detrimental effect on MAP, nCPP, or nICP and should therefore be considered in cases of systemic and cerebral hypoxemia when ICP is unstable. Respiratory dialysis/ECCO2R has good efficacy in reducing both PaCO2 and nICP values, but it also causes a reduction in systemic and cerebral oxygenation. While reduction of rSO2 could be consequent to a rapid reduction of PaCO2, thus causing cerebral arterial vasoconstriction (with decrease in the arterial component of rSO2), the effect on systemic oxygenation is unclear; however, we hypothesize that the combination of higher pHa and lower PaCO2 reduces hypoxic pulmonary vasoconstriction, leading to lower oxygenation [58].
Overall, we found a strong correlation between systemic and cerebral oxygenation, thus confirming that systemic oxygenation values are the major determinants of cerebral oxygen status, as previously demonstrated [59–62]. Also, the strong correlation we found between the changes in SpO2 and rSO2 suggests that oxygenation should be monitored constantly during RMs, as changes in SpO2 are promptly reflected by changes in rSO2. Maneuvers that decrease systemic oxygen saturation expose the patient to the risk of cerebral hypoxia. As expected, rSO2 was also correlated to PaCO2 and MAP values, as both can be surrogates of cerebral blood flow and volume.
Limitations
Several limitations of this study need to be mentioned. First, this is a single-center study with a small number of patients, especially in each subgroup; second, as this is an observational study, we only analyzed the rescue therapies currently adopted in our practice. For example, the type of RM adopted and the dose used for iNO test—although not completely established in the literature [63]—reflect our own policies.
Data on ECMO are missing as we opted to use ECCO2R to provide protective ventilation [64], with less need of external blood flow—minimizing the potential risks.
In this context, after ECCO2R PEEP from T0 and T1 was reduced. However, PEEP reduction was on average 1.5 cmH2O, clinically not significant and likely not affecting the results.
Moreover, we only evaluated the early effects of ventilator strategies on cerebral and systemic hemodynamics. Although we are aware that some rescue therapies might require time of application to produce a clinically relevant effect [65], we decided to focus on the early phase in order to evaluate the possible acute effects on cerebral oxygenation. As suggested by Chiumello et al. [66], PEEP variations exert their effects on oxygenation after a precise time lag, but in individual patients the change of oxygenation-related variables after PEEP modifications observed after 5′ can predict the changes observed after 60′.
Further, more specific data on physiological parameters including invasive neuro, respiratory, and hemodynamic monitoring would have been useful to assess changes in these parameters consequent to the application of rescue therapies. In particular, we assessed noninvasive ICP using TCD, using a formula which has been previously validated in experimental settings and brain-injured patients [67–69], but not in the general ICU population. However, although this method presents some limitations [70] in terms of accuracy, it has shown to be reliable to exclude intracranial hypertension and to assess the trajectory of ICP [71], making it very suitable in the context of our study. Also, we did not study patients’ autoregulatory status, which can also influence the rSO2 response to hypoxia. Finally, our population represents a specific subgroup with peculiar characteristics, and our results may thus not be generalizable to other clinical settings.
Conclusions
In our population of COVID-19 patients with severe ARDS, ample physiologic variability was observed, with different early effects of rescue therapies on cerebral and systemic oxygenation. Treatment must be personalized and should take in consideration both pulmonary and cerebral needs. Strict use of neuromonitoring is warranted even in patients who are not primarily brain-injured, in order to prevent and ensure early detection of neurological complications. Future multicenter studies are warranted to confirm our results.
Supplementary Information
Additional file 1. STROBE checklist, and additional analysis.
Acknowledgements
The authors would like to acknowledge the following as Collaborators to be searchable on PubMed: Elena Ciaravolo, Department of Surgical Sciences and Integrated Diagnostics (DISC), University of Genoa, Italy; Fabio Tarantino, Ospedale Policlinico San Martino, IRCCS for Oncology and Neuroscience, Genoa, Italy; Marco Sottano, Ospedale Policlinico San Martino, IRCCS for Oncology and Neuroscience, Genoa, Italy; Francesco Marramao, Ospedale Policlinico San Martino, IRCCS for Oncology and Neuroscience, Genoa, Italy; Angelo Gratarola, Ospedale Policlinico San Martino, IRCCS for Oncology and Neuroscience, Genoa, Italy; Paolo Frisoni, Ospedale Policlinico San Martino, IRCCS for Oncology and Neuroscience, Genoa, Italy; Chiara Berri, Ospedale Policlinico San Martino, IRCCS for Oncology and Neuroscience, Genoa, Italy; Chiara Dentone, Infectious Diseases Unit, Ospedale Policlinico San Martino, Genoa, Italy; Lucia Taramasso, Infectious Diseases Unit, Ospedale Policlinico San Martino, Genoa, Italy; Laura Magnasco, Infectious Diseases Unit, Ospedale Policlinico San Martino, Genoa, Italy; Gianluigi Zona, Department of Neurosurgery, Ospedale Policlinico San Martino, Genoa, Italy; Pietro Fiaschi, Department of Neurosurgery, Ospedale Policlinico San Martino, Genoa, Italy; Pasquale Anania, Department of Neurosurgery, Ospedale Policlinico San Martino, Genoa, Italy.
Abbreviations
- ARDS
Acute respiratory distress syndrome
- cHbi
The sum of ΔO2Hbi and ΔHHbi values
- COVID-19
Coronavirus disease-2019
- CPP
Cerebral perfusion pressure
- CRRT
Continuous renal replacement therapy
- Crs
Respiratory system compliance
- CVVHD
Continuous venovenous hemodialysis
- ECCO2R
Extracorporeal carbon dioxide removal
- ECMO
Extracorporeal membrane oxygenation
- FiO2
Fraction of inspired oxygen
- FVd
Diastolic flow velocity
- FVm
Mean flow velocity
- FVs
Systolic flow velocity
- Hb
Hemoglobin
- HHbi
Index associated with changes in the deoxygenated component of Hb
- iNO
Inhaled nitric oxide
- MAP
Mean arterial pressure
- MCA
Middle cerebral artery
- nCPP
Noninvasive cerebral perfusion pressure
- nICP
Noninvasive intracranial pressure
- O2Hbi
Oxygenated component of Hb
- PaCO2
Partial pressure of carbon dioxide
- PaO2
Partial pressure of oxygen
- PEEP
Positive end-expiratory pressure
- Pplat
Plateau pressure
- RMs
Recruitment maneuvers
- RR
Respiratory rate
- rSO2
Total value of regional cerebral oxygen saturation
- SARS-CoV-2
Severe acute respiratory syndrome coronavirus-2
- VT
Tidal volume
Authors' contributions
CR, BM and PP designed and led the study, performed the statistical analysis, and drafted the first version of the manuscript. All the authors participated in data interpretation, collection, and editing of the first version of the manuscript. All authors approved the final version of the manuscript.
Funding
None.
Availability of data and materials
Data are fully available upon request from the corresponding author.
Declarations
Ethics approval and consent to participate
The study protocol was approved by the ethics review board (Comitato Etico Regione Liguria, protocol n. CER Liguria: 23/2020).
Consent for publication
Local ethical approval was obtained, and consent form was obtained from next of kin, as patients were unconscious at the time of inclusion.
Competing interests
Dr. Bassetti reports personal fees and other from Angelini, personal fees and other from AstraZeneca, other from Bayer, personal fees and other from Cubist, personal fees and other from Pfizer, personal fees and other from Menarini, personal fees and other from MSD, other from Nabriva, other from Paratek, other from Roche, other from Shionogi, other from Tetraphase, other from The Medicine Company, personal fees and other from Astellas Pharma Inc., personal fees from Gilead Sciences, personal fees from Teva, personal fees from Novartis, grants from Ranbaxy, personal fees from Correvio, personal fees from Molteni, personal fees from Thermo Fisher, outside the submitted work. Dr. Giacobbe reports personal fees from Stepstone Pharma GmbH, personal fees from MSD Italia, personal fees from Correvio Italia, outside the submitted work. Dr. Matta reports personal fees from Masimo.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Lorenzo Ball and Denise Battaglini have contributed equally to this work
Contributor Information
Chiara Robba, Email: kiarobba@gmail.com.
Lorenzo Ball, Email: lorenzo.loryball@gmail.com.
Denise Battaglini, Email: battaglini.denise@gmail.com.
Danilo Cardim, Email: danilo.cardim@gmail.com.
Emanuela Moncalvo, Email: manulb@virgilio.it.
Iole Brunetti, Email: brunettimed@gmail.com.
Matteo Bassetti, Email: matteo.bassetti@hsanmartino.it.
Daniele R. Giacobbe, Email: daniele.roberto.giacobbe@gmail.com
Antonio Vena, Email: anton.vena@gmail.com.
Nicolò Patroniti, Email: npatroniti@gmail.com.
Patricia R. M. Rocco, Email: prmrocco@gmail.com
Basil F. Matta, Email: basil.matta@addenbrookes.nhs.uk
Paolo Pelosi, Email: ppelosi@hotmail.com.
collaborators, Email: fabiotara76@gmail.com.
collaborators:
Pasquale Anania, Chiara Berri, Elena Ciaravolo, Chiara Dentone, Pietro Fiaschi, Paolo Frisoni, Angelo Gratarola, Laura Magnasco, Francesco Marramao, Marco Sottano, Lucia Taramasso, Fabio Tarantino, and Gianluigi Zona
References
- 1.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy. JAMA. 2020;323:1545. doi: 10.1001/jama.2020.4031. [DOI] [PubMed] [Google Scholar]
- 3.Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46:846–848. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Robba C, Battaglini D, Pelosi P, Rocco RMP. Multiple organ dysfunction in SARS-CoV-2: MODS-CoV-2. Expert Rev Respir Med. 2020;14:865–868. doi: 10.1080/17476348.2020.1778470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 Patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323:1574. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Robba C, Battaglini D, Ball L, Patroniti N, Loconte M, Brunetti I, et al. Distinct phenotypes require distinct respiratory management strategies in severe COVID-19. Respir Physiol Neurobiol. 2020;279:103455. doi: 10.1016/j.resp.2020.103455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gattinoni L, Coppola S, Cressoni M, Busana M, Rossi S, Chiumello D. COVID-19 does not lead to a “typical” acute respiratory distress syndrome. Am J Respir Crit Care Med. 2020;201:1299–1300. doi: 10.1164/rccm.202003-0817LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gattinoni L, Chiumello D, Caironi P, Busana M, Romitti F, Brazzi L, et al. COVID-19 pneumonia: different respiratory treatments for different phenotypes? Intensive Care Med. 2020;46:1099–1102. doi: 10.1007/s00134-020-06033-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marini JJ, Gattinoni L. Management of COVID-19 respiratory distress. JAMA. 2020;323:2329. doi: 10.1001/jama.2020.6825. [DOI] [PubMed] [Google Scholar]
- 11.Grasselli G, Tonetti T, Protti A, Langer T, Girardis M, Bellani G, et al. Pathophysiology of COVID-19-associated acute respiratory distress syndrome: a multicentre prospective observational study. Lancet Respir Med. 2020;S2213–2600:30370–30372. doi: 10.1016/S2213-2600(20)30370-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fan E, Beitler JR, Brochard L, Calfee CS, Ferguson ND, Slutsky AS, et al. COVID-19-associated acute respiratory distress syndrome: is a different approach to management warranted? Lancet Respir Med. 2020;8:816–821. doi: 10.1016/S2213-2600(20)30304-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Husain-Syed F, Birk H-W, Wilhelm J, Ronco C, Ranieri VM, Karle B, et al. Extracorporeal carbon dioxide removal using a renal replacement therapy platform to enhance lung-protective ventilation in hypercapnic patients with coronavirus disease 2019-associated acute respiratory distress syndrome. Front Med. 2020;7:598379. doi: 10.3389/fmed.2020.598379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lotz C, Muellenbach RM, Meybohm P, Mutlak H, Lepper PM, Rolfes C, et al. Effects of inhaled nitric oxide in COVID‐19–induced ARDS—Is it worthwhile? Acta Anaesthesiol Scand. 2020;aas.13757. [DOI] [PubMed]
- 15.Li M, Gu S-C, Wu X-J, Xia J-G, Zhang Y, Zhan Q-Y. Extracorporeal membrane oxygenation support in 2019 novel coronavirus disease. Chin Med J (Engl) 2020;133:1115–1117. doi: 10.1097/CM9.0000000000000778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heinsar S, Peek GJ, Fraser JF. ECMO during the COVID-19 pandemic: When is it justified? Crit Care. 2020;24:650. doi: 10.1186/s13054-020-03386-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Battaglini D, Santori G, Chandraptham K, Iannuzzi F, Bastianello M, Tarantino F, et al. Neurological complications and noninvasive multimodal neuromonitoring in critically ill mechanically ventilated COVID-19 patients. Front Neurol. 2020;11:602114. doi: 10.3389/fneur.2020.602114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Helms J, Kremer S, Merdji H, Clere-Jehl R, Schenck M, Kummerlen C, et al. Neurologic features in severe SARS-CoV-2 infection. N Engl J Med. 2020;382:2268–2270. doi: 10.1056/NEJMc2008597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Battaglini D, Brunetti I, Anania P, Fiaschi P, Zona G, Ball L, et al. Neurological manifestations of severe SARS-CoV-2 infection: potential mechanisms and implications of individualized mechanical ventilation settings. Front Neurol. 2020;11:845. doi: 10.3389/fneur.2020.00845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Robba C, Poole D, McNett M, Asehnoune K, Bösel J, Bruder N, et al. Mechanical ventilation in patients with acute brain injury: recommendations of the European Society of Intensive Care Medicine consensus. Intensive Care Med. 2020;46:2397–2410. doi: 10.1007/s00134-020-06283-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Frisvold SK, Robba C, Guérin C. What respiratory targets should be recommended in patients with brain injury and respiratory failure? Intensive Care Med. 2019;45:683–686. doi: 10.1007/s00134-019-05556-7. [DOI] [PubMed] [Google Scholar]
- 22.Corradi F, Robba C, Tavazzi G, Via G. Combined lung and brain ultrasonography for an individualized “brain-protective ventilation strategy” in neurocritical care patients with challenging ventilation needs. Crit Ultrasound J. 2018;10:24. doi: 10.1186/s13089-018-0105-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335:806–808. doi: 10.1136/bmj.39335.541782.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ranieri V, Rubenfeld G, Thompson B, Ferguson N, Caldwell E, Fan E, et al. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307:2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 25.World Health Organization. Clinical management of severe acute respiratory infection when novel coronavirus (2019-nCoV) infection is suspected: interim guidance, 28 January 2020 [Internet]. 2020. https://apps.who.int/iris/handle/10665/330893.
- 26.Combes A, Hajage D, Capellier G, Demoule A, Lavoué S, Guervilly C, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med. 2018;378:1965–1975. doi: 10.1056/NEJMoa1800385. [DOI] [PubMed] [Google Scholar]
- 27.Chen L, Liu P, Gao H, Sun B, Chao D, Wang F, et al. Inhalation of nitric oxide in the treatment of severe acute respiratory syndrome: a rescue trial in Beijing. Clin Infect Dis. 2004;39:1531–1535. doi: 10.1086/425357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Robba C, Bragazzi NL, Bertuccio A, Cardim D, Donnelly J, Sekhon M, et al. Effects of prone position and positive end-expiratory pressure on noninvasive estimators of ICP. J Neurosurg Anesthesiol. 2017;29:243–250. doi: 10.1097/ANA.0000000000000295. [DOI] [PubMed] [Google Scholar]
- 29.Robba C, Cardim D, Donnelly J, Bertuccio A, Bacigaluppi S, Bragazzi N, et al. Effects of pneumoperitoneum and Trendelenburg position on intracranial pressure assessed using different non-invasive methods. Br J Anaesth. 2016;117:783–791. doi: 10.1093/bja/aew356. [DOI] [PubMed] [Google Scholar]
- 30.Rasulo FA, Bertuetti R, Robba C, Lusenti F, Cantoni A, Bernini M, et al. The accuracy of transcranial Doppler in excluding intracranial hypertension following acute brain injury: a multicenter prospective pilot study. Crit Care. 2017;21:44. doi: 10.1186/s13054-017-1632-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mauri T, Spinelli E, Scotti E, Colussi G, Basile MC, Crotti S, et al. Potential for lung recruitment and ventilation-perfusion mismatch in patients with the acute respiratory distress syndrome from coronavirus disease 2019*. Crit Care Med. 2020;48:1129–1134. doi: 10.1097/CCM.0000000000004386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mauri T, Eronia N, Turrini C, Battistini M, Grasselli G, Rona R, et al. Bedside assessment of the effects of positive end-expiratory pressure on lung inflation and recruitment by the helium dilution technique and electrical impedance tomography. Intensive Care Med. 2016;42:1576–1587. doi: 10.1007/s00134-016-4467-4. [DOI] [PubMed] [Google Scholar]
- 33.Mauri T, Bellani G, Confalonieri A, Tagliabue P, Turella M, Coppadoro A, et al. Topographic distribution of tidal ventilation in acute respiratory distress syndrome. Crit Care Med. 2013;41:1664–1673. doi: 10.1097/CCM.0b013e318287f6e7. [DOI] [PubMed] [Google Scholar]
- 34.Bland JM, Altman DG. Statistics notes: Calculating correlation coefficients with repeated observations: part 2—correlation between subjects. BMJ. 1995;310:633–633. doi: 10.1136/bmj.310.6980.633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bakdash JZ, Marusich LR. Repeated measures correlation. Front Psychol. 2017;66:8. doi: 10.3389/fpsyg.2017.00456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pun BT, Badenes R, Heras La Calle G, Orun OM, Chen W, Raman R, et al. Prevalence and risk factors for delirium in critically ill patients with COVID-19 (COVID-D): a multicentre cohort study. Lancet Respir Med. 2021;66:S2213. doi: 10.1016/S2213-2600(20)30552-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hodgson C, Carteaux G, Tuxen DV, R Davies AR, Pellegrino V, Capellier G, et al. Hypoxaemic rescue therapies in acute respiratory distress syndrome: Why, when, what and which one? Injury. 2013;44(12):1700–9. [DOI] [PubMed]
- 38.Guérin C, Reignier J, Richard J-C, Beuret P, Gacouin A, Boulain T, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368:2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 39.Ball L, Serpa Neto A, Trifiletti V, Mandelli M, Firpo I, Robba C, et al. Effects of higher PEEP and recruitment manoeuvres on mortality in patients with ARDS: a systematic review, meta-analysis, meta-regression and trial sequential analysis of randomized controlled trials. Intensive Care Med Exp. 2020;8:39. doi: 10.1186/s40635-020-00322-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Grieco DL, Bongiovanni F, Chen L, Menga LS, Cutuli SL, Pintaudi G, et al. Respiratory physiology of COVID-19-induced respiratory failure compared to ARDS of other etiologies. Crit Care. 2020;24:529. doi: 10.1186/s13054-020-03253-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Seethala RR, Frakes MA, Cocchi MN, Cohen JE, Dargin J, Friedman F, et al. Feasibility and safety of prone position transport for severe hypoxemic respiratory failure due to coronavirus disease 2019. Crit Care Explor. 2020;2:e0293. doi: 10.1097/CCE.0000000000000293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Maeda A, Nabeya D, Nagano H, Yagi N, Miyagi T, Kishaba T. Prone position ventilation and femoro-femoral veno-venous extracorporeal membrane oxygenation for COVID-19 treatment. Respirol Case Rep. 2021;9:66. doi: 10.1002/rcr2.700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bagate F, Tuffet S, Masi P, Perier F, Razazi K, de Prost N, et al. Rescue therapy with inhaled nitric oxide and almitrine in COVID-19 patients with severe acute respiratory distress syndrome. Ann Intensive Care. 2020;10:151. doi: 10.1186/s13613-020-00769-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tavazzi G, Marco P, Mongodi S, Dammassa V, Romito G, Mojoli F. Inhaled nitric oxide in patients admitted to intensive care unit with COVID-19 pneumonia. Crit Care. 2020;24:508. doi: 10.1186/s13054-020-03222-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Thomson RJ, Hunter J, Dutton J, Schneider J, Khosravi M, Casement A, et al. Clinical characteristics and outcomes of critically ill patients with COVID-19 admitted to an intensive care unit in London: A prospective observational cohort study. PLoS One. 2020;15:e0243710. doi: 10.1371/journal.pone.0243710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yu H, Sun T, Feng J. Complications and pathophysiology of COVID-19 in the nervous system. Front Neurol. 2020;11:573421. doi: 10.3389/fneur.2020.573421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Siow I, Lee KS, Zhang JJY, Saffari SE, Ng A, Young B. Stroke as a neurological complication of COVID-19: a systematic review and meta-analysis of incidence, outcomes and predictors. J Stroke Cerebrovasc Dis. 2021;30:105549. doi: 10.1016/j.jstrokecerebrovasdis.2020.105549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Robba C, Bonatti G, Battaglini D, Rocco PRM, Pelosi P. Mechanical ventilation in patients with acute ischaemic stroke: from pathophysiology to clinical practice. Crit Care. 2019;23:388. doi: 10.1186/s13054-019-2662-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gritti P, Lanterna LA, Re M, Martchenko S, Olivotto P, Brembilla C, et al. The use of inhaled nitric oxide and prone position in an ARDS patient with severe traumatic brain injury during spine stabilization. J Anesth. 2013;27:293–297. doi: 10.1007/s00540-012-1495-2. [DOI] [PubMed] [Google Scholar]
- 50.Cornejo R, Romero C, Ugalde D, Bustos P, Diaz G, Galvez R, et al. High-volume hemofiltration and prone ventilation in subarachnoid hemorrhage complicated by severe acute respiratory distress syndrome and refractory septic shock. Rev Bras Ter Intensiva. 2014;26:193–199. doi: 10.5935/0103-507X.20140028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Munoz-Bendix C, Beseoglu K, Kram R. Extracorporeal decarboxylation in patients with severe traumatic brain injury and ARDS enables effective control of intracranial pressure. Crit Care. 2015;19:381. doi: 10.1186/s13054-015-1088-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nekludov M, Bellander B-M, Mure M. Oxygenation and cerebral perfusion pressure improved in the prone position. Acta Anaesthesiol Scand. 2006;50:932–936. doi: 10.1111/j.1399-6576.2006.01099.x. [DOI] [PubMed] [Google Scholar]
- 53.Nemer SN, Caldeira JB, Azeredo LM, Garcia JM, Silva RT, Prado D, et al. Alveolar recruitment maneuver in patients with subarachnoid hemorrhage and acute respiratory distress syndrome: a comparison of 2 approaches. J Crit Care. 2011;26:22–27. doi: 10.1016/j.jcrc.2010.04.015. [DOI] [PubMed] [Google Scholar]
- 54.Reinprecht A, Greher M, Wolfsberger S, Dietrich W, Illievich UM, Gruber A. Prone position in subarachnoid hemorrhage patients with acute respiratory distress syndrome: Effects on cerebral tissue oxygenation and intracranial pressure*. Crit Care Med. 2003;31:1831–1838. doi: 10.1097/01.CCM.0000063453.93855.0A. [DOI] [PubMed] [Google Scholar]
- 55.Della Torre V, Badenes R, Corradi F, Racca F, Lavinio A, Matta B, et al. Acute respiratory distress syndrome in traumatic brain injury: How do we manage it? J Thorac Dis. 2017;9:5368–5381. doi: 10.21037/jtd.2017.11.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Robba C, Hemmes SNT, Serpa Neto A, Bluth T, Canet J, Hiesmayr M, et al. Intraoperative ventilator settings and their association with postoperative pulmonary complications in neurosurgical patients: post-hoc analysis of LAS VEGAS study. BMC Anesthesiol. 2020;20:73. doi: 10.1186/s12871-020-00988-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Picetti E, Pelosi P, Taccone FS, Citerio G, Mancebo J, Robba C. VENTILatOry strategies in patients with severe traumatic brain injury: the VENTILO Survey of the European Society of Intensive Care Medicine (ESICM) Crit Care. 2020;24:158. doi: 10.1186/s13054-020-02875-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lumb AB, Slinger P. Hypoxic pulmonary vasoconstriction. Anesthesiology. 2015;122:932–946. doi: 10.1097/ALN.0000000000000569. [DOI] [PubMed] [Google Scholar]
- 59.Johnston AJ, Steiner LA, Coles JP, Chatfield DA, Fryer TD, Smielewski P, et al. Effect of cerebral perfusion pressure augmentation on regional oxygenation and metabolism after head injury*. Crit Care Med. 2005;33:189–195. doi: 10.1097/01.CCM.0000149837.09225.BD. [DOI] [PubMed] [Google Scholar]
- 60.Oddo M, Nduom E, Frangos S, MacKenzie L, Chen I, Maloney-Wilensky E, et al. Acute lung injury is an independent risk factor for brain hypoxia after severe traumatic brain injury. Neurosurgery. 2010;67:338–344. doi: 10.1227/01.NEU.0000371979.48809.D9. [DOI] [PubMed] [Google Scholar]
- 61.Menon DK, Coles JP, Gupta AK, Fryer TD, Smielewski P, Chatfield DA, et al. Diffusion limited oxygen delivery following head injury. Crit Care Med. 2004;32:1384–1390. doi: 10.1097/01.CCM.0000127777.16609.08. [DOI] [PubMed] [Google Scholar]
- 62.Robba C, Asgari S, Gupta A, Badenes R, Sekhon M, Bequiri E, et al. Lung injury is a predictor of cerebral hypoxia and mortality in traumatic brain injury. Front Neurol. 2020;11:771. doi: 10.3389/fneur.2020.00771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Germann P, Braschi A, DellaRocca G, Dinh-Xuan AT, Falke K, Frostell C, et al. Inhaled nitric oxide therapy in adults: European expert recommendations. Intensive Care Med. 2005;31(8):1029–1041. doi: 10.1007/s00134-005-2675-4. [DOI] [PubMed] [Google Scholar]
- 64.Goursaud S, Valette X, Dupeyrat J, Daubin C, du Cheyron D. Ultraprotective ventilation allowed by extracorporeal CO2 removal improves the right ventricular function in acute respiratory distress syndrome patients: a quasi-experimental pilot study. Ann Intensive Care. 2021;11(1):3. doi: 10.1186/s13613-020-00784-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Guérin C, Albert RK, Beitler J, Gattinoni L, Jaber S, Marini JJ, et al. Prone position in ARDS patients: why, when, how and for whom. Intensive Care Med. 2020;46:2385–2396. doi: 10.1007/s00134-020-06306-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chiumello D, Coppola S, Froio S, Mietto C, Brazzi L, Carlesso E, et al. Time to reach a new steady state after changes of positive end expiratory pressure. Intensive Care Med. 2013;39:1377–1385. doi: 10.1007/s00134-013-2969-x. [DOI] [PubMed] [Google Scholar]
- 67.Cardim D, Robba C, Donnelly J, Bohdanowicz M, Schmidt B, Damian M, et al. Prospective study on noninvasive assessment of intracranial pressure in traumatic brain-injured patients: comparison of four methods. J Neurotrauma. 2016;33:792–802. doi: 10.1089/neu.2015.4134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Czosnyka M, Matta BF, Smielewski P, Kirkpatrick PJ, Pickard JD. Cerebral perfusion pressure in head-injured patients: a noninvasive assessment using transcranial Doppler ultrasonography. J Neurosurg. 1998;88:802–808. doi: 10.3171/jns.1998.88.5.0802. [DOI] [PubMed] [Google Scholar]
- 69.Robba C, Donnelly J, Bertuetti R, Cardim D, Sekhon MS, Aries M, et al. Doppler non-invasive monitoring of ICP in an animal model of acute intracranial hypertension. Neurocrit Care. 2015;23:419–426. doi: 10.1007/s12028-015-0163-4. [DOI] [PubMed] [Google Scholar]
- 70.Robba C, Goffi A, Geeraerts T, Cardim D, Via G, Czosnyka M, et al. Brain ultrasonography: methodology, basic and advanced principles and clinical applications. A narrative review. Intensive Care Med. 2019;45:913–927. doi: 10.1007/s00134-019-05610-4. [DOI] [PubMed] [Google Scholar]
- 71.Rasulo FA, Togni T, Romagnoli S. Essential noninvasive multimodality neuromonitoring for the critically ill patient. Crit Care. 2020;24:100. doi: 10.1186/s13054-020-2781-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hypoxaemic rescue therapies in acute respiratory distress syndrome: Why, when, what and which one? [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. STROBE checklist, and additional analysis.
Data Availability Statement
Data are fully available upon request from the corresponding author.



