Abstract
Sexual health education interventions have generally yielded modest impact, but may be more successful when integrated into programs designed to alleviate poverty and empower women. Between December 2017 and February 2018, we interviewed 304 Haitian female microfinance clients, 75 of whom had received health education training delivered within their regular meetings. Participants reported six key sexual health outcomes. We used log-binomial models to estimate the association between health education training and each outcome, and tested for interaction by age and literacy status. Women with health education training reported more condom use with unfaithful partners [PR (95% CI): 1.78 (1.04, 3.02)], more HIV tests [PR (95% CI): 1.56 (1.28, 1.90)], and fewer STI symptoms [PR (95% CI): 0.37 (0.19, 0.73)], compared to women with no training. Some of the associations were stronger among older women [e.g. HIV testing: PR (95% CI): 2.09 (1.49, 2.82)] and illiterate women [e.g. condom use: PR (95% CI): 3.46 (1.05, 11.38)]. These findings add to the growing body of evidence demonstrating the potential to use microfinance programs as platforms for health education delivery, and provide the first evidence for the association in Haiti.
Keywords: microfinance, HIV, STI, sexual behavior, Haiti
Introduction
Despite decades of public health education and intervention, global HIV and sexually transmitted infection (STI) prevalence remain unacceptably high, particularly in resource-poor settings like Haiti.(1) In 2016, approximately 150,000 Haitians were living with HIV, accounting for more than half of all HIV infections and AIDS-related deaths in the Caribbean.(2–4) The burden of HIV disproportionately affects Haitian women. In 2016, the prevalence of HIV in Haitian women was estimated at 2.3% compared to 1.9% among Haitian men.(3) Other STIs also occur at high rates in Haitian women. Chlamydia, gonorrhea, syphilis, and trichomoniasis have all been documented as common infections in Haitian women in multiple studies from 2000 to 2014.(5–8) Educational campaigns have long been deployed in attempt to reduce the spread of HIV and STIs. Yet few evidence-based educational interventions have proven to be effective at increasing uptake of safer sexual behaviors.(9) For example, despite widespread condom campaigns in Haiti, condom use among Haitians remains quite low. In the most recent Demographic and Health Survey (DHS) in 2016-2017, less than half of Haitian women with multiple sexual partnerships reported using a condom at last sex;(10) these estimates were essentially unchanged from those measured in the previous DHS survey in 2012.(11) One potential explanation for the low efficacy of educational interventions for sexual health promotion is that they fail to address the underlying structural drivers of HIV and STI transmission.
Poverty is consistently identified as an upstream driver of HIV and STI transmission, particularly among vulnerable women.(12, 13) This study was conducted in Haiti, a low-income country with 60% of the 10 million inhabitants living below the poverty line.(14) In Haiti, STI and HIV rates tend to be higher among people with lower socioeconomic status.(5, 8, 15) One plausible mechanism for the relationship between socioeconomic status and poor sexual health outcomes is that insufficient financial resources could limit access to condoms, HIV testing, and STI treatment and care.(16) Another plausible mechanism, in line with the Theory of Gender and Power,(17) is that women who are economically dependent on their male partners are unable to negotiate for safer sex within their relationships for fear of losing economic stability.(18, 19) For these reasons, poverty alleviation has become a key target for HIV prevention and sexual health promotion in lower-income countries.(20)
Thus, it is possible that sexual health education interventions may be more successful when combined with programs designed to alleviate poverty and empower women.(21–23) Microfinance organizations are designed to alleviate poverty by lending small amounts of money to fund income generation projects and foster economic independence in resource poor settings.(24) These microfinance programs almost exclusively serve women and often have an explicit goal to improve the health and well-being of clients.(24–26) To that end, additional health-promotional activities like health education are often incorporated into and delivered through the microfinance framework.(22, 25) Generally positive findings about the effectiveness of delivering sexual health education through a microfinance platform have been observed in Mongolia,(27) and India,(28); more mixed results were observed in South Africa(29) and Colombia,(30) However, no prior studies have been conducted on the subject in Haiti.(31, 32)
In this study, we analyze survey data provided by clients of a Haitian microfinance organization to better understand the relationship between health education training and sexual health behaviors in a microfinance program context.
Methods
Study setting and study population
This study was conducted in partnership with Fonkoze, Haiti’s largest microfinance organization, which has been serving Haitians living in poverty since 1994.(33) Fonkoze has wide geographic reach with 44 branch offices across all 10 departments of Haiti and serves primarily women. Fonkoze’s most utilized service is the solidarity lending program, in which groups of five women organize together to take out and repay loans. In general, Fonkoze provides clients with increasing loan sizes and opportunities as they progress through the program; solidarity group loans range in size from US$100 up to US$1300. Fonkoze also has a history of integrating educational programs and training into its framework, offering separate training modules on business skills (e.g. asset management and strategic planning), life skills (e.g. disaster preparedness), literacy (e.g. reading and writing), and health education (e.g. nutrition and HIV/STI prevention).
Between December 2017 and February 2018, we conducted a cross-sectional survey with clients served by the Fonkoze branch office in Okay, Haiti. Okay is a port city on Haiti’s southern peninsula with a population of approximately 70,000. Fonkoze has served clients in the Okay area since 1996. There are over 200 smaller client centers served by this regional branch office, and, in total, the Okay branch office currently serves over 6,200 Fonkoze clients in the city of Okay and surrounding towns. This branch office was selected because the large population it serves allowed us a sufficient target population size from which to sample, because the length of time it has offered services in the area meant that we would expect to see intervention impact if it existed, and because local branch leadership were interested and willing to collaborate on the project.
We used the complete client database of the Okay Fonkoze branch office in 2017 as a sampling frame to identify a random sample of current clients for interview. Clients were eligible to participate if they were current Fonkoze clients served by the Okay branch office, female, and between the ages of 18-49 years. This age range was chosen to limit the study population to women of reproductive age, and to maximize the chance that we would enroll a study population for whom questions about sexual and reproductive health would be most relevant.
Households of potential participants were contacted in person up to three times. If the potential participant was home, fieldworkers gave her information about the study. Study information scripts emphasized that participation in the study would be completely voluntary and that refusal would have no influence on Fonkoze membership or future access to microloans. Those who elected to participate provided written informed consent. Ethical approval for this study’s protocol was obtained from Indiana University’s Human Subjects Office (Protocol #1705661852). The study protocol was further reviewed and approved internally by Fonkoze.
Health education training
Fonkoze trainings are delivered at the client center level and client center chiefs make the decisions about whether their members receive health education training. Client centers are collections of around 8-12 solidarity groups (approximately 40–60 total members) that meet together bi-monthly to repay loans and receive training. Client center chiefs are Fonkoze clients chosen by the client center members to represent them. The health education training is delivered over the course of approximately 12 monthly meetings by the center chiefs who have volunteered to facilitate the education delivery. Interested center chiefs travel to the branch office for initial training in the curriculum by a nurse. The curriculum was developed by Fonkoze health programmers in partnership with USAID and the Haitian Ministry of Health, and based on material originally developed by UNICEF.(34) It covers a broad range of topics including: child nutrition, hygiene, HIV/AIDS, and reproductive health, and is presented in picture-based handbooks. Much of the relevant sexual health education is given in the HIV/AIDS module, including sub-topics on: modes of transmission; testing and counselling; prevention of sexual transmission (reducing sex partners, practicing mutual monogamy, and using condoms consistently and correctly); and identifying, testing, and treating other STIs. The sexual health education content is generally delivered over the course of 3-4 monthly meetings.
Data collection procedures
Four local fieldworkers were recruited and hired using Fonkoze’s standard hiring procedures based on previous experience with monitoring and evaluation. Prior to study start, a three-day training, led by the study investigators, educated the fieldworkers on research ethics, and familiarized them with the study instruments and standard operating procedures. All data used in this study were collected electronically in tablet-based surveys, designed and administered with REDCap web and off-line mobile application. The instrument was translated from English to Haitian Creole with back-translation to ensure proper translation, and the survey was conducted exclusively in Haitian Creole. The surveys were conducted in a private location in the participant’s home though other private locations were made available as requested by the participant. Data were collected on a broad range of topics including physical and economic well-being: sociodemographics, infectious disease risk, microfinance experience, natural disaster resilience, and sexual behavior.
Key variables
The primary exposure of interest was receipt of the Fonkoze health education training. Participants were asked about which of four possible Fonkoze trainings they had received. Those who responded ‘yes’ to having received the health education training were considered exposed.
We assessed six sexual health outcomes. Of the women who reported having a sex partner in the last 12 months, (1) condom use was measured by the self-reported response to the question: ‘Did you use a condom the last time you had sex with your most recent partner (Yes/No)?’ Because some women may choose not to use condoms if they feel confident in the monogamous nature of their relationship, we also assessed (2) condom use with an unfaithful partner, considering condom use at last sex in the sub-population of women who reported their most recent partner had sex with someone else during their relationship, or was unsure about their partners’ outside partnership sexual activity. We assessed (3) HIV test status by identifying the women who reported ever having tested for HIV and who’s most recent test dates were within the last 12 months from their interview date. We assessed (4) transactional sex based on participant responses to a query about if they felt obligated to have sex with a partner because of gifts or money they were provided. This broad definition encompasses both formal and informal transactional sex, and has been previously used in multiple HIV prevention studies across a range of low-resource settings.(35–40) We assessed (5) recent STI diagnosis by querying if participants had a doctor tell them they had any of the following STIs: chlamydia, gonorrhea, syphilis, or trichomoniasis within the last 12 months from the interview date. Finally, we assessed (6) recent STI symptoms by querying whether participants had any of the following symptoms suggestive of a STI in the last 12 months: bad-smelling abnormal genital discharge, genital sore, or genital ulcer.
To contextualize the study population and to control for potential confounding, we also assessed several key socio-demographic covariates: Age, in years; marital status, categorized as currently married or living as married, divorced or separated, and never married; educational attainment, categorized as none, preschool or primary, and secondary and higher; literacy, defined as the self-reported ability to read, verified with a test sentence in Haitian Creole; household size, defined as the number of people sharing the participant’s household; and household assets, defined as the self-reported value (in Haitian gourdes, at time of purchase) of 20 potential items in the participants’ households. Example items in the list of household items we queried were oven, television, radio, and refrigerator. If the household did not contain an item, the value was coded as 0. We categorized the household asset index in quartiles, from lowest (Q1) to highest (Q4). We also assessed several variables to characterize the participants’ experiences with the microfinance program, including the duration of program membership (in months), the size of their most recent microloan (in Haitian Gourdes), and the size of their savings account (in Haitian Gourdes).
Statistical analysis
We used log-binomial models to estimate prevalence ratios for the relationship between exposure to the health education training program and each of the six sexual health outcomes. Because of the way the health education training exposure was allocated (decisions not by individual clients but by client center chiefs), we expected those who received and did not receive the training to be fairly well-balanced in terms of covariates. As a sensitivity analysis to test this assumption, we also adjusted the log-binomial models for age and education to compare the magnitude of the associations between adjusted and unadjusted analyses. We chose to run the sensitivity analyses with age and education as they are both strong predictors of sexual health outcomes.
We conducted two post-hoc subgroup analyses to assess whether the relationship between health education training and sexual health differed by age and by literacy status. To do so, we incorporated interaction terms between health education training (yes/no) and age (above/below median age of 36), and health education training (yes/no) and literacy (yes/no). We assessed whether the effect estimates for the subgroups (by age and literacy status) were statistically different from each other with Wald tests for the interaction terms. Wald test statistics with p-values <0.05 were considered statistically significant. All statistical analyses were performed using SAS 9.4 (Cary, NC).(41)
We georeferenced the location of each household survey using ArcGIS Online mapping tools to visually assess the geographic distribution of households of clients who did and did not receive the health education training. We further checked for spatial clustering of locations using Kulldorff’s spatial scan statistic in SaTScan software (Information Management Services, Boston, MA, USA) in order to ensure similar geographic distributions among those who did and did not receive the health education training.(42) Specifically, a Bernoulli model was used to scan for clustering of household locations in each group. A maximum spatial cluster size of 50% of the total population was used. For statistical inference, 999 Monte Carlo replications were performed. The null hypothesis of no spatial clustering was rejected when the simulated p-value ≤ 0.05.
Results
We approached 349 women for potential participation (Figure I). We excluded 41 women because they did not meet eligibility criteria (outside of age range 18-49 or no longer a Fonkoze client), we were unable to locate three women, and one woman refused to participate. A total of 304 Fonkoze clients enrolled in this study and completed surveys for an overall participation rate of 98.7% among those eligible to participate.
Figure I.
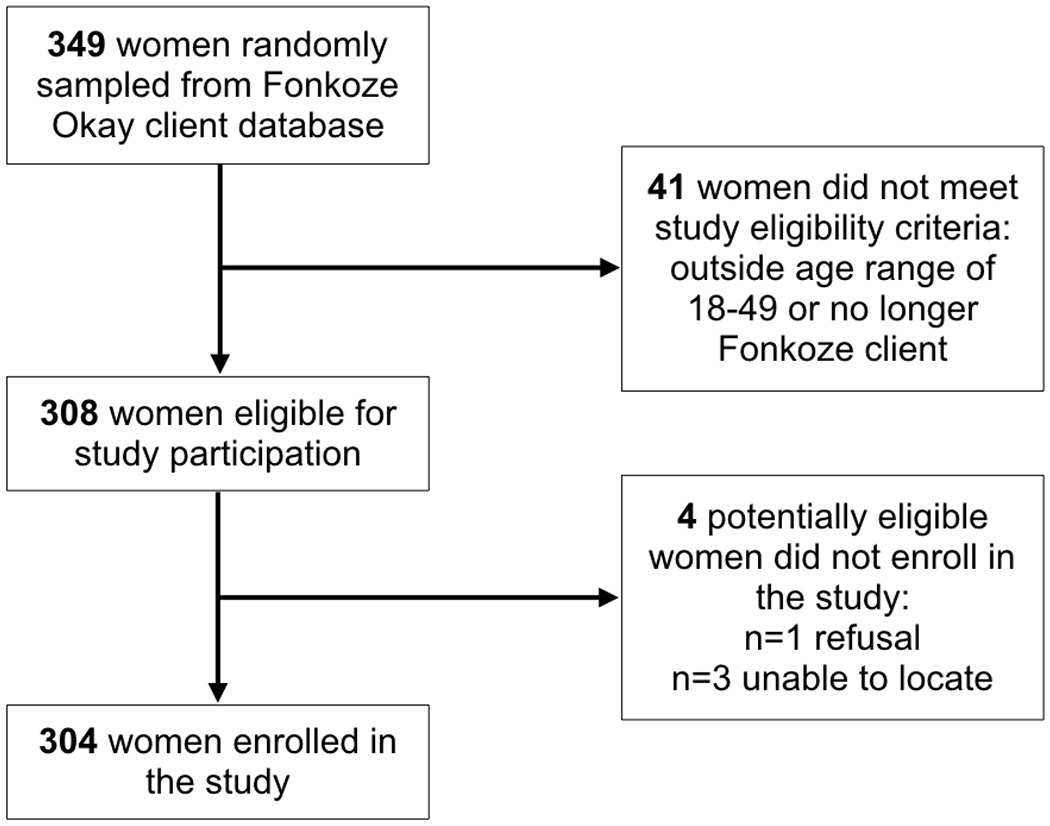
Flowchart detailing recruitment and enrollment of 304 Haitian women, December 2017 to February 2018
The participants ranged in age from 20 to 49 with a median age of 36 years (interquartile range: 30.0 to 42.5 years) (Table I). Most of the women were currently married (55.0%). Educational attainment was relatively low, with 16.9% of women reporting no formal education and 39.5% reporting attainment at the preschool or primary school level. Over a quarter of the women (25.9%) reported being unable to read. The participants shared households with an average size of 4.9 members. With respect to their experience with the microfinance program, the average participant had been a member for 29.3 months, with an average loan size of 8478 Haitian Gourdes (approximately USD$135), and an average savings account size of 2128 Haitian Gourdes (approximately USD$34).
Table I.
Characteristics of the study population of 304 female Haitian microfinance clients from Okay, Haiti, 2017-2018.
| Health education training | ||||
|---|---|---|---|---|
| Total N=304 |
Yes N=75 |
No N=229 |
p1 | |
| Socio-demographic characteristics | ||||
| N (%) | N (%) | N (%) | ||
| Age | 0.2 | |||
| 20-29 | 69 (22.7) | 12 (16.0) | 57 (24.9) | |
| 30-39 | 127 (41.8) | 32 (42.7) | 95 (41.5) | |
| 40-49 | 108 (35.5) | 31 (41.3) | 77 (33.6) | |
| Marital status | 0.8 | |||
| Currently married | 164 (55.0) | 42 (57.5) | 122 (54.2) | |
| Divorced/separated | 26 (8.7) | 7 (9.6) | 19 (8.4) | |
| Never married | 108 (36.2) | 24 (32.9) | 84 (37.3) | |
| Missing | 6 | 2 | 4 | |
| Education | 0.3 | |||
| None | 51 (16.9) | 17 (22.0) | 34 (15.0) | |
| Preschool/Primary | 119 (39.5) | 26 (35.1) | 93 (40.0) | |
| HS or more | 131 (43.5) | 31 (41.9) | 100 (44.1) | |
| Missing | 3 | 1 | 2 | |
| Literacy | 0.6 | |||
| Yes | 223 (74.1) | 54 (72.0) | 169 (74.8) | |
| No | 78 (25.9) | 21 (28.0) | 57 (25.2) | |
| Missing | 3 | 0 | 3 | |
| Household asset quartile2 | 0.5 | |||
| Q1 | 75 (24.8) | 23 (31.1) | 52 (22.8) | |
| Q2 | 76 (25.2) | 18 (24.3) | 58 (25.4) | |
| Q3 | 75 (24.8) | 16 (21.6) | 59 (25.9) | |
| Q4 | 76 (25.2) | 17 (23.0) | 59 (25.9) | |
| Missing | 2 | 1 | 1 | |
| Mean (SD) | Mean (SD) | Mean (SD) | ||
| Household size | 4.9 (1.86) | 4.9 (1.66) | 4.9 (1.93) | 1.0 |
| Microfinance membership characteristics | ||||
| Mean (SD) | Mean (SD) | Mean (SD) | ||
| Duration of microfinance membership (months) | 29.3 (36.2) | 25.8 (27.4) | 30.4 (38.7) | 0.3 |
| Current loan size (Haitian gourdes3) | 8478 (7663.5) | 9747 (7579.9) | 8062 (7661.4) | 0.1 |
| Savings account balance (Haitian gourdes3) | 2128 (1885.2) | 2259 (1544.2) | 2085 (1985.4) | 0.5 |
| Sexual health outcomes | ||||
| N (%) | N (%) | N (%) | ||
| Condom use at last sex4 | 0.08 | |||
| Yes | 48 (20.7) | 18 (28.1) | 30 (17.9) | |
| No | 184 (79.3) | 46 (71.9) | 138 (82.1) | |
| Missing | 11 | 0 | 11 | |
| Condom use at last sex with unfaithful partner5 | 0.04 | |||
| Yes | 42 (21.5) | 17 (31.5) | 25 (17.7) | |
| No | 153 (78.5) | 37 (68.5) | 116 (82.3) | |
| Missing | 1 | 0 | 1 | |
| HIV test6 | <0.0001 | |||
| Yes | 158 (53.7) | 55 (73.3) | 103 (47.0) | |
| No | 136 (46.3) | 20 (26.7) | 116 (53.0) | |
| Missing | 10 | 0 | 10 | |
| Transactional sex7 | 0.7 | |||
| Yes | 112 (41.2) | 32 (43.2) | 80 (40.4) | |
| No | 160 (58.8) | 42 (56.8) | 118 (59.6) | |
| Missing | 32 | 1 | 31 | |
| STI diagnosis6 | 0.5 | |||
| Yes | 30 (10.8) | 6 (8.6) | 24 (11.5) | |
| No | 248 (89.2) | 64 (91.4) | 184 (88.5) | |
| Missing | 26 | 5 | 21 | |
| STI symptoms6 | 0.001 | |||
| Yes | 74 (25.0) | 8 (11.0) | 66 (29.6) | |
| No | 222 (75.0) | 65 (89.0) | 157 (70.4) | |
| Missing | 8 | 2 | 6 | |
p-value reported for chi-square test for categorical variables and t-test for continuous variables. P-values calculated among observations with non-missing values.
Measured by adding up the self-reported value (at time of purchase) of 20 key items in participant’s household
In January 2018 (midpoint of study), USD$1 was roughly equivalent to 62.5 Haitian gourdes
Among those with at least one sex partner in the last year (n=243)
Among those who endorsed that their most recent partner (in last 12 months) had sex with others or were unsure whether they had sex with others (n=196)
In last 12 months
Reports feeling obligated to have sex with most recent partner in return for gifts or money
One quarter (24.7%) of the participants reported receiving the health education training. Visual inspection of the geographic distribution of the health education training suggested it was similar to the overall distribution of the surveys we conducted (Figure II). This was confirmed statistically; no clusters were detected with our cluster analysis.
Figure II. Map of study site and geographic distribution of the household surveys and health education training.
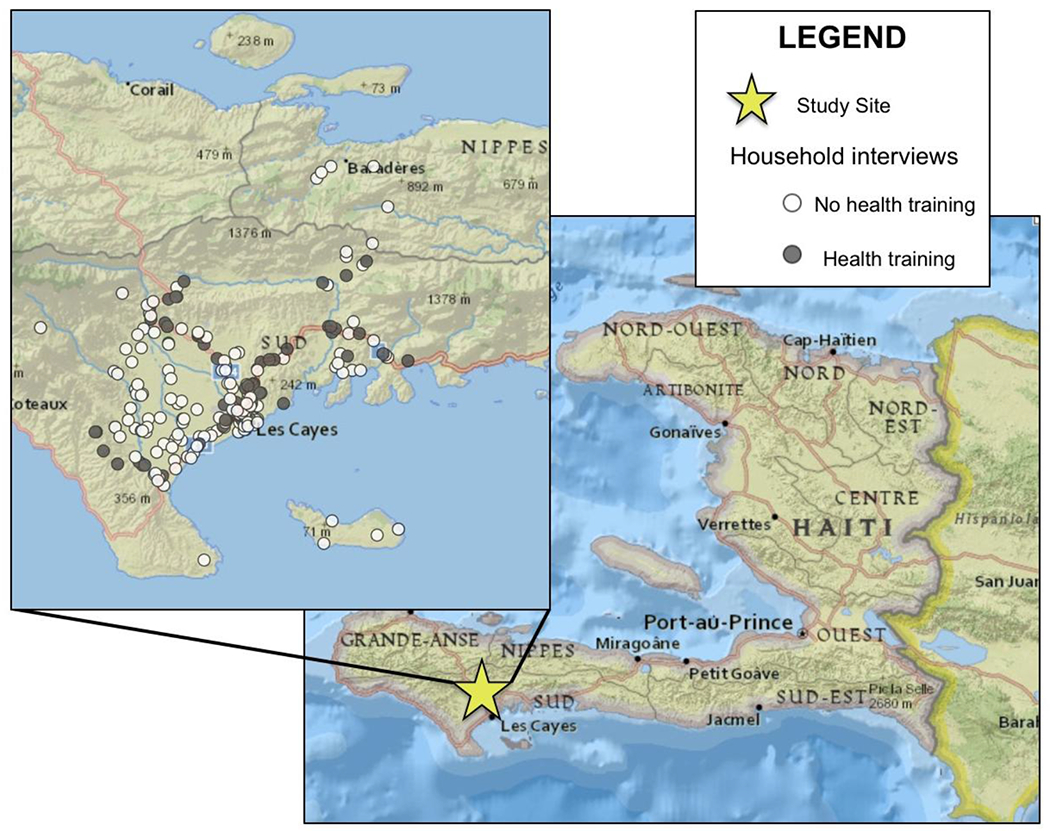
Sources: National Geographic, Esri, DeLorme, HERE, UNEP-WCMC, USGS, NASA, ESA, METI, NRCAN, GEBCO, NOAA, iPC
There were no significant sociodemographic differences between participants who received and did not receive the health education training. Women who received the training were similar to women who did not with respect to marital status, literacy status, household asset quartiles, household size, duration of Fonkoze membership, and savings account size. Although the differences were not statistically significant, women who received the training tended to be slightly older, slightly less educated, and had slightly larger loan sizes than women who did not receive the training.
Sexual behaviors and sexual risk outcomes reported by the participants were consistent with ongoing STI transmission (Table I). Only one-fifth of the participants reported using a condom at last sex (20.7%) and condom use did not markedly increase when they reported being unsure if their partner had outside sex partners (21.5%). Slightly more than half of the participants had been tested for HIV in the last 12 months (53.7%), while more than 40% reported feeling obligated to have sex with their partners in return for gifts or money (41.2%). A quarter of participants reported symptoms consistent with an STI in the last 12 months (25.0%), and just over 10% of the participants had been diagnosed with an STI in the last 12 months (10.8%).
Receipt of health education training was generally associated with less risky sexual behaviors (Table II). Women with health education training were 58% more likely to report condom use at last sex compared to women with no health education training [PR (95% CI): 1.58 (0.95, 2.62)], though the confidence intervals for this association included the null. When restricted to women whose partners may have had outside sex partners, receipt of health education training was associated more strongly with condom use at last sex [PR (95% CI): 1.78 (1.04, 3.02)]. Women who received health education training were 56% more likely to have recently tested for HIV [PR (95% CI): 1.56 (1.28, 1.90)], and 63% less likely to report recent STI symptoms [PR (95% CI): 0.37 (0.19, 0.73)]. No significant associations were observed between health education training and either transactional sex or STI diagnosis. After adjustment for age and education, the magnitudes of the associations were essentially unchanged.
Table II.
Relationship between receipt of health education training and sexual health outcomes
| Unadjusted | Age + education adjusted1 | |||||
|---|---|---|---|---|---|---|
| PR (95% CI) |
p | aPR (95% CI) |
p | |||
| Condom use at last sex2 | 1.58 | (0.95, 2.62) | 0.08 | 1.54 | (0.94, 2.55) | 0.09 |
| Condom use at last sex with unfaithful partner3 | 1.78 | (1.04, 3.02) | 0.03 | 1.70 | (1.00, 2.86) | 0.05 |
| HIV test4 | 1.56 | (1.28, 1.90) | <0.0001 | 1.50 | (1.23, 1.81) | <0.0001 |
| Transactional sex5 | 1.07 | (0.78, 1.46) | 0.7 | 1.08 | (0.79, 1.47) | 0.6 |
| STI diagnosis4 | 0.74 | (0.32, 1.74) | 0.5 | 0.73 | (0.31, 1.71) | 0.5 |
| STI symptoms4 | 0.37 | (0.19, 0.73) | 0.004 | 0.36 | (0.18, 0.72) | 0.004 |
Adjusted for age with cutpoint at above/below median age of 36 and for education with cutpoint at any versus no formal schooling
Among those with at least one sex partner in the last year (n=243)
Among those who endorsed that their most recent partner (in last 12 months) had sex with others or were unsure whether they had sex with others (n=196)
In last 12 months
Reports feeling obligated to have sex with most recent partner in return for gifts or money
Some differences existed in the associations by age and literacy status (Table III). The associations between health education training and the two condom use outcomes were particularly strong for older women (ages 36-49 years). For example, older women with health education training were more than two times as likely to have a recent HIV test compared to older women with no training [PR (95% CI): 2.05 (1.49, 2.82)] while the association for younger women was closer to the null: [PR (95% CI): 1.27 (0.99, 1.62)]. The associations between health education training also tended to be stronger among illiterate women, however these interactions were not statistically significant. For example, among illiterate women health education training was associated with a nearly 3.5 fold increase in condom use at last sex [PR (95% CI): 3.46 (1.05, 11.38)] while only a 30% increase among literate women [PR (95% CI): 1.29 (0.62, 2.29)]. The interaction terms between age and health education training were statistically different from zero for the following outcomes: Condom use at last sex with unfaithful partner (p=0.03) and HIV testing (p=0.02). None of the interaction terms between literacy and health education training were statistically different from zero at p<0.05, but the following outcomes were borderline significant: condom use at last sex (p=0.1) and condom use at last sex with unfaithful partner (p=0.09).
Table III.
Relationship between receipt of health education training and sexual health outcomes, stratified by age and literacy status
| Age 20-35 | Age 36-49 | Literate | Illiterate | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PR (95% CI) |
p | PR (95% CI) |
p | PR (95% CI) |
p | PR (95% CI) |
p | |||||
| Condom use at last sex1 | 1.15 | (0.60, 2.20) | 0.7 | 2.78 | (1.17, 6.60) | 0.02 | 1.29 | (0.72, 2.29) | 0.4 | 3.46 | (1.05, 11.38) | 0.04 |
| Wald p-value for interaction term |
0.1 | 0.1 | ||||||||||
| Condom use at last sex with unfaithful partner2 |
1.11 | (0.56, 2.22) | 0.8 | 4.40 | (1.62, 11.93) | 0.004 | 1.41 | (0.79, 2.50) | 0.2 | 6.00 | (1.62, 29.04) | 0.03 |
| Wald p-value for interaction term |
0.03 | 0.09 | ||||||||||
| HIV test3 | 1.27 | (0.99, 1.62) | 0.06 | 2.05 | (1.49, 2.82) | <0.0001 | 1.55 | (1.25, 1.91) | <0.0001 | 1.62 | (1.01, 2.61) | 0.05 |
| Wald p-value for interaction term |
0.02 | 0.9 | ||||||||||
| Transactional sex4 | 1.23 | (0.80, 1.87) | 0.3 | 0.95 | (0.60, 1.50) | 0.8 | 1.04 | (0.72, 1.50) | 0.8 | 1.09 | (0.60, 1.99) | 0.8 |
| Wald p-value for interaction term |
0.4 | 0.9 | ||||||||||
| STI diagnosis3 | 0.79 | (0.24, 2.62) | 0.7 | 0.71 | (0.21, 2.2.37) | 0.6 | 1.01 | (0.38, 2.63) | 0.6 | 0.30 | (0.04, 2.20) | 0.2 |
| Wald p-value for interaction term |
0.9 | 0.3 | ||||||||||
| STI symptoms3 | 0.21 | (0.05, 0.83) | 0.03 | 0.50 | (0.23, 1.09) | 0.08 | 0.41 | (0.19, 0.91) | 0.03 | 0.29 | (0.08, 1.15) | 0.08 |
| Wald p-value for interaction term |
0.3 | 0.7 | ||||||||||
Among those with at least one sex partner in the last year (n=243)
Among those who endorsed that their most recent partner (in last 12 months) had sex with others or were unsure whether they had sex with others (n=196)
In last 12 months
Reports feeling obligated to have sex with most recent partner in return for gifts or money
Discussion
In this study of 304 Haitian microfinance clients, we found that women who received health education training generally reported safer sexual health outcomes than women who did not. Even though the training was not exclusively focused on sexual health, we saw strong associations with specific sexual health outcomes. Women who received the training were over 50% more likely to use condoms, over 50% more likely to have a recent HIV test, and over 60% less likely to report recent STI symptoms. These findings add to the growing body of evidence that demonstrates the potential for microfinance programs to be used as an effective platform for health education delivery,(43–46) and provides the first evidence for the association in a Haitian microfinance context.
Some of the associations we observed were unexpectedly strong given the broad focus of the health education training. Even more targeted sexual health interventions have rarely demonstrated effect sizes of this magnitude.(47, 48) There are several potential explanations for this discrepancy. First, the health education training was integrated into a microfinance program. As noted previously, this integration could increase the effectiveness of health messages because they were conducted within a program designed to empower women and provide them with the financial resources needed to implement some sexual health improvement measures (e.g. purchase of condoms or travel to clinic for HIV testing).
Second, women in microfinance groups may be particularly receptive to self-help messages. Our study population consisted of women who had self-selected into the Fonkoze microfinance program. Women who are inclined to enroll in financial improvement programs like these may also be open to adopting behavior changes suggested in the trainings.
Finally, unmeasured and uncontrolled confounding could plausibly account for the strength of our findings if those who received the training differed systematically from those who did not. This concern is mitigated because health education training receipt appeared to be relatively exogenous to the individual participant. The decision to undergo health education training was made by the leaders of each client center, not individual participants. We did not collect data on the reasoning behind a center leader’s choice to engage in health education training. However, informal observations from Fonkoze staff reveal that the choice may be driven by the availability of the center chief to receive the initial training. This training requires an additional time commitment from the center chief of approximately two days a month. In line with this hypothesis of somewhat random allocation of the health education training exposure, we found no evidence for geographic or socio-demographic differences between the members who did and did not receive the training.
We also found that some of the associations between health education training and sexual health outcomes were stronger among older women and illiterate women. Specifically, for older women, the association was particularly strong between health education training and both condom use and HIV testing. Although the interaction was not statistically significant, illiterate women tended to have stronger associations between health education training and condom use. One potential explanation for these interactions is that older women and illiterate women may have particularly large room for improvement to be made by health education. Younger women and literate women may be more likely to already be exposed to the health messages presented in the training, either through formal education or through generational differences. Another potential explanation for these interactions is that the style of education delivery may have been particularly effective at reaching illiterate women.(49, 50) The health education training is centered around a picture-based handbook and verbal delivery of the content. Women without the ability to read would still be able to engage with and process the material of this educational training, though they may be excluded from more cognitive and literacy-demanding styles of education delivery. There has been a large focus on reaching young adults with HIV prevention and sexual health promotion messages, but it is also important to reach older adults, who may have differing educational backgrounds than young adults, with these messages.(51) Educational interventions like the one evaluated in this study that appear to be particularly effective in older women will be important to examine further.
Due to the design of the study, cautious interpretation of the findings is warranted. This was a cross-sectional study so the temporal relationship between receipt of the health education training and sexual health outcomes is not clear. This was also an observational study and the health education training was not randomly assigned. However, the way the health education training exposure was allocated appears to have been somewhat random in that socio-demographic covariates were balanced between those who did and did not receive the training. This finding, in concert with our sensitivity analysis adjusting for age and education, reduces the concern that our findings are biased due to confounding. Finally, all covariates of interest were self-reported in an interviewer administered quantitative survey. It is possible that interviewer bias and social desirability bias influenced our results, particularly given the sensitive nature of the sexual health outcomes. It is also possible that there is some misclassification of the health education training exposure as we did not finely assess the number of training sessions the clients received.
It is also possible that clustering of the data by client center could artificially inflate the precision of our estimates. Unfortunately, we did not collect identifying information about client center membership, so were unable to statistically test this hypothesis. However, the total number of client centers (n=229) was relatively large compared to our overall sample size (n=304), indicating that the size of each cluster would likely be small (average size=1.3). It is therefore unlikely that clustering would have a large effect on the standard errors of our effect estimates.
On the other hand, some of the design choices we used were stronger than common designs used in health education impact evaluation. We randomly sampled women from all clients of a Haitian microfinance branch office and obtained an extremely high participation rate (98.7%). Given this, we are confident that our study population was representative of the population from which we were sampling. Further, participants were not aware that we were evaluating the health education program as it was not the focus of the overall survey. The survey queried a broad array of topics, ranging from malaria to recent hurricane experience. Thus, participant responses about their sexual health outcomes were not likely to be affected by social desirability or response shift bias in ways that systematically differed by health education training status.
Conclusions
Our findings suggest that a simple, low-cost health education training program has the potential to improve sexual health outcomes when delivered using an existing microfinance program. The global HIV response costs more than $20 billion per year and between 15-25% of those funds are spent on HIV prevention.(52–54) Identifying more effective and sustainable modes of delivering prevention messages to vulnerable populations will be critical to reducing the global HIV burden.(55) We found that delivering prevention messages within a program designed to alleviate poverty has the potential to improve the impact of these programs on sexual health outcomes. The health education training program we evaluated was broad and covered topics beyond those focused on sexual and reproductive health. Perhaps more targeted sexual health educational programs could be even more effective at improving the sexual health of women in resource-poor settings. Future studies incorporating a longitudinal design and more objective measures of sexual health outcomes should be conducted to better understand the relationship between health education trainings conducted within a microfinance platform and the adoption of safer sexual practices.
Acknowledgments
The authors are very grateful to all involved in the field research and data collection activities including fieldworkers (Phidler Etienne, Donald Louis, Roltila Antoine, Keketie Ibo Nella Leopold), the Fonkoze Okay branch manager (Jn Moise Jean Pierre), and, most importantly, the study participants themselves. This project was supported by a Project Development Team within the Indiana CTSI NIH/NCRR (Grant Number UL1TR001108) and by the Indiana University Vice Provost for Research through the Faculty Research Support Program. Reginal Jules and Florence Jean-Louis are employed by Fonkoze. Molly Rosenberg, the corresponding author, had full access to the complete dataset, was responsible for data analysis, and had the final responsibility to decide to submit for publication.
REFERENCES
- 1.Coates TJ, Richter L, Caceres C. Behavioural strategies to reduce HIV transmission: how to make them work better. Lancet (London, England). 2008;372(9639):669–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Joint United Nations Programme on HIV/AIDS. The Gap Report. Geneva: UNAIDS; 2014. [Google Scholar]
- 3.UNAIDS. Country Fact Sheet: Haiti: 2017. [Available from: http://www.unaids.org/en/regionscountries/countries/haiti. [Google Scholar]
- 4.Republique D’Haïti Ministere de la Sante Publique et de la Population. Declaration d’engagement sur le VIH/sida: Rapport de situation nationale, Haïti. 2016. [Google Scholar]
- 5.Fawzi MS, Lambert W, Singler J, Koenig S, Leandre F, Nevil P, et al. Prevalence and risk factors of STDs in rural Haiti: implications for policy and programming in resource-poor settings. International journal of STD & AIDS. 2003;14(12):848–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jobe KA, Downey RF, Hammar D, Van Slyke L, Schmidt TA. Epidemiology of sexually transmitted infections in rural southwestern Haiti: the Grand’Anse Women’s Health Study. The American journal of tropical medicine and hygiene. 2014;91(5):881–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bristow CC, Desgrottes T, Cutler L, Cutler D, Devarajan K, Ocheretina O, et al. The aetiology of vaginal symptoms in rural Haiti. International journal of STD & AIDS. 2014;25(9):669–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fitzgerald DW, Behets F, Caliendo A, Roberfroid D, Lucet C, Fitzgerald JW, et al. Economic hardship and sexually transmitted diseases in Haiti’s rural Artibonite Valley. The American journal of tropical medicine and hygiene. 2000;62(4):496–501. [DOI] [PubMed] [Google Scholar]
- 9.Lo NC, Lowe A, Bendavid E. Abstinence funding was not associated with reductions in HIV risk behavior in sub-Saharan Africa. Health affairs. 2016;35(5):856–63. [DOI] [PubMed] [Google Scholar]
- 10.Institut Haïtien de l’Enfance (IHE) [Haïti] et ICF. 2016–2017 Enquête Mortalité, Morbidité et Utilisation des Services (EMMUS-VI): Indicateurs Clés. Rockville, Maryland, et Pétion- Ville, Haïti: IHE et ICF; 2017. [Google Scholar]
- 11.Cayemittes M, Busangu M, Bizimana J, Barrère B, Sévère B, Cayemittes V. Enquête Mortalité, Morbidité et Utilisation des Services, Haïti. 2012 Calverton, Maryland, USA: MSPP, IHE and ICF International; 2013. 2012. [Google Scholar]
- 12.Channon AA, Falkingham J, Matthews Z. Sexual and reproductive health and poverty. Social determinants of sexual and reproductive health. 2010:73. [Google Scholar]
- 13.Krishnan S, Dunbar MS, Minnis AM, Medlin CA, Gerdts CE, Padian NS. Poverty, gender inequities, and women’s risk of human immunodeficiency virus/AIDS. Annals of the New York Academy of Sciences. 2008;1136(1):101–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Agency CI. The World Factbook 2016: Central Intelligence Agency; 2016. [Google Scholar]
- 15.Dorjgochoo T, Noel F, Deschamps MM, Theodore H, Charles S, Dupont W, et al. Risk factors for HIV infection among Haitian adolescents and young adults seeking counseling and testing in Port-au-Prince. Journal of acquired immune deficiency syndromes (1999). 2009;52(4):498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Agha S, Kusanthan T. Equity in access to condoms in urban Zambia. Health Policy and Planning. 2003;18(3):299–305. [DOI] [PubMed] [Google Scholar]
- 17.Connell RW. Gender and power: Society, the person and sexual politics: Polity Press Cambridge; 1987. [Google Scholar]
- 18.Wamoyi J, Stobeanau K, Bobrova N, Abramsky T, Watts C. Transactional sex and risk for HIV infection in sub‐Saharan Africa: a systematic review and meta‐analysis. Journal of the international AIDS society. 2016;19(1):20992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Luke N, Goldberg RE, Mberu BU, Zulu EM. Social exchange and sexual behavior in young women’s premarital relationships in Kenya. Journal of Marriage and Family. 2011;73(5):1048–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pettifor A, Macphail C, Nguyen N, Rosenberg M. Can Money Prevent the Spread of HIV? A Review of Cash Payments for HIV Prevention. AIDS Behav. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rosenberg MS, Seavey BK, Jules R, Kershaw TS. The role of a microfinance program on HIV risk behavior among Haitian women. AIDS and Behavior. 2011;15(5):911–8. [DOI] [PubMed] [Google Scholar]
- 22.Isangula KG. Improving women and family’s health through integrated microfinance, health education and promotion in rural areas. Journal of sustainable development. 2012;5(5):76. [Google Scholar]
- 23.Hargreaves JR, Delany-Moretlwe S, Hallett TB, Johnson S, Kapiga S, Bhattacharjee P, et al. The HIV prevention cascade: integrating theories of epidemiological, behavioural, and social science into programme design and monitoring. The lancet HIV. 2016;3(7):e318–e22. [DOI] [PubMed] [Google Scholar]
- 24.Pomeranz D The Promise of Microfinance and Women’s Empowerment: What Does the Evidence Say? Netherlands: Ernst & Young Study Google Scholar. 2014. [Google Scholar]
- 25.Leatherman S, Metcalfe M, Geissler K, Dunford C. Integrating microfinance and health strategies: examining the evidence to inform policy and practice. Health policy and planning. 2012;27(2):85–101. [DOI] [PubMed] [Google Scholar]
- 26.Maes J, Reed L. State of the microcredit summit campaign report 2012. Washington, DC: MCS; 2012. [Google Scholar]
- 27.Witte SS, Aira T, Tsai LC, Riedel M, Offringa R, Chang M, et al. Efficacy of a savings-led microfinance intervention to reduce sexual risk for HIV among women engaged in sex work: a randomized clinical trial. American journal of public health. 2015;105(3):e95–e102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spielberg F, Crookston BT, Chanani S, Kim J, Kline S, Gray BL. Leveraging microfinance to impact HIV and financial behaviors among adolescents and their mothers in West Bengal: a cluster randomized trial. International journal of adolescent medicine and health. 2013;25(2):157–66. [DOI] [PubMed] [Google Scholar]
- 29.Pronyk PM, Kim JC, Abramsky T, Phetla G, Hargreaves JR, Morison LA, et al. A combined microfinance and training intervention can reduce HIV risk behaviour in young female participants. AIDS (London, England). 2008;22(13):1659–65. [DOI] [PubMed] [Google Scholar]
- 30.Arrivillaga M, Salcedo JP, Pérez M. The IMEA project: an intervention based on microfinance, entrepreneurship, and adherence to treatment for women with HIV/AIDS living in poverty. AIDS Education and Prevention. 2014;26(5):398–410. [DOI] [PubMed] [Google Scholar]
- 31.Stratford D, Mizuno Y, Williams K, Courtenay-Quirk C, O’leary A. Addressing poverty as risk for disease: recommendations from CDC’s consultation on microenterprise as HIV prevention. Public health reports. 2008;123(1):9–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lorenzetti LM, Leatherman S, Flax VL. Evaluating the effect of integrated microfinance and health interventions: an updated review of the evidence. Health policy and planning. 2017;32(5):732–56. [DOI] [PubMed] [Google Scholar]
- 33.Tucker M, Tellis W. Microfinance Institutions in Transition: Fonkoze in Haiti Moves toward Regulated Banking Status. ESR Review. 2005;7(2):101. [Google Scholar]
- 34.UNICEF, WHO, UNESCO, UNFPA, UNDP, UNAIDS, et al. Facts for life, 4th Edition: UNICEF; 2010. [Google Scholar]
- 35.Abels MD, Blignaut RJ. Sexual-risk behaviour among sexually active first-year students at the University of the Western Cape, South Africa. Ajar-Afr J Aids Res. 2011;10(3):255–61. [DOI] [PubMed] [Google Scholar]
- 36.Chatterji M, Murray N, London D, Anglewicz P. The factors influencing transactional sex among young men and women in 12 sub-saharan African countries. Soc Biol. 2005;52(1–2):56–72. [DOI] [PubMed] [Google Scholar]
- 37.Cluver L, Orkin M, Boyes M, Gardner F, Meinck F. Transactional Sex Amongst AIDS-Orphaned and AIDS-Affected Adolescents Predicted by Abuse and Extreme Poverty. Jaids-J Acq Imm Def. 2011;58(3):336–43. [DOI] [PubMed] [Google Scholar]
- 38.Jewkes R, Morrell R, Sikweyiya Y, Dunkle K, Penn-Kekana L. Transactional relationships and sex with a woman in prostitution: prevalence and patterns in a representative sample of South African men. BMC public health. 2012;12:325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ranganathan M, Heise L, Pettifor A, Silverwood RJ, Selin A, MacPhail C, et al. Transactional sex among young women in rural South Africa: prevalence, mediators and association with HIV infection. Journal of the International Aids Society. 2016;19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wamoyi J, Stoebenau K, Kyegombe N, Heise L, Ranganathan M. STRIVE Technical Brief: Transactional sex and HIV risk. Washington, DC: International Center for Research on Women; 2018. [Google Scholar]
- 41.SAS. 9.4 ed. Cary, NC: SAS Institute Inc.; 2014. [Google Scholar]
- 42.Kulldorff M A Spatial Scan Statistic In Communications in Statistics-Theory and Methods 26, 1481–1496. ACM, New York, NY. 1997. [Google Scholar]
- 43.Lorenzetti LMJ, Leatherman S, Flax VL. Evaluating the effect of integrated microfinance and health interventions: an updated review of the evidence. Health Policy Plan. 2017;32(5):732–56. [DOI] [PubMed] [Google Scholar]
- 44.Kim J, Ferrari G, Abramsky T, Watts C, Hargreaves J, Morison L, et al. Assessing the incremental effects of combining economic and health interventions: the IMAGE study in South Africa. Bulletin of the World Health Organization. 2009;87:824–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dunford C Building better lives: Sustainable integration of microfinance and education in child survival, reproductive health, and HIV/AIDS prevention for the poorest entrepreneurs. Journal of Microfinance/ESR Review. 2001;3(2):2. [Google Scholar]
- 46.Hamad R, Fernald LC, Karlan DS. Health education for microcredit clients in Peru: a randomized controlled trial BMC public health. 2011;11(1):51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mwale M, Muula A. Systematic review: a review of adolescent behavior change interventions [BCI] and their effectiveness in HIV and AIDS prevention in sub-Saharan Africa. BMC public health. 2017;17(1):718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.AJ Scott-Sheldon L, Walstrom P, Harrison A, C Kalichman S, P Carey M. Sexual risk reduction interventions for HIV prevention among South AfricanYouth: a meta-analytic review. Current HIV research. 2013;11(7):549–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Peregrin T Picture this: visual cues enhance health education messages for people with low literacy skills. Journal of the American Dietetic Association. 2010;110(5):S28–S32. [DOI] [PubMed] [Google Scholar]
- 50.Garcia-Retamero R, Cokely ET. Communicating health risks with visual aids. Current Directions in Psychological Science. 2013;22(5):392–9. [Google Scholar]
- 51.Rosenberg MS, Gómez-Olivé FX, Rohr JK, Houle BC, Kabudula CW, Wagner RG, et al. Sexual Behaviors and HIV Status: A Population-Based Study Among Older Adults in Rural South Africa. Journal of acquired immune deficiency syndromes (1999). 2017;74(1):e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Arán-Matero D, Amico P, Arán-Fernandez C, Gobet B, Izazola-Licea JA, Avila-Figueroa C. Levels of spending and resource allocation to HIV programs and services in Latin America and the Caribbean. PloS one. 2011;6(7):e22373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Stover J, Bollinger L, Izazola JA, Loures L, DeLay P, Ghys PD, et al. What is required to end the AIDS epidemic as a public health threat by 2030? The cost and impact of the fast-track approach. PloS one. 2016;11(5):e0154893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Poku NK. UN political declaration on HIV and AIDS: where to begin? The Lancet. 2016;388(10046):743–4. [DOI] [PubMed] [Google Scholar]
- 55.Isbell MT, Kilonzo N, Mugurungi O, Bekker L-G. We neglect primary HIV prevention at our peril. The Lancet HIV. 2016;3(7):e284–e5. [DOI] [PubMed] [Google Scholar]


