BACKGROUND
Breast and colorectal cancer are two of the most commonly diagnosed cancers in the USA, generating 400,000 new cases and 90,000 attributable deaths in 2019 alone. Early detection through routine screenings is essential for improving cancer-related morbidity and mortality rates.1 The COVID-19 pandemic has created the potential for a backslide in cancer screening rates, particularly forms of screening like mammography and colonoscopy that rely on office-based medical technologies.2 Yet, whether cancer screening rates have declined, and how reductions vary across patient populations, remains largely unknown.
OBJECTIVE
To examine mammography and colonoscopy rates among commercially insured American adults before and after March 13, 2020—the date on which COVID-19 was declared a national emergency—as well as US county-level characteristics predictive of screening rates.
METHODS
We quantified weekly medical claims from commercially insured US adults between January 15, 2020, and July 31, 2020. Medical claims data were provided by Castlight Health, a health benefits manager for employer-sponsored health insurance plans across all 50 states, which included 6.8 million individuals.3 We limited the study sample to those ages 46 to 64, target populations for cancer screening procedures prior to Medicare eligibility. For screening mammography, we limited our sample to women. Procedures were identified using IBM Watson Health procedure categories.4 We calculated weekly number of individuals, per 10,000 eligible beneficiaries, who received cancer screenings. We also included patient age category (ages 46–59, 60–64) and sex, and linked claims to county-level demographic characteristics: percent non-Hispanic black and percent Hispanic, and median household income, according to the U.S. Census Bureau; and weekly prevalence of SARS-CoV-2 cases per 10,000 population, according to USAFacts.
Longitudinal multivariable fixed-effects regression analyses estimated change in screening rates following March 13, 2020, relative to prior weeks. Fixed effects were included for calendar year, calendar week, and US state. Standard errors were clustered at the state level. Additional models interacted the dichotomous time variable with demographic characteristics. For each model, marginal means were generated to estimate adjusted, weekly screening rates through July 2020. This study was approved by the RAND IRB.
RESULTS
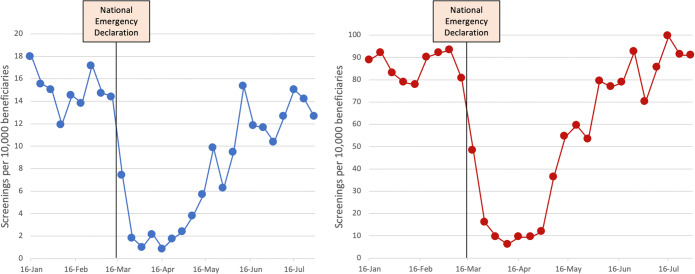
Prior to the national emergency declaration on March 13, 2020, median weekly rate of screening mammography was 87.8 women per 10,000 beneficiaries, which declined to 6.9 in April—a 96% decline (Table 1). By the end of July, this figure had rebounded to 88.2 screenings per 10,000 beneficiaries. Over the same period, colonoscopy screenings declined from 15.1 per 10,000 beneficiaries to 0.9, a 95% difference, and rebounded to 12.6 per 10,000 beneficiaries by the end of July. Adjusted estimates from multivariable regression analyses confirmed a significant decline (mammography: − 84.7 screenings per 10,000 beneficiaries, 95%CI − 96.8, − 72.3; colonoscopy: − 11.6, 95%CI − 14.8, − 8.4), with marginal adjusted means comparable to pre-COVID levels by the end of July (mammography: 0.2, 95%CI − 14.5, 14.9; colonoscopy: 1.6, 95%CI − 1.3, 4.5) (Fig. 1). For colonoscopy screenings, we observed a sharper decline in highest-income quartile counties compared to lowest-income quartile counties (3.0 fewer screenings; 95% CI 0.3, 5.8). We did not find any significant demographic differences when inspecting screening mammography rates.
Table 1.
Screening Mammography and Colonoscopy Rates
| Demographic characteristic | Mammography | Colonoscopy | ||||
|---|---|---|---|---|---|---|
| Rate, pre-COVID (SD) | Rate, low pointa (SD) | Rate, end of July (SD) | Rate, pre-COVID (SD) | Rate, low pointa (SD) | Rate, end of July (SD) | |
| All | 87.8 (367.3) | 6.9 (67.1) | 88.2 (386.1) | 15.1 (144.1) | 0.88 (16.3) | 12.6 (132.1) |
| Age group | ||||||
| 46–59 | 87.3 (331.4) | 7.0 (58.6) | 88.0 (375.0) | 14.5 (133.7) | 1.1 (18.9) | 11.6 (143.1) |
| 60+ | 88.3 (402.4) | 6.7 (75.0) | 88.5 (397.6) | 15.7 (154.4) | 0.6 (12.8) | 13.7 (119.2) |
| Income | ||||||
| 1st quartile (lowest) | 86.9 (406.3) | 6.6 (85.9) | 78.7 (408.6) | 14.4 (163.9) | 0.9 (16.6) | 12.6 (138.7) |
| 2nd quartile | 92.7 (405.0) | 7.7 (68.4) | 85.6 (288.8) | 15.0 (167.9) | 1.0 (20.4) | 15.0 (199.8) |
| 3rd quartile | 83.5 (357.6) | 8.5 (74.6) | 111.3 (566.4) | 14.7 (139.7) | 0.7 (9.0) | 10.8 (86.5) |
| 4th quartile (highest) | 88.0 (292.9) | 4.9 (25.7) | 76.9 (171.9) | 16.2 (95.2) | 0.9 (16.9) | 12.1 (58.1) |
| Rurality | ||||||
| Metropolitan | 88.1 (117.8) | 8.1 (44.5) | 85.3 (115.0) | 16.1 (51.4) | 0.9 (13.5) | 13.8 (41.3) |
| Non-metropolitan | 87.7 (430.9) | 6.4 (74.5) | 89.5 (454.1) | 14.7 (168.2) | 0.9 (17.3) | 12.1 (155.0) |
| % African American | ||||||
| 1st quartile (lowest) | 87.2 (509.2) | 7.8 (103.0) | 88.1 (594.6) | 15.2 (202.8) | 0.5 (12.2) | 11.6 (219.0) |
| 2nd quartile | 85.5 (361.5) | 5.3 (57.5) | 97.2 (434.6) | 15.5 (154.6) | 1.1 (19.6) | 11.5 (78.1) |
| 3rd quartile | 87.7 (312.3) | 5.7 (50.9) | 81.4 (230.5) | 14.2 (102.1) | 0.9 (18.5) | 13.9 (116.0) |
| 4th quartile (highest) | 90.3 (278.8) | 8.7 (51.2) | 87.5 (226.0) | 15.5 (109.8) | 0.9 (13.5) | 13.1 (83.3) |
| % Hispanic | ||||||
| 1st quartile (lowest) | 88.6 (385.8) | 8.6 (101.5) | 76.8 (276.6) | 14.9 (166.6) | 0.8 (20.9) | 16.1 (217.2) |
| 2nd quartile | 89.0 (352.7) | 6.1 (48.0) | 95.1 (439.1) | 16.3 (161.6) | 1.1 (16.5) | 12.8 (89.4) |
| 3rd quartile | 85.2 (331.7) | 5.2 (33.3) | 97.7 (404.5) | 14.8 (95.8) | 0.8 (11.6) | 10.4 (49.0) |
| 4th quartile (highest) | 88.6 (400.3) | 7.9 (66.9) | 82.3 (403.9) | 14.3 (142.2) | 0.8 (14.7) | 11.1 (111.3) |
| Prevalence of SARS-CoV-2 | ||||||
| 1st quartile (lowest) | 91.0 (460.5) | 4.7 (77.9) | 74.7 (403.2) | 14.3 (195.8) | 1.0 (19.4) | 15.5 (241.3) |
| 2nd quartile | 82.6 (360.8) | 8.9 (81.5) | 95.3 (481.5) | 14.3 (125.5) | 0.7 (17.8) | 11.7 (82.2) |
| 3rd quartile | 89.6 (329.1) | 6.8 (54.1) | 81.3 (248.6) | 14.6 (92.3) | 1.0 (13.8) | 11.1 (65.8) |
| 4th quartile (highest) | 88.3 (320.1) | 6.9 (52.2) | 99.3 (380.6) | 16.9 (151.4) | 0.8 (14.0) | 12.5 (81.5) |
Mean and standard deviation reflect the number of patients per 10,000 beneficiaries by patient gender, age category and county
aLow point represents the lowest weekly number of screenings per 10,000 beneficiaries—in mid-April
Figure 1.
Cancer screening rates during 2020.
DISCUSSION
While the COVID-19 pandemic has catalyzed a shift from office-based medical visits to telemedicine, routine cancer screenings typically require office-based care. We found that, following the COVID-19 national emergency declaration, mammography and colonoscopy rates declined by over 90% in a large cross-section of commercially insured adults throughout the country. Furthermore, despite an even larger spike in COVID case rates during summer months, cancer screening rates continued to rebound to pre-COVID levels—suggesting that health systems were able to recalibrate resources and protocols in a relatively short interval. Early in the pandemic, experts expressed concerns about the potential for a large drop-off in cancer screenings,5 confirmed by these findings. However, health systems also rapidly responded with protocols and strategies to reopen in an appropriate manner,6 and this study is the first to document the success of this effort.
We note three study limitations. First, the data derive from a subset of individuals with private insurance and does not include publicly insured or uninsured patients. Second, our colonoscopy results do not include alternative forms of colorectal cancer screening, such as FOBT. Finally, our results are limited to the first 7 months of 2020.
Funding
Support was provided by the National Institutes on Aging (1K01AG061274, Dr. Whaley) and the Office of the Director, National Institutes of Health (1DP5OD017897, Dr. Jena).
Declarations
Conflict of Interest
Drs. McBain, Cantor, Bavata, and Ms. Pera declare no conflicts of interest. Dr. Jena reports receiving consulting fees unrelated to this work from Pfizer, Hill Rom Services, Bristol Myers Squibb, Novartis, Amgen, Eli Lilly, Vertex Pharmaceuticals, AstraZeneca, Celgene, Tesaro, Sanofi Aventis, Biogen, Precision Health Economics, and Analysis Group. The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
REFERENCES
- 1.Common Cancer Types - National Cancer Institute [Internet]. 2015 [cited 2020 Aug 21]. Available from: https://www.cancer.gov/types/common-cancers.
- 2.Jones D, Neal RD, Duffy SRG, Scott SE, Whitaker KL, Brain K. Impact of the COVID-19 pandemic on the symptomatic diagnosis of cancer: the view from primary care. The Lancet Oncology. 2020;21(6):748–50. doi: 10.1016/S1470-2045(20)30242-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Castlight Health. Castlight Health: Health Navigation Platform [Internet]. 2020 [cited 2020 Dec 8]. Available from: https://www.castlighthealth.com/.
- 4.IBM Watson Health. The Medical Episode Grouper: Applications and Methodology. [Internet]. IBM; 2018. Available from: https://www.ibm.com/downloads/cas/EZALXAMB. Accessed 1 Nov 2020.
- 5.Nelson B. Covid-19 is shattering US cancer care. BMJ [Internet]. 2020 Apr 17 [cited 2020 Dec 1];369. Available from: https://www.bmj.com/content/369/bmj.m1544. [DOI] [PubMed]
- 6.Coomes EA, Al-Shamsi HO, Meyers BM, Alhazzani W, Alhuraiji A, Chemaly RF, et al. Evolution of Cancer Care in Response to the COVID-19 Pandemic [Internet]. Vol. 25, The oncologist. Oncologist; 2020 [cited 2020 Dec 1]. Available from: https://pubmed.ncbi.nlm.nih.gov/32536024/. [DOI] [PMC free article] [PubMed]