Abstract
Objectives
To test the hypothesis that intraoperative cone beam computed tomography (CBCT) using the Allura augmented reality surgical navigation (ARSN) system in a dedicated hybrid operating room (OR) matches computed tomography (CT) for identification of pedicle screw breach during spine surgery.
Methods
Twenty patients treated with spinal fixation surgery (260 screws) underwent intraoperative CBCT as well as conventional postoperative CT scans (median 12 months after surgery) to identify and grade the degree of pedicle screw breach on both scan types, according to the Gertzbein grading scale. Blinded assessments were performed by three independent spine surgeons and the CT served as the standard of reference. Screws graded as Gertzbein 0 or 1 were considered clinically accurate while grades 2 or 3 were considered inaccurate. Sensitivity, specificity, and negative predictive value were the primary metrics of diagnostic performance.
Results
For this patient group, the negative predictive value of an intraoperative CBCT to rule out pedicle screw breach was 99.6% (CI 97.75–99.99%). Among 10 screws graded as inaccurate on CT, 9 were graded as such on the CBCT, giving a sensitivity of 90.0% (CI 55.5–99.75%). Among the 250 screws graded as accurate on CT, 244 were graded as such on the CBCT, giving a specificity of 97.6% (CI 94.85–99.11%).
Conclusions
CBCT, performed intraoperatively with the Allura ARSN system, is comparable and non-inferior to a conventional postoperative CT scan for ruling out misplaced pedicle screws in spinal deformity cases, eliminating the need for a postoperative CT.
Key Points
• Intraoperative cone beam computed tomography (CT) using the Allura ARSN is comparable with conventional CT for ruling out pedicle screw breaches after spinal fixation surgery.
• Intraoperative cone beam computed tomography can be used to assess need for revisions of pedicle screws making routine postoperative CT scans unnecessary.
• Using cone beam computed tomography, the specificity was 97.6% and the sensitivity was 90% for detecting pedicle screw breaches and the negative predictive value for ruling out a pedicle screw breach was 99.6%.
Keywords: Cone beam computed tomography, Image-guided surgery, Pedicle screws, Sensitivity and specificity
Introduction
Pedicle screw placement, a crucial step in all posterior spinal fixation surgeries, carries an inherent risk due to the close anatomical relationship between the pedicles and important neurovascular structures [1, 2]. A recent meta-analysis demonstrated that 3.3% of free-hand (FH) spinal fixation surgeries led to a postoperative revision surgery to correct misplaced screws [3]. If these incorrect placements of screws could be prevented, patient morbidity would be reduced as well as costs amounting to $23,865–$32,915 per revision surgery [3, 4].
To increase pedicle screw accuracy and minimize the misplacement risk, technical aids such as fluoroscopy, computer-assisted navigation, surgical robots, and neurophysiological monitoring can be used [5–7]. Probing the pilot hole before placing the pedicle screw is commonly part of the surgical routine [8], but cannot reveal a breach occurring after pedicle screw insertion [9]. Irrespective of surgical method, however, the use of intraoperative radiology to evaluate final screw positions can help the surgeon to avoid complications related to screw misplacements and minimize the need for reoperation [10, 11].
Several techniques for detecting pedicle breaches have been described. When the procedures are performed using the FH technique, a mobile C-arm is typically used to acquire 2D fluoroscopic images to intraoperatively verify screw placement [12]. However, this type of imaging cannot create axial views and therefore mediolateral breaches can only be identified through an anteroposterior projection view. The sensitivity of 2D radiographic imaging to identify screws breaching mediolaterally in non-deformity cases is 74% [13] and decreases to 52% in deformity cases [14]. Other intraoperative imaging options include intraoperative CT [15] and intraoperative 3D fluoroscopy [16, 17], both of which have shown promising results in detecting misplaced pedicle screws, thereby potentially reducing the rate of revision surgery.
Cone beam computed tomography (CBCT) was initially developed for use in dentistry, interventional radiology, and orthopedics [18]. The cone beam geometry was developed as an alternative to conventional CT using either fan-beam or spiral-scan geometries, to enable fast data acquisition of the entire field of view (FOV). Imaging is performed by a rotating gantry incorporating an x-ray source and a detector. In contrast to conventional CT which uses a fan-shaped x-ray beam in a helical progression, a divergent pyramidal- or cone-shaped radiation source is directed towards the area of interest and onto an x-ray detector on the opposite side. Using a complete or partial arc, multiple (from 150 to more than 600) sequential planar projection images of the FOV are acquired during the rotation. Since CBCT exposure incorporates the entire FOV, one rotational sequence of the gantry is enough to acquire required data for image reconstruction. A shorter examination time results in increased image sharpness and reduced distortion caused by patient movement, and increased x-ray tube efficiency. A disadvantage, however, is a limitation in image quality related to noise and contrast resolution since large amounts of scattered radiation are detected [19, 20].
An augmented reality surgical navigation (ARSN) system for spine surgery has previously been evaluated in a prospective cohort study and it was demonstrated that it can be used for accurate pedicle screw placement [21, 22]. The ARSN system relies on an intraoperative CBCT (Allura Xper FD20, Philips Healthcare) for preoperative planning as well as postoperative confirmation of screw positions. In brief, a ceiling-mounted robotic C-arm with integrated video cameras within the flat x-ray detector frame is used for imaging and subsequent augmented reality navigation in a hybrid operating room. Multiple adhesive skin markers form the basis for a virtual reference grid to track the patient’s position. The system uses an inherent software providing automatic spine segmentation and pedicle identification, utilized for planning of pedicle screw trajectories and surgical navigation as well as intraoperative confirmation of results [23, 24]. In this study, we retrospectively compared the screw grading on intraoperative CBCT scans to postoperative CT scans of the same patients to evaluate whether the image quality of CBCT is adequate to rule out pedicle breach.
Methods
This retrospective study was performed as part of a prospective cohort study approved by the institutional review board (2018/1490-31 and 2015/1640-31/2). The prospective enrollment was performed consecutively and all patients eligible for deformity correction spine surgery over the age of 16 were included after signed informed consent was signed. Authors without conflicts of interest had full control of inclusion of data and information submitted for publication.
Patient characteristics
In total, 20 patients (260 pedicle screws; overall mean age 30.5 years; 11 women and 9 men) undergoing spinal fixation surgery including placement of pedicle screws using the augmented reality surgical navigation (ARSN) system were included [22]. There were 13 scoliosis (9 idiopathic, 2 neuromuscular, and 2 degenerative), 2 kyphosis (1 post fracture and 1 Scheuermann’s), 3 lumbar spondylolisthesis, 1 lumbar spinal stenosis, and 1 lumbar degenerative disk disease. The pre- and postoperative Cobb angles for the 15 deformity cases were 55 ± 16 and 23 ± 13°, respectively [22, 25, 26]. Of the 260 assessed screws, 166 (64%) were placed in the thoracic and 94 (36%) in the lumbosacral spine. The average pedicle width-to-screw size ratio for the whole cohort was 1.3 ± 0.7 and 1.1 ± 0.5 in the 15 deformity cases; The ratio was 1.4 ± 0.8, 1.0 ± 0.3, and 0.8 ± 0.2 for screws rated as grade 0, 1, and 2, respectively [22, 26].
Surgical technique
The detailed workflow of the surgical setup and system has been published previously [22, 24, 27]. All surgeries were performed in a hybrid operating room (OR) with intraoperative CBCT capability and adapted for spine surgery. In short, all patients were operated on in the prone position. After draping and exposure of the relevant levels, adhesive skin markers were used for patient position tracking. An initial CBCT was acquired, and a surgical plan adapted for the intended pedicle screws using the ARSN software [23]. For every pedicle, an awl followed by a gearshift or power drill was used to create a pilot hole, before placing the pedicle screw using a screwdriver. After placement of all pedicle screws, a confirmatory CBCT was performed to evaluate all screw positions. If needed, according to this CBCT, screws were revised [22].
CBCT imaging technique
The system consists in part of a ceiling-mounted robotic C-arm (Allura Xper FD20, Philips Healthcare) used for both the initial CBCT scan, for planning and navigation features, as well as the confirmatory CBCT scan at the end of the surgery. Fluoroscopy imaging in 2D with 3.75 x-ray pulses/second was used for spinal level identification and iso-centering of the region of interest prior to 3D CBCT imaging. There were three types of CBCT protocols available: small (12.6 × 12.6 cm2), medium (17.3 × 17.3 cm2), and large (25.2 × 19.5 cm2) detector FOV, as has previously been described [27]. The small FOV protocol used 482 x-ray pulses to generate the CBCT image (the other protocols used 302 pulses), providing an improved image quality at the expense of an increased patient radiation exposure. The three protocols typically include 4 to 7, 5 to 9, and 6 to 10 spinal levels, respectively. During the first 10 procedures, a total of 38 CBCT acquisitions were performed (19 small and 19 medium FOV). During the final 10 procedures, a total of 39 CBCT acquisitions were performed (1 small, 21 medium, and 17 large FOV) [24]. All three protocols had a fixed tube kilovoltage of 120 kV, and a tube current time product ranging from 50 to 325 mAs, modulated by an automatic dose rate control to achieve a similar image quality independent of the patient size. Beam spectral filtration of 0.4 mm copper (Cu) and 1 mm aluminum (Al) was used for all protocols, in addition to 3.5 mm Al inherent x-ray tube filtration yielding 2.4 to 3.1% noise levels based on the ACR 464 CT phantom [27, 28]. For image acquisition, the C-arm rotated 180° in 8–10 s, and in an additional 15 s, a 3D reconstructed volume with 0.5 mm voxel size was displayed at 1 mm thickness in axial and sagittal views with a contrast resolution of 3 to 5 HU [28, 29]. This procedure was performed under temporary apnea in clinical cases [22].
The median total procedure time was 379 min (232–548). The median preparation time from skin incision until before the CBCT acquisition was 107 min (68–174 min), accounting for 28% of the total procedure time. The CBCT acquisition time (for both planning and verification of screw placement) and segmentation of the spinal levels of interest for surgery corresponded to 2% of the total procedure time with a median time of 8 min (range 2–44 min). Total navigation time corresponded to almost 25% of the total procedure time [24]. For verification, the C-arm can be tilted ± 20°, to avoid collinearity between the x-ray beam and the direction of the screws, thus reducing metal artifacts in the 3D images.
For navigation planning and screw placement, a median of 2 [1–4] CBCT acquisitions was performed. An additional 2 [1–4] CBCT acquisitions were performed for verification, replacing postoperative CT. The average AK and DAP per procedure was 159 ± 16 mGy and 31.3 ± 2.8 Gy cm2, respectively. The average patient ED was 15.8 ± 1.8 mSv with CBCT contributing to 97 ± 1% of the total procedure ED. The average staff exposure per procedure was 0.21 ± 0.06 mSv [27].
Screw position assessment
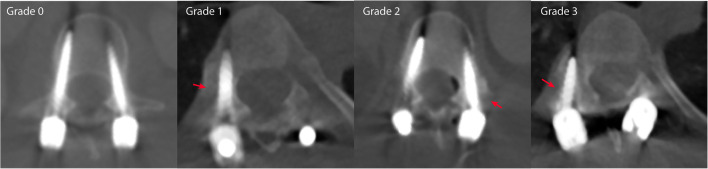
In addition to the intraoperative CBCT at the end of the surgery, the follow-up protocol included a conventional postoperative follow-up CT at median 12 months (0–21 months) after surgery, as detailed in Table 1. For this study, both the intraoperative CBCT and the postoperative CT were analyzed to determine the presence and degree of pedicle screw perforation outside of the pedicles. Blinded radiological assessments of pedicle screw positions were performed by three independent spine surgeons on both the CBCT and CT scans, and the CT scans served as the standard of reference. All screws were graded according to the Gertzbein grading scale on both the intraoperative CBCT and the postoperative conventional CT scans [30]. Examples of all Gertzbein gradings are seen in Fig. 1, grade 0 (screw within the pedicle without cortical breach), grade 1 (0–2 mm breach, minor perforation including cortical encroachment), grade 2 (> 2–4 mm breach, moderate breach), and grade 3 (> 4 mm breach, severe displacement). Screws graded as 0 or 1 according to the Gertzbein grading scale were considered clinically accurate while grades 2 or 3 were considered clinically inaccurate. Sensitivity, specificity, and negative predictive value were the primary metrics of diagnostic performance.
Table 1.
Specifications of CT scans used as gold standard
| CT scan specification | Median (IQR) |
|---|---|
| No. of rows | 128 (128–256) |
| Spiral pitch factor | 0.98 (0.8–1.38) |
| Peak tube voltage (kV) | 120 (100–120) |
| Tube current (mA) | 92 (54–187) |
| Slice thickness (mm) | 0.65 (0.63–0.75) |
| Single detector collimation (mm) | 0.60 (0.60–0.63) |
| Rotation speed (s) | 0.50 (0.50–0.50) |
| CTDIvol (mGy) | 6.60 (1.68–12.51) |
| Voxel size | 0.71 (0.63–0.75) |
CTDIvol volume computed tomography dose index, CT computed tomography, IQR interquartile range
Fig. 1.
Examples of screws graded as Gertzbein grades 0–3. Red arrows highlight the position of each breach
Statistical analysis
Analyses were performed using RStudio (RStudio Team (2016). RStudio: Integrated Development for R. RStudio, Inc.) and R version 3.6.1. Absolute interrater agreement was calculated without corrections, meaning the number of screws where all three raters agreed was divided by the total number of screws [31, 32]. Fleiss’ Kappa was used for calculating reliability of agreement between the 3 raters [33]. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of screw placement assessment based on intraoperative CBCT imaging were computed, using assessment of postoperative CT scans as the gold standard. Values of sensitivity, specificity, PPV, and NPV are presented with their 95% confidence intervals (CI: min%–max%). Confidence intervals for sensitivity, specificity, diagnostic accuracy, and positive and negative predictive values were calculated as described by Collet using R-library “epiR” [34]. ROC analysis was performed using R-library “ROCR” [35].
Results
In total, 260 pedicle screws were assessed on both intraoperative CBCT and postoperative CT (Table 2). Three screws were identified as severely misplaced on the CBCT and revised intraoperatively and could consequently not be assessed on CT and were excluded from the material. The absolute interrater agreement was 72.7% in the CT group and 63.1% in the CBCT group while Fleiss’ Kappa was 0.48 in the CT group and 0.63 in the CBCT group. Among the 10 (3.8%) screws graded as inaccurate on CT, 9 were graded as such on the CBCT, giving a sensitivity of 90.0% (CI 55.5–99.75%). The single case of false negative screw rating had a Gertzbein grading of 1 according to the CBCT and 2 according to the CT, indicating a borderline case. Among the 250 screws graded as accurate on CT, 244 were graded as such on the CBCT, giving a specificity of 97.6% (CI 94.85–99.11%). In all cases where a screw was rated as incorrect on CBCT but correct on CT, the Gertzbein grading was 2 on CBCT and 1 on CT, indicating borderline cases. Table 3 summarizes the test results and Fig. 2 shows the ROC curve for sensitivity and specificity for detecting inaccurate screws (i.e., Gertzbein grades 2–3).
Table 2.
Comparison between screw assessment on intraoperative CBCT scans and postoperative CT scans according to the Gertzbein grading scale
| Postoperative CT assessment | ||||||
|---|---|---|---|---|---|---|
| Grade | 0 | 1 | 2 | 3 | Total | |
| Intraoperative CBCT assessment | 0 | 149 | 10 | 0 | 0 | 159 |
| 1 | 32 | 53 | 1 | 0 | 86 | |
| 2 | 0 | 6 | 8 | 1 | 15 | |
| 3 | 0 | 0 | 0 | 0 | 0 | |
| Total | 181 | 69 | 9 | 1 | 260 | |
CBCT cone beam computed tomography
Note: Italicized numbers indicate number of agreements between CT and CBCT assessment
Table 3.
Summary of test statistics for intraoperative CBCT assessment of screws
| Parameter | Value | CI (95%) |
|---|---|---|
| Sensitivity | 90% (9/10) | 55–100% |
| Specificity | 98% (244/250) | 95–99% |
| Diagnostic accuracy | 97% (253/260) | 95–99% |
| PPV | 60% (9/15) | 32–84% |
| NPV | 100% (244/245) | 98–100% |
CI confidence interval, NPV negative predictive value, PPV positive predictive value
Fig. 2.
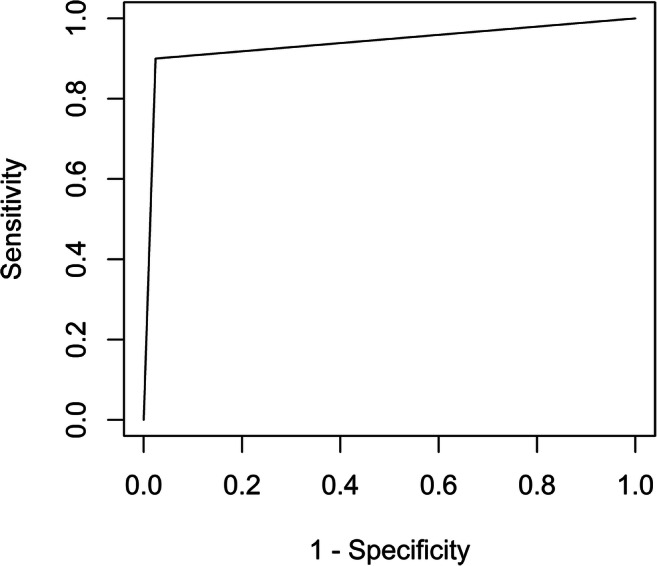
ROC curve for Gertzbein gradings on intraoperative CBCT with postoperative CT as gold standard
The NPV was 99.6% (CI 97.75–99.99%), indicating a high predictive confidence for ruling out pedicle screw breaches in this patient population and setting. The PPV was 60% (CI 32.29–83.66%) indicating a medium predictive confidence for finding pedicle screw breaches. The detailed gradings of all cases where the two methods disagreed are seen in Table 4.
Table 4.
Screw gradings per reader and modality of cases where CBCT and CT differed in their final screw rating (i.e., correct/incorrect screw rating)
| Reader 1—CBCT | Reader 2—CBCT | Reader 3—CBCT | Reader 1—CT | Reader 2—CT | Reader 3—CT | Pedicle | Follow-up time, CT (months) | Breach direction | Pedicle:screw width ratio | |
|---|---|---|---|---|---|---|---|---|---|---|
| Case: False negative | 2 | 1 | 1 | 1 | 2 | 2 | T9 left | 12 | Lateral | 1.25 |
| Case: False positive #1 | 2 | 2 | 2 | 1 | 1 | 1 | T7 left | 12 | Lateral | 0.67 |
| Case: False positive #2 | 1 | 2 | 2 | 1 | 2 | 1 | T7 left | 0 | Lateral | 0.78 |
| Case: False positive #3 | 2 | 2 | 2 | 1 | 1 | 1 | T11 left | 7 | Medial | 1.44 |
| Case: False positive #4 | 2 | 2 | 2 | 0 | 1 | 1 | T10 left | 8 | Lateral | 1.20 |
| Case: False positive #5 | 2 | 2 | 2 | 1 | 1 | 1 | T9 right | 9 | Lateral | 0.89 |
| Case: False positive #6 | 2 | 1 | 2 | 1 | 1 | 1 | T10 right | 9 | Lateral | 0.84 |
CBCT cone beam computed tomography, CT computed tomography
Discussion
Traditionally, fluoroscopy has been the method of choice for image guidance when placing pedicle screws using the free-hand technique. Most modern surgical navigation technologies, however, use a 3D imaging modality for intraoperative guidance [11]. While surgical navigation enables the surgeon to place screws safely and with higher accuracy than the conventional free-hand method [6], anatomical variations, bone quality, and pedicle geometry may affect the placement and result in a number of pedicle screws needing revision. Detecting these screws intraoperatively would allow immediate repositioning to minimize misplacement-related injuries and reduce revision surgery rates.
Compared with fluoroscopy, the patient radiation dose may increase with a 3D CBCT acquisition. However, this dose is on average less than that from a single-spine CT examination [36]. On the other hand, intraoperative 3D CBCT imaging may potentially prevent repeat surgeries and reduce the amount of follow-up imaging needed, thereby reducing the cumulative patient radiation exposure. This is particularly important in young adult scoliosis patients who are more radio-sensitive than older patient groups and have a higher overall long-term cancer mortality [37, 38]. CBCT scanners are a heterogenous group differing in patient radiation dose and image quality. The hybrid OR-based system used in this study exceeds the performance of common mobile systems regarding Hounsfield unit accuracy, noise, and uniformity due to added x-ray filtration and automatic exposure control [28]. Replacing the postoperative CT scan by a good-quality intraoperative CBCT may therefore have multiple benefits.
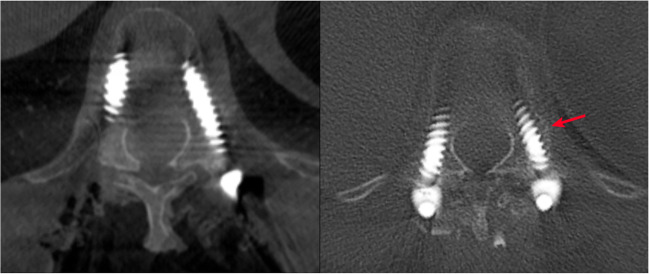
Thus, correct intraoperative assessment of pedicle screw placement is of great importance. In this study, we have shown that the use of intraoperative CBCT to assess pedicle breach in a consecutively enrolled cohort of deformity cases has a NPV of 99.6%. This means that if the CBCT does not indicate that a breach has occurred, the surgeon can be highly confident that this is in fact true. The PPV of 60% indicates that even though a screw looks misplaced on CBCT, this might not be the case on a postoperative CT. In fact, only 3 screws in our series were intraoperatively revised [22]. When looking at the cases where CT showed a lower Gertzbein grading than the CBCT, we could conclude that part of the difference may be explained by bone remodeling and bone growth around the pedicle screw between the time of intraoperative CBCT and follow-up CT, as demonstrated in Fig. 3.
Fig. 3.
Comparison between CBCT (left) and CT images (right) depicting suspected bone overgrowth between the two images were taken. Red arrow highlights suspected bone overgrowth
Our results are in accordance with results obtained by Cordemans et al, comparing CBCT (Artis Zeego II) to conventional CT scans performed on average 3 months after surgery due to different clinical requirements [39]. Grading was performed by the two operating surgeons separately and in a joint session to reach consensus. This approach may bias the final grading, and hence, we did not attempt to reach consensus between our independent raters. Only 2% of their cases were scoliotic, compared with our 65%. Dysplastic pedicles, as seen in spinal deformities, may be more difficult to assess radiologically, especially if screw diameters are large compared with pedicle width. In our case with a pedicle-to-screw diameter ratio of 1.1 ± 0.5, distinguishing between grades 1 and 2 was often a delicate matter. In a similar study Nevzati et al, using Allura FD20 without ARSN, demonstrated that the sensitivity and specificity for breach detection was higher for severe displacement compared with perfectly placed screws [10]. A summary of similar comparative studies is presented in Table 5.
Table 5.
Overview of studies and their test statistics for intraoperative screw position assessment
| Study | Year | No. of screws | Device | Compared to | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|---|---|---|---|
| Rao [40] | 2002 | 155 | CT | Open dissection | 86 | 85 | 95 | 62 |
| Santos [17] | 2012 | 416 | O-arm | Open dissection | 76 | 71 | 74 | 72 |
| Garber [16] | 2012 | 73 | O-arm | CT | 85 | 97 | 82 | 98 |
| Nevzati [10] | 2017 | 241 | Allura FD20 | CT | 71–92 | 77–99 | ||
| Cordemans [39] | 2017 | 348 | Artis Zeego II | CT | 77 | 98 | 86 | 96 |
| Current study | 2019 | 260 | Allura ARSN | CT | 90 | 98 | 60 | 100 |
ARSN augmented reality surgical navigation, CBCT cone beam computed tomography, CT computed tomography, NPV negative predictive value, PPV positive predictive value
Compared with previous studies, we have a higher sensitivity, specificity, and NPV while the PPV is lower in our study. This could in part be explained by a lower proportion of inaccurate pedicle screws in our material, reflected in the high NPV but low PPV. In part, this is explained by intraoperative revision of obviously misplaced screws identified by CBCT, removing them from the statistical analysis. In total, 3 screws were revised intraoperatively. Assuming that they could also be correctly identified on postoperative CT would increase the PPV to 0.67. In any case, this study was performed on an unbiased patient material consisting of consecutively enrolled patients at our institution; the NPV and PPV reflect the clinical reality of using the system for the intended patient group. Our test statistics would therefore be expected to be valid for spine deformity cases at similar tertiary care institutions.
A hybrid OR can improve facility utilization by covering many procedures—from endovascular to minimally invasive or open surgery—and enable exploration of new procedures that leverage intraoperative high-quality imaging and high level of device integration [41]. The results of this study indicate that the intraoperative CBCT imaging generated in a hybrid OR is of sufficient quality, comparable with that of conventional CT, to reliably identify pedicle screw misplacements. Extending these findings to other uses in the hybrid OR, we suggest that intraoperative CBCT may replace the postoperative CT in many spine and interventional procedures requiring accurate 3D imaging.
Limitations of this study
One of the main limitations of this study is the use of conventional CT as the gold standard. We justified this approach with CT being the currently used standard for evaluating pedicle screw placement [40]. However, the image quality of CT scans and CBCT scans varies depending on manufacturer and used dose protocol, indicating that some CBCT protocols might provide better image quality than CT and vice versa. Consequently, we used CT scans performed as part of the normal clinical routine to reflect the clinical reality. A drawback with this approach is that the image quality of the postoperative CT scans was variable, in part due to several different low-dose protocols applied in the routine care, as detailed in Table 1. In some cases, we subjectively found the image quality to be better in the Allura CBCT scans than the conventional CT scans. Data on radiation exposure for staff and patient using the ARSN system has been previously reported [27].
The CT scans included in this study were performed when clinically advised and therefore varied in time after surgery with a median follow-up of 12 months (0–21 months) postoperatively. It could be argued that scans obtained a long time after the operation would not necessarily be identical to the intraoperative imaging due to bone remodeling including both bone resorption and new bone formation around the pedicle screws. If anything, this would work to attenuate the findings of this study and not exaggerate them. One example of this was where we suspected bone formation around pedicle screws that were judged as false positives in our study, as highlighted in Fig. 3, since CBCT indicated breach but CT did not.
Another limitation could be that the intraoperative CBCT was obtained after pedicle screw placement but prior to rod placement and deformity correction. In that way, breaches resulting from pressure applied on pedicle screws due to rod placement and correction forces might be missed. However, we could not identify any clinically relevant effect of this possible phenomenon in our material.
Conclusion
Intraoperative CBCT, performed in a hybrid OR equipped with the Allura ARSN system, is reliable for ruling out pedicle screw breaches and can be used for intraoperative breach detection and revision, making routine postoperative CT scans unnecessary.
Abbreviations
- ARSN
Augmented reality surgical navigation
- CBCT
Cone beam computed tomography
- CI
Confidence interval
- CT
Computed tomography
- FH
Free hand
- FOV
Field of view
- NPV
Negative predictive value
- OR
Operating room
- PPV
Positive predictive value
Funding
Open access funding provided by Karolinska Institute. The authors state that this work has not received any direct funding but that one of the authors is an employee of Philips Healthcare, which has a vested interest in the product in this manuscript. The research has been conducted as part of a major collaboration agreement between Karolinska University Hospital and Philips Healthcare. For the remaining authors, no funding was declared beyond the major collaboration agreement of their employer.
Compliance with ethical standards
Guarantor
The scientific guarantor of this publication is Adrian Elmi Terander, MD, PhD, Karolinska University Hospital (Adrian.elmi-terander@sll.se).
Conflict of interest
R.N. is employed by Philips Healthcare, which has a vested interest in the product in this manuscript. The research has been conducted as part of a major collaboration agreement between Karolinska University Hospital and Philips Healthcare. For the remaining authors, no conflicts of interest were declared beyond the major collaboration agreement of their employer.
Statistics and biometry
One of the authors has significant statistical expertise (G.B.).
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained (Stockholm: 2018/1490-31 and 2015/1640-31/2).
Study subjects or cohorts overlap
Study subjects or cohorts have been previously reported but not related to this subject, in:
Elmi Terander A, Burström G, Nachabe R et al (2019) Pedicle Screw Placement Using Augmented Reality Surgical Navigation with Intraoperative 3D Imaging: A First In-Human Prospective Cohort Study. Spine (Phila Pa 1976) 44:517–525.
Methodology
• Retrospective analysis of prospectively enrolled cohort
• diagnostic or prognostic study
• performed at one institution
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gautschi OP, Schatlo B, Schaller K, Tessitore E. Clinically relevant complications related to pedicle screw placement in thoracolumbar surgery and their management: a literature review of 35,630 pedicle screws. Neurosurg Focus. 2011;31:E8. doi: 10.3171/2011.7.FOCUS11168. [DOI] [PubMed] [Google Scholar]
- 2.Inamasu J, Guiot BH (2006) Vascular injury and complication in neurosurgical spine surgery. Acta Neurochir (Wien) 148:375–387 [DOI] [PubMed]
- 3.Staartjes VE, Klukowska AM, Schroder ML. Pedicle screw revision in robot-guided, navigated, and freehand thoracolumbar instrumentation: a systematic review and meta-analysis. World Neurosurg. 2018;116:433–443 e438. doi: 10.1016/j.wneu.2018.05.159. [DOI] [PubMed] [Google Scholar]
- 4.Adogwa O, Parker SL, Shau D, et al. Cost per quality-adjusted life year gained of revision fusion for lumbar pseudoarthrosis: defining the value of surgery. J Spinal Disord Tech. 2015;28:101–105. doi: 10.1097/BSD.0b013e318269cc4a. [DOI] [PubMed] [Google Scholar]
- 5.Amato V, Giannachi L, Irace C, Corona C. Accuracy of pedicle screw placement in the lumbosacral spine using conventional technique: computed tomography postoperative assessment in 102 consecutive patients. J Neurosurg Spine. 2010;12:306–313. doi: 10.3171/2009.9.SPINE09261. [DOI] [PubMed] [Google Scholar]
- 6.Du JP, Fan Y, Wu QN, Wang DH, Zhang J, Hao DJ. Accuracy of pedicle screw insertion among 3 image-guided navigation systems: systematic review and meta-analysis. World Neurosurg. 2018;109:24–30. doi: 10.1016/j.wneu.2017.07.154. [DOI] [PubMed] [Google Scholar]
- 7.Siller S, Raith C, Zausinger S, Tonn JC, Szelenyi A (2019) Indication and technical implementation of the intraoperative neurophysiological monitoring during spine surgeries-a transnational survey in the German-speaking countries. Acta Neurochir (Wien). 10.1007/s00701-019-03974-6 [DOI] [PubMed]
- 8.Lehman RA, Potter BK, Kuklo TR, et al. Probing for thoracic pedicle screw tract violation(s): is it valid? J Spinal Disord Tech. 2004;17:277–283. doi: 10.1097/01.bsd.0000095399.27687.c5. [DOI] [PubMed] [Google Scholar]
- 9.Troni W, Benech CA, Perez R, Tealdi S, Berardino M, Benech F. Focal hole versus screw stimulation to prevent false negative results in detecting pedicle breaches during spinal instrumentation. Clin Neurophysiol. 2019;130:573–581. doi: 10.1016/j.clinph.2018.11.029. [DOI] [PubMed] [Google Scholar]
- 10.Nevzati E, Fandino J, Schatlo B et al (2017) Validation and accuracy of intraoperative CT scan using the Philips AlluraXper FD20 angiography suite for assessment of spinal instrumentation. Br J Neurosurg. 10.1080/02688697.2017.1297764:1-6 [DOI] [PubMed]
- 11.Farber GL, Place HM, Mazur RA, Jones DE, Damiano TR. Accuracy of pedicle screw placement in lumbar fusions by plain radiographs and computed tomography. Spine (Phila Pa 1976) 1995;20:1494–1499. doi: 10.1097/00007632-199507000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Kim YJ, Lenke LG, Bridwell KH, Cho YS, Riew KD. Free hand pedicle screw placement in the thoracic spine: is it safe? Spine (Phila Pa 1976) 2004;29:333–342. doi: 10.1097/01.BRS.0000109983.12113.9B. [DOI] [PubMed] [Google Scholar]
- 13.Maejima R, Takeuchi M, Wakao N, et al. Reliability of an intraoperative radiographic anteroposterior view of the spinal midline for detection of pedicle screws breaching the medial pedicle wall in the thoracic, lumbar, and sacral spine. World Neurosurg. 2019;125:e257–e261. doi: 10.1016/j.wneu.2019.01.058. [DOI] [PubMed] [Google Scholar]
- 14.Sarwahi V, Ayan S, Amaral T, et al. Can postoperative radiographs accurately identify screw misplacements? Spine Deform. 2017;5:109–116. doi: 10.1016/j.jspd.2016.10.007. [DOI] [PubMed] [Google Scholar]
- 15.Scheufler KM, Franke J, Eckardt A, Dohmen H. Accuracy of image-guided pedicle screw placement using intraoperative computed tomography-based navigation with automated referencing. Part II: thoracolumbar spine. Neurosurgery. 2011;69:1307–1316. doi: 10.1227/NEU.0b013e31822ba190. [DOI] [PubMed] [Google Scholar]
- 16.Garber ST, Bisson EF, Schmidt MH. Comparison of three-dimensional fluoroscopy versus postoperative computed tomography for the assessment of accurate screw placement after instrumented spine surgery. Global Spine J. 2012;2:95–98. doi: 10.1055/s-0032-1319775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Santos ER, Ledonio CG, Castro CA, Truong WH, Sembrano JN. The accuracy of intraoperative O-arm images for the assessment of pedicle screw postion. Spine (Phila Pa 1976) 2012;37:E119–E125. doi: 10.1097/BRS.0b013e3182257cae. [DOI] [PubMed] [Google Scholar]
- 18.Robb RA. The dynamic spatial reconstructor: an X-ray video-fluoroscopic CT scanner for dynamic volume imaging of moving organs. IEEE Trans Med Imaging. 1982;1:22–33. doi: 10.1109/TMI.1982.4307545. [DOI] [PubMed] [Google Scholar]
- 19.Scarfe WC, Farman AG. What is cone-beam CT and how does it work? Dent Clin N Am. 2008;52:707–730. doi: 10.1016/j.cden.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 20.Nasseh I, Al-Rawi W. Cone beam computed tomography. Dent Clin N Am. 2018;62:361–391. doi: 10.1016/j.cden.2018.03.002. [DOI] [PubMed] [Google Scholar]
- 21.Burström G, Nachabe R, Persson O, Edstrom E, Elmi Terander A. Augmented and virtual reality instrument tracking for minimally invasive spine surgery: a feasibility and accuracy study. Spine (Phila Pa 1976) 2019;44:1097–1104. doi: 10.1097/BRS.0000000000003006. [DOI] [PubMed] [Google Scholar]
- 22.Elmi-Terander A, Burström G, Nachabe R, et al. Pedicle screw placement using augmented reality surgical navigation with intraoperative 3D imaging: a first in-human prospective cohort study. Spine (Phila Pa 1976) 2019;44:517–525. doi: 10.1097/BRS.0000000000002876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Burström G, Buerger C, Hoppenbrouwers J, et al. Machine learning for automated 3-dimensional segmentation of the spine and suggested placement of pedicle screws based on intraoperative cone beam computer tomography. J Neurosurg Spine. 2019;31:147–154. doi: 10.3171/2018.12.SPINE181397. [DOI] [PubMed] [Google Scholar]
- 24.Edström E, Burström G, Nachabe R, Gerdhem P, Elmi Terander A. A novel augmented-reality-based surgical navigation system for spine surgery in a hybrid operating room: design, workflow, and clinical applications. Oper Neurosurg (Hagerstown) 2020;18:496–502. doi: 10.1093/ons/opz236. [DOI] [PubMed] [Google Scholar]
- 25.Elmi-Terander A, Burström G, Nachabe R, et al. Augmented reality navigation with intraoperative 3D imaging vs fluoroscopy-assisted free-hand surgery for spine fixation surgery: a matched-control study comparing accuracy. Sci Rep. 2020;10:707. doi: 10.1038/s41598-020-57693-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Edström E, Burström G, Persson O et al (2020) Does augmented reality navigation increase pedicle screw density compared to free-hand technique in deformity surgery? Single surgeon case series of 44 patients. Spine (Phila Pa 1976) 45(17):E1085-E1090 [DOI] [PubMed]
- 27.Edström E, Burström G, Omar A, et al. Augmented reality surgical navigation in spine surgery to minimize staff radiation exposure. Spine (Phila Pa 1976) 2020;45:E45–E53. doi: 10.1097/BRS.0000000000003197. [DOI] [PubMed] [Google Scholar]
- 28.Nachabe R, Strauss K, Schueler B, Bydon M. Radiation dose and image quality comparison during spine surgery with two different, intraoperative 3D imaging navigation systems. J Appl Clin Med Phys. 2019;20:136–145. doi: 10.1002/acm2.12534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Elmi-Terander A, Skulason H, Soderman M, et al. Surgical navigation technology based on augmented reality and integrated 3D intraoperative imaging: a spine cadaveric feasibility and accuracy study. Spine (Phila Pa 1976) 2016;41:E1303–E1311. doi: 10.1097/BRS.0000000000001830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gertzbein SD, Robbins SE. Accuracy of pedicular screw placement in vivo. Spine (Phila Pa 1976) 1990;15:11–14. doi: 10.1097/00007632-199001000-00004. [DOI] [PubMed] [Google Scholar]
- 31.Altman DG (1990) Practical statistics for medical research. CRC Press, Boca Raton, pp 403–406
- 32.Chaturvedi H, Shweta R. Evaluation of inter-rater agreement and inter-rater reliability for observational data: an overview of concepts and methods. J Indian Acad Appl Psychol. 2015;41:20–27. [Google Scholar]
- 33.Fleiss JL. Measuring nominal scale agreement among many raters. Psychol Bull. 1971;76:378. doi: 10.1037/h0031619. [DOI] [Google Scholar]
- 34.Collett D. Modelling binary data. Boca Raton: Chapman and Hall/CRC Press; 1999. p. 24. [Google Scholar]
- 35.Sing T, Sander O, Beerenwinkel N, Lengauer T. ROCR: visualizing classifier performance in R. Bioinformatics. 2005;21:3940–3941. doi: 10.1093/bioinformatics/bti623. [DOI] [PubMed] [Google Scholar]
- 36.Mendelsohn D, Strelzow J, Dea N, et al. Patient and surgeon radiation exposure during spinal instrumentation using intraoperative computed tomography-based navigation. Spine J. 2016;16:343–354. doi: 10.1016/j.spinee.2015.11.020. [DOI] [PubMed] [Google Scholar]
- 37.Kleinerman RA. Cancer risks following diagnostic and therapeutic radiation exposure in children. Pediatr Radiol. 2006;36(Suppl 2):121–125. doi: 10.1007/s00247-006-0191-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ronckers CM, Land CE, Miller JS, Stovall M, Lonstein JE, Doody MM. Cancer mortality among women frequently exposed to radiographic examinations for spinal disorders. Radiat Res. 2010;174:83–90. doi: 10.1667/RR2022.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cordemans V, Kaminski L, Banse X, Francq BG, Cartiaux O. Accuracy of a new intraoperative cone beam CT imaging technique (Artis zeego II) compared to postoperative CT scan for assessment of pedicle screws placement and breaches detection. Eur Spine J. 2017;26:2906–2916. doi: 10.1007/s00586-017-5139-y. [DOI] [PubMed] [Google Scholar]
- 40.Rao G, Brodke DS, Rondina M, Dailey AT. Comparison of computerized tomography and direct visualization in thoracic pedicle screw placement. J Neurosurg. 2002;97:223–226. doi: 10.3171/spi.2002.97.2.0223. [DOI] [PubMed] [Google Scholar]
- 41.Berazaluce AMC, Hanke RE, von Allmen D, Racadio JM (2019) The state of the hybrid operating room: technological acceleration at the pinnacle of collaboration. Curr Surg Rep 7(4):7