Abstract
During the COVID-19 pandemic, restaurant sanitation and disinfection have become more important than ever although customers can hardly check visually. The most recent research argues that one invisible element leaving people vulnerable to the health effects of COVID-19 is particulate matter (PM), micron-sized particles known to cause acute or chronic respiratory illnesses, including lung cancer. While research shows PM is emitted from cooking, this study examines indoor PM pollution of an open-kitchen full-service chain restaurant, where commercial cooking occurs in the dining room, as a case study. The results of a week-long field test showed offensively harmful levels of PM10 and PM2.5, far beyond US EPA and WHO standards, while ambient outdoor PM associated with the sample restaurant was safe. The study reveals that working or frequently dining in an open-kitchen restaurant where grilling or frying takes place is likely to cause respiratory health problems and elevate susceptibility to COVID-19 unless surveillance and preventative measures are taken. Based on our findings, implications and recommendations for the industry are provided.
Keywords: Particulate matter, Indoor air quality, Indoor air pollution, Open-kitchen restaurants
1. Introduction
As of September 2020, amid COVID-19, diners in selected states in the United States can return to restaurants as full capacity in-room dining is permitted. In compliance with Centers for Disease Control (CDC) recommendations (CDC, 2020), restaurants are expected to perform a course of hygiene practices that include cleaning, sanitization, disinfection, and ventilation. Adjusting to the so-called new normal, customers likewise pay more attention to health and safety than they did pre-COVID-19 when choosing a restaurant at which to dine. Among the types of restaurants to choose from in pre-pandemic times in the past decade, open-kitchen restaurants that have “nothing to hide” have been selected by a growing number of diners who are conscious about cleanliness, safety, and health (Chow et al., 2010; Sohn and Lee, 2018). Open-kitchen restaurants have been a popular design option, spanning the gamut from quick service to fine dining (Forbes, 2015; National Restaurant Association, 2017). Literature documents that transparency in terms of food quality and cleanliness has made the open kitchen concept grow very quickly (Sohn and Lee, 2018).
Moreover, open-kitchen restaurants provide intangible dining experiences that other restaurants cannot. For example, customers can see who is cooking their food, and under what conditions, in relatively full view. Before the advent of such restaurants, customers were accustomed to hearing horror stories regarding dirty kitchens behind closed doors. Since the kitchen is open to view, customers can watch the flames, steam, and hustle inside, all of which become part and parcel of the dining experience. In addition, the sights, sounds, and smells of cooking help whet the appetites of onlooking diners. Moreover, diners in open-kitchen restaurants are likely to perceive their food as tastier than those in closed-kitchen restaurants, according to Buell et al. (2014).
As the open kitchen concept proliferates, however, a certain level of discomfort and unpleasant dining experiences have been reported in the hospitality management literature (Byun and Jang, 2018). Among the negative experiences, cooking fumes are of particular concern since they are thought to have adverse health effects in humans (Neghab et al., 2017; Svedahl et al., 2009). Another stream of research in public health highlights cooking as a significant source of indoor particulate matter (PM) pollution that does harm to human health in both the home (Buonanno et al., 2014; Long and Koutrakis, 2000) and the commercial kitchen (Gysel et al., 2018; Taner et al., 2013). PM is a mixture of micron-size solid particles or liquid droplets in the air (EPA, 2006), and has been known to cause acute or chronic respiratory diseases, including heart and lung cancer (Cadelis et al., 2014; Valavanidis et al., 2008; WHO, 2013). The International Agency for Research on Cancer (IARC), affiliated with the WHO, classifies PM as a major component of air pollution and as carcinogenic to humans (WHO, 2013). Research shows that exposure to PM pollution from cooking may be responsible for a variety of respiratory health effects. For instance, See and Balasubramanian (2006) have demonstrated that chefs and other restaurant personnel are likely to experience elevated health risks due to PM exposure in the commercial kitchen. Occupational health researchers have also found that lung cancer rates are relatively higher among chefs (Ko et al., 2000; Lin et al., 2019).
PM pollution has become a vital point of concern under COVID-19. Emerging evidence shows a significant correlation between PM pollution and the spread of COVID-19 in the U.S., leading to a series of adverse health effects (Liang et al., 2020; Petroni et al., 2020; Wu et al., 2020). More specifically, Wu et al. (2020) provided empirical evidence in support of the correlation between exposure to PM pollution and COVID-19 mortality from an analysis of 3,080 counties in the U.S., demonstrating a 15% increase in the COVID-19 death rate with an increase of 1 μg/m3 of long-term exposure to PM2.5. They also reported that even short-term exposure to PM pollution has been attested to increase probability of viral infection. Another study by Zhu et al. (2020) exhibited a significant positive association of short-term exposure to PM2.5 and PM10 with confirmed COVID-19 cases in China. They argued that exposure to PM pollution is likely to make people more vulnerable to getting the coronavirus or to having worse outcomes if they are infected because it would have weakened their defenses against respiratory infections such as COVID-19. They emphasized that COVID-19 is a severe acute respiratory illness (SARS-CoV-2) and that exposure to PM pollution could contribute to the development of acute or chronic respiratory issues. Interestingly, Fisher et al. (2020) have demonstrated that a higher number of confirmed COVID-19 cases in the U.S. was found among those who patronized restaurants than among those who did not. They found that study participants who tested positive for the coronavirus were about twice as likely as those who tested negative to have dined at restaurants in the two weeks before they got sick. Public health experts in the U.S. have listed bars and restaurants as indoor environments in which the virus can spread relatively easily (Fisher et al., 2020; MLive, 2020), and data from states and cities in the U.S. have confirmed that many community outbreaks of the coronavirus have indeed centered around restaurants and bars (NYTimes, 2020). Moreover, popular restaurants throughout the country, in places like Nashville, Las Vegas, Atlanta, and Milwaukee, have had to close temporarily due to rising cases among restaurant employees (NYTimes, 2020). Most recently, Afshari (2020) and Saha and Chouhan (2020) averred that indoor air pollution resulting from cooking is a contributing factor to COVID-19.
As of September 2020, Dr. Anthony Fauci, America’s top infectious disease expert, admitted that coronavirus can spread indoors through the air and farther than six feet, and that the virus remains in the air for minutes to hours at a time (Reuters, 2020). Because epidemiologists have warned that indoor air pollution may play a role in the spread or exacerbation of COVID-19, it is important to examine indoor PM10 and PM2.5 pollution levels in restaurants—more specifically, in open-kitchen restaurant settings, where commercial cooking takes place near the dining area. Although literature has shown that the grilling or frying of meats emits a significant source of unhealthy indoor PM (Abdullahi et al., 2013; Gysel et al., 2018), not a single study in the hospitality management literature has investigated indoor air quality of an open-kitchen restaurant in the U.S., where the open-kitchen concept is most popular. There remains a large gap in literature addressing indoor PM pollution in open-kitchen restaurants in connection to the current pandemic situation. Therefore, the purpose of the present study is to establish a baseline assessment of indoor PM pollution in open-kitchen restaurant dining rooms and to offer public health officials and restaurant management insights to consider for ongoing development of enhanced cleaning protocols. Our hope is that these suggestions will help maintain safe and healthy restaurant environments for both customers and employees in a post-COVID world. To accomplish the purpose of the study, a series of field tests was conducted to assess real-time PM10 and PM2.5 concentrations in the dining room of an open-kitchen, full-service, chain-operated restaurant as a case study. In addition, ambient PM immediately outside of the restaurant was also monitored in relation to that of the dining room. The comparison would reveal the inherent and invisible condition contrary to that of the ambient environment immediately outside the restaurant.
The results of the study would highlight safe and healthy conditions that are invisible in the indoor dining space of an open-kitchen restaurant during (and after) the current pandemic, since indoor PM might play a role in elevating the health effects of COVID-19 (Afshari, 2020; Saha and Chouhan, 2020; Buonanno et al., 2009). The results would serve as empirical and quantitative evidence of indoor PM pollution in open-kitchen restaurants and be used for references in developing public health and safety protocols by public health officials and restaurant management for the “new normal” in the coming years. Ultimately, the findings of the study would offer a better understanding of dining room air quality in an open-kitchen environment and be utilized to surmise whether any sort of regulation should be mandated to keep the indoor environment of an open-kitchen restaurant safe and healthy.
2. Literature review
2.1. Particulate matter (PM)
According to the United States Environmental Protection Agency (EPA), particulate matter, or particle pollution, is a mixture of solid particles (e.g., dirt, dust, smoke, or other visible particles) or liquid droplets in the air (EPA, 2006). Although some particles can be seen with the naked eye, many others can be only detected with an electron microscope. For example, PM10 is comprised of coarse-mode particles (10 micrometers and smaller) while PM2.5 is comprised of fine-mode particles (2.5 micrometers) (EPA, 2006). The EPA has established a health-based standard for an acceptable concentration of PM in the atmosphere: the short-term standard (24-h or daily average) is 35 μg/m3 for PM2.5 and 150 μg/m3 for PM10. The standards of the World Health Organization (WHO) are 25 μg/m3 of PM2.5 and 150 μg/m3 of PM10, which are more stringent because the WHO has hypothesized that exposure to even low levels of particulate pollution can affect human health (WHO, 2016). These standards are for ambient outdoor environments. There are no standards for indoor environments, even though urban Americans spend 90% of their time indoors and some pollutants are often 2–5 times higher than typical outdoor concentrations (EPA, 1989). Multiple studies have found that humans and their activities generate considerable amounts of PM indoors (Afshari et al., 2005; Chang et al., 2020; Torkmahalleh et al., 2017). Such activities include cleaning (Chang et al., 2020) and cooking (Buonanno et al., 2014; Gysel et al., 2018; Torkmahalleh et al., 2017). Among the activities, PM emissions from commercial cooking are particularly enormous (Gysel et al., 2018).
2.2. PM pollution and COVID-19
The most recent research in public health regarding the coronavirus pandemic finds a correlation between PM pollution and COVID-19 health effects. Wu et al. (2020) of the Harvard School of Public Health show that an increase of only 1 μg/m3 of PM2.5 correlates with a 15% increase in the COVID-19 death rate. They contend that a small increase in long-term exposure to PM2.5 leads to a large increase in COVID-19 death rate. They suggest that air pollution should be closely monitored to protect human health both during and after the COVID-19 crisis. In Europe, where COVID-19 death rates were highest in April 2020, the Italian Society of Environmental Medicine found a significant correlation between daily PM10 levels exceeding the legal limit of 50 μg/m3 and the spreading of COVID-19 infection (Setti et al., 2020). The same scholars contend that the frequency of PM10 levels exceeding the limit in Lombardy, Italy, where the COVID-19 death rate was highest at the beginning of the pandemic, has been much higher than in Southern Italy.
In addition, research shows that PM is likely to act as a “carrier” of viruses. As evidenced, Zhao et al. (2019) demonstrated that the majority of positive cases of highly pathogenic avian influenza H5N2 in Iowa in 2015 might have been the result of airborne viruses carried by fine particulate from infected farms both within the same state and from neighboring states. Moreover, Qin et al. (2020) analyzed the microbiome of airborne particulate matter (PM2.5 and PM10) in Beijing over a period of 6 months in 2012 and 2013. Temporal distribution of the relative abundance of the microbiome on particulate matter showed the highest incidence of viruses during January and February, which was known to be the period of highest concentration of PM in any given year in Beijing. These studies suggest that air pollution particles do harbor microbes and can carry the viruses, causing disease over considerable distances.
In another line of COVID-19 outbreak research, Qian et al. (2020) contend that indoor environments are more serious than their outdoor counterparts. Among 318 identified outbreaks in 320 Chinese cities between 4 January and 11 February 2020, they found that all of the outbreaks, with one exception, occurred in an indoor environment. In addition, they demonstrate that indoor restaurant environments are ranked third (after the home and public transportation) among places where the outbreaks have occurred. Li et al. (2020) and Lu et al. (2020) confirm that the COVID-19 outbreak tied to a restaurant in China was due to the airborne spread of the virus inside the restaurant.
2.3. PM emissions from commercial cooking
According to Gysel et al. (2018), grilling burgers at fast food restaurants releases twice as much PM into the air per year as truck and factory emissions. They argue that restaurant operations outfitted with charbroilers (chain-driven and under-fired) are responsible for about 84% of the PM2.5 emissions in the greater Los Angeles Basin. Ample research shows that commercial cooking also contributes to ambient particle emissions in urban environments (Li et al., 2015; Sjaastad et al., 2010; Torkmahalleh et al., 2012). In particular, charbroiling emits more PM2.5 than all other cooking activities due to the characteristics of the cooking methods and fuel types in question (Li et al., 2015). Among the latter, gas is likely to produce higher PM levels than electricity. Sjaastad et al. (2010) created a kitchen typical of those in Western European restaurants, measuring 19 square meters (62 feet) and containing both a gas stove and an electric stove with a canopy hood. They fried 17 pieces of beefsteak, each weighing about a pound, in both margarine and soybean oil for 15 min. The results showed higher levels of ultrafine particles produced via gas than electric. The level of PM emission was found to correlate with the type of oil used and the temperature to which it was heated. Torkmahalleh et al. (2012) showed that soybean, safflower, canola, and peanut oils produced lower PM2.5 emission than corn, coconut, and olive oils. They also found a correlation between the smoke point of the oil in question and PM emission rates. In their later study, they argued that cooking method, type of pan, food, additives, cooking temperature, and ventilation were all influential factors affecting cooking PM emission rates and resulting concentrations (Torkmahalleh et al., 2017).
2.4. Effects of particulate matter (PM) from cooking on human health
The International Agency for Research on Cancer of WHO has also classified cooking fumes as likely carcinogenic (Straif et al., 2006). Research in the medical field has shown cooking to be a significant source of indoor air pollution that causes adverse health effects such as lung cancer, as well as cancers of the bladder and cervix (Sjaastad et al., 2010; Svedahl et al., 2009). These studies contend that those who cook on a daily basis would have the highest risk. Occupational health researchers have found that cancer rates are relatively higher among chefs (Ko et al., 2000; Lin et al., 2019). In Taiwan, high lung cancer rates among chefs have been linked to the practice of tossing food in a wok, often in a confined space, which increases the concentration of hot oil in the cook’s breathing zone. Although smoking is the main cause of lung cancer in most countries, only 10% of women with lung cancer smoke in Taiwan. By comparison, 86% of Taiwanese men with lung cancer smoke (Ko et al., 2000). The evidence suggests that it is exposure to cooking fumes that accounts for the high rates of lung cancer in women, despite their low smoking rates. The same research argues that the more time women spend cooking food, the more at risk they are for lung cancer. Insufficient ventilation might be also the cause of lung cancer since higher cases of the cancer were found among chefs who did not have fume extractors in their kitchens than among those who did (Sjaastad et al., 2010). Without effective ventilation, cooking-related PM emissions are likely to accumulate in the kitchen and travel into the dining room. Therefore, it is essential to have high capacity ventilation systems in commercial kitchens not only for kitchen staff members, but also for customers in dining areas.
2.5. Indoor PM pollution in restaurants
Previous research on indoor PM pollution in restaurants is scarce. Among the few extant studies, those of Wallace and Ott (2011) and Ott et al. (2017) constitute the only research documenting empirical evidence of indoor air quality of restaurants in the United States. Wallace and Ott (2011) measured the indoor air quality of 22 restaurants in several states such as Maryland, Virginia, and California by counting ultrafine particles 1 μm or smaller in size while dining in the restaurants themselves. Among the different types of restaurants at which they dined—including French, Chinese, Indian, and steakhouses—they found that restaurants with open-flame cooking or grills located in dining areas in close proximity to patrons had relatively high ultrafine particle concentrations. However, the duration of their measurement lasted only for two hours during their meal. PM10 and PM2.5 were not reported in their investigation (see Table 1 ). Ott et al. (2017) measured PM2.5 at a Japanese steakhouse where customers sit close to the grill under an overhead ventilation hood and a chef cook dinner in front of them. They observed a peak of over 300 μg/m3 of PM2.5 while the mean for the duration of a two-hour dinner was moderately high at 38.4 μg/m3. Research shows, however, that intermittent events of high particle concentration levels are detrimental to respiratory health (Valavanidis et al., 2008; Zhu et al., 2020).
Table 1.
Restaurant PM studies in literature.
| Authors | Discipline | Site Location | Restaurant Type | Particle Size | Mean | Maximum | Measurement Unit | Measurement Period | Measurement Duration (hr.) |
|---|---|---|---|---|---|---|---|---|---|
| Lee et al. (2001) | Environmental Science | Hong Kong | Korean BBQ | PM10 | 1,442.0 | 4,052.0 | μg/m3 (Mass concentration) | Dinner | 2 |
| PM2.5 | 1,167.0 | 1,911.0 | |||||||
| Western Canteen | PM10 | 38.8 | 55.1 | Lunch | 2 | ||||
| PM2.5 | 21.8 | 27.0 | |||||||
| Lee et al. (2007) | Environmental Engineering | Korea | Korean BBQ with plate on gas | PM10 | 32.0 | – | Dinner | 2 | |
| PM2.5 | 71.1 | – | |||||||
| Korean BBQ with grill over charcoal | PM10 | 169.4 | – | Dinner | 2 | ||||
| PM2.5 | 124.1 | – | |||||||
| Wilson et al. (2011) | Public Health | New Zealand | BBQ | PM2.5 | 368.0 | 1,472.0 | Dinner | 2 | |
| 166.0 | 932.0 | ||||||||
| Wallace and Ott (2011) | Environmental Epidemiology | USA | French | PM1.0 | 228 | – | × 103 cm−3 (Particle count) | Dinner | 1 |
| Indian | 222.0 | – | 1.3 | ||||||
| Chinese | 203.0 | – | 1.3 | ||||||
| Sports Tavern | 88.0 | – | 0.5 | ||||||
| Steak House | 16.0 | – | 1.2 | ||||||
| Ott et al. (2017) | Environmental Science | USA | Japanese Steakhouse | PM2.5 | 38.4 | 300.0 | μg/m3 (Mass concentration) | Dinner | 1.4 |
| Italian | 337.0 | 600 | 1.5 |
A study conducted by Lee et al. (2001) is the first empirical research performed outside of the U.S. documenting indoor PM levels in restaurants. They measured indoor PM of four different restaurants for a two-hour period. Among the four restaurants—including a Western canteen, Chinese dim sum, hot pot, and Korean BBQ—average PM levels in the Western canteen and Chinese dim sum restaurants were found to be lower than those of Korean BBQ and Chinese hot pot. PM levels in the Western canteen restaurant, where food was cooked in the kitchen, were the lowest. The Chinese dim sum restaurant, which offered dim sum in steaming equipment installed in the dining area, exhibited lower average PM levels as well. By contrast, the dining area of the Chinese hot pot restaurant showed significantly higher PM levels than those of the Chinese dim sum and Western canteen restaurants. However, the Korean BBQ restaurant, where food is cooked in oil on a hot frying pan in the dining area, showed obscene levels of 1,442 (SD = 301) μg/m3 of PM10 and 1,167 (SD = 173) μg/m3 of PM2.5 while US EPA regards 150 μg/m3 of PM10 and 35 μg/m3 of PM2.5 are acceptable. The researchers noted that the cooking methods used for food preparation in both the dining area and kitchen were inadequately ventilated, thus leaving employees and customers easily exposed to the PM being generated. In New Zealand, Wilson et al. (2011) conducted an indoor PM2.5 investigation in four BBQ restaurants. They observed a maximum of 1,472 μg/m3 and an average of 368 μg/m3. Taner et al. (2013) measured PM in 14 restaurants that cooked with charcoal in Kocaeli, Turkey and investigated the human health risks associated with PM2.5 for each restaurant. They found that charcoal combustion and indoor activities produced fine particles in the air, thereby increasing carcinogenic risk, and that the total hazard quotient was above the acceptable limit for each restaurant.
Scientists of countries where open-flame cooking is popular have conducted a number of empirical studies examining restaurant air quality in the context of environmental science and public health. Lee et al. (2007) examined PM mass concentrations of BBQ restaurants in which tabletop grills with a ventilation system were installed in Korea. They observed 7.2 μg/m3 of PM2.5 and 12.6 μg/m3 of PM10 in the restaurants before grilling. As the stainless plate was being heated on a liquefied pressurized gas (LPG) stove, the PM concentrations were found to nearly double. As expected, PM concentrations sharply increased as the meat was grilled on the plate, reaching 32.0 μg/m3 of PM2.5 and 71.1 μg/m3 of PM10. They also examined the difference of PM concentrations by heat source and grill type: stainless steel plate with LPG vs. stainless steel grill with charcoal. They observed higher PM concentrations—as high as 124.1 μg/m3 of PM2.5 and 169.4 μg/m3 of PM10—when cooking on a grill with charcoal. They argued that drippage of incompletely combusted fat onto the charcoal flames was the cause.
In sum, we assume that PM pollution would be present in the dining room of an open-kitchen restaurant where commercial cooking involving grilling or frying is performed wide open to the dining area. While it is unknown whether particulate matter pollution plays any role in the spread of the coronavirus, the presence of indoor PM in the restaurant is still detrimental to the health and well-being of employees and frequent customers. Accordingly, the public and restaurant operators alike should be made aware. Thus, this study, conducting a field test tracking indoor PM in the dining room of an open-kitchen restaurant in the U.S. will be able to provide quantitative and empirical evidence for the public sector toward implementing new regulation, for the industry to seek out a mitigation effort, and for hospitality management literature to expand into a post-COVID-19 era.
3. Methodology
3.1. Sampling location
Open-kitchen restaurants are designed to provide customers with a feeling of elevated hygiene and transparency standards toward instilling a sense of quality and trust (Sohn and Lee, 2018; Time, 2012). However, cooking is known to emit micron-size appreciable aerosol that is harmful to human health, especially regarding the respiratory system. The latest research shows that the micron-size aerosol known as particulate matter (PM) is likely to exacerbate the effects of COVID-19 (Setti et al., 2020; Wu et al., 2020). Therefore, the primary goal of this study was to quantify and document indoor PM in the dining room of an open-kitchen restaurant to see whether additional cleaning of invisible pollutants in the restaurant is necessary beyond distancing and disinfecting high-touch points. To achieve this goal, an upscale casual open-kitchen full service restaurant in the southeastern United States was selected as the sample for our case study. One of the authors was a staff member at the restaurant at the time and able to obtain management’s approval to conduct field tests monitoring real-time indoor PM in the dining room. Said restaurant is one of the fastest-growing upscale casual chain restaurants in North America and has a standalone structure in an outdoor shopping mall. It serves primarily grilled meats and pastas during lunch and dinner. The restaurant has a Type 1 commercial kitchen hood ventilation system for such kitchen appliances as fryers and griddles that produce grease and smoke in accordance with building code regulations. The exhaust system is in place to remove heat, grease-laden steam, and cooking smoke in the kitchen. Separate from the kitchen ventilation system, the dining ventilation is integrated into the air conditioning system via natural ventilation when customers and employees enter and exit the restaurant entrance and two patio doors. The restaurant has a seating capacity of 370. The number of covers is approximately 400 during weekdays and 600 on weekends. Details about the restaurant are listed in Table 2 .
Table 2.
Sampling site information.
| Facility Type | Open-kitchen |
|---|---|
| Kitchen Hood | Type 1 with makeup air supply |
| Type of Operations | Chain |
| Style | American bar and grill |
| Food Type | Grilled meats and pastas |
| Meal Serving | Lunch and Dinner Sunday Brunch |
| Seating Capacity | 370 |
| Daily covers on average | 400 weekdays 600 weekends |
| Number of Kitchen Staff (Full & part time) | 30 |
| Number of front of House Staff (Full & part time) | 60 |
| Building space (Sq. ft.) | 8500 |
| Dining space (Sq. ft.) | 5100 |
| Dining layout | Open space |
| Ceiling Height (ft.) | 9 |
3.2. Sampling instrument
To measure indoor PM10 and PM2.5 concentrations of the dining room in the recruited restaurant, a portable real-time particle counter (specifically, a Lighthouse Worldwide Solutions’ Model Handheld 3016 IAQ instrument) was used, which is equipped with a laser-diode light source and collection optics for particle detection. The same instrument has been used in previous academic studies monitoring indoor PM (Chang et al., 2020; Ramos et al., 2014). Two instruments were ordered and calibrated before being shipped to the researchers. One device was placed on a four-foot high countertop in the center of the dining room to collect air samples from the breathing zone of seated customers. For outdoor measurements, the other device was set on a five-foot counter outside of the restaurant where no public access was granted. Both devices were set to take samples for a consecutive 300 s (5 min) with a 10-second pause between samples, as administered in other studies (Chang et al., 2020; Lee et al., 2007).
3.3. Sample collection
Air monitoring investigations were carried out in the third week of January 2019 at the selected restaurant during dinner hours (4 p.m. to 10 p.m.). PM measurements were taken continuously for 6 h a day for the week so that temporal variations could be examined. A descriptive analysis was performed to obtain mean, maximum, minimum, and standard deviation for PM10 and PM2.5 levels. A series of line charts was created to display a pattern of PM concentrations over time.
4. Results
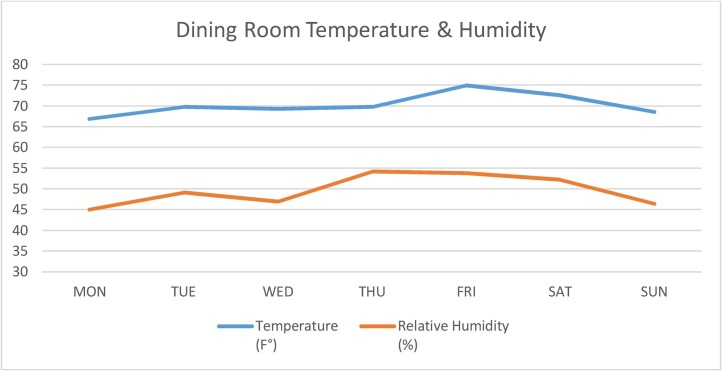
Basic environmental parameters such as temperature and relative humidity of the dining room have been measured and presented in Table 3 and Fig. 1 . The dining room temperature was well maintained in a comfortable range, from 66.9 °F (SD = 0.5 °F) to 74.9 °F (SD = 0.9 °F), throughout the week of the field test. The small standard deviations showed that indoor room temperatures were consistent. Relative humidity percentages were also stable between 45% and 54%.
Table 3.
Dining room temperature and relative humidity.
| Dining Room | Mon | Tue | Wed | Thu | Fri | Sat | Sun |
|---|---|---|---|---|---|---|---|
| Temperature (F°) | 66.9 | 69.8 | 69.2 | 69.8 | 74.9 | 72.6 | 68.6 |
| S.D. | 0.5 | 1.0 | 0.7 | 0.6 | 0.9 | 0.8 | 0.5 |
| Relative Humidity (%) | 45.0 | 49.1 | 46.9 | 54.2 | 53.8 | 52.1 | 46.4 |
| S.D. | 2.3 | 3.1 | 1.8 | 3.4 | 2.7 | 1.6 | 1.6 |
aS.D. stands for Standard Deviation.
Fig. 1.
Dining room temperature and relative humidity.
4.1. PM10
Each PM mass concentration level observed in this study was a five-minute sample. Technically, a set of 12 samples was supposed to be collected for each hour (60 min / 5-min sample = 12 samples), but since there was a 10-second pause between samples (12 samples × 10-second pause = 120 s / 60 s = 2 min), there were approximately 11 samples an hour. Overall, there were 66 samples collected for the 6-h dinner business per day.
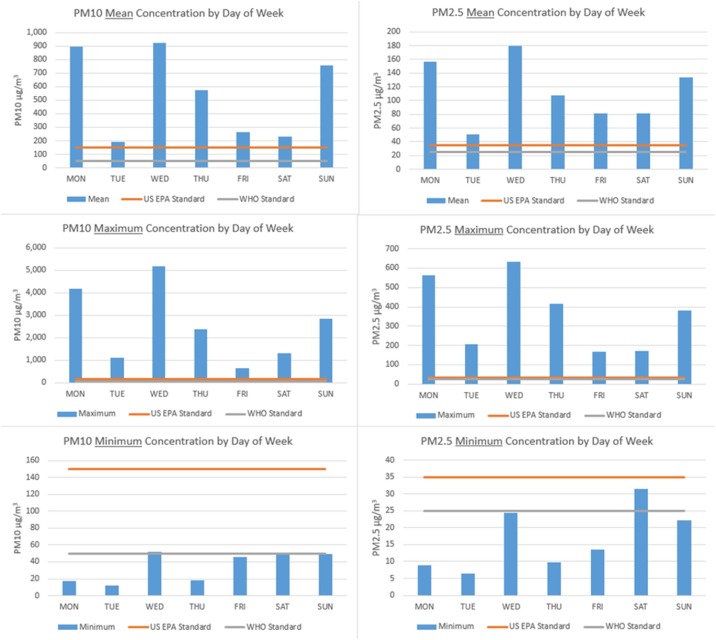
Among the 66 samples observed, the highest PM10 levels for each day are shown in Table 4 and in Fig. 2 , ranging from 634.8 μg/m3 on Friday to 5,172.1 μg/m3 on Wednesday. The latter level was the highest, followed by 4,180 μg/m3 on Monday. Despite being only five-minute samples, they were thought to show an obvious negative impact on short-term exposure. Any level over 4,000 μg/m3 is unheard of even in the deadliest polluted cities (Tara, 2018) and was closer to levels found in lab experiments measuring PM10 from the exhaust pipes of running cars. Friday’s 634.8 μg/m3 was the lowest in the given week, followed by 1,092 μg/m3 of PM10 on Tuesday.
Table 4.
PM10 field test results.
| Day of Week | Statistics | PM10 (ug/m3) | US EPA Standards (ug/m3) | WHO Standards (ug/m3) |
|---|---|---|---|---|
| Monday | Mean | 896.3 | 150 | 50 |
| Maximum | 4,180.0 | |||
| Minimum | 17.8 | |||
| S.D.a | 1,050.6 | |||
| Tuesday | Mean | 190.6 | ||
| Maximum | 1,092.0 | |||
| Minimum | 11.9 | |||
| S.D. | 217.7 | |||
| Wednesday | Mean | 922.4 | ||
| Maximum | 5,172.1 | |||
| Minimum | 51.9 | |||
| S.D. | 961.9 | |||
| Thursday | Mean | 576.1 | ||
| Maximum | 2,372.8 | |||
| Minimum | 18.5 | |||
| S.D. | 557.0 | |||
| Friday | Mean | 263.7 | ||
| Maximum | 634.8 | |||
| Minimum | 46.1 | |||
| S.D. | 155.6 | |||
| Saturday | Mean | 228.2 | ||
| Maximum | 1,315.4 | |||
| Minimum | 50.9 | |||
| S.D. | 161.9 | |||
| Sunday | Mean | 759.8 | ||
| Maximum | 2,830.7 | |||
| Minimum | 49.5 | |||
| S.D. | 648.5 | |||
| Measurement Duration | 6 h | 24 h | 24 h | |
Fig. 2.
PM10 and PM2.5 field test results.
Note: Two straight lines in each graph are US EPA & WHO standards.
Daily PM10 averages of 6-h dinner operations for a week are presented in Table 4 and Fig. 2 as well. While the acceptable EPA standard for PM10 is 150 μg/m3 for a 24-h period, all of the daily PM10 averages were much higher than the standard, ranging from a minimum of 190.6 (SD = 217.7) μg/m3 on Tuesday to a maximum of 922.4 (SD = 961.9) μg/m3 on Wednesday. The standard deviations (SDs) were greater than those of the mean, thus depicting an abnormal distribution of data and their deviation from the mean value. The SDs of the remaining days were also large enough to show that the observed PM levels had large variations, which might indicate that high PM levels were monitored in a certain period during the 6-h business period, such as 7 p.m. to 9 p.m. of the busy dinner hours as exhibited in Fig. 3 .
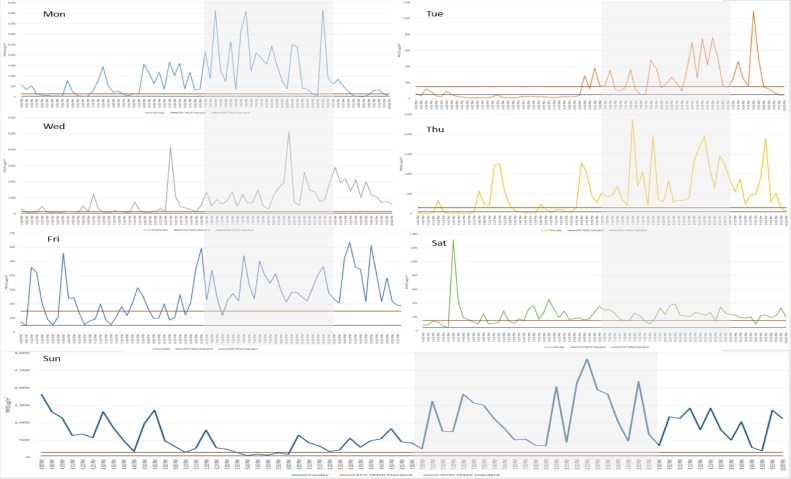
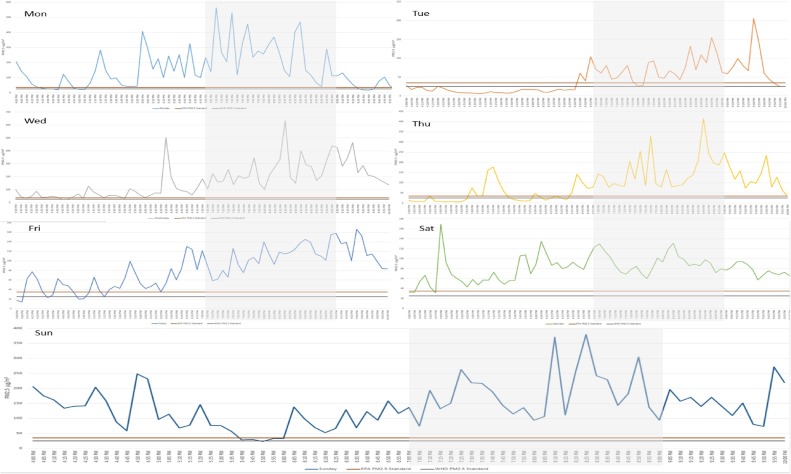
Fig. 3.
Temporal variations of dining room PM10.
Note: Two straight lines in each graph are US EPA & WHO standards.
The high 6-h daily PM10 averages are substantiated when the stringent WHO standard of 50 μg/m3 is applied. Among the 7 days, the averages of Wednesday and Monday were the highest—922.4 (SD = 961.9) μg/m3 and 896.3 (SD = 1,050.6) μg/m3, respectively—followed by Sunday’s 759.8 (SD = 648.5) μg/m3. A minimum PM10 level among the 66 samples for each day is also presented in Table 4. Each PM10 minimum level in the dining room was comparable or even lower than that of the strict WHO limit of 50 μg/m3, indicating there was a brief period of time (at least for five minutes) on each day when the dining room air quality was acceptable.
As shown in Fig. 3, the PM10 temporal variation of each day is plotted on a chart with the EPA and WHO standards applied over time. A series of sharp peaks and troughs higher than those two straight lines of the standards over time are displayed. In general, gentle spikes and troughs appeared in the early, so-called happy hours (from 4 p.m. to 7 p.m.) on weekdays from Monday to Thursday and excluding the weekend. This pattern somewhat makes sense because a busy weekend begins late Friday afternoon. The sharpest spikes were mostly monitored during the prime dinner hours of 7 p.m. to 9 p.m., as shaded in the charts. As a full-service open kitchen restaurant is being operated, business over the course of the day comes in waves. As the tables get up and are cleaned, the next guests are brought in to have their orders taken. These waves in service are represented by the peaks and troughs in PM pollution observed in the charts. On Saturday, it was interesting to observe that the peaks and troughs of PM10 were gentle in overall unlike those of others. The PM10 trends of late evening hour on Tuesday and on Friday exhibited a difference as a few sharp peaks were also observed after prime dinner hours.
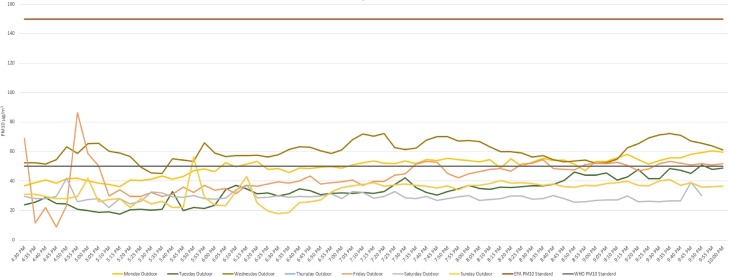
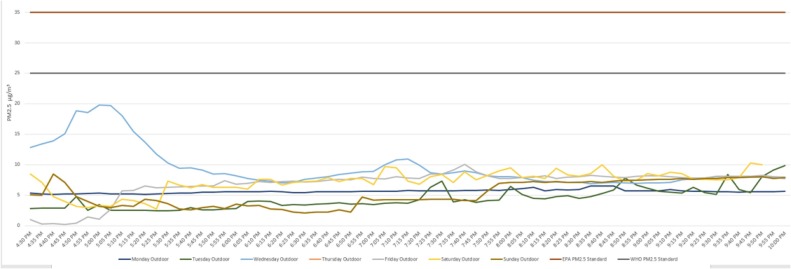
As exhibited in Fig. 4 , outdoor PM10 temporal variations are plotted over time. Observed outdoor PM10 trends for the week were below the EPA standard of 150 μg/m3. The trends overlapped either over or below the WHO standard limit of 50 μg/m3. As shown, outdoor PM levels were much lower than those of the dining room inside the restaurant. Therefore, it can be assumed that the indoor PM pollution is not associated with outdoor PM pollution. If anything, indoor air quality could be enhanced if outdoor air was brought into the dining room.
Fig. 4.
Outdoor PM10 temporal variations.
Note: Two straight lines in each graph are US EPA & WHO standards.
4.2. PM2.5
Among the 66 measurement samples collected for six hours a day for the week, a peak level of PM2.5 for each day is shown in Table 5 and Fig. 2, ranging from the lowest (166.5 μg/m3 of PM2.5 on Friday) to the highest (631.6 μg/m3 of PM2.5 on Wednesday). As exhibited, that on Wednesday was the highest, followed by 562.7 μg/m3 of PM2.5 on Monday. A 5-minute exposure to over 500 μg/m3 of PM2.5 is critical enough to pose a health concern in both the short and long term. Even the peak level of 166.5 μg/m3 of PM2.5 on Friday would be considered high enough to issue an alert people in the community to take precaution if it were monitored outdoors in a polluted city. A minimum level among the samples for each day was retrieved and is charted in Fig. 2. As shown, all were below the EPA PM2.5 standard of 35 μg/m3, meaning there was a brief period of each day during which the dining room air quality was acceptable.
Table 5.
PM2.5 field test results.
| Day of Week | Statistics | PM2.5 (ug/m3) | US EPA Standard (ug/m3) | WHO Standard (ug/m3) |
|---|---|---|---|---|
| Monday | Mean | 157.0 | 35 | 25 |
| Maximum | 562.7 | |||
| Minimum | 8.9 | |||
| S.Da | 139.2 | |||
| Tuesday | Mean | 50.9 | ||
| Maximum | 205.8 | |||
| Minimum | 6.4 | |||
| S.D. | 41.0 | |||
| Wednesday | Mean | 179.5 | ||
| Maximum | 631.6 | |||
| Minimum | 24.3 | |||
| S.D. | 131.7 | |||
| Thursday | Mean | 107.9 | ||
| Maximum | 413.9 | |||
| Minimum | 9.7 | |||
| S.D. | 79.8 | |||
| Friday | Mean | 81.1 | ||
| Maximum | 166.5 | |||
| Minimum | 13.6 | |||
| S.D. | 40.6 | |||
| Saturday | Mean | 81.6 | ||
| Maximum | 169.2 | |||
| Minimum | 31.4 | |||
| S.D. | 26.3 | |||
| Sunday | Mean | 134.0 | ||
| Maximum | 379.3 | |||
| Minimum | 22.2 | |||
| S.D. | 82.2 | |||
| Measurement Duration | 6 h | 24 h | 24 h | |
S.D. stands for Standard Deviation.
Daily PM2.5 averages for 6-h dinner operations during the week are presented in Table 5. While the acceptable EPA standard for PM2.5 is 35 μg/m3 for a 24-h period, all of the daily PM2.5 averages were much higher than the standard, ranging from the lowest at 50.9 (SD = 41) μg/m3 on Tuesday to the highest of 179.5 (SD = 131.7) μg/m3 on Wednesday. When the WHO standard of 25 μg/m3 is applied, indoor PM2.5 pollution in the restaurant would be considered harmful during the six hours. Among the 7 days, the averages of Wednesday and Monday were the highest—179.5 (SD = 131.7) μg/m3 and 157.0 (SD = 139.2) μg/m3, respectively—followed by Sunday’s average of 134.0 (SD = 82.2) μg/m3.
Continuous PM2.5 observations for each day, plotted on a chart with EPA and WHO standards aligned over time, are shown in Fig. 5 . There was a series of sharp peaks and troughs above and below those standards. As in the case of PM10, the sharp and successive spikes generally appeared in waves, in particular, during the prime dinner hours of 7 p.m. to 9 p.m., as shown in the shaded timeframe of Fig. 5. During the happy hours from 4 p.m. to 7 p.m., there were gentle spikes on weekdays and sharp spikes over the weekend. The sharp spikes during happy hours were more obvious on weekends—i.e., from Friday to Sunday. Whereas dining room PM2.5 levels after prime dinner hours generally showed signs of settling, those of Friday were the opposite. Regarding both PM10 and PM2.5 on Saturday, it was interesting to monitor that the Saturday PM2.5 trended far above the acceptable standards during the entire day while that of the Saturday PM10 did not.
Fig. 5.
Temporal variations of dining room PM2.5.
Note: Two straight lines are US EPA & WHO standards.
Outdoor PM2.5 temporal variations are shown in Fig. 6 . The observed PM2.5 trends for the week were under both the EPA standard of 35 μg/m3 and the WHO standard limit of 50 μg/m3. Outdoor air quality during the weeklong field test was much better than inside the dining room of the restaurant. Thus, indoor PM2.5 pollution is not brought in from the outdoors. It also appears that outdoor air could be brought indoors to enhance dining room air quality.
Fig. 6.
Outdoor PM2.5 temporal variations.
5. Conclusions and discussion
Rarely addressed in the hospitality management domain, this study is the first empirical investigation uncovering compelling evidence of harmful PM pollution in an open-kitchen restaurant. While the study highlighting unhealthy indoor PM concentrations in occupied hotel guestrooms is considered to be the first empirical evidence in the hospitality management literature (Chang et al., 2020), the findings of the current study extend the literature by revealing hazardous indoor PM pollution in the dining room of an open-kitchen restaurant, which is in need of attention. As PM pollution has become a vital point of concern under COVID-19, the results of this study illuminate the unsafe and unhealthy environment that is invisible to occupants in an open-kitchen restaurant. They would enlighten public health officials and restaurant management to the vulnerability to COVID-19 in open-kitchen restaurants associated with their hazardous indoor PM concentrations. The results of our week-long field test provide empirical evidence that leads to the following conclusions.
First, our study confirms that commercial cooking emits an excessive level of indoor PM concentration. Therefore, a serious indoor PM pollution is likely present in the dining room of an open-kitchen restaurant where grilling meats or frying with oil is carried out. The results are aligned with previous studies in public health (Ott et al., 2017; Wallace and Ott, 2011), demonstrating high particle concentrations in the dining rooms of restaurants with open-kitchen designs. The PM levels observed in our study were much higher than theirs. This result may be due to the large volume of food that the sample restaurant handles throughout a given day. Moreover, our field test was conducted for six hours a day over the course of a full week, compared to the two-hour samplings of their studies. Therefore, our results much more closely represent reality and carry more weight in terms of gauging the severity of, and long-term exposure to, hazardous indoor PM pollution.
Second, our results provide evidence that there may be serious health risks when working regularly or dining frequently in open-kitchen restaurants. We uncover that dining room PM during six-hour dinner business hours is hazardous enough to put the health of employees and frequent customers at risks. Not only are the six-hour PM averages that are much higher than those of EPA and WHO standards alarming, but so do the maximum levels observed pose acute (Soppa et al., 2014) or chronic health concerns (Valavanidis et al., 2008). In particular, the PM temporal variations for the busy dinner hours of 7 p.m. to 9 p.m. show sharp spikes far above acceptable standards. Those peaks correlate with the high volume of meals produced in the prime dinner hours. Although the sharp PM surge appear briefly, research shows that the high particle concentration occurring erratically is detrimental to respiratory health (Valavanidis et al., 2008; Zhu et al., 2020). Public health experts argue that there are short-term effects of PM pollution on human respiratory, cardiovascular, nervous, and immune systems, as well as reproductive development (Afshari et al., 2005; Huang et al., 2019). Long-term exposure is more serious according to Valavanidis et al. (2008), whose study asserts that events of high particle concentration levels are associated with adverse health effects in the long run. Therefore, the obscene indoor PM levels observed in the present study provide empirical evidence that indoor environments where commercial cooking is performed may leave employees and customers vulnerable to adverse health effects, especially those affecting the respiratory system like COVID-19. Exposure of those personnel working in the kitchen is assumed to be much higher than those of wait staff members and frequent customers in the restaurant, as previous studies have asserted (Sjaastad et al., 2010).
Third, our study reveals that an open-kitchen restaurant may no longer be considered the clean, healthy, and safe restaurant that many have perceived it to be. As Byun and Jang (2018) have exhibited customers’ perception of service failure in an open-view setting as one particular disadvantage of open-kitchen restaurants, our study uncovers another weakness of the functional design of open-kitchen restaurants when taking indoor air quality into account. The unexpected obscene levels of the results have led to further analysis of long-term exposure, as shown in Table 6 . The results of our week-long field test show that indoor PM in the dining room of an open-kitchen restaurant is high enough to pose not only short-term but also long-term health risks for staff members and frequent customers in the restaurant. As shown in Table 6, the 42-h averages of PM10 and PM2.5 for the entire week are 548.1 μg/m3 (SD = 701.0) and 113.1 (SD = 97.0) μg/m3, respectively. While the lenient US EPA limits are 150 μg/m3 of PM10 and 50 μg/m3 of PM2.5 for 24 h, the observed PM levels would raise a serious health concern if the exposure were to occur repeatedly over a career- or lifelong period. Long-term exposure to PM is more serious according to the WHO and EPA (EPA, 2018; WHO, 2016). That is why the guidelines for long-term PM pollution are different and stricter than those for 24-h standards. For instance, the WHO dictates that the annual mean of PM10 should be 20 μg/m3 or under, and that the annual mean of PM2.5 should be 10 μg/m3 or lower. The EPA’s annual standard for PM2.5 is 12 μg/m3; there is no EPA annual standard for PM10. While acceptable annual averages are below 20 μg/m3, our 42-h averages are 548.1 μg/m3 of PM10 and 113.1 μg/m3 of PM2.5, which are far above the accepted standards. As indicated earlier, one of co-authors of this study was an employee of the sample restaurant and had worked over 40 h during the week of the field test. Upon our discovery, he said, “I had spent hundreds of hours for months working in this polluted environment unknowingly. The worst piece is that this restaurant (and many others like it) is not aware of the risk to which it is exposing their guests and employees each day. Restaurant management and diners should be made aware of hazardous PM levels and the possible effects. My deepest sympathies go out to the chefs who are likely the most exposed.” For the sake of comparison, the average annual PM pollution levels of Delhi, India, a polluted urban city that is home to 25.7 million people, were 292.3 μg/m3 of PM10 and 143.1 μg/m3 of PM2.5 in 2018 (USA Today, 2019). Residents of Delhi are well aware of the city’s poor air quality, so they are advised to protect themselves from exposure by wearing a mask. The national government has also made a relentless effort to reduce the air pollution. Obviously, neither full-time employees nor frequent customers of the sample restaurant are aware of this. They must now face the reality that the dining room environment where they spend a fair amount of time working or dining on a regular basis is comparable to that of Delhi, India, where air pollution is at a seriously high level. No regulations are currently in place to keep the indoor air pollution monitored and controlled for public health.
Table 6.
PM field test results.
| PM Size | Statistics | Indoor PM Mass (μg/m3) | US EPA Standard (μg/m3) | WHO Standard (μg/m3) |
|---|---|---|---|---|
| Mon. – Sun. | ||||
| PM10 | Mean | 548.1 | – | 20 |
| Maximum | 5,172.1 | |||
| Minimum | 11.9 | |||
| S.Da | 701.0 | |||
| PM2.5 | Mean | 113.1 | 12 | 10 |
| Maximum | 631.6 | |||
| Minimum | 6.4 | |||
| S.D. | 97.0 | |||
| Measurement Duration | 42 h | 1 year | 1 year | |
S.D. stands for Standard Deviation.
Lastly, our results infer that open-kitchen restaurants are likely to be the indoor environment where occupants are susceptible to health effects of COVID-19. As Wu et al. (2020) argue, a long-term exposure to 1 μg/m3 of PM2.5 is associated with a 15% increase in the COVID-19 death rate, meaning that kitchen personnel in the subject restaurant are likely to be very much susceptible to the health effects of COVID-19, which is a potentially fatal respiratory disease. Interdisciplinary research investigating a correlation between exposure to indoor PM emitted from commercial cooking and the health effects of COVID-19 is suggested. Since previous studies contend that PM plays a role in the spread of infectious viruses (Setti et al., 2020; Zhao et al., 2019) and microbiomes (Qin et al., 2020), further interdisciplinary research assessing whether indoor PM resulting from commercial cooking would exacerbate the spread of contagious viruses in the poorly ventilated dining rooms is recommended. Investigating the air quality of the brew-pub restaurant in Michigan where 85 people were contracted with COVID-19 in mid-June 2020 (CNN, 2020) can be a great start to begin the study. In essence, local health authorities should take immediate action to audit indoor PM levels in open-kitchen restaurants where a large volume of grilled meats or fried foods are cooked and served for public and occupational health. In addition, public health policymakers should consider mandating proper regulations on indoor air quality in restaurants to maintain the health and well-being of employees and customers for the new normal after COVID-19.
To reduce harmful indoor PM levels in the dining space of an open-kitchen restaurant, the following actions may be taken. First, restaurant management should check the kitchen hood ventilation system to determine whether it is functioning properly. Hood ventilation is key to keeping the kitchen clean and preventing harmful PM from traveling to the dining room. A properly working hood system should effectively vent cooking effluents. It is recommended to hire certified engineers and to check the entire kitchen hood ventilation system, including the makeup air system, which is required in a commercial kitchen by law and in accordance with local building code regulations. The system vents out all smoke, grease, odors, and PM generated by the cooking process through a hood system by supplying fresh air to the kitchen. Thus, restaurant management should make sure that the kitchen hood ventilation system is properly working and preventing air pollutants from traveling to the dining area. Also, Hood filters that are not cleaned often enough can clog and compromise the airflow of a hood, which decreases hood performance. Thus, rigorous hood filter maintenance should be implemented on a regular basis.
Second, open-kitchen restaurant brands should investigate which particular menu items emit the most harmful PM emissions in the kitchen. Prior literature reported that hazardous PM emissions are dependent on raw food, cooking style, cooking oils, cooking temperature, type of pots and pans, and so on (Abdullahi et al., 2013; Torkmahalleh et al., 2017). Thus, restaurant corporate chain brands should develop a course of cooking processes to minimize PM emissions under their purview. The safety and health of kitchen personnel are secured, as are those of customers in the dining room of open-kitchen restaurants.
Third, open-kitchen restaurant brands should consider implementing new mechanical dining room ventilation systems similar to kitchen hood ventilation. Although costly, such expenses are increasingly necessary in the age of COVID-19. Medical experts and scientists continue to emphasize the importance of ventilation in enclosed spaces, such as restaurants and bars, where crowds are known to gather (CDC, 2020). Epidemiologists have stated that aerosol transmission of the virus can be mitigated by proper ventilation (Morawska et al., 2020). Therefore, a ventilation system that draws in treated outdoor air and filters indoor contaminants should join the list of necessary safety measures along with surface disinfecting, handwashing, masking, and social distancing. Because restaurants are a difficult place to use masks, proper ventilation is key to reducing indoor air pollutants and the spread of the novel coronavirus indoors. Adding a number of portable air purifiers with high-efficiency particulate air filters is one viable, if temporary, solution. As evidence by Zhao et al. (2020), air purifiers may be an effective supplementary measure for indoor transmission of viruses, including COVID-19.
Reflecting the abovementioned recommendations would require restaurant brands to make a capital investment and corporate commitment against COVID-19. To obtain fair return on said investment, restaurant brands should help customers recognize the intrinsic value created. As a result, safe and healthy dining experiences can be offered by brands in the fight against the pandemic and for the post-COVID period to come. PwC’s (2020) most recent market report highlighted that customers after COVID-19 will seek evidence of safety protocols as they adjust to so-called new normal. Based on mounting evidence, we suggest that open-kitchen brands consider air quality surveillance systems with smart technology that integrate HVAC with the newly enhanced ventilation systems. This will help customers perceive scientifically proven safety protocols while motivating their willingness to pay for the service being offered. For example, a smart display that informs customers and employees of a restaurant’s real-time indoor air quality can be placed in a visible location in the dining space. The display can serve as a visual cue that shows indoor air quality and educates customers and employees how the ventilation system is reacting (or not reacting) in response to poor air quality. Further, a system that allows potential customers to check out indoor air quality while making a reservation on the restaurant’s website will be to the restaurant’s advantage. Such measures can give customers an impression of what open-kitchen restaurants and their transparency should be in the age of COVID-19. After all, the smart system would show tangible proof of how much care restaurant brands put into invisible cleanliness to protect the health and well-being of customers and employees in open-kitchen restaurants. It would also surely restore confidence in in-room dining and build brand trust in the long run.
6. Limitations and future research
Although the offensively high indoor PM levels monitored in the study were obtained by placing the equipment in the center of the restaurant on a counter to match the height of seated customers’ breathing zone, there might be variations in indoor PM levels according to the specific spot where it is measured due to the distance from the kitchen and the air currents made by the air conditioning system blowing indoor PM in a certain direction. This led us to expect that the observed PM levels in the center of the restaurant might be different from other spots only a few feet away. Therefore, future studies should address this aspect and monitor PM levels in multiple spots of the dining room. Among an average of 52 weeks in a year, the results of this study were obtained only from a week in a single open-kitchen facility. Although the week would represent a typical week without any holiday, cautions should be applied when interpreting the results. Also generalization of the results on other open-kitchen restaurants might not be feasible since previous research indicated that PM emissions from commercial cooking might vary due to a variety of factors including type of food, oil, energy source, and so on (Torkmahalleh et al., 2017). Thus, examining indoor PM levels of another open-kitchen restaurant of a bigger scale in terms of national presence is suggested for part of future studies. Obtaining a corporate approval for data usage of its sales and menu items ordered by the hour would be able to further investigate the relationship between those pieces information with indoor PM pollution. Lastly, in order to increase awareness and convince restaurant/food service entrepreneurs and local policymakers regarding hazardous PM pollution in full service open-kitchen restaurants, future studies should be oriented toward the time series and chemical monitoring in source apportionment studies. This way, convincing and realistic attributions of sources of indoor PM will be obtained.
Acknowledgements
The authors would like to express our sincere gratitude to Lighthouse Worldwide Solutions, in particular to Mr. Mark VonHolle, Marketing Manager, and to Mr. Peter Maguire, Vice President for their continuous support on our research with their air quality equipment, “Handheld 3016 IAQ Particle Counter.”
References
- Abdullahi K.L., Delgado-Saborit J.M., Harrison R.M. Emissions and indoor concentrations of particulate matter and its specific chemical components from cooking: a review. Atmos. Environ. 2013;71:260–294. [Google Scholar]
- Afshari R. Indoor air quality and severity of COVID-19: where communicable and non-communicable preventive measures meet. Asia Pac. J. Med. Toxicol. 2020;9:1–2. [Google Scholar]
- Afshari A., Matson U., Ekberg L.E. Characterization of indoor sources of fine and ultrafine particles: a study conducted in a full-scale chamber. Indoor Air. 2005;15:141–150. doi: 10.1111/j.1600-0668.2005.00332.x. [DOI] [PubMed] [Google Scholar]
- Buell R.W., Kim T., Tsay C.-J. Cooks make tastier food when they can see their customers. Harv. Bus. Rev. 2014;92:34–35. [Google Scholar]
- Buonanno G., Morawska L., Stabile L. Particle emission factors during cooking activities. Atmos. Environ. 2009;43:3235–3242. [Google Scholar]
- Buonanno G., Stabile L., Morawska L. Personal exposure to ultrafine particles: the influence of time-activity patterns. Sci. Total Environ. 2014;468-469:903–907. doi: 10.1016/j.scitotenv.2013.09.016. [DOI] [PubMed] [Google Scholar]
- Byun J., Jang S. Open kitchen vs closed kitchen. Int. J. Contemp. Hosp. Manage. 2018;30:2214–2229. [Google Scholar]
- Cadelis G., Tourres R., Molinie J. Short-term effects of the particulate pollutants contained in Saharan dust on the visits of children to the emergency department due to asthmatic conditions in Guadeloupe (French Archipelago of the Caribbean) PLoS One. 2014;9 doi: 10.1371/journal.pone.0091136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC . 2020. COVID-19: Considerations for Restaurants and Bars.https://www.cdc.gov/coronavirus/2019-ncov/community/organizations/business-employers/bars-restaurants.html Available from. [Google Scholar]
- Chang H., Huh C., Legendre T.S., Simpson J.J. Exploring particulate matter pollution in hotel guestrooms. Int. J. Contemp. Hosp. Manage. 2020;32:1131–1162. [Google Scholar]
- Chow A.J., Alonso A.D., Douglas A.C., O’Neill M.A. Exploring open kitchens’ impact on restaurateurs’ cleanliness perceptions. J. Retail Leisure Prop. 2010;9:93–104. [Google Scholar]
- CNN . 2020. Patrons are Asked to Self-Quarantine after About 85 People Who Visited a Michigan Bar Get Covid-19.https://www.cnn.com/2020/06/27/us/michigan-coronavirus-bar-harpers/index.html Available from. [Google Scholar]
- EPA . 1989. Report to Congress on Indoor Air Quality.https://www.epa.gov/report-environment/indoor-air-quality Available from. [Google Scholar]
- EPA . 2006. Particulate Matter Basics.https://www.epa.gov/pm-pollution/particulate-matter-pm-basics#PM Available from. [Google Scholar]
- EPA . 2018. Particulate Matter (PM) Pollution.https://www.epa.gov/pm-pollution Available from. [Google Scholar]
- Fisher, Tenforde, Feldstein Community and close contact exposures associated with COVID-19 among symptomatic adults ≥18 years in 11 outpatient health care facilities — united States, July 2020. Morb. Mortal. Wkly. Rep. 2020;2020:1258–1264. doi: 10.15585/mmwr.mm6936a5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes . 2015. Consumer Trends in Health and Wellness.https://www.forbes.com/sites/thehartmangroup/2015/11/19/consumer-trends-in-health-and-wellness/#7acbbde9313e Available from. [Google Scholar]
- Gysel N., Welch W.A., Chen C.-L., Dixit P., Cocker D.R., Karavalakis G. Particulate matter emissions and gaseous air toxic pollutants from commercial meat cooking operations. J. Environ. Sci. 2018;65:162–170. doi: 10.1016/j.jes.2017.03.022. [DOI] [PubMed] [Google Scholar]
- Huang J., Liu Q., Guo X. In: Encyclopedia of Environmental Health. second edition. Nriagu J., editor. Elsevier; Oxford: 2019. Short-term effects of particulate air pollution on human health; pp. 655–662. [Google Scholar]
- Ko Y.-C., Cheng L.S.-C., Lee C.-H., Huang J.-J., Huang M.-S., Kao E.-L., Wang H.-Z., Lin H.-J. Chinese food cooking and lung cancer in women nonsmokers. Am. J. Epidemiol. 2000;151:140–147. doi: 10.1093/oxfordjournals.aje.a010181. [DOI] [PubMed] [Google Scholar]
- Lee S.C., Li W.-M., Yin Chan L. Indoor air quality at restaurants with different styles of cooking in metropolitan Hong Kong. Sci. Total Environ. 2001;279:181–193. doi: 10.1016/s0048-9697(01)00765-3. [DOI] [PubMed] [Google Scholar]
- Lee B.K., Jeong U.R., Dong T.T.T. Concentration comparison of the indoor air pollutants identified from the restaurants with the different cooking and ventilation methods. The 6th International Conference on Indoor Air Quality, Ventilation & Energy Conservation in Buildings; IAQVEC, Sendai, Japan; 2007. [Google Scholar]
- Li Y.-C., Shu M., Ho S.S.H., Wang C., Cao J.-J., Wang G.-H., Wang X.-X., Wang K., Zhao X.-Q. Characteristics of PM2.5 emitted from different cooking activities in China. Atmospheric Res. 2015;166:83–91. [Google Scholar]
- Li Y., Qian H., Hang J., Chen X., Hong L., Liang P., Li J., Xiao S., Wei J., Liu L., Kang M. 2020. Evidence For Probable Aerosol Transmission Of Sars-Cov-2 In A Poorly Ventilated Restaurant. medRxiv, 2020.2004.2016.20067728. [Google Scholar]
- Liang D., Shi L., Zhao J., Liu P., Sarnat J.A., Gao S., Schwartz J., Liu Y., Ebelt S.T., Scovronick N., Chang H.H. Urban air pollution may enhance COVID-19 case-fatality and mortality rates in the United States. Innovation (N Y) 2020 doi: 10.1016/j.xinn.2020.100047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin P.C., Peng C.Y., Pan C.H., Lin P.D., Wu M.T. Gender differences and lung cancer risk in occupational chefs: analyzing more than 350,000 chefs in Taiwan, 1984-2011. Int. Arch. Occup. Environ. Health. 2019;92:101–109. doi: 10.1007/s00420-018-1358-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long Suh, Koutrakis Characterization of indoor particle sources using continuous mass and size monitors. J. Air. Waste Manag. Assoc. 2000;50:1236–1250. doi: 10.1080/10473289.2000.10464154. [DOI] [PubMed] [Google Scholar]
- Lu J., Gu J., Li K., Xu C., Su W., Lai Z., Zhou D., Yu C., Xu B., Yang Z. COVID-19 outbreak associated with air conditioning in restaurant, Guangzhou, China, 2020. Emerg. Infect. Dis. 2020:26. doi: 10.3201/eid2607.200764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MLive . 2020. From Hair Salons to Gyms, Experts Rank 36 Activities by Coronavirus Risk Level.https://www.mlive.com/public-interest/2020/06/from-hair-salons-to-gyms-experts-rank-36-activities-by-coronavirus-risk-level.html Available from. [Google Scholar]
- Morawska L., Tang J.W., Bahnfleth W., Bluyssen P.M., Boerstra A., Buonanno G., Cao J., Dancer S., Floto A., Franchimon F., Haworth C., Hogeling J., Isaxon C., Jimenez J.L., Kurnitski J., Li Y., Loomans M., Marks G., Marr L.C., Mazzarella L., Melikov A.K., Miller S., Milton D.K., Nazaroff W., Nielsen P.V., Noakes C., Peccia J., Querol X., Sekhar C., Seppänen O., Tanabe S.-I., Tellier R., Tham K.W., Wargocki P., Wierzbicka A., Yao M. How can airborne transmission of COVID-19 indoors be minimised? Environ. Inter. 2020;142 doi: 10.1016/j.envint.2020.105832. 105832-105832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Restaurant Association . 2017. Healthy Foods Drive Dining Choices.https://restaurant.org/Articles/News/Batch2_201901/State-of-the-Industry-Healthy-foods-drive-dining-c Available from. [Google Scholar]
- Neghab M., Delikhoon M., Norouzian Baghani A., Hassanzadeh J. Exposure to cooking fumes and acute reversible decrement in lung functional capacity. Int. J. Occup. Environ. Med. 2017;8:207–216. doi: 10.15171/ijoem.2017.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NYTimes . 2020. Nation Wanted to Eat Out Again Everyone Has Paid the Price.https://www.nytimes.com/2020/08/12/health/Covid-restaurants-bars.html Available from. [Google Scholar]
- Ott W.R., Wallace L.A., McAteer J.M., Hildemann L.M. Fine and ultrafine particle exposures on 73 trips by car to 65 non-smoking restaurants in the San Francisco Bay Area. Indoor Air. 2017;27:205–217. doi: 10.1111/ina.12292. [DOI] [PubMed] [Google Scholar]
- Petroni M., Hill D., Younes L., Barkman L., Howard S., Howell I.B., Mirowsky J., Collins M.B. Hazardous air pollutant exposure as a contributing factor to COVID-19 mortality in the United States. Environ. Res. Lett. 2020;15 0940a0949. [Google Scholar]
- PwC . 2020. How to Restore Confidence in Travel during an Uncertain Time.https://www.pwc.com/us/en/industries/consumer-markets/library/how-to-restore-confidence-in-travel-during-covid-19.html Available from. [Google Scholar]
- Qian H., Miao T., LIU L., Zheng X., Luo D., Li Y. 2020. Indoor Transmission of SARS-CoV-2. medRxiv, 2020.004.2004.20053058. [DOI] [PubMed] [Google Scholar]
- Qin N., Liang P., Wu C., Wang G., Xu Q., Xiong X., Wang T., Zolfo M., Segata N., Qin H., Knight R., Gilbert J.A., Zhu T.F. Longitudinal survey of microbiome associated with particulate matter in a megacity. Genome Biol. 2020;21:55. doi: 10.1186/s13059-020-01964-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramos C.A., Wolterbeek H.T., Almeida S.M. Exposure to indoor air pollutants during physical activity in fitness centers. Buil. Environ. 2014;82:349–360. [Google Scholar]
- Reuters . 2020. Fauci: Data ‘good enough’ on Aerosol Spread.https://news.yahoo.com/fauci-data-good-enough-aerosol-215108384.html Available from. [Google Scholar]
- Saha J., Chouhan P. Indoor air pollution (IAP) and pre-existing morbidities among under-5 children in India: are risk factors of coronavirus disease (COVID-19)? Environ. Pollut. 2020;266 doi: 10.1016/j.envpol.2020.115250. 115250-115250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- See S.W., Balasubramanian R. Risk assessment of exposure to indoor aerosols associated with Chinese cooking. Environ. Res. 2006;102:197–204. doi: 10.1016/j.envres.2005.12.013. [DOI] [PubMed] [Google Scholar]
- Setti L., Passarini F., De Gennaro G., Barbieri P., Perrone M.G., Palmisani J., Di Gilio A., Piscitelli P. Is there a plausible role for particulate matter in the spreading of COVID-19 in Northern Italy? BMJ Rapid Resp. 2020:8. doi: 10.1136/bmjopen-2020-039338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sjaastad A.K., Jørgensen R.B., Svendsen K. Exposure to polycyclic aromatic hydrocarbons (PAHs), mutagenic aldehydes and particulate matter during pan frying of beefsteak. Occup. Environ. Med. 2010;67:228–232. doi: 10.1136/oem.2009.046144. [DOI] [PubMed] [Google Scholar]
- Sohn E.-M., Lee K.-W. The effect of chefs’ nonverbal communication in open kitchens on service quality. J. Foodserv. Bus. Res. 2018;21:483–492. [Google Scholar]
- Soppa V.J., Schins R.P.F., Hennig F., Hellack B., Quass U., Kaminski H., Kuhlbusch T.A.J., Hoffmann B., Weinmayr G. Respiratory effects of fine and ultrafine particles from indoor sources--a randomized sham-controlled exposure study of healthy volunteers. Int. J. Environ. Res. Public Health. 2014;11:6871–6889. doi: 10.3390/ijerph110706871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straif K., Baan R., Grosse Y., Secretan B., El Ghissassi F., Cogliano V. Carcinogenicity of household solid fuel combustion and of high-temperature frying. Lancet Oncol. 2006;7:977–978. doi: 10.1016/s1470-2045(06)70969-x. [DOI] [PubMed] [Google Scholar]
- Svedahl S., Svendsen K., Qvenild T., Sjaastad A.K., Hilt B. Short term exposure to cooking fumes and pulmonary function. J. Occup. Med. Toxicol. 2009;4:9. doi: 10.1186/1745-6673-4-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taner S., Pekey B., Pekey H. Fine particulate matter in the indoor air of barbeque restaurants: elemental compositions, sources and health risks. Sci. Total Environ. 2013;454-455:79–87. doi: 10.1016/j.scitotenv.2013.03.018. [DOI] [PubMed] [Google Scholar]
- Tara . 2018. Countries with the Highest and Lowest Levels of Air Pollution.https://biofriendlyplanet.com/eco-awareness/air-quality/air-pollution/countries-least-polluted-urban-areas/ Available from. [Google Scholar]
- Time . 2012. Nothing to Hide: Why Restaurants Embrace the Open Kitchen.http://business.time.com/2012/08/20/nothing-to-hide-why-restaurants-embrace-the-open-kitchen/ Available from. [Google Scholar]
- Torkmahalleh M.A., Goldasteh I., Zhao Y., Udochu N.M., Rossner A., Hopke P.K., Ferro A.R. PM2.5 and ultrafine particles emitted during heating of commercial cooking oils. Indoor Air. 2012;22:483–491. doi: 10.1111/j.1600-0668.2012.00783.x. [DOI] [PubMed] [Google Scholar]
- Torkmahalleh M.A., Gorjinezhad S., Unluevcek H.S., Hopke P.K. Review of factors impacting emission/concentration of cooking generated particulate matter. Sci. Total Environ. 2017;586:1046–1056. doi: 10.1016/j.scitotenv.2017.02.088. [DOI] [PubMed] [Google Scholar]
- USA Today . 2019. India, Pakistan, China and Africa Have 30 of the Most Polluted Places on Earth.https://www.usatoday.com/story/money/2019/12/10/china-india-pakistan-africa-30-most-polluted-places-on-earth/40744635/ Available from. [Google Scholar]
- Valavanidis A., Fiotakis K., Vlachogianni T. Airborne particulate matter and human health: toxicological assessment and importance of size and composition of particles for oxidative damage and carcinogenic mechanisms. J. Environ. Sci. Health C Environ. Carcinog. Ecotoxicol. Rev. 2008;26:339–362. doi: 10.1080/10590500802494538. [DOI] [PubMed] [Google Scholar]
- Wallace L., Ott W. Personal exposure to ultrafine particles. J. Exposure Sci. Environ. Epidemiol. 2011;21:20–30. doi: 10.1038/jes.2009.59. [DOI] [PubMed] [Google Scholar]
- WHO . 2013. Outdoor Air Pollution a Leading Environmental Cause of Cancer Deaths.http://www.euro.who.int/en/health-topics/environment-and-health/air-quality/news/news/2013/10/outdoor-air-pollution-a-leading-environmental-cause-of-cancer-deaths Available from. [Google Scholar]
- WHO . 2016. Ambient (outdoor) Air Quality and Health.http://www.who.int/mediacentre/factsheets/fs313/en/ Available from. [Google Scholar]
- Wilson N., Parry R., Jalali J., Jalali R., McLean L., McKay O. High air pollution levels in some takeaway food outlets and barbecue restaurants. Pilot study in Wellington City, New Zealand. N. Z. Med. J. 2011;124:81–86. [PubMed] [Google Scholar]
- Wu X., Braun D., Schwartz J., Kioumourtzoglou M.A., Dominici F. Evaluating the impact of long-term exposure to fine particulate matter on mortality among the elderly. Sci. Adv. 2020;6 doi: 10.1126/sciadv.aba5692. eaba5692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y., Richardson B., Takle E., Chai L., Schmitt D., Xin H. Airborne transmission may have played a role in the spread of 2015 highly pathogenic avian influenza outbreaks in the United States. Sci. Rep. 2019;9:11755. doi: 10.1038/s41598-019-47788-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., Xie J., Huang F., Cao L. Association between short-term exposure to air pollution and COVID-19 infection: evidence from China. Sci. Total Environ. 2020;727 doi: 10.1016/j.scitotenv.2020.138704. [DOI] [PMC free article] [PubMed] [Google Scholar]