Abstract
In this article we present the theoretical and empirical bases of distress tolerance research. Although distress tolerance offers a promising lens through which to better understand various psychological symptoms and disorders, further theoretical development and empirical inquiry is needed to promote our understanding of the construct. Overall, a number of questions regarding its theoretical conceptualization and measurement, associations with related constructs and psychopathology, and role(s) in therapeutic change and intervention remain unanswered. Directions for future research are discussed to stimulate further empirical study on this theoretically and clinically promising topic.
Keywords: distress tolerance, psychopathology, vulnerability, mechanism, assessment
Distress tolerance has been a continued focus of interest for clinical scientists and practitioners (Zvolensky, Bernstein, & Vujanovic, in press). Extant distress tolerance research has involved various conceptual and measurement models of the construct. Growing research interest in distress tolerance has been paralleled by the proliferation of psychosocial interventions for psychological disorders designed to promote tolerance for distress. The present article aims to present scientific information on the nature of distress tolerance and its relations to psychopathology and to highlight future directions for research on the topic.
Theoretical Framework
Two broad, conceptually distinct forms of distress tolerance have been formulated (Leyro, Zvolensky, & Bernstein, 2010). Specifically, distress tolerance has been referred to as (a) the perceived capacity to withstand negative emotional and/or other aversive states (e.g., physical discomfort) and (b) the behavioral act of withstanding distressing internal states elicited by some type of stressor. Accordingly, there have been two methodological literatures related to distress tolerance. Namely, the self-report literature has focused on the generalized perceived capacity to withstand aversive states, whereas the non-self-report (sometimes termed biobehavioral) literature has focused on the behavioral capacity to tolerate acute aversive states. There are numerous assessment tactics in each literature; in the current article, we present only a number of illustrative examples (see Leyro et al., 2010, for a comprehensive review and the psychometrics of this methodological literature).
Although nested conceptually within a broader network of risk and protective processes, distress tolerance is theorized to be related to, though conceptually distinct from, other variables (e.g., avoidant coping, anxiety sensitivity, emotion regulation, experiential avoidance; Leyro et al., 2010). Individuals with lower levels of distress tolerance may be prone to maladaptively respond to distress and distress-eliciting contexts. As a result, individuals with lower distress tolerance may attempt to avoid negative emotions and/or related aversive states. In contrast, persons with higher levels of distress tolerance may be more able to adaptively respond to distress or distress-eliciting contexts. Theoretically, distress tolerance may affect, and be affected by, a variety of processes involved in self-regulation, including attention, cognitive appraisals of distressing emotional and physical states, and emotional as well as behavioral responses to distress. For example, individual differences in the experience of emotions—both their strength and their frequency—may possibly influence the nature of distress tolerance.
Presently, there is no overarching integrative model of distress tolerance. Most distress tolerance perspectives are informed by personality, self-regulation, and coping literatures. A number of authors have described possible latent structural models that attempt to integrate work on this and related constructs (Bernstein, Zvolensky, Vujanovic, & Moos, 2009). These perspectives suggest that distress tolerance may be hierarchical in nature—composed of a global hierarchical experiential (in)tolerance construct and a number of specific lower-order, domain-specific dimensions (see Fig. 1). An alternative yet empirically unexplored interpretation of these findings is that a higher-order ‘‘experiential avoidance’’ factor may be comprised of a number of specific lower-order, domain-specific distress tolerance dimensions.
Fig. 1.
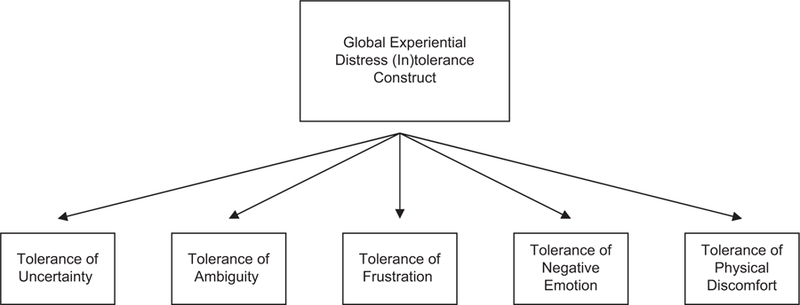
Heuristic depiction of the global experiential distress (in)tolerance construct and lower-order, domain-specific dimensions.
There also has been express interest in providing a conceptual model for understanding distress tolerance on functional and neurobiological levels. Here, Trafton and Gifford (in press) have posited that distress tolerance (a) involves the ability to not respond to an opportunity for negative reinforcement (e.g., relief from distress represents a negative reinforcement opportunity), (b) reflects self-control over responding to immediate reward opportunities, and (c) may be understood as a facet of impulsivity in responding to immediate reinforcement. This perspective suggests that neurobiological substrates underlying reward learning and responding may mediate tolerance to distress.
Conceptual and Operational Definitions
Perceived capacity to tolerate distress
The perceived capacity to tolerate distress has been operationalized in five principle ways, including tolerance of (a) uncertainty, (b) ambiguity, (c) frustration, (d) negative emotional states, and (e) physical sensations (Leyro et al., 2010). Although these constructs are theorized to focus on the tolerance of some form of experiential distress, they are derived from distinct conceptualizations and have not yet been integrated into one overarching model. Yet, each of these aspects of distress tolerance has been measured using self-report indices and theorized to be generally stable across contexts and time.
Tolerance of uncertainty is defined as individual differences in the tendency to react emotionally, cognitively, or behaviorally to uncertain situations (Buhr & Dugas, 2002). Intolerance of uncertainty has been studied most extensively in regard to generalized anxiety disorder (GAD). For instance, variations in a person’s ability to tolerate uncertainty may be related to the degree to which he or she worries about and experiences emotional distress in response to life uncertainties. Indeed, intolerance of uncertainty is (a) concurrently related to greater degrees of anxiety symptoms among nonclinical populations, (b) elevated among persons with GAD relative to other anxiety disorders, and (c) an active element of change underlying positive GAD treatment outcome (Buhr & Dugas, 2002).
Tolerance of ambiguity reflects individual differences in perceived tolerance of complicated, foreign, and/or vague situations or stimuli (Furnham & Ribchester, 1995). This construct differs from tolerance of uncertainty in that it is aimed at ambiguous stimuli (cf. unpredictable stimuli). To the extent a person has relatively lower levels of tolerance of ambiguity, he or she is expected to react with greater emotional distress when faced with an ambiguous situation. Although the psychometric properties of scales used to measure tolerance of ambiguity have been questioned, the construct has been significantly concurrently related to behavioral rigidity and worry (Leyro et al., 2010).
Tolerance of frustration reflects individual differences in the perceived capacity to withstand aggravation (e.g., thwarted life goals). Tolerance for frustration is concurrently related to a variety of self-control and affective variables. For example, tolerance for frustration is concurrently related to procrastination problems and self-harm and prospectively related to greater anxiety and depression symptoms (Leyro et al., 2010).
Tolerance of negative emotional states reflects individual differences in the perceived capacity to withstand internal distress (Simons & Gaher, 2005). Lower levels of tolerance for negative emotional states are concurrently and prospectively related to greater risk for substance use disorders, coping-oriented drug use, bulimic symptoms, and posttraumatic stress symptoms (Vujanovic, Bernstein, & Litz, in press). In many studies, distress tolerance for negative emotional states has demonstrated incremental predictive value relative to other established factors (e.g., neuroticism; Leyro et al., 2010).
Tolerance of physical sensations reflects individual differences in the perceived capacity to withstand uncomfortable physical sensations (Schmidt, Richey, & Fitzpatrick, 2006). So-called discomfort-intolerant persons—those less able to withstand aversive physical sensations (e.g., dizziness)—may be more motivated to escape or avoid situations or activities that may trigger the sensations. Discomfort intolerance is (a) elevated among persons with panic disorder compared to nonclinical populations, (b) concurrently and prospectively associated with more intense anxiety symptoms, and (c) predictive of self-reported fearful and anxious responding to laboratory-based stress tasks (Leyro et al., 2010).
Behavioral capacity to tolerate distress
A number of approaches to behaviorally measure tolerance to various forms of distress by means of physical and cognitive experimental tasks have been used. These approaches measure the duration of time that an individual can withstand exposure to a specific type of aversive task or stimulus from which tolerance to the experiential distress elicited by such stimuli/tasks is inferred.
In one area of study, distress tolerance has been indexed via tasks that elicit symptoms of physiological arousal and anxiety. These procedures (e.g., voluntary hyperventilation, CO2-enriched air challenge) are used to acutely change levels of oxygen and CO2 in order to induce physiological sensations associated with anxious arousal (e.g., shortness of breath, dizziness). Levels of tolerance for procedures that induce abrupt anxious arousal sensations are indexed by how long it takes the participant to discontinue the task (latency). Such studies suggest that lower tolerance to distress elicited by these experimental tasks may be related to greater difficulties abstaining from substance use among active users. This work has been greatly influenced by the field of tobacco dependence and cessation. For example, Brown and colleagues (2009) found that pre-smoking-cessation distress tolerance levels, as indexed by breath-holding duration and persistence on a CO2 challenge, predicted an increased risk for early relapse to smoking following a self-guided quit attempt. Thus, there may be segments of the smoking population that benefit from specialized cessation interventions focused on distress tolerance (Brown et al., 2009).
In another line of study, distress tolerance has been evaluated by means of difficult or frustrating cognitive tasks. The most well-known measures in this domain include the Paced Auditory Serial Addition Test (PASAT), Mirror-tracing, and Anagram Persistence Tasks. Levels of tolerance to distress elicited by these procedures are measured by latency to discontinue the task. Research employing these methodological approaches has largely focused on addictive behaviors. Performance on these tasks is related to problematic alcohol use, substance abuse history, and smoking cessation failure. For example, Daughters, Lejuez, Kahler, Strong, and Brown (2005) found that latency to PASAT termination was related to the duration of the most recent drug/alcohol cessation attempt. Thus, duration of task engagement appears to be related to the ability to maintain substance use abstinence.
Future Directions
Construct validity
There are a number of pressing construct validity questions central to distress tolerance research. One issue at the nexus of our conceptual understanding of distress tolerance and measurement strategies involves the relations between perceived distress tolerance and behavioral acts of tolerating distress. Indeed, it is not yet clear how self- and non-self-report measures of distress tolerance relate to one another or to the overarching construct(s). Self-report and behavioral distress tolerance measures tend not to exhibit significant associations with one another but are associated within each measurement modality (McHugh et al., in press). This observation calls for consideration of at least two possible directions: (a) the development and evaluation of a multimethod measurement of the putative overarching distress tolerance construct and (b) the development and evaluation of an alternative theoretical account of distress tolerance in which perceived distress tolerance and behavioral capacity to withstand distress reflect distinct latent individual difference factors.
Related factors and processes
Another important gap in the distress tolerance literature is the lack of theory and empirical study regarding the putative associations between distress tolerance and other risk and protective factors (e.g., anxiety sensitivity, emotion (dys)regulation, experiential avoidance, avoidant or disengagement coping, and mindfulness and acceptance). Future research might focus study on the functionally unique and overlapping relations between distress tolerance and factors theorized to be structurally and functionally distinct.
Psychopathology vulnerability
Research evaluating relations between distress tolerance and various forms of psychopathology is limited. One central question for future study is the degree to which distress tolerance may be related to specific psychological disorders or to multiple forms of psychopathology. This type of knowledge is central to guiding prevention and treatment strategies targeting distress tolerance and related processes. It may be useful to explore the possibility that while certain facets of distress tolerance may have transdiagnostic relations, others may be more narrowly related to vulnerability for specific disorders.
Flexibility and context
The roles of flexibility and context sensitivity in distress tolerance and related psychopathology vulnerability also may represent an important domain for future study. For example, lower levels of distress tolerance may not be necessarily maladaptive in all contexts; similarly, higher levels of distress tolerance may not necessarily be adaptive in all contexts. Flexibility in one’s degree of distress tolerance as a function of its contextual adaptivity and the role of such a contextual perspective on distress tolernace for understanding psychopathology vulnerability may reflect an important direction for research (e.g., Lynch & Mizon, in press).
There also is a paucity of data regarding the extent to which distress tolerance is or is not stable across time and/or context. Specifically, distress tolerance may be characterized by a context-sensitive or context-dependent expression (Bernstein, Trafton, Ilgen, & Zvolensky, 2008). Research may usefully focus on advancing our understanding of how context may shape distress tolerance and its expression, as well as its relations to psychopathology.
Developmental origins and processes
Our empirical understanding of the development and maintenance of distress tolerance is still largely unknown. Distress tolerance may be influenced by learning history, genetic/biological factors, or environmental stressors. There has been a striking paucity of research on this topic. Furthermore, neither the temporal impact of change in distress tolerance on psychopathology nor the impact of change in psychopathology on distress tolerance has received much empirical study. Exploration of these developmentally oriented questions is likely to substantively advance theory regarding the nature of distress tolerance and psychopathology relations. Here, it may be especially useful to draw from related bodies of work such as that on emotion regulation.
Therapeutic mechanism(s) and effective therapeutic strategies
There has been limited direct study of distress tolerance in the context of clinical intervention (see Dugas & Ladoucer, 2000, for an exception). This lack of investigation is notable given that many psychosocial treatment programs for psychopathology incorporate distress tolerance, directly or indirectly, in therapeutic approaches (Zvolensky et al., in press). Study of the role(s) of change in distress tolerance and therapeutic change in various psychological disorders is a necessary and important domain for future study. In addition, we lack study of effective and efficient therapeutic means by which to promote change in distress tolerance; such study may prove important in advancing our understanding of distress tolerance and determination of its potential clinical importance.
Summary
Distress tolerance has increasingly been viewed as important to the development and maintenance of multiple forms of psychopathology and as a promising target within a variety of psychotherapeutic approaches. A number of promising ways to conceptualize and measure distress tolerance are available, and a growing body of research is exploring the nature of distress tolerance and its relations to psychopathology. Though theoretically and clinically promising in many respects, future work is needed to explicate a variety of questions regarding the nature of distress tolerance and its potential role(s) in psychopathology research and practice.
Acknowledgments
The views expressed here are those of the authors and do not necessarily represent the Department of Veterans Affairs.
Funding
This research was supported by several National Institutes of Health (NIH) grants (1 R01 DA027533–01; 1 R01 MH076629–01) awarded to Dr. Zvolensky. Dr. Bernstein recognizes the funding support from the Israeli Council for Higher Education Yigal Alon Fellowship, the European Union FP-7 Marie Curie Fellowship International Reintegration Grant, and the Rothschild-Caesarea Foundation’s Returning Scientists Project at the University of Haifa. This work also was supported by a NIH predoctoral fellowship awarded to Ms. Leyro (1 F31 DA024919–01).
Footnotes
Declaration of Conflicting Interests
The authors declared that they had no conflicts of interest with respect to their authorship or the publication of this article.
References
- Bernstein A, Trafton J, Ilgen M, & Zvolensky MJ (2008). An evaluation of the role of smoking context on a biobehavioral index of distress tolerance. Addictive Behaviors, 33, 1409–1415. [DOI] [PubMed] [Google Scholar]
- Bernstein A, Zvolensky MJ, Vujanovic AA, & Moos R (2009). Anxiety sensitivity, distress tolerance, and discomfort intolerance: A hierarchical model of affect sensitivity and tolerance. Behavior Therapy, 40, 291–301. [DOI] [PubMed] [Google Scholar]
- Brown RA, Lejuez CW, Strong DR, Kahler CW, Zvolensky MJ, Carpenter L, et al. (2009). A prospective examination of distress tolerance and early smoking lapse in adult self-quitters. Nicotine and Tobacco Research, 11, 493–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buhr K, & Dugas MJ (2002). The intolerance of uncertainty scale: Psychometric properties of the English version. Behaviour Research and Therapy, 40, 931–945. [DOI] [PubMed] [Google Scholar]
- Daughters SB, Lejuez CW, Kahler CW, Strong DR, & Brown RA (2005). Psychological distress tolerance and duration of most recent abstinence attempt among residential treatment-seeking substance abusers. Psychology of Addictive Behaviors, 19, 208–211. [DOI] [PubMed] [Google Scholar]
- Dugas MJ, & Ladouceur R (2000). Treatment of GAD: Targeting intolerance of uncertainty in two types of worry. Behavior Modification, 24, 635–657. [DOI] [PubMed] [Google Scholar]
- Furnham A, & Ribchester T (1995). Tolerance of ambiguity: A review of the concept, its measurement and applications. Current Psychology, 14, 179–199. [Google Scholar]
- Leyro TM, Zvolensky MJ, & Bernstein A (2010). Distress tolerance and psychopathological symptoms and disorders: A review of the empirical literature among adults. Psychological Bulletin, 136, 576–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch TR, & Mizon GA (in press). Distress over-tolerance and distress intolerance: A behavioral perspective. In Zvolensky MJ , Bernstein A, & Vujanovic AA (Eds.), Distress tolerance New York, NY: Guilford. [Google Scholar]
- McHugh RK, Daughters SB, Lejuez CW, Murray HW, Hearon BA, Gorka SM, & Otto MW (in press). Shared variance among self-report and behavioral measures of distress intolerance. Cognitive Therapy and Research [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt N, Richey J, & Fitzpatrick K (2006). Discomfort intolerance: Development of a construct and measure relevant to panic disorder. Journal of Anxiety Disorders, 20, 263–280. [DOI] [PubMed] [Google Scholar]
- Simons J, & Gaher R (2005). The distress tolerance scale: Development and validation of a self-report measure. Motivation and Emotion, 29, 83–102. [Google Scholar]
- Trafton JA, & Gifford EV (in press). Biological bases of distress tolerance. In Zvolensky MJ, Bernstein A, & Vujanovic AA (Eds.). Distress tolerance New York: Guilford. [Google Scholar]
- Vujanovic AA, Bernstein A, & Litz BT (in press). Distress tolerance and traumatic stress. In Zvolensky MJ, Bernstein A, & Vujanovic AA (Eds.), Distress tolerance New York, NY: Guilford. [Google Scholar]
- Zvolensky MJ, Bernstein A & Vujanovic AA (Eds.). (in press). Distress tolerance New York: Guilford. [Google Scholar]


