Abstract
Background:
Patients with firearm injuries are at high risk of subsequent arrest and injury following hospital discharge. We sought to evaluate the effect of a 6-month joint hospital- and community-based low-intensity intervention on risk of arrest and injury among patients with firearm injuries.
Methods:
We conducted a cluster randomized controlled trial, enrolling patients with firearm injuries who received treatment at Harborview Medical Center, the Level 1 trauma center in Seattle, Washington, were 18 years or older at the time of injury, spoke English, were able to provide consent and a method of contact, and lived in one of the five study counties. The intervention consisted of hospital-based motivational interviewing, followed by a 6-month community-based intervention, and multiagency support. The primary outcome was the risk of subsequent arrest. The main secondary outcome was the risk of death or subsequent injury requiring treatment in the emergency department or hospitalization.
Results:
Neither assignment to, or engagement with, the intervention, defined as having at least 1 contact point with the Support Specialist, was associated with risk of arrest at 2 years post hospital discharge (Relative Risk for intervention assignment = 1.15; 95% CI: 0.90, 1.48; Relative Risk for intervention engagement = 1.07; 95% CI: 0.74, 2.19). There was similarly no association observed for subsequent injury.
Conclusions:
This study represents one of the first randomized controlled trials of a joint hospital- and community-based intervention delivered exclusively among patients with firearm injuries. The intervention was not associated with changes in risk of arrest or injury, a finding most likely due to the low intensity of the program.
Level of evidence:
Care Management, level II.
Registration:
Registered at clinicaltrials.gov NCT02630225
Keywords: randomized controlled trial; firearm injury; violence prevention; wounds, gunshot
BACKGROUND
At least 67,000 patients are treated for non-fatal firearm injuries each year in the United States, at an estimated $4 billion dollars of combined lifetime medical and work loss costs.1 A prior study indicated that these individuals are at substantially higher risk than the general population of subsequent rehospitalization for sustaining another firearm injury, arrest for firearm-related or violent crime perpetration, or firearm-related death after discharge from the hospital.2 Thus, interventions among this group of individuals to promote their health and well-being and reduce the high risk of subsequent perpetration, victimization, morbidity, and mortality are much needed. Such interventions may also lead to lower rates of firearm violence and its consequences in the community.
A number of hospitals across the country have created violence intervention programs to specifically help patients who sustain violent injuries, following recommendations of the Department of Justice and various medical societies.3,4 These hospital- and community-based violence intervention programs (HVIPs) seek to engage patients after their injury, viewing the immediate injury as a “teachable moment” for patients to change their lives and reduce retaliation and subsequent perpetration and victimization.5-7 HVIPs typically have community members with histories of assault and trauma, and trained in crisis intervention and de-escalation, meet patients in the hospital to provide motivational interviewing and prevent retaliatory violence.8-10 Community based staff often respond to the site where the violence occurred to intervene and prevent ongoing violence from that incident and may work with anyone connected to the violent event.9 Case managers may be selected for patients to confirm language and cultural matches11 and case management is often quite intensive, with staff seeing their clients in person several times a week, resulting in smaller caseloads per case manager.12 Additionally, there may be staff whose work is to identify and mediate ongoing conflicts such as recent arrests and release from prison to prevent violence and engagement with community leaders to change social norms around violence acceptability.9,13,14
Several observational or quasi-experimental studies have been conducted to examine the effectiveness of these programs.10,15-23 Some non-randomized studies have indicated that HVIPs are associated with reduced risk10,17 and costs23,24 for both subsequent perpetration and victimization; however, a 2016 review of these hospital-based violence intervention programs was not able to make definitive recommendations for the use of these programs based on existing evidence.25 Additionally, there have been no randomized trials evaluating the effectiveness of hospital-based or community-based violence intervention programs specifically for patients with firearm injuries.
We conducted the Helping Individuals with Firearm Injuries (HiFi) study to reduce the gap between the increasing number of violence intervention programs and the scientific evidence for evaluating their effectiveness. As it may not always be possible for hospitals and trauma centers to provide and support a HVIP program with high intensity, we sought to evaluate whether a less intensive program that broadly aligned with HVIP principles could reduce the risk of subsequent perpetration and victimization among individuals with a firearm injury. In addition to patients with an assault-related firearm injury, HiFi included patients with unintentional firearm injuries because prior research has shown that several of those individuals too are at substantial risk of subsequent violence26 and may have similar needs for services to support their health and well-being post-injury. To our knowledge, this is one of the first randomized trials of a multicomponent dual hospital and community-based intervention exclusively focused on individuals with firearm injuries.
METHODS
Study Design
HiFi was a cluster randomized controlled trial conducted at Harborview Medical Center (HMC), the regional Level 1 Trauma Center in Seattle, WA. HMC is the only Level 1 trauma center in Washington State. Eligible patients had sustained an assault or unintentional firearm injury and presented for care at HMC, were 18 years or older at the time of injury, able to speak and understand English, able to provide consent within 4 weeks of hospital discharge, able to provide at least one method of direct contact or an alternate contact, were discharged back into the community (since the intervention used in this study was designed to be used upon re-entry back to the community), and were planning to reside in one of the study counties for at least 6 months following hospital discharge (so the study Support Specialist could interact with them (Figure 1 [CONSORT diagram]). When the study began, we had two study counties (King and Pierce) but expanded later to include three additional counties (Snohomish, Thurston and Yakima) to allow increased eligibility and expanded recruitment. All patients with intentional self-inflicted firearm injuries were discharged to in-patient care for continued monitoring following hospital discharge, and as such were ineligible. HiFi was registered at clinicaltrials.gov as the “Helping Individuals with Firearm Injuries (HiFi)” with the following identifier: NCT02630225.
Figure 1.
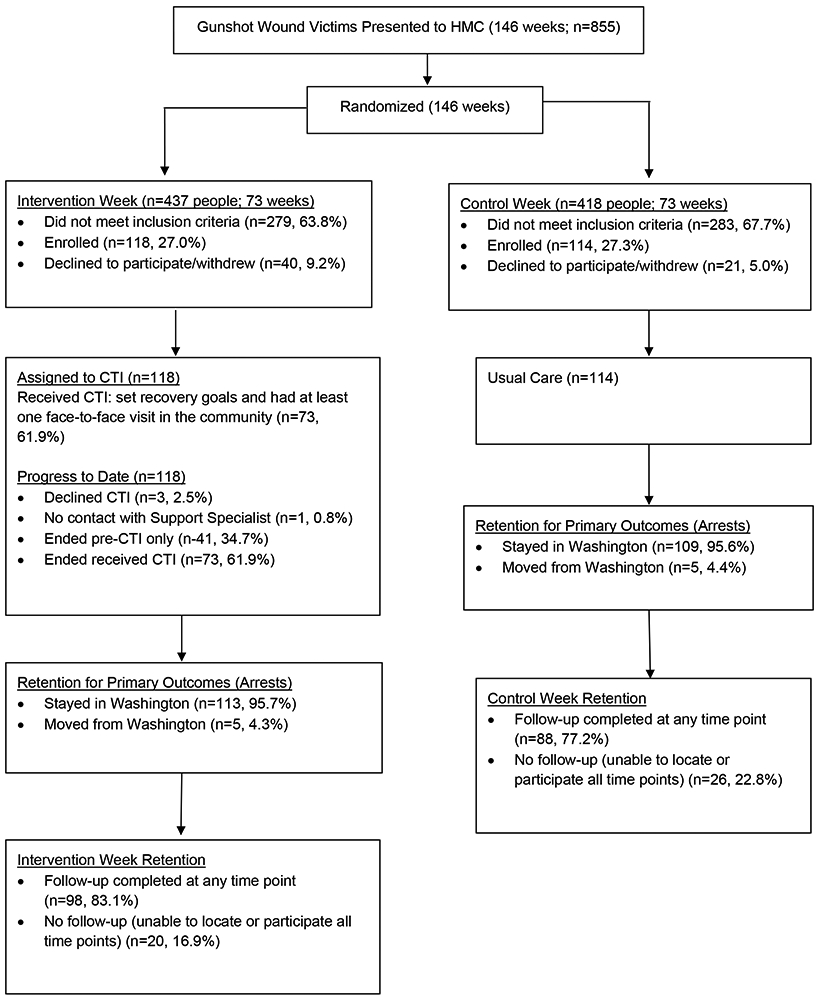
CONSORT Diagram, HiFi Study
Patient enrollment by the research assistants (RAs) preferentially took place at the bedside during the acute hospitalization, at a follow up appointment, or in the community. The RA team was diverse in their background and lived experiences and its members were trained by the Support Specialist in cultural competency prior to approaching patients. The trial enrollment took place between March 20, 2016 and December 31, 2018 with all follow-up ending on June 30, 2019.
Randomization
The trial utilized a cluster randomized design with the unit of randomization being calendar week; that is, the study staff assigned patients to one of the two groups based on the week in which they were injured and treated at HMC. All patients admitted in the same week were assigned to the same group to facilitate Support Specialist’s schedule and ensure that patients who sustained injuries in shootings involving more than one person were assigned to the same group, reducing concerns about contamination.27 We used block randomization with varying block sizes of 2 and 4 to assign each week to one of the two groups during the trial. While the study group assignment was at the cluster level, the intervention and evaluation of outcomes occurred at the individual level. As commonly done in cluster randomized controlled trials, the consent was obtained after randomization; that is when approached for enrollment, patients knew which group of the trial they would be joining if they consented to participate. As such, the goal was to enroll as many eligible participants as possible in each group to reduce the likelihood of selection bias.
Control Group
Patients in the control group were provided with usual care, including referrals to services that typically occur in the hospital setting by hospital Social Workers. All patients in the Emergency Department (ED) were treated by emergency physicians, trauma surgeons, and specialists as needed. In addition, all patients who were injured due to assault were seen by a member of the Social Work staff during their hospital stay. Patients who were admitted and screened positive for substance use (e.g., alcohol or drugs) could be seen by the Harborview Addiction Intervention Service. Among patients with an assault or unintentional firearm injury, all who additionally endorsed suicidal ideation or intent received a comprehensive psychiatric evaluation once medically stable. As part of the study, RAs provided control patients with a pamphlet outlining services that patients had found helpful after firearm injury, such as services for housing, employment, food, education and substance use services (Appendix A).
Intervention Group
The intervention program consisted of three main components: 1) motivational interviewing,28 2) care management using an adaptation of the Critical Time Intervention (CTI),29 and 3) a multidisciplinary team review, which provided oversight and support to our study Support Specialist.
Motivational interviewing was done by the study Support Specialist, in person or over the phone and was aimed at increasing patient motivation to link to services provided by the Support Specialist during the community-based portion of the intervention. When possible, the Support Specialist met with patients prior to hospital discharge. When this was not possible, study RAs facilitated a phone call between the patient and Support Specialist during or soon after enrollment.
We used an adaptation of CTI for our community-based component as it has a robust evidence-base; CTI has been rated as a ‘Top Tier’ evidence-based program.30 CTI supports vulnerable individuals during a “critical period” of transition in their lives and uses a time-limited, 3 phased approach (transition, try-out, and transfer of care). While CTI was originally designed to apply to multiple types of vulnerable patients, this was one of the first trials which applied the CTI model exclusively to patients with firearm injury. Our adaptation of CTI for HiFi, with additional intervention program, has been described in detail elsewhere.31 Hereafter, we will refer to the HiFi adaptation of the CTI program as HiFi-CTI.
Following enrollment, patients in the intervention group were visited in person or called by the Support Specialist, a master’s level social worker with specific additional training in CTI. The Support Specialist was a person of color, had training in social competency for low income and minority patients, and had worked as a counselor or in case management for 6 years previously. Following hospital discharge, patients in the intervention group received 6 months of regular contacts by the Support Specialist either over the phone, by text message, or in person, depending on patient preference and location. During weekly team meetings, cases were reviewed, and clinical consultation was provided when needed by study co-investigators.
The third component of the intervention program, the multidisciplinary team, was comprised of representatives from local community organizations including a large community mental health agency, law enforcement agencies, as well as public service agencies (Appendix B). They contributed as consultants for our study and helped the Support Specialist identify relevant recovery resources needed by the intervention patients.
Outcomes
The primary outcome was arrest for any crime. Arrest was measured using the administrative databases maintained by the Washington State Administrative Office of the Courts (AOC) and the Washington State Patrol (WSP), a statewide law enforcement agency. Both were used to ensure complete capture of all arrests which occurred in Washington State. A patient was counted as being arrested if there was a record of arrest in either the AOC or WSP.
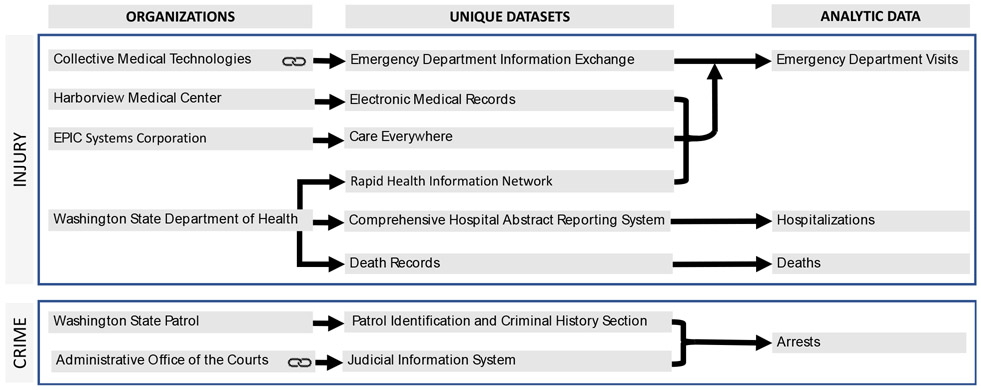
The main secondary outcome was subsequent injury requiring medical treatment in an ED, hospitalization, or an injury resulting in death. This was measured by using the Emergency Department Information Exchange (a health information exchange of emergency department visits throughout Washington and 20 other states collected by Collective Medical Technologies), HMC Electronic Medical Records (EMR), CareEverywhere (a feature of EPIC, the EMR system used at HMC, that links to visit records at participating hospitals across the state also using EPIC), the Rapid Health Information Network (a state-wide dataset of ED visits developed by the Department of Health during the HiFi study period for syndromic surveillance), the Washington State Comprehensive Hospital Abstract Reporting System (an annual abstraction of all hospital discharges in the state), and Washington vital statistics records (Appendix C). There was one death in our study during the follow up period, which was the result of a firearm injury that occurred during the commission of a crime. For this patient, their death was counted as an arrestable offense for the arrest analysis and an injury for the injury analysis.
Other secondary outcomes included patient reported measures of health and well-being collected by surveys conducted at baseline and follow-up including post-traumatic stress disorder (PTSD) symptoms,32 depression symptoms,33 perceived social support,34 happiness,35 physical and mental health,36 as well as alcohol use37 and lifetime drug use (Appendix D).38 To capture sociodemographic and secondary outcome data, patients completed a baseline assessment at time of enrollment and follow up surveys at 1, 3, 6, 9 and 12 months following hospital discharge. Surveys were completed in person, over the phone or online using Research Electronic Data Capture (REDCap).39 Multiple modalities to obtain outcome assessments were used as previous studies had noted no difference in response between internet-assessments and interviewer-administered assessments.40 Patients were given a gift card with the completion of each survey ranging from $25-$50; amount depended on survey length and time since enrollment. We additionally abstracted patient age, sex, race, ethnicity and injury intent from the patient’s electronic medical record of the initial hospital encounter for the firearm injury. Injury severity scores (ISS) were obtained from the Harborview Trauma Registry following comprehensive review of patient charts by trained abstractors. Study staff responsible for collecting outcome and censoring data (arrests and hospitalizations), conducting linkages and identifying outcome events were blinded to the patient’s intervention group (Figure 2).
Figure 2.
Illustration of Linking Processes for HiFi Data Sources. Note:  Indicates that linking occurred at the agency level. All other linking was conducted by our study team.
Indicates that linking occurred at the agency level. All other linking was conducted by our study team.
Analytic Power
Arrest, as the primary outcome of interest, was used to calculate analytic power. A prior study of patients with firearm injury in Washington State and King County indicated that the rate of subsequent arrest following hospital discharge among these individuals was 15,528 cases per 100,000 person-years2 for a two-year cumulative incidence of arrest of 26%. We assumed a significance level of 0.05, a power of 80%, an intervention-to-control ratio of 1, 78 clusters (i.e., weeks) per group during the three-year enrollment phase, a sample size of about 2 patients per cluster, correlation between history of arrest and subsequent arrest of 0.70 and an intraclass correlation coefficient of 0.01. With a 3-year enrollment plan total, 304 enrolled patients, and up to 2 years of follow-up, we expected to be able to identify a minimally detectable relative risk reduction of 29% for the primary outcome of arrest. We were able to enroll a total of 232 patients by the end of study recruitment.
Statistical Analyses
We first performed an intent-to-treat (ITT) analysis. We obtained group-specific unadjusted estimates of the cumulative incidence of arrest during 1 year of follow-up by calculating the Kaplan-Meier estimator separately among participants randomized to the intervention versus control group and used the estimates of cumulative incidence to calculate the unadjusted relative risk of arrest. Wald-type confidence intervals were calculated based on a complementary log-log transformation. In order to relax the independent censoring assumption required by the Kaplan-Meier method and increase statistical efficiency, we also estimated the adjusted cumulative incidence of arrest during 1 year of follow-up using a G-computation approach.41 The relative risk was calculated by dividing the adjusted estimate of the cumulative incidence during 1 year of follow-up for the intervention group to the corresponding estimate for the control group. Confidence intervals were computed using the nonparametric bootstrap.
We then performed a per-protocol effect (PPE) analysis to account for varying levels of participant engagement with the Support Specialist during the study. To estimate the casual effect of a time-varying exposure in the presence of time-varying confounders affected by prior exposure, we used a parametric multi time-point G-computation approach.42 We estimated the counterfactual cumulative incidence of patients with an arrest during 1 and 2 years of follow-up that would have been seen: (1) had all patients engaged with the Support Specialist at least one time per study phase for a total of three study meetings, and (2) had all patients been instead assigned to the control arm.
We adjusted this analysis for stable housing, age, injury intent, and prior arrest at baseline, and stable housing collected post-randomization at the 1 and 3-month marks. Because the intervention ended at 6 months following hospital discharge, only data from the baseline, 1 and 3-month marks could provide information on individual characteristics that would predict intervention engagement; as such, only information from those surveys were included. Confidence intervals and hypothesis tests were computed using the nonparametric bootstrap (Appendix E).
For secondary outcome of subsequent injury, the same analytic process was followed as with arrest, with the exception that we used injury prior to the index event as a covariate instead of prior arrest. Data from surveys for self-reported secondary outcomes were analyzed using linear mixed models. Interim analyses, including main outcomes, secondary outcomes and summary statistics of the intervention, were conducted and presented quarterly to our multidisciplinary team for discussion. The study and full protocol (Appendix F) were approved by the University of Washington Human Subjects Division (STUDY00000852) and Washington State Institutional Review Board (D-100616-H), and study participants provided informed consent for all study procedures. Analyses were conducted in SAS, Stata, and R.43,44
RESULTS
Of the 855 patients who presented to HMC with a firearm injury during the enrollment period, 293 were found to be eligible, and 232 enrolled in the study with 114 patients assigned to the control group and 118 to the intervention group; the enrollment proportions were essentially the same for the two groups (Figure 1). Among patients assigned to the intervention group, 77 (65.2%) received some intervention from the Support Specialist with an average of 2.4 in-person contacts (standard deviation [SD]: 2.3); these patients identified a range of goals for working with the Support Specialist (Appendix G). Patients in the intervention group were slightly older and more likely to be White, be working, have unstable housing, be enrolled following admission, have a lower income, and have a higher ISS than those in the control group (Table 1). A total of 86 control patients (75.4%) and 95 intervention patients (80.5%) completed at least one follow-up survey. Appendix H presents the survey completion proportion at each follow-up point among patients eligible for the corresponding survey.
Table 1.
Characteristics for HiFi patients, 2016-2019
| Characteristic | Total (n=232) |
Control (n=114) |
Intervention (n=118) |
Standardized Difference |
|---|---|---|---|---|
| Age in years, mean (SD) | 29.8(10.6) | 29.0(9.9) | 30.5(11.3) | −0.14 |
| Male, no. (%) | 199(85.8) | 99(86.8) | 100(84.8) | 0.06 |
| Race/Ethnicity, no. (%) | 0.10 | |||
| Non-Hispanic White | 78(33.6) | 34(29.8) | 44(37.3) | |
| Non-Hispanic Black | 101(43.5) | 52(45.6) | 49(41.5) | |
| Non-Hispanic Asian or Pacific Islander | 17(7.3) | 11(9.7) | 6(5.1) | |
| Non-Hispanic American Indian/Alaska Native | 8(3.5) | 3(2.6) | 5(4.2) | |
| Hispanic (all races) | 28(12.1) | 14(12.3) | 14(11.9) | |
| Employment, no. (%) | 0.14 | |||
| Working | 124(58.5) | 56(54.9) | 68(61.8) | |
| Laid off | 41(19.3) | 23(22.5) | 18(16.4) | |
| Student | 18(8.5) | 10(9.8) | 8(7.3) | |
| Homemaker | 4(1.9) | 4(3.9) | 0(0.0) | |
| Retired | 3(1.4) | 2(2.0) | 1(0.9) | |
| Other | 22(10.4) | 7(6.9) | 15(13.6) | |
| Current housing situation, no. (%) | 0.16 | |||
| Stable | 157(70.1) | 82(73.9) | 75(66.4) | |
| Transitional | 35(15.7) | 17(15.5) | 18(15.9) | |
| Unstable | 32(14.3) | 12(10.9) | 20(17.7) | |
| Injury intent, no. (%) | 0.01 | |||
| Assault | 169(80.1) | 83(79.8) | 86(80.4) | |
| Unintentional | 41(19.4) | 20(18.9) | 21(19.4) | |
| Shot by law enforcement | 1(0.5) | 1(0.9) | 0(0.0) | |
| Enrollment location, no. (%) | 0.17 | |||
| ED | 26(11.6) | 16(14.6) | 10(8.7) | |
| Inpatient | 126(56.0) | 57(51.8) | 69(60.0) | |
| Clinic | 70(31.1) | 34(30.9) | 36(31.3) | |
| Other | 3(1.3) | 3(2.7) | 0(0.0) | |
| Household income, no. (%) | 3(1.3) | 3(2.7) | 0(0.0) | 0.22 |
| <25K | 76(48.1) | 29(42.0) | 47(52.8) | |
| 25-50K | 43(27.2) | 21(30.4) | 22(24.7) | |
| 50-100K | 25(15.8) | 11(15.9) | 14(15.7) | |
| >100K | 14(8.9) | 8(11.6) | 6(6.7) | |
| Length of stay in hours, mean(SD) | 133.8(225.5) | 132.3(254.2) | 135.3(194.9) | −0.01 |
| Injury Severity Score, mean (SD) | 10.1(8.4) | 9.2(9.2) | 11.0(9.0) | −0.21 |
| Arrested before injury, no. (%) | 169(72.8) | 83(72.8) | 86(72.9) | 0.04 |
SD: Standard Deviation. Missing subject: Current housing situation (n=8), Employment (n=20), Injury intent (n=21), Enrollment location (n=7), Income (n=74), Injury Severity Score (n=3). Note: Stable housing includes individuals living in a private home, private apartment, or other dwelling (e.g. trailer) who indicated that the dwelling was their address. Transitional housing includes individuals living in a private home, private apartment, or other dwelling (e.g. trailer) who indicated that the dwelling was not their address. Unstable housing includes individuals who indicated that they were couch surfing, homeless, or in a shelter.
Patients were followed-up for an average of 1.78 years (SD: 0.81). In the ITT analysis, assignment to the intervention group was not associated with a change in cumulative incidence of arrest either during 1 year (relative risk [RR]=1.17; 95% CI: 0.90, 1.57; p=0.26) or 2 years of follow-up (RR=1.15; 95% CI: 0.90, 1.48; p=0.27). Similarly, in the per-protocol effect analysis, engagement with the intervention, defined as having at least 1 contact point with the Support Specialist during each of the three study phases, was not associated with a change in cumulative incidence of arrest during 1 year (RR=1.08; 95% CI: 0.91, 1.28; p=0.39) or 2 years of follow-up (RR=1.07; 95% CI: 0.74, 2.19; p=0.34; Table 2)
Table 2.
Risk of subsequent arrest following hospital discharge for initial firearm injury among the intervention group compared to the control group, HiFi Study, 2016-2019
| Intent-To-Treat |
Per-Protocol Effect |
||||||
|---|---|---|---|---|---|---|---|
| Number of Events |
Unadjusted Cumulative Incidence (95% CI) |
Unadjusted Relative Risk (95% CI) |
Adjusted Cumulative Incidencea (95% CI) |
Relative Riska (95% CI) |
Adjusted Cumulative Incidenceb (95% CI) |
Relative Riskb (95% CI) |
|
| Arrest – 1 year | |||||||
| Control | 41 | 37.2 (27.5, 45.7) | 1.00 (ref) | 35.6 (27.5, 44.1) | 1.00 (ref) | 40.9 (23.9, 57.5) | 1.00 (ref) |
| Intervention | 48 | 42.7 (33.3, 50.6) | 1.15 (0.74, 1.79) | 41.7 (33.3, 50.6) | 1.17 (0.90, 1.57) | 44.2 (25.7, 62.4) | 1.08 (0.91, 1.28) |
| Arrest – 2 years | |||||||
| Control | 49 | 46.7 (35.9, 55.7) | 1.00 (ref) | 44.9 (35.5, 54.1) | 1.00 (ref) | 53.3 (36.1, 67.5) | 1.00 (ref) |
| Intervention | 56 | 53.0 (41.8, 62.1) | 1.13 (0.76, 1.70) | 51.5 (41.9, 61.4) | 1.15 (0.90, 1.48) | 56.9 (38.6, 70.8) | 1.07 (0.74, 2.19) |
Adjusted for prior arrest, stable living, age, and injury intent (coded as assault or not).
Adjusted for prior arrest, stable living, age, and injury intent (coded as assault or not) at baseline, and stable housing collected post-randomization at the 1- and 3-month mark.
As with arrest, neither assignment nor engagement with the intervention was associated with risk of incident injury during 1 year (RR for assignment=1.52; 95% CI: 0.92, 2.68; p=0.10; RR for engagement=1.21; 95% CI: 0.81, 1.63; p=0.29) or 2 years (RR for assignment=1.49; 95% CI: 0.94, 2.55; p=0.09; RR for engagement=1.16; 95% CI: 0.56, 3.34; p=0.30) of follow-up (Table 3). The two groups did not show significant differences in most of the self-reported measures; however, there was a pattern of poorer reported physical health among intervention patients than control patients during follow-up compared to their pre-injury baseline reported scores at enrollment (Table 4 and Appendix H).
Table 3.
Risk of subsequent injury following hospital discharge for initial firearm injury among the intervention group compared to the control group, HiFi Study, 2016-2019
| Intent-to-treat |
Per-Protocol Effect |
||||||
|---|---|---|---|---|---|---|---|
| Number of Events |
Unadjusted Cumulative Incidence (95% CI) |
Unadjusted Relative Risk (95% CI) |
Adjusted Cumulative Incidencea (95% CI) |
Relative Riska (95% CI) |
Adjusted Cumulative Incidenceb (95% CI) |
Relative Riskb (95% CI) |
|
| Injury – 1 year | |||||||
| Control | 14 | 13.0 (6.4, 19.1) | 1.00 (ref) | 13.3 (7.8, 19.5) | 1.00 (ref) | 14.2 (6.9, 27.9) | 1.00 (ref) |
| Intervention | 23 | 20.5 (12.6, 27.7) | 1.58 (0.80, 3.40) | 20.2 (13.3, 27.7) | 1.52 (0.92, 2.68) | 17.1 (8.2, 33.5) | 1.21 (0.81, 1.63) |
| Injury – 2 years | |||||||
| Control | 18 | 18.1 (10.0, 25.5) | 1.00 (ref) | 17.9 (10.9, 25.2) | 1.00 (ref) | 23.4 (12.0, 37.9) | 1.00 (ref) |
| Intervention | 28 | 26.8 (17.6, 35.1) | 1.48 (0.79, 2.85) | 26.6 (18.5, 35.4) | 1.49 (0.94, 2.55) | 27.3 (14.0, 43.7) | 1.16 (0.56, 3.34) |
Adjusted for prior arrest, stable living, age, and injury intent.
Adjusted prior arrest, stable living, age, and injury intent at baseline, and stable housing collected post-randomization at the 1 and 3-month marks.
Table 4.
Change in self-reported secondary outcome average scores for each follow-up survey
| Mean Difference from Baseline Comparing Intervention to Control Patients (95% CI) | |||||
|---|---|---|---|---|---|
| Scales | 1 month | 3 months | 6 months | 9 months | 12 months |
| PCL-C total | 1.4 (−4.6, 7.3) | 4.5 (−2.0, 10.9) | 2.5 (−2.5, 7.5) | −1.5 (−8.2, 5.3) | −2.2 (−7.2, 2.9) |
| PHQ-8 total | 0.5 (−1.8, 2.8) | 0.6 (−1.9, 3.1) | 0.1 (−1.9, 2.0) | 0.1 (−2.5, 2.7) | −0.2 (−2.2, 1.8) |
| Audit total | 0.2 (−0.8, 1.2) | −0.2 (−1.3, 0.9) | 0.2 (−0.6, 1.1) | 0.4 (−0.7, 1.5) | 0.2 (−0.6, 1.0) |
| IPAS IA mean | −0.03 (−0.56, 0.49) | −0.11 (−0.68, 0.46) | 0.03 (−0.41, 0.48) | −0.09 (−0.68, 0.51) | −0.10 (−0.54, 0.34) |
| IPAS PM mean | 0.08 (−0.38, 0.54) | −0.03 (−0.53, 0.47) | 0.17 (−0.21, 0.56) | 0.34 (−0.18, 0.86) | 0.05 (−0.34, 0.44) |
| MPSS scale total | −0.45 (−0.94, 0.05) | −0.17 (−0.71, 0.36) | −0.09 (−0.51, 0.33) | −0.14 (−0.70, 0.42) | −0.09 (−0.51, 0.33) |
| SAL total | 0.3 (−9.8, 10.4) | −1.6 (−12.7, 9.4) | −6.0 (−14.6, 2.6) | −4.8 (−16.3, 6.7) | −5.3 (−13.9, 3.3) |
| SF-12 physical | −2.8 (−7.2, 1.6) | −7.1 (−11.9, −2.3) | −4.0 (−7.8, −0.3) | −6.7 (−11.6, −1.7) | −3.1 (−6.8, 0.6) |
| SF-12 mental | −2.2 (−7.3, 3.0) | −0.6 (−6.2, 5.0) | −3.1 (−7.5, 1.3) | 2.4 (−3.4, 8.2) | −1.1 (−5.4, 3.3) |
| SF-12 global | −5.1 (−10.3, 0.2) | −7.1 (−12.8, −1.4) | −6.9 (−11.3, −2.4) | −7.5 (−13.5, −1.6) | −8.1 (−12.6, −3.7) |
| ASSIST total score | 2.9 (−5.8, 11.6) | 2.0 (−7.4, 11.4) | 2.7 (−4.6, 10.0) | 0.4 (−9.4, 10.1) | 4.4 (−2.9, 11.6) |
PCL-C: PTSD Checklist Civilian Version (post-traumatic stress symptoms); PHQ-8: Patient Health Questionnaire (depression); AUDIT: The Alcohol Use Identification Test (alcohol use); IPAS: Impulsive-Premeditated Aggression Scale (aggression); IA: Impulsive Aggression; PM: Premeditated Aggression; MPSS: Multidimensional Scale of Perceived Social Support (social support); SAL: Satisfaction with Areas of Life (happiness). SF: Short Form Health Survey (health-related quality of life); ASSIST: Alcohol, Smoking and Substance Involvement Screening Test (drug use). Note: Linear mixed models were adjusted for age, employment, injury severity score, stable living, inpatient enrollment, completion mode and prior arrest as well as clustering by week.
DISCUSSION
In this study, neither intervention assignment nor engagement with the intervention was associated with reduction in the risk of the primary outcome of arrest or the main secondary outcome of injury during follow-up.
This finding is likely partially due to the low level of intervention intensity in the HiFi program. Although a fidelity assessment of HiFi conducted while the study was ongoing found the HiFi-CTI program was well implemented according to CTI principles,31 it was offered with less in-person contacts than other CTI implementations and over a shorter time period. HiFi-CTI was also generally in line with the four core HVIP principles including: [1] a brief intervention in the ED or at bedside; [2] long-term community-based case management services; [3] follow-up services provided by a culturally competent Support Specialist that included linkages to community-based services, home visits, and [4] offering services that address social determinants of health.13 However, HiFi-CTI was less intensive by design. For example, while we did engage with community organizations through the multidisciplinary team and by providing referrals and care coordination support to patients, the engagement with the organizations themselves was less frequent and less patient specific than recommended for HVIPs.6 Additionally, many HVIPs treat the hospital-based component of the intervention as a violence interruption opportunity rather than motivation for engagement in the program9 and also work closely with all persons impacted by firearm injury, not just the victim of violence. HiFi-CTI was selected to evaluate if a modified version of HVIP programs with the same core principles, but less intensive implementation, could be effective in low-resourced settings. Likely HVIP style interventions need to be offered with higher intensity to be effective at reducing subsequent perpetration and victimization. It is also possible that the ‘teachable moment’ that HVIPs utilize may exist for some, but not all, patients with injury,7 potentially highlighting the importance of initial screening for patient openness to behavioral interventions prior to program enrollment.
This study had some limitations. We were not able to meet our enrollment goal; it is not clear, however, if enrolling additional 72 people would have notably changed our estimates. Additionally, we were able to enroll the majority of eligible people during our enrollment period. Future larger studies could also examine the potential differential effects of such interventions by injury intent to avoid “diluting” their true impact via studying patients with injuries of differing intent together. Second, while we were not able to include non-English speaking patients in our study due to language restrictions of our Support Specialist, only 4% of the 855 patients who presented to HMC for treatment of a firearm injury during our enrollment period were ineligible due to language. Third, while injury outcomes are often included in evaluations of hospital-based violence intervention programs, we were not able to include this as a primary outcome in our study due to low frequency of recurrent injuries in our study.2 Fourth, our study allowed for enrollment up to 4 weeks following firearm injury, at which point the time window for a “teachable moment” may have ended for some patients. However, patients were enrolled within a median of 3 days following their firearm injury (interquartile range: 1-12 days), minimizing this concern. Additionally, it is possible that our secondary outcome of interest was not well captured due to the incompleteness of chief complaint information in our Emergency Department data even after our linking efforts to address this missingness.
Finally, our primary outcome of interest (i.e., arrest) is a biased measure of our true outcome of interest (i.e., crime perpetration) given the documented racial disparities in arrest rates. Numerous studies have demonstrated that people of color, especially Black individuals, live in communities with heavier policing45,46 and are much more likely to be arrested than White individuals for the same crime,46-49 reflecting both interpersonal and structural racism. Importantly, the health consequences of arrest, potential subsequent jail or prison time as well as convictions can be severe, affecting both mental and physical health for even lower levels of criminal justice system contact.50
This study utilized both intent-to-treat and per-protocol effect analyses to better characterize the effect of the intervention. While our results produced by these two analyses were not substantively different, we do believe the use of the per-protocol effect analyses in addition to intent-to-treat analyses is an important innovation in the assessment of behavioral interventions. Another strength of this study was its use of several administrative datasets to measure outcomes as it reduced bias due to reliance on self-reported measures and allowed for continuous follow up among study participants for main outcomes even when participants stopped responding to study staff or completing follow-up surveys. Finally, our lack of intervention effect does provide valuable insight into the level of intensity which may be required for intervention efficacy and cautions against implementing low-intensity interventions as a means to reduce risk of arrest and injury following a firearm injury.
In conclusion, neither intervention assignment nor engagement was associated with a change in risk of outcomes in this trial. It is likely that the HiFi-CTI adaptation case management program was not intensive enough to interrupt violence or recurrent injuries in patients with firearm injuries. Our study provides evidence that less intensive versions of HVIP programs like ours are likely insufficient to reduce risk of arrest or injury among patients with a firearm injury. Hospitals considering implementing programs to support patients with violent injuries will likely not see changes in patient outcomes if they implement a low intensity intervention and instead should consider investing in a high-intensity HVIP style program potentially offered to those at highest risk of violence perpetration and victimization.
Supplementary Material
Acknowledgments
The authors would like to thank Alvaro Martinez, Manal Jmaileh, Emma Bent, Cara Currier, Erin Ballsmith, Alice Yan, Tamara Almira, Lina Benson, Navya Gunaje and Serena Skidmore for their valuable contributions to this study as well as Dr. Joel Fein for review of an earlier version of this manuscript.
Funding
Funding for this study was provided by the City of Seattle (contracts DA16-1570, DA17-1570, DA18-1570, and DA19-1570) in 2016-2019, Arnold Ventures in 2017-2018, and the Department of Justice (2015-GP-BX-0006/PSN-2015-003 in 2016-2017). This study was also supported by the National Center for Advancing Translational Sciences (UL1 TR002319) and the National Institute of Child Health and Human Development (P2C HD042828) of the National Institutes of Health. VHL was additionally supported by the National Center for Advancing Translational Sciences (TL1 TR002318) and the FACTS (Firearm Safety Among Children & Teens) Consortium funded by the National Institute for Child Health and Human Development (1R24HD087149). The views expressed in this report are the authors’ and do not necessarily reflect the views of the funders.
Footnotes
Conflicts of Interest
None
Conference Presentations: Some preliminary findings of this project were presented at the 51st Annual Meeting of the Society for Epidemiologic Research, June 18-21, 2019 in Minneapolis, MN and the 1st Annual Meeting for the Firearm Safety Among Children & Teens Consortium, October 21, 2019 in Ann Arbor, MI.
REFERENCES
- 1.Fowler KA, Dahlberg LL, Haileyesus T, Annest JL. Firearm injuries in the United States. Prev Med (Baltim). 2015;79:5–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rowhani-Rahbar A, Zatzick D, Wang J, Mills BM, Simonetti JA, Fan MD, Rivara FP. Firearm-related hospitalization and risk for subsequent violent injury, death, or crime perpetration: a cohort study. Ann Intern Med. 2015;162(7):492–500. [DOI] [PubMed] [Google Scholar]
- 3.Office for Victims of Crimes. New Directions from the Field: Victims’ Rights and Services for the 21st Century. Washington (DC); 1998. [Google Scholar]
- 4.Dicker R, Gaines B, Bonne S, Duncan T, Violano P, Aboutanos M, Allee L, Burke PA, Masiakos PT, Hink A, et al. Violence Intervention Programs: A Primer for Developing a Comprehensive Program for Trauma Centers.; 2017. [Google Scholar]
- 5.Boudreaux ED, Bock B, O’Hea E. When an Event Sparks Behavior Change: An Introduction to the Sentinel Event Method of Dynamic Model Building and Its Application to Emergency Medicine. Acad Emerg Med. 2012;19(3):329–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Network of Hospital Based Violence Intervention Programs. Hospital-based Violence Intervention: Practices and Policies to End the Cycle of Violence. NNHVIP Policy White Pap. 2019. [Google Scholar]
- 7.Melzer-lange MD, Zonfrillo MR, Gittelman MA. Injury Prevention Opportunities in the Emergency Department. Pediatr Clin NA. 2020;60(5):1241–1253. [DOI] [PubMed] [Google Scholar]
- 8.Cheng TL, Haynie D, Brenner R, Wright JL, Chung S, Simons-Morton B. Effectiveness of a mentor-implemented, violence prevention intervention for assault-injured youths presenting to the emergency department: results of a randomized trial. Pediatrics. 2008;122(5):938–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Skogan W, Harnett S, Bump N, Dubois J. Evaluation of CeaseFire-Chicago. Chicago; 2008. [Google Scholar]
- 10.Becker MG, Hall JS, Ursic CM, Jain S, Calhoun D. Caught in the Crossfire: the effects of a peer-based intervention program for violently injured youth. J Adolesc Health. 2004;34(3):177–183. [DOI] [PubMed] [Google Scholar]
- 11.Smith R, Evans A, Adams C, Cocanour C, Dicker R. Passing the torch: evaluating exportability of a violence intervention program. Am J Surg. 2013;206(2):223–228. [DOI] [PubMed] [Google Scholar]
- 12.Smith R, Dobbins S, Evans A, Balhotra K, Dicker RA. Hospital-based violence intervention: risk reduction resources that are essential for success. J Trauma Acute Care Surg. 2013;74(4):972–976. [DOI] [PubMed] [Google Scholar]
- 13.The Health Alliance for Violence Intervention. What is a hospital-based violence intervention program (HVIP)? 2020. https://www.thehavi.org/what-is-an-hvip. Published 2020. Accessed March 12, 2020. [Google Scholar]
- 14.Butts JA, Roman CG, Bostwick L, Porter JR. Cure violence: a public health model to reduce gun violence. Annu Rev Public Health. 2015;36:39–53. [DOI] [PubMed] [Google Scholar]
- 15.Aboutanos MB, Jordan A, Cohen R, Foster RL, Goodman K, Halfond RW, Poindexter R, Charles R, Smith SC, Wolfe LG, et al. Brief violence interventions with community case management services are effective for high-risk trauma patients. J Trauma. 2011;71(1):227–228. [DOI] [PubMed] [Google Scholar]
- 16.Cooper C, Eslinger DM, Stolley PD. Hospital-based violence intervention programs work. J Trauma. 2006;61(3):534–540. [DOI] [PubMed] [Google Scholar]
- 17.Shibru D, Zahnd E, Becker M, Bekaert N, Calhoun D, Victorino GP. Benefits of a hospital-based peer intervention program for violently injured youth. J Am Coll Surg. 2007;205(5):684–689. [DOI] [PubMed] [Google Scholar]
- 18.Snider C, Jiang D, Logsetty S, Strome T, Klassen T. Wraparound care for youth injured by violence: Study protocol for a pilot randomised control trial. BMJ Open. 2015;5(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Walton MA, Chermack ST, Shope JT, Bingham CR, Zimmerman MA, Blow FC, Cunningham RM. Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: a randomized controlled trial. JAMA. 2010;304(5):527–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Watt K, Shepherd J, Newcombe R. Drunk and dangerous: a randomised controlled trial of alcohol brief intervention for violent offenders. J Exp Criminol. 2007;4(1):1–19. [Google Scholar]
- 21.Zatzick D, Russo J, Lord SP, Varley C, Wang J, Berliner L, Jurkovich G, Whiteside LK, O'Connor S, Rivara FP. Collaborative care intervention targeting violence risk behaviors, substance use, and posttraumatic stress and depressive symptoms in injured adolescents: a randomized clinical trial. JAMA Pediatr. 2014;168(6):532–539. [DOI] [PubMed] [Google Scholar]
- 22.Zun LS, Downey L, Rosen J. The effectiveness of an ED-based violence prevention program. Am J Emerg Med. 2006;24(1):8–13. [DOI] [PubMed] [Google Scholar]
- 23.Purtle J, Dicker R, Cooper C, Corbin T, Greene MB, Marks A, Creaser D, Topp D, Moreland D. Hospital-based violence intervention programs save lives and money. J Trauma Acute Care Surg. 2013;75(2):331–333. [DOI] [PubMed] [Google Scholar]
- 24.Purtle J, Rich LJ, Bloom SL, Rich JA, Corbin TJ. Cost-benefit analysis simulation of a hospital-based violence intervention program. Am J Prev Med. 2015;48(2):162–169. [DOI] [PubMed] [Google Scholar]
- 25.Affinati S, Patton D, Hansen L, Ranney M, Christmas AB, Violano P, Sodhi A, Robinson B, Crandall M from the Eastern Association for the Surgery of Trauma Injury Control and Violence Prevention Section and Guidelines Section. Hospital-based violence intervention programs targeting adult populations: an Eastern Association for the Surgery of Trauma evidence-based review. Trauma Surg Acute Care Open. 2016;1(1):e000024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rowhani-Rahbar A, Fan MD, Simonetti JA, Lyons VH, Wang J, Zatzick D, Rivara FP. Violence perpetration among patients hospitalized for unintentional and assault-related firearm injury: A case-control study and a cohort study. Ann Intern Med. 2016;165(12). [DOI] [PubMed] [Google Scholar]
- 27.Heagerty P, DeLong E, for the NIH Health Care Systems Research Collaboratory Biostatistics and Study Design Core. Experimental Designs and Randomization Schemes: Cluster Randomized Trials. In: Rethinking Clinical Trials: A Living Textbook of Pragmatic Clinical Trials. Bethesda, MD: NIH Health Care Systems Research Collaboratory; 2020. [Google Scholar]
- 28.Stanhope V, Tennille J, Bohrman C, Hamovitch E. Motivational Interviewing: Creating a Leadership Role for Social Work in the Era of Healthcare Reform. Soc Work Public Health. 2016;31(6):474–480. [DOI] [PubMed] [Google Scholar]
- 29.Center for the Advancement of Critical Time Intervention. CTI Model. https://www.criticaltime.org/cti-model/. Published 2016. [Google Scholar]
- 30.Coalition for Evidence-Based Policy. Evidence Summary for the Critical Time Intervention.; 2013. https://evidencebasedprograms.org/document/critical-time-intervention-evidence-summary/. [Google Scholar]
- 31.Lyons VH, Benson LR, Griffin E, Floyd AS, Kiche SW, Haggerty KP, Whiteside LK, Conover S, Herman DB, Rivara FP, et al. Fidelity Assessment of a Social Work–Led Intervention Among Patients With Firearm Injuries. Res Soc Work Pract. March 2020:1049731520912002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Weathers F, Litz B, Herman D, Huska J, Keane T. The PTSD Checklist (PCL): Reliability, validity and diagnostic utility. 1993. [Google Scholar]
- 33.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zimet G, Dahlem N, Zimet S, Farley G. The Multidimensional Scale of Perceived Social Support. J Pers Assess. 1988;52:30–41. [Google Scholar]
- 35.Meyers RJ, Roozen HG, Smith JE. The Community Reinforcement Approach. Alcohol Res Heal. 1989:380–388. [PMC free article] [PubMed] [Google Scholar]
- 36.Ware J, Kosinki M, Keller S. SF-12: How to Score the SF-12 Physical and Mental Health Summary Scales. Boston, MA; 1995. [Google Scholar]
- 37.Babor T, de la Fuente J, Saunders J, Grant M. AUDIT: The Alcohol Use Disorders Identification Test. Guidelines for use in primary health care. 1992. [Google Scholar]
- 38.Humeniukm R, Henry-Edwards S, Ali R, Poznyak V, Monteiro M. The Alcohol, Smoking and Substance Involvment Screening Test (ASSIST): manual for use in primary care. 2010. [Google Scholar]
- 39.Harris PA, Taylor R, Thielke R, Jonathon P, Gonzalez N, Conde J. Research electronic data capture (REDCap) - A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fleming CB, Marchesini G, Elgin J, Haggerty KP, Woodward D, Abbott RD, Catalano RF. Use of web and phone survey modes to gather data from adults about their young adult children: An evaluation based on a randomized design. Field methods. 2013;25(4):388–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rothman K, Greenland S, Lash T. Modern Epidemiology. 3rd Editio. Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 42.Robins J Robust estimation in sequentially ignorable missing data and causal inference models. In: American Statistical Association Section on Bayesian Statistical Science. ; 1999:6–10. [Google Scholar]
- 43.SAS Institute Inc. SAS 9.4. 2013. [Google Scholar]
- 44.R Core Team. R: A language and environment for statistical computing. 2019. https://www.r-project.org/. [Google Scholar]
- 45.Peterson R, Krivo L. Divergent Social World: Neighborhood Crime and the Racial-Spatial Divide. New York, NY; 2012. [Google Scholar]
- 46.The Sentencing Project. Report of The Sentencing Project to the United Nations Special Rapporteur on contemporary forms of racism, racial discrimination, xenophobia, and related intolerance. Res Advocacy Reform. 2018;(March):1–16. https://www.sentencingproject.org/publications/un-report-on-racial-disparities/. [Google Scholar]
- 47.Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future National Survey Results on Drug Use, 1975-2012: Volume 1, Secondary School Students. Ann Arbor: Institution for Social Research, The University of Michigan; 2013. [Google Scholar]
- 48.Beckett K, Nyrop K, Pfingst L. Race, Drugs, and Policing: Understanding Disparities in Drug Delivery Arrests. Criminology. 2006;44(1):105–137. [Google Scholar]
- 49.Edwards E, Bunting W, Garcia L. The War on Marijuana in Black and White. New York, NY; 2013. [Google Scholar]
- 50.Fernandez AD. How Far Up the River? Criminal Justice Contact and Health Outcomes. Soc Curr. 2019. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.