Abstract
Background/Aims:
We evaluated relationships between visual acuity and eye-related quality of life (ER-QOL) and functional vision in children, across a spectrum of pediatric eye conditions, using the Pediatric Eye Questionnaire (PedEyeQ).
Design:
Cross-sectional study
Methods:
397 children (aged 5 to 11 years) with an eye condition and 104 visually normal controls, completed the Child PedEyeQ (Functional vision, Bothered by Eyes/Vision, Social, and Frustration/Worry domains). One parent for each child completed the Proxy PedEyeQ (same domains as Child plus Eye care) and Parent PedEyeQ (Impact on Parent and Family, Worry about Child’s Eye Condition, Worry about Child’s Self-perception and Interactions, Worry about Functional Vision domains). Each domain was Rasch-scored and Spearman rank correlations calculated to evaluate relationships between better-seeing-eye and worse-seeing-eye visual acuity and PedEyeQ domain score.
Results:
There was a significant relationship between poorer better-seeing-eye visual acuity and lower (worse) PedEyeQ score on 2 of 4 Child domains (e.g., Functional Vision: r=−0.1474 ; P=.005), on 2 of 5 Proxy PedEyeQ domains (e.g., Functional Vision: r=−0.2183; P<.001) and on 2 of 4 Parent PedEyeQ domains (e.g., Impact on parent and family r=−0.1607 ; P=.001). Worse-seeing eye visual acuity was associated with lower PedEyeQ scores across all Child, Proxy and Parent domains (P<.01 for each) with the exception of the Child Social domain (P=.15).
Conclusions:
Both better-seeing-eye and worse-seeing-eye visual acuity were associated with functional vision and ER-QOL in children, assessed using the PedEyeQ, although other factors may also influence relationships. These data further validate using the PedEyeQ across pediatric eye conditions.
INTRODUCTION
Previous studies have reported that children with visual impairment have reduced functional vision and quality of life compared with visually normal controls, using analytic methods that dichotomize subjects with and without visual impairment.1-5 Others have reported no association between visual acuity and functional vision.6 Birch and colleages7 reported a significant effect of severity of visual acuity deficit on some functional vision domains but did not study quality of life. Most studies have assumed that everyday visual function reflects primarily the visual acuity of the better-seeing eye, and have therefore assigned children to visual impairment categories based soley on better-seeing-eye visual acuity. Nevertheless some studies in adults have highlighted the contributions of both the better-seeing and worse-seeing-eye visual acuity to functional vision and quality of life.8-13 In the present study we evaluated the relationship between better-seeing-eye and worse-seeing-eye visual acuity and functional vision and specific domains of eye-related quality of life (ER-QOL), by evaluating children across the spectrum of eye conditions, with a wide range of visual acuities, using the recently reported, patient-derived Pediatric Eye Questionnaire (PedEyeQ).14
METHODS
Approval for this for this prospective, cross-sectional study was obtained from Institutional Review Boards at the Mayo Clinic, Rochester, Minnesota, and the University of Texas Southwestern Medical Center, Dallas, Texas. All procedures and data collection were conducted in a manner compliant with the Health Insurance Portability and Accountability Act, and all research procedures adhered to the tenets of the Declaration of Helsinki. Informed consent and informed assent were obtained as required by local IRBs. Both the child and one of their parents were enrolled.
Subjects
Three-hundred ninety-seven children aged 5 to 11 years, with a range of different eye conditions were prospectively enrolled. Primary eye disease type was determined based on review of the medical record and classified as either: amblyopia, anterior segment, central nervous system conditions affecting vision, esotropia, exotropia, hypertropia, nystagmus, orbital and external conditions, refractive error, retina, or optic nerve. Seventy-seven (19%) of these 397 were reported in previous studies of strabismus,15 glasses for refractive error,16 or bilateral moderate/severe visual impairment.1 Nevertheless, in these previous studies we did not specifically analyze associations with different levels of visual acuity deficit. Visually normal control subjects (n=104; aged 5 to 11 years) were also enrolled, with normal visual acuity for age17, 18 and no current or previous eye condition or treatment (including no current or previous glasses). Ninety-one (88%) of these 104 visually normal children have been reported in previous studies.1, 15, 16
Classification of visual acuity for subjects with an eye condition
Included subjects had visual acuity tested for each eye separately, in habitual refractive correction, using age-appropriate tests. If Teller acuity cards were used (due to developmental delay; N=8), values were converted to logMAR for analysis. If visual acuity was too poor to quantify by optotypes (N=13 eyes), we assigned logMAR scores for non-parametric analysis as follows: hand motions 1.9 logMAR, light perception 2.0 logMAR, no light perception 2.1 logMAR.
In separate analyses of better-seeing eye and worse-seeing eye, subjects were assigned to one of four visual acuity categories:. (1) normal visual acuity in the presence of any eye condition (including refractive error only), defined as meeting previously published normal visual acuity criteria (20/32 or better for 5- to 6- year-olds and 20/25 or better for 7- to 11-year-olds17, 18); (2) worse than 20/32 to 20/70 for 5- to 6-year-olds and worse than 20/25 to 20/70 for 7- to 11-year-olds (below normal for age17, 18); (3) worse than 20/70 to better than or equal to 20/200; (4) worse than 20/200. Categories 3 and 4 correspond to World Health Organization criteria (https://icd.who.int/browse11/l-m/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f11036676).
The Pediatric Eye Questionnaire (PedEyeQ)
The patient-derived PedEyeQ14 consists of Child, Proxy and Parent components, each with distinct domains, and utilizes a 3-point frequency scale for responses: “never,” “sometimes,” and “all of the time”14 (full questionnaires, with Rasch scoring look up tables, freely available at: https://public.jaeb.org/pedig/view/Other_Forms). Children completed the Child PedEyeQ, and one parent or legal guardian for each child completed the Proxy and Parent PedEyeQ. The Child 5- to 11-year-old PedEyeQ consists of one Functional Vision domain, and three distinct ER-QOL domains: Bothered by eyes/vision, Social, and Frustration/Worry.14 The Proxy 5- to 11-year-old PedEyeQ consists of one Functional Vision domain, and three ER-QOL domains: Bothered by Eyes/Vision, Social, Frustration/Worry, and Eye care.14 The Parent PedEyeQ has 4 distinct quality of life domains: Impact on Parent and Family, Worry about Child’s Eye Condition, Worry about Child’s Self-perception and Interactions, and Worry about Child’s Functional Vision.14
Analysis
For all PedEyeQ analyses, Rasch domain scores were calculated and converted to 0 (worst) to 100 for interpretation. The median, 25th and 75th quartiles, and range of PedEyeQ domain scores were calculated for each visual acuity category, for better-seeing eye and worse-seeing eye separately, and for normal control children (for reference only). Spearman rank correlations were calculated for each PedEyeQ domain with better-seeing-eye visual acuity and worse-seeing-eye visual acuity (as separate potential correlative factors) excluding visually normal controls. In secondary analyses, we repeated evaluation of correlations with worse-seeing-eye visual acuity, limiting the analyses to children with normal better-seeing-eye visual acuity (n=310 of 397 with an eye condition). SAS software version 9.4 (SAS Institute. Cary, NC) was used for all statistical analyses.
RESULTS
For the 397 children with eye conditions, and 104 visually normal controls, demographics are shown in Table 1. Regarding broad diagnostic category for children with eye conditions, 94 (24%) had a primary diagnosis of amblyopia, 61 (15%) anterior segment condition, 9 (2%) central nervous system conditions affecting vision, 60 (15%) esotropia, 38 (10%) exotropia, 20 (5%) hypertropia, 21 (5%) nystagmus, 16 (4%) orbital and external conditions, 53 (13%) refractive error, and 25 (6%) retina and optic nerve condition.
Table 1.
Demographics and Clinical Characteristics of 397 Children With Eye Conditions and 104 Visually Normal Controls Completing the Pediatric Eye Questionnaire, and Their Parents.
| Children with Eye Conditions (n=397) N (%) |
Visually Normal Controls (n=104) N (%) |
|
|---|---|---|
| Sex of child | ||
| Female | 202 (51) | 53 (51) |
| Race | ||
| White (including Hispanic / Latino) | 322 (81) | 80 (77) |
| Asian | 30 (8) | 11 (11) |
| More than 1 race | 24 (6) | 9 (9) |
| Black/African American | 11 (3) | 3 (3) |
| American Indian / Alaskan Native | 6 (2) | 0 (0) |
| Native Hawaiian / Other Pacific Islander | 0 (0) | 0 (0) |
| Other | 4 (1) | 0 (0) |
| Not reported | 0 (0) | 1 (1) |
| Ethnicity | ||
| Not Hispanic / Latino and not Middle Eastern/North African and not Indian Subcontinent | 322 (81) | 88 (85) |
| Hispanic / Latino | 42 (11) | 6 (6) |
| Indian Subcontinental | 17 (4) | 1 (1) |
| Middle Eastern / North African | 2 (1) | 2 (2) |
| More than one | 14 (4) | 6 (6) |
| Not reported | 0 (0) | 1 (1) |
| Developmental Delay present | 47 (12) | 0 (0) |
| Parent / Legal Guardian Completing Questionnaires | ||
| Mother | 317 (80) | 92 (88) |
| Father | 77 (19) | 11 (11) |
| Legal guardian | 3 (1) | 0 (0) |
| Not reported | 0 (0) | 1 (1) |
| Parent / Legal Guardian Age | ||
| Under 21 | 1 (<1) | 0 (0) |
| 21 to 30 | 30 (8) | 5 (5) |
| 31 to 40 | 218 (55) | 63 (61) |
| 41 to 50 | 134 (34) | 35 (34) |
| 51 to 60 | 11 (3) | 0 (0) |
| Over 60 | 3 (1) | 0 (0) |
| Not reported | 0 (0) | 1 (1) |
| Parent / Legal Guardian Highest Level of Education | ||
| Attended high school | 14 (4) | 0 (0) |
| High school graduate | 30 (8) | 2 (2) |
| Attended college | 69 (17) | 19 (18) |
| College graduate | 186 (47) | 59 (57) |
| Post-graduate / professional degree | 95 (24) | 23 (22) |
| Not reported | 3 (1) | 1 (1) |
| Housing | ||
| Own | 333 (84) | 86 (83) |
| Rent | 57 (14) | 16 (15) |
| Other | 5 (1) | 1 (1) |
| Not reported | 2 (1) | 1 (1) |
| Number of parents in home | ||
| 1 | 56 (14) | 11 (11) |
| 2 | 341 (86) | 93 (89) |
Better-seeing-eye visual acuity was classified as category 1 for 310 (78%), category 2 for 61 (15%), category 3 for 12 (3%), and category 4 for 14 (4%). Worse-seeing-eye visual acuity was classified as category 1 for 128 (32%), category 2 for 176 (44%), category 3 for 60 (15%), and category 4 for, 33 (8%). There was a significant correlation between better-seeing-eye and worst-seeing-eye visual acuity (n=397, R=0.6374, P < .001). Overall 29 (7%) children with eye conditions were unable to complete Child questionnaires due to developmental delay.
Relationship between better-seeing eye visual acuity and PedEyeQ domain scores
There was a significant relationship between poorer better-seeing-eye visual acuity and lower (worse) Child PedEyeQ scores in 2 of the 4 domains (functional vision and bothered by eyes/vision domains, P<.04 for each domain, Table 2). We did not identify an association with visual acuity for the Child PedEyeQ frustration/worry or social domains (P>.6 for each, Table 2). In general, median Child PedEyeQ scores were lower for children with poorer visual acuity (Figure 1A-D). For the Proxy PedEyeQ, there was a significant relationship between poorer better-seeing eye visual acuity and lower scores for the Functional Vision and Bothered by Eyes/Vision domains (P<.009 for each, Table 2) but not for the Frustration/Worry, Social and Eye Care domains (P>.43 for each, Table 2). Median Proxy PedEyeQ scores tended to be lower in groups with poorer better-seeing eye visual acuity (Figure 2 A-E). For the Parent PedEyeQ there was a significant relationship between poorer child visual acuity and lower parental quality of life on the Impact on Parent and Family and Worry about Child’s Functional Vision domains (P≤.006 for each, Table 2), but not on the other 2 domains (P ≥.21 for each, Table 2). In general, median scores were lower in groups with poorer visual acuity (Figure 3 A-D).
Table2.
Association of PedEyeQ domain scores with better-seeing eye and worse-seeing-eye visual acuity, assessed using Spearman rank correlations, across 397 children with eye conditions.
| PedEyeQ domains | Spearman rank correlation (P value) |
|||
|---|---|---|---|---|
| Better-seeing eye VA | Worse-seeing eye VA | |||
| Rho (95% CI) | P-value | Rho (95% CI) | P-value | |
| Child PedEyeQ 5-11 years domains | n=368* | n=368* | ||
| Functional vision | −0.1474 (−0.2459, −0.0458) |
.005 | −0.2298 (−0.3244, −0.1306) |
<.001 |
| Bothered by eyes / vision | −0.1079 (−0.2079, −0.0058) |
.04 | −0.1499 (−0.2483, −0.0484) |
.004 |
| Social | 0.0265 (−0.0760, 0.1283) |
.61 | −0.0751 (−0.1760, 0.0273) |
.15 |
| Frustration / worry | 0.0003 (−0.1020, 1025) |
>.99 | −0.1322 (−0.2313,−0.0304) |
.01 |
| Proxy PedEyeQ 5-11 years domains | n=397 | n=397 | ||
| Functional vision | −0.2183 (−0.3100, −0.1225) |
<.001 | −0.4142 (−0.4926, −0.3292) |
<.001 |
| Bothered by eyes / vision | −0.1315 (−0.2270, −0.0335) |
.009 | −0.3278 (−0.4129, −0.2370) |
<.001 |
| Social | 0.0209 (−0.0777, 0.1191) |
.68 | −0.1625 (−0.2568, −0.0651) |
.001 |
| Frustration / worry | 0.0397 (−0.0590, 0.1375) |
.43 | −0.2037 (−0.2962, −0.1074) |
<.001 |
| Eye care | 0.0275 (−0.0711, 0.1256) |
.58 | −0.2273 (−0.3186, −0.1318) |
<.001 |
| Parent PedEyeQ domains | n=397 | n=397 | ||
| Impact on parent and family | −0.1607 (−0.2551, −0.0633) |
.001 | −0.3590 (−0.4418, −0.2701) |
<.001 |
| Worry about child’s eye condition | −0.0602 (−0.1577, 0.0384) |
.23 | −0.3567 (−0.4397, −0.2676) |
<.001 |
| Worry about child’s self-perception and interactions | −0.0635 (−0.1609, 0.0351) |
.21 | −0.2230 (−0.3146, −0.1274) |
<.001 |
| Worry about child’s functional vision | −0.1370 (−0.2323, −0.0391) |
.006 | −0.3171 (−0.4030, −0.2258) |
<.001 |
29 of 397 children were unable to complete the Child PedEyeQ
Figure 1:
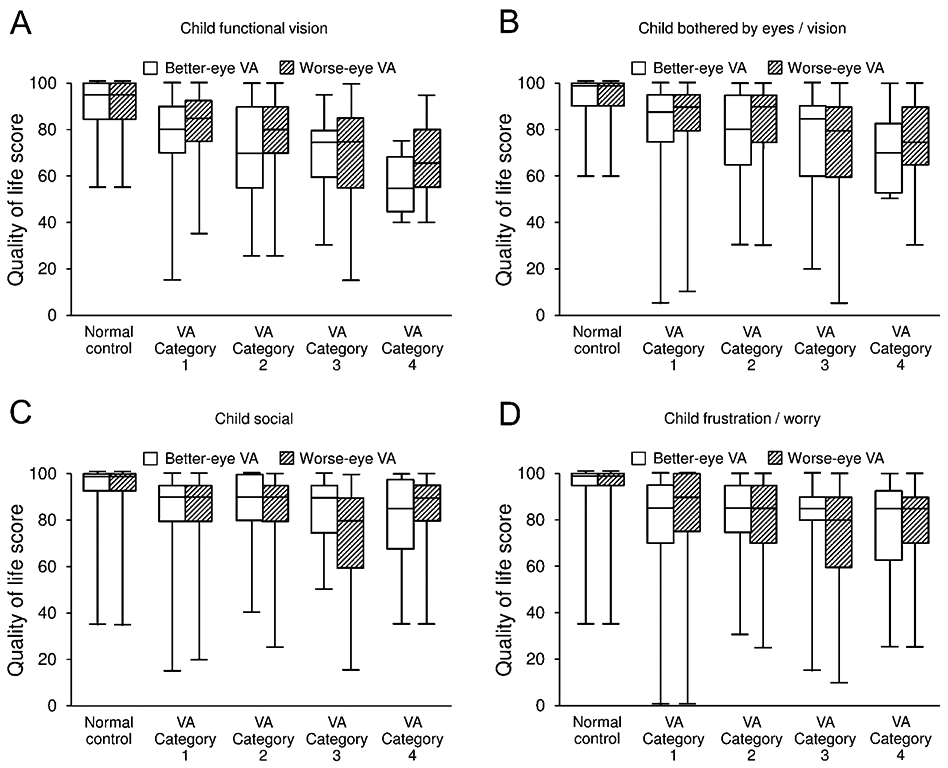
Child 5- to 11-year-old PedEyeQ median domain scores (functional vision, bothered by eyes/vision, social, and frustration / worry) showing classification by better-seeing-eye visual acuity and by worse-seeing-eye visual acuity. Boxes represent 1st quartile, median and 3rd quartile values; whiskers represent extreme values.
VA Category 1 = Normal visual acuity in the presence of an eye condition (20/32 or better for 5-to 6-year-olds and 20/25 or better for 7- to 11-year-olds). VA Category 2 = worse than 20/32 to 20/70 for 5- to 6-year-olds and worse than 20/25 to 20/70 for 7- to 11-year-olds (below age norms). VA Category 3 = worse than 20/70 to better than or equal to 20/200. VA Category 4 = worse than 20/200.
Figure 2:
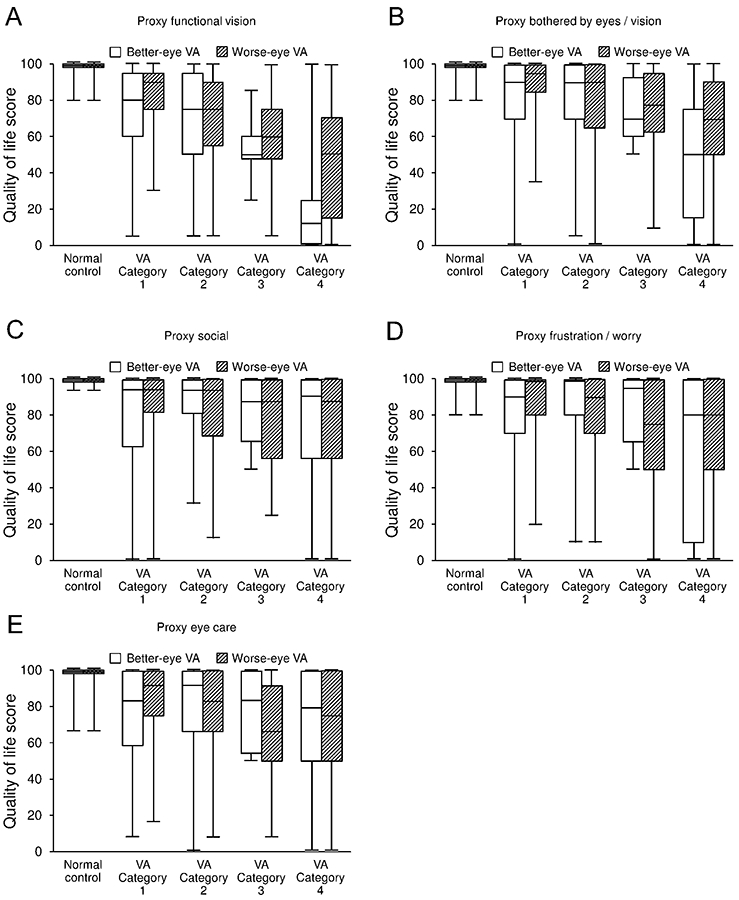
Proxy 5- to 11-year-old PedEyeQ median domain scores (functional vision, bothered by eyes / vision, social, frustration / worry, and eye care) showing classification by better-seeing-eye visual acuity and by worse-seeing-eye visual acuity. Boxes represent 1st quartile, median and 3rd quartile values; whiskers represent extreme values.
VA Category 1 = Normal visual acuity in the presence of an eye condition (20/32 or better for 5-to 6-year-olds and 20/25 or better for 7- to 11-year-olds). VA Category 2 = worse than 20/32 to 20/70 for 5- to 6-year-olds and worse than 20/25 to 20/70 for 7- to 11-year-olds (below age norms). VA Category 3 = worse than 20/70 to better than or equal to 20/200. VA Category 4 = worse than 20/200.
Figure 3:
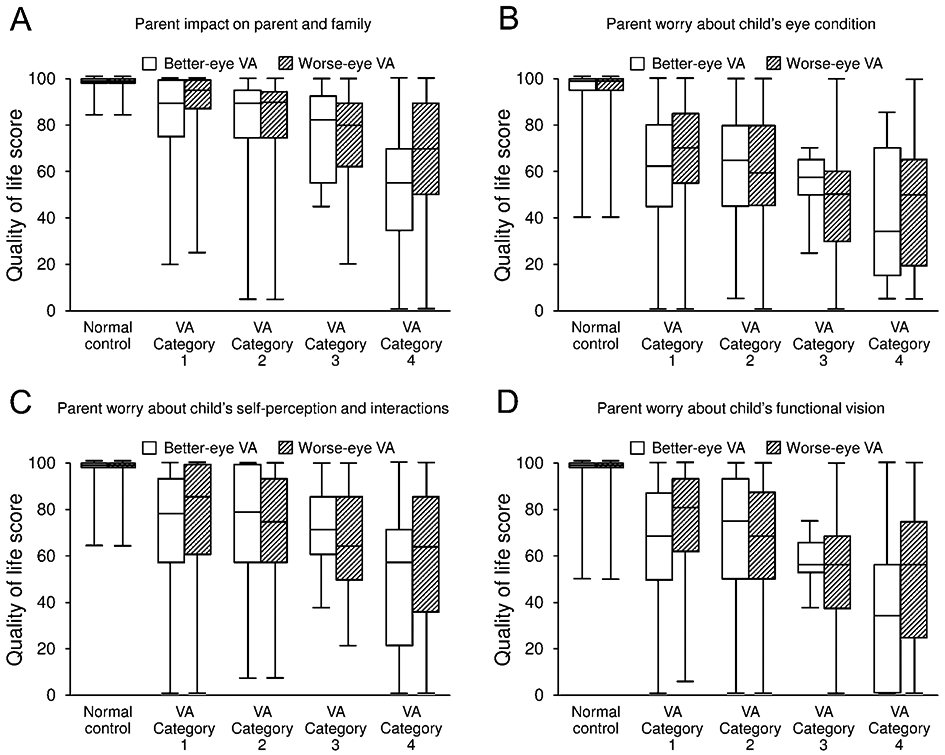
Parent PedEyeQ median domain scores (impact on parent and family, worry about child’s eye condition, worry about self-perception and interactions, and worry about functional vision) showing classification by child’s better-seeing-eye visual acuity and by child’s worse-seeing-eye visual acuity. Boxes represent 1st quartile, median and 3rd quartile values; whiskers represent extreme values.
VA Category 1 = Normal visual acuity in the presence of an eye condition (20/32 or better for 5-to 6-year-olds and 20/25 or better for 7- to 11-year-olds). VA Category 2 = worse than 20/32 to 20/70 for 5- to 6-year-olds and worse than 20/25 to 20/70 for 7- to 11-year-olds (below age norms). VA Category 3 = worse than 20/70 to better than or equal to 20/200. VA Category 4 = worse than 20/200.
Relationship between worse-seeing-eye visual acuity and PedEyeQ domain scores
There was a significant relationship between poorer worse-seeing-eye visual acuity and lower (worse) scores for 3 of the 4 Child PedEyeQ domains (P≤.01 for each, Table 2) but no significant relationship on the Social domain (P=.15, Table 2). Median scores tended to be lower in children with poorer worse-seeing-eye visual acuity (Figure 1 A-D). For each of the 5 Proxy PedEyeQ domains there was a significant relationship between poorer worse-seeing-eye visual acuity and lower (worse) scores (P<.001 for each, Table 1) with lower median scores for children with poorer worse-seeing-eye visual acuity (Figure 2 A-E). For each of the 4 Parent PedEyeQ domains there was a significant relationship between poorer worse-seeing-eye visual acuity and lower (worse) scores (P<.001 for each, Table 2), again with lower median scores in subjects with poorer visual acuity (Figure 3 A-D).
When we limited the analysis to the 310 subjects with normal better-seeing-eye visual acuity (only 87 [28%] of whom had a primary diagnosis of amblyopia), we also found significant correlations with worse-seeing-eye visual acuity across all Proxy and Parent PedEyeQ domains (P<.001 for each, Table 3) and on the functional vision and frustration/worry domains of the Child PedEyeQ (P<.02, Table 3).
Table 3.
Association of PedEyeQ domain scores with worse-seeing-eye visual acuity, assessed using Spearman rank correlations, in children with normal better-seeing eye visual acuity (310 children with eye conditions).
| PedEyeQ domains | Rho (95% CI) | P-value |
|---|---|---|
| Child PedEyeQ 5-11 years domains | n=302* | |
| Functional vision | −0.1561 (−0.2643, −0.0440) | .007 |
| Bothered by eyes / vision | −0.1017 (−0.2121, 0.113) | .08 |
| Social | −0.0814 (−0.1925, 0.0318) | .16 |
| Frustration / worry | −0.1350 (−0.2441, −0.0225) | .02 |
| Proxy PedEyeQ 5-11 years domains | n=310 | |
| Functional vision | −0.3545 (−0.4482, −0.2531) | <.001 |
| Bothered by eyes / vision | −0.3031 (−0.4009, −0.1984) | <.001 |
| Social | −0.1946 (−0.2995, −0.0851) | <.001 |
| Frustration / worry | −0.2376 (−0.3400, −0.1296) | <.001 |
| Eye care | −0.2839 (−0.3831, −0.1781) | <.001 |
| Parent PedEyeQ domains | n=310 | |
| Impact on parent and family | −0.3212 (−0.4176, −0.2176) | <.001 |
| Worry about child’s eye condition | −0.3825 (−0.4737, −0.2832) | <.001 |
| Worry about child’s self-perception and interactions | −0.2245 (−0.3277, −0.1160) | <.001 |
| Worry about child’s functional vision | −0.3025 (−0.4004, −0.1978) | <.001 |
8 of 310 children were unable to complete the Child PedEyeQ
DISCUSSION
In this large prospective study, we found an overall association of poorer better-seeing-eye visual acuity with worse functional vision scores and with worse specific ER-QOL domain scores, across the range of visual acuity deficits in children.In addition we found an overall association of poorer worse-seeing-eye visual acuity with worse functional vision scores and worse specific ER-QOL domain scores, across the range of visual acuity deficits in children. Child visual acuity was also associated with lower quality of life for the parent themselves. The validity and clinical utility of the PedEyeQ was initially reported in our prior study1 of children with bilateral visual impairment. In the present study, the correlations of visual acuity and PedEyeQ domain scores, across the range of visual acuity deficits, now further support the validity and clinical utility of the PedEyeQ.
Comparison of our results with those of previous studies is challenging because different instruments were used in prior studies; some evaluated functional vision, whereas others evaluated specific quality of life domains. Even when ostensibly measuring the same construct, differences in items and scoring limit direct comparison of findings. In addition, many of the instruments were designed to target vision-related concerns (VR-QOL) particularly in the context of bilateral visual impairment, while ours was designed to target a wider range of eye-related concerns (ER-QOL), including eye conditions that may or may not affect visual acuity. As a result, our discussion of previous studies (using instruments other than the PedEyeQ), is intended to provide general context, rather than direct comparison.
Most previous studies evaluating the relationship between visual acuity and quality of life do so by dichotomizing between children with visual impairment and visually normal controls.1-5 Bathelt and colleagues5 divided visual impairment into mild/moderate versus severe/profound and found significantly lower scores for both categories of visually impaired children compared with controls on most domains of the generic Proxy Pediatric Quality of Life Inventory (PedsQL). Birch and colleagues7 compared Children’s Visual Function Questionnaire (CVFQ) scores across five discrete visual acuity categories and found a significant effect of visual acuity category on some CVFQ subscales, but did not explore impact on quality-of-life domains. In previous studies evaluating correlations between visual acuity and quality of life, Chadha and Subramanian2 found a moderate correlation with distance visual acuity (r=−0.44; P<0.05) and near visual acuity (r=−0.52; P<0.01) in 24 children with 0.30 logMAR or worse in their better-seeing eye, whereas Tadic and colleagues6 reported no relationship between visual acuity deficit and vision-related quality of life (no correlation data provided). In the present study, which included a wide range of childhood eye conditions and wide range of visual acuity deficits, there were relationships between both better-seeing eye and worse-seeing eye visual acuity and functional vision and between both better-seeing-eye and worse-seeing-eye visual acuity and specific ER-QOL domains, as assessed by child self-report, proxy report and parent self-report.
Although we found an overall relationship between visual acuity and PedEyeQ scores, correlations were relatively weak, and children who had an eye condition associated with normal visual acuity in each eye often had reduced functional vision and ER-QOL. This is to be expected in a pediatric population with clinical conditions that might lower quality of life and/or functional vision, whether or not visual acuity was subnormal in either or both eyes. For example, strabismus, glasses wear, nystagmus, ptosis, or microphthalmia each might be expected to impact the social domain, and reduced stereoacuity and reduced contrast sensitivity might be expected to impact the functional vision domain. We previously reported that glasses wear for refractive error16 and the presence of strabismus15 affect PedEyeQ scores across domains. In a multiple regression analysis of factors associated with reduced quality of life, Chadha and Subramanian2 found that distance and near visual acuity accounted for only a small proportion of the variability (approximately 27%) in their model, suggesting that the majority of the effect was accounted for by other factors. We did not perform multivariate analyses because our current broad grouping of primary diagnoses is likely not sufficiently granular to account for the influence of specific diagnosis and because our sample size, even though large, was inadeqate for analyzing all factors of interest.
We evaluated associations with PedEyeQ scores based on better-seeing-eye visual acuity and also based on worse-seeing-eye visual acuity, and found correlations were stronger for worse-seeing-eye visual acuity. This stronger association with worse-seeing-eye visual acuity may seem paradoxical because one might expect that better-seeing-eye visual acuity should more profoundly influence visual function and many aspects of quality of life. Nevertheless, it is important to note that better-seeing-eye visual acuity and worse-seeing-eye visual acuity were correlated in our population. Such correlations preclude using multi-variable analysis to try to separate the effect of worse-seeing-eye and better-seeing-eye visual acuity. Also, the weaker association with better-seeing-eye acuity in this present study may be because the majority of our participants with any visual acuity deficit had a unilateral visual acuity deficit. When a population is comprised of many individuals that have predominantly unilateral rather than bilateral visual acuity deficit, there are predictable mathematical effects on the relative strengths of relationships between domain scores and better-seeing-eye versus worse-seeing-eye visual acuity. For each individual, the visual acuity score for the better-seeing eye can only move towards the normal end of the visual acuity range (compared with the worse-seeing-eye visual acuity score), along with its associated PedEyeQ domain score, increasing the scatter of PedEyeQ domain scores at that normal end of the range and thereby weakening the correlation. Most previous studies evaluating visual acuity and quality of life in children, have analyzed only better-seeing-eye visual acuity, although previous studies in adults have recognized the importance of the worse-seeing-eye visual acuity when evaluating quality of life.10 Data from the present study highlight the importance of recognizing the effect of worse-seeing-eye visual acuity on functional vision and quality of life in children and their parents.
The potential for a child’s health condition to impact the quality of life of the parent and family is often overlooked. In previous studies we have reported the effect of the child’s refractive error,16 strabismus,15 and moderate/severe visual impairment,1 on the quality of life of the parent themselves, assessed using the Parent PedEyeQ. In addition, reduced parental quality of life has been reported in parents of children with intermittent exotropia,19 and parental stress has been reported in parents of children with cataract.20 Outside of pediatric eye-care, children’s cancer treatment has been shown to reduce the parent’s own quality of life.21 In the present study, we now report that parental quality of life can be impacted by their child’s reduced visual acuity. We have previously speculated that educational interventions may be helpful in ameliorating some adverse effects on parental quality of life.15, 16 Psychosocial interventions have been shown to be helpful for improving quality of life in parents of children with cancer22 and peer support groups have been advocated as a model of psychosocial support for parents of children with type 1 diabetes.23 These interventional approaches aimed at reducing the impact of a child’s health condition on the parent, deserve to be evaluated for parents of children with eye conditions.
There are some limitations to this present study. We aimed to evaluate the relationship between visual acuity and PedEyeQ scores but it is evident that other, coexistent clinical and demographic factors not assessed in the present study also influence the relationship. It would be of interest in future studies to simultaneously analyze the relative impact of multiple factors in a large, diverse patient population. In addition, unlike some previous studies of bilateral visual impairment, the majority of children included in the present study had unilateral visual acuity deficit in the context of conditions such as amblyopia, strabismus, and/or refractive error. While this may be considered a limitation regarding measuring the impact of severe better-seeing-eye visual acuity deficits, we were interested in evaluating associations of visual acuity with functional vision and ER-QOL even in children with relatively mild visual acuity deficits and in those with unilateral deficits, and in fact we found such associations across domains.
Across a wide spectrum of childhood eye conditions, we found an overall association of visual acuity with functional vision and eye-related quality of life in the children themselves and an effect on the quality of life of their parents. Nevertheless, visual acuity may be one of many factors that likely influence relationships, and further study of many other factors in larger populations would be informative. Data from the present study further validate the use of the PedEyeQ across pediatric eye conditions.
ACKNOWLEDGEMENTS
Role of the Funder/Sponsor: The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
a. Funding/Support: Financial assistance for this study came from National Institutes of Health Grants EY024333 (JMH, PI & EEB, Co-I), EY011751 (JMH) and EY022313 (EEB), and Mayo Foundation, Rochester, Minnesota.
b. Financial Disclosures: None of the authors have any financial disclosures
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Leske DA, Hatt SR, Castaneda YS, et al. Validation of the Pediatric Eye Questionnaire (PedEyeQ) in children with visual impairment. Am J Ophthalmol 2019;208(December 2019):124–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chadha RK, Subramanian A. The effect of visual impairment on quality of life of children aged 3–16 years. Br J Ophthalmol 2011;95(5):642–645. [DOI] [PubMed] [Google Scholar]
- 3.Cochrane GM, Marella M, Keeffe JE, Lamoureux EL. The impact of vision impairment for children (IVI_C): validation of a vision-specific pediatric quality-of-life questionnaire using Rasch analysis. Invest Ophthalmol Vis Sci 2011;52(3):1632–1640. [DOI] [PubMed] [Google Scholar]
- 4.Nirmalan PK, John RK, Gothwal VK, Baskaran S, Vijayalakshmi P, Rahmathullah L. The impact of visual impairment on functional vision of children in rural South India: the Kariapatti Pediatric Eye Evaluation Project. Invest Ophthalmol Vis Sci 2004;45(10):3442–3445. [DOI] [PubMed] [Google Scholar]
- 5.Bathelt J, de Haan M, Dale NJ. Adaptive behaviour and quality of life in school-age children with congenital visual disorders and different levels of visual impairment. Res Dev Disabil 2019;85:154–162. [DOI] [PubMed] [Google Scholar]
- 6.Tadic V, Robertson AO, Cortina-Borja M, Rahi JS. An age- and stage-appropriate patient-reported outcome measure of vision-related quality of life of children and young people with visual impairment. Ophthalmology 2020;127(2):249–260. [DOI] [PubMed] [Google Scholar]
- 7.Birch EE, Cheng CS, Felius J. Validity and reliability of the Children’s Visual Function Questionnaire (CVFQ). J AAPOS 2007;11(5):473–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nickels S, Schuster AK, Elflein H, et al. Vision-related quality of life considering both eyes: results from the German population-based Gutenberg Health Study (GHS). Health Qual Life Outcomes 2019;17(1):98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Varma R, Wu J, Chong K, Azen SP, Hays RD. Impact of severity and bilaterality of visual impairment on health-related quality of life. Ophthalmology 2006;113(10):1846–1853. [DOI] [PubMed] [Google Scholar]
- 10.Hirneiss C The impact of a better-seeing eye and a worse-seeing eye on vision-related quality of life. Clin Ophthalmol 2014;8:1703–1709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Finger RP, Fenwick E, Hirneiss CW, et al. Visual impairment as a function of visual acuity in both eyes and its impact on patient reported preferences. PLoS One 2013;8(12):e81042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vu HT, Keeffe JE, McCarty CA, Taylor HR. Impact of unilateral and bilateral vision loss on quality of life. Br J Ophthalmol 2005;89(3):360–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kidd Man RE, Liang Gan AT, Fenwick EK, et al. Using uniocular visual acuity substantially underestimates the impact of visual impairment on quality of life compared with binocular visual acuity. Ophthalmology 2020;127(9):1145–1151. [DOI] [PubMed] [Google Scholar]
- 14.Hatt SR, Leske DA, Castaneda YS, et al. Development of pediatric eye questionnaires for children with eye disease. Am J Ophthalmol 2019;200(April 2019):201–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hatt SR, Leske DA, Castaneda YS, et al. Association of strabismus with functional vision and eye-related quality of life in children. JAMA Ophthalmol 2020;138(5):528–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leske DA, Hatt SR, Castaneda YS, et al. Eye-related quality of life and functional vision in children wearing glasses. J AAPOS 2020;24(2):91.e1–91.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Drover JR, Felius J, Cheng CS, Morale SE, Wyatt L, Birch EE. Normative pediatric visual acuity using single surrounded HOTV optotypes on the Electronic Visual Acuity Tester following the Amblyopia Treatment Study protocol. J AAPOS 2008;12(2):145–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pan Y, Tarczy-Hornoch K, Cotter SA, et al. Visual acuity norms in pre-school children: the Multi-Ethnic Pediatric Eye Disease Study. Optom Vis Sci 2009;86(6):607–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yamada T, Hatt SR, Leske DA, Holmes JM. Health-related quality of life in parents of children with intermittent exotropia. J AAPOS 2011;15(2):135–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Drews C, Celano M, Plager DA, Lambert SR. Parenting stress among caregivers of children with congenital cataracts. J AAPOS 2003;7(4):244–250. [DOI] [PubMed] [Google Scholar]
- 21.Klassen AF, Klaassen R, Dix D, et al. Impact of caring for a child with cancer on parents’ health-related quality of life. J Clin Oncol 2008;26(36):5884–5889. [DOI] [PubMed] [Google Scholar]
- 22.Safarabadi-Farahani A, Maarefvand M, Biglarian A, Khubchandani J. Effectiveness of a brief psychosocial intervention on quality of life of primary caregivers of Iranian children with cancer: A randomized controlled trial. J Pediatr Nurs 2016;31(4):e262–e270. [DOI] [PubMed] [Google Scholar]
- 23.Tully C, Shneider C, Monaghan M, Hilliard ME, Streisand R. Peer coaching interventions for parents of children with Type 1 diabetes. Curr Diab Rep 2017;17(6):39. [DOI] [PMC free article] [PubMed] [Google Scholar]


