Abstract
Trigeminal neuralgia is a chronic pain condition affecting one or more distributions of the trigeminal nerve. Patients with this condition experience short, sharp, shooting pain attacks, which can progress to longer, more frequent durations. The pain is often difficult to control. We report of a man who was admitted with severe neuralgia of the third division of the trigeminal nerve. Talking and any oral intake triggered a severe agonising pain. The latter made the regular oral intake of analgesia challenging. The pain was temporarily controlled with frequent local anaesthesia (LA). Dental core trainees were performing regular inferior alveolar nerve blocks which significantly improved patients’ condition allowing him to communicate and have oral intake. Subsequently, a catheter was placed allowing for a continuous anaesthesia. The connecting tube of the cannula was then used by nursing staff to administer LA providing pain relief without the need of repeated intraoral injections.
Keywords: dentistry and oral medicine, mouth, oral and maxillofacial surgery, head and neck surgery
Background
Trigeminal neuralgia (TN) occurs when the trigeminal nerve’s function is disrupted which may be due to pressure from a local blood vessel, a tumour or secondary to an underlying condition involving the nerve.2 The pain can be so intense that it effects normal functioning and can have a significant impact on quality of life. The location of the pain is dependent on which branch of the trigeminal nerve is affected. Eighty per cent of patients can be treated with pharmaceutical methods alone,1 with the prescription of sodium channel blockers combined with lamotrigine, baclofen, pregabalin or gabapentin if required.2 If the medications are ineffective or cannot reach therapeutic dosage due to adverse events then surgical intervention is considered.2 3 Microvascular decompression is used for patients with a proven neurovascular conflict. The surgery usually provides immediate pain relief post operatively and has the longest period of pain-free relief compared with other methods.1 Ablative methods that deliberately disrupt the nerve function include glycerol blockade, balloon compression or radiofrequency thermocoagulation.3
Our patient suffered from a severe case of TN affecting the mandibular division that required admittance and regular local anaesthesia (LA) to suppress the agonising pain. Dental core trainees (DCTs) are often the first members of the maxillofacial team to see these patients in accident and emergency (A&E) or look after them on the wards. DCTs are trained with the intraoral approach for LA of the inferior alveolar nerve (IAN) and administration of mandibular nerve blocks compared with other junior staff in the front line. We introduce a feasible method for continuous mandibular nerve block for regular administration of LA. This allows for the nerve block to be maintained for a longer period of time and LA can easily be administered by the nursing staff providing continuous pain relief.
Case presentation
An 84-year-old man was initially seen in the maxillofacial department in 2014 for an onset of right-sided lower jaw pain. He was suffering from sharp, shooting, severe pain attacks which were triggered by touch such as shaving. An IAN block was administered for diagnostic purposes and had the desired effect of relieving the pain. A diagnostic MRI scan did not show any mass lesions or underlying cause. There were only age-related multiple hyperintensities within the subcortical periventricular and deep white matter that may reflect severe small vessel disease. The patient was started on carbamazepine 200 mg three times a day and gabapentin to control his symptoms. Cryotherapy was considered; however, the pain went into remission under the medication for a significant period of time. The patient returned 6 years later to the hospital in August 2020 when the pain emerged more intensely hindering him from any oral intake and speaking.
Differential diagnosis
The patients’ MRI did not show any neurovascular conflict; however, MRI scans have not proven to be sufficient in establishing or excluding this.1 The man was diagnosed with the atypical form of TN affecting the mandibular division due to the continuous background pain between the exacerbations.1
Treatment
On the ward, the patient required continuous LA to suppress the agonising pain and to be able to function normally while awaiting radiofrequency ablation of the third division of trigeminal nerve. The maxillofacial team had to frequently administer IAN blocks using intraoral lidocaine and bupivacaine injections. The nerve blocks would only last for a limited period of time before the pain returned. Administering repeated intraoral nerve blocks was in itself a painful undertaking for the patient. Hence, a conventional intravenous cannula (IVC) was placed for LA to the mandibular division of the trigeminal nerve. The catheter remained in situ allowing us and the nursing staff to administer the local anaesthetics regularly within the limits of maximal dosage. This method prevented the patient having repeated intraoral injections.
We used an IVC of 17 gauge which comes with a needle length of 45 mm with an adequate tube length once the needle is removed to reach the mandibular foramen. The catheter is inserted in the same anatomical position as the IAN block (figure 1). The IVC is placed between the coronoid notch and the pterygomandibular raphe and the needle is removed.4 The cannula wings were secured to the buccal mucosa with 3.0 silk stitches (Ethicon) and used to administer anaesthesia through the port (figure 2). The method can be adapted for patients with limited mouth opening using the Vazirani-Akinosi technique.5
Figure 1.
Photo showing the final inserted position of the cannula.
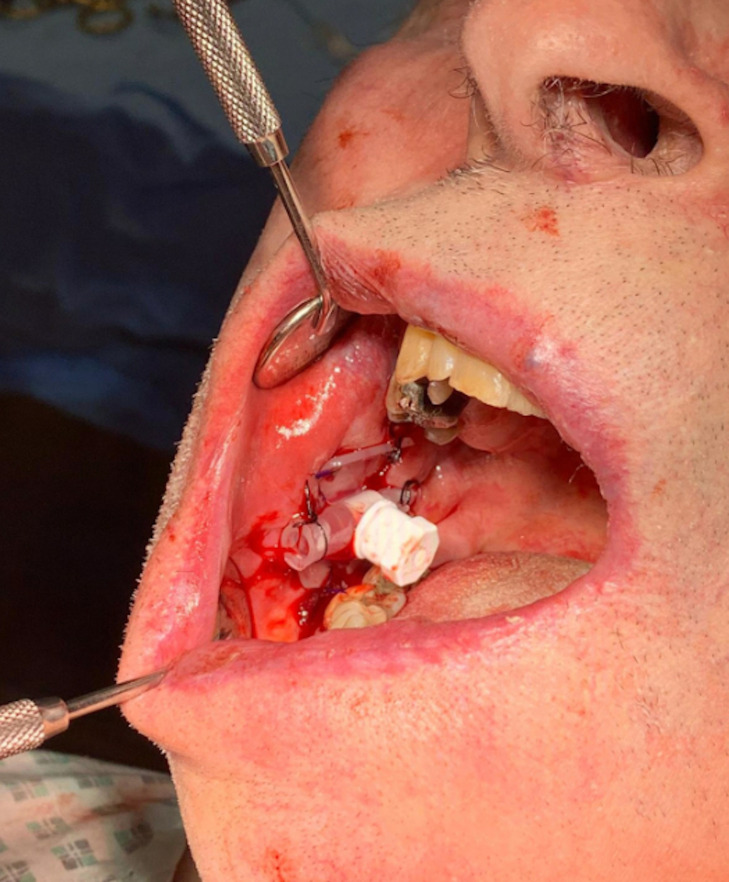
Figure 2.
Placement of the cannula with a line attached to the port allowing easy anaesthesia delivery.
Outcome and follow-up
We bridged the time before RFA of the trigeminal nerve was performed using the above method. This allowed for pain-free episodes where the patient could communicate and have oral intake painlessly including oral analgesia. The patient was discharged from our care after RFA and increasing the dose of carbamazepine deemed him pain free. However, he remained under the care of the medical team and sadly he passed away in hospital shortly after due to his underlying comorbidities.
Discussion
The use of an intraoral catheter such as IVC for a continuous IAN block is a feasible solution with an immediate effect in patients with severe and agonising pain. In our case, it helped the patient in oral intake and he was able to communicate without triggering the agonising neuralgic pain.6 We were, therefore, able to bridge the gap between admission and a definite treatment. The method is feasible when other methods of analgesia are not possible or contraindicated.
There are not many reported cases of continuous intraoral catheter-based LA. Hammond et al report of a spinal needle used as an intraoral catheter for pain control in a patient with a fractured mandible.6 In our reported case and in the acute setting, the most accessible catheter was a conventional IVC of 17 gauge and 45 mm needle length. IAN blocks are routinely given with a 25 gauge conventional dental needle with a penetration depth of 25–30 mm from the mucosal surface to reach the mandibular foramen.5 If IVC is being used for a continuous LA of IAN a 22G needle with a 25 mm length would be more feasible. The disadvantage of using a conventional IVC in dentate patients can be the injection port which may interfere with the occlusion (figure 1). The spinal needle used by Hammond et al is however longer and would protrude from the mouth and it may be more difficult to secure intraorally due to the lack of wings. Alternatively the catheter for IAN block can be placed from an extra-oral approach however this method may not be feasible in the acute setting.6
The potential risks of catheter based continuous nerve block may include wire tract infection, failure to anaesthetise the nerve and neuropraxia due to mal-positioning.6 Most maxillofacial doctors are dentally trained and familiar with intraoral approach for mandibular nerve block. IVCs are readily available and long acting local anaesthetics can be administered through the connecting port catheter by medical staff. However, the maximum dosage of the local anaesthetic used has not to be exceeded and the clinicians need to be aware of interactions of the local anaesthetics used with patient’s comorbidities.
Learning points.
Intraoral catheter-based continuous inferior alveolar nerve block is a temporary and feasible method for continuous pain control in acute setting.
This technique allows for a non-invasive regular administration of anaesthesia by medical staff.
The maximal dosage and patient comorbidities have to be respected.
Footnotes
Contributors: Case discussed between both authors. Written and drafted by HKS and edited and finalised by FB.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Silva M, Ouanounou A. Trigeminal neuralgia: etiology, diagnosis, and treatment. SN Compr Clin Med 2020;2:1585–92. 10.1007/s42399-020-00415-9 [DOI] [Google Scholar]
- 2.Turton M, Malan-Roux P. Trigeminal neuralgia: case report and literature review. SDS 2019;2019. 10.20517/2573-0002.2019.08 [DOI] [Google Scholar]
- 3.Obermann M. Treatment options in trigeminal neuralgia. Ther Adv Neurol Disord 2010;3:107–15. 10.1177/1756285609359317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khalil H. A basic review on the inferior alveolar nerve block techniques. Anesth Essays Res 2014;8:3–8. 10.4103/0259-1162.128891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reed KL, Malamed SF, Fonner AM. Local anesthesia Part 2: technical considerations. Anesth Prog 2012;59:127–37. 10.2344/0003-3006-59.3.127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hammond D, Olaore S, Salker M, et al. Catheter-based local analgesia for the fractured mandible in a patient with a history of hereditary angioedema. J Surg Case Rep 2019;2019. 10.1093/jscr/rjz126 [DOI] [PMC free article] [PubMed] [Google Scholar]