Abstract
The novel Coronavirus-2019 (COVID-19) was declared a pandemic by the World Health Organization (WHO) in March 2020, impacting the lifestyles, economy, physical and mental health of individuals globally. This study aimed to test the model triggered by physical symptoms resembling COVID-19 infection, in which the need for health information and perceived impact of the pandemic mediated the path sequentially, leading to adverse mental health outcomes. A cross-sectional research design with chain mediation model involving 4612 participants from participating 8 countries selected via a respondent-driven sampling strategy was used. Participants completed online questionnaires on physical symptoms, the need for health information, the Impact of Event Scale-Revised (IES-R) questionnaire and Depression, Anxiety and Stress Scale (DASS-21). The results showed that Poland and the Philippines were the two countries with the highest levels of anxiety, depression and stress; conversely, Vietnam had the lowest mean scores in these areas. Chain mediation model showed the need for health information, and the perceived impact of the pandemic were sequential mediators between physical symptoms resembling COVID-19 infection (predictor) and consequent mental health status (outcome). Excessive and contradictory health information might increase the perceived impact of the pandemic. Rapid COVID-19 testing should be implemented to minimize the psychological burden associated with physical symptoms, whilst public mental health interventions could target adverse mental outcomes associated with the pandemic.
Subject terms: Diseases, Medical research, Risk factors
Introduction
The coronavirus disease 2019 (COVID-19) was declared a pandemic by the World Health Organization (WHO) in March 2020. As of December 4 2020, the number of confirmed cases was 65,528,133, the number of death cases was 1,511,726 and the number of recovered cases was 45,371,073 worldwide1. While one may not necessarily contract COVID-19 during this time, certainly, his or her mental health is likely affected due to financial burden2, occupational injury due to potential risk of infection3 as well as the loss of livelihoods and opportunities4. The COVID-19 pandemic has become an urgent issue on global mental health and an unprecedented challenge for healthcare systems of all countries5. Emerging psychological disorders and mental health has been identified as the tenth leading research topic during the COVID-19 pandemic6.
A study of the early-stage COVID-19 pandemic in China found anxiety in 6.33% and depression in 17.17% of 600 respondents7. In other Asian countries, a new questionnaire, i.e., the Fear of COVID-19 Scale, was developed in Iran8, but this questionnaire did not measure other psychiatric symptoms such as depression. In Pakistan, mental illness poses a significant challenge to its under-resourced health care system9. In Italy, the healthcare system stretched to its limit because healthcare workers constituted10% of Italy’s confirmed COVID-19 cases10 As a result, recent guidelines recommended all healthcare workers should receive psychological support based on coping strategies for managing stress11. In Europe, the levels of psychiatric symptoms were generally low at the beginning of the COVID-19 pandemic. However, younger Spanish individuals with chronic diseases reported more symptoms than the rest of the population12. In the United States (US), Asian Americans were less likely to report psychiatric symptoms than Caucasian Americans during the COVID-19 pandemic13. Studies from China, Italy, Germany and Russia identified protective and risk person factors for mental health during COVID-19. Risk factors for adverse mental health include younger age14, especially young people who had to work outside their domicile15, reduced income14, family member infected by COVID-1915, having chronic diseases14, concerns related to COVID-19 infection for themselves or family members14, living alone14, having family conflicts14. Protective factors for mental health include disseminating reliable information16 and personal confidence by mastering knowledge of the pandemic17.
Researchers observed that mental health conditions such as depression and anxiety were affected by the pandemic18, but the underlying mechanisms remained unknown. Several behavioral theories could be applied to identify factors that influence mental health during the pandemic. One health behavior theory is the protection motivation theory developed by R.W. Rogers in 197519. According to this theory, the COVID-19 pandemic might trigger the threat-appraisal and coping-appraisal processes19. The public would experience uncertainty and become very concerned about physical symptoms, which resemble COVID-19 infection. Due to the potential threat and impact of the pandemic, they would become worried that they did not have enough health information to protect themselves. For the coping-appraisal process, a person would search for health information to enhance understanding of the pandemic and take measures to reduce the risk of developing an infection20. The information-buffer hypothesis suggests that health information could buffer against physical symptom threats, thus reducing anxiety, depression, and stress. On the contrary, the overload of health information, especially inaccurate and misleading information, might lead to adverse mental health outcomes. Recently, Amanzio et al. (2020) proposed a theoretical framework to explain the association between health information, the psychological impact of a pandemic, physical symptoms and mental health outcomes based on the nocebo phenomenon for the infectious disease21. During the COVID-19 pandemic, conflicting and inaccurate health information (e.g., contradictory advice on face mask use) could lead to negative thinking and expectation22, resulting in the nocebo effect21, which ultimately lead to adverse mental health outcomes23. In summary, the physical symptoms resembling COVID-19 infection would trigger the need to search for health information, affecting the perceived impact of the pandemic and ultimately adverse mental health outcomes (i.e., anxiety, depression and stress).
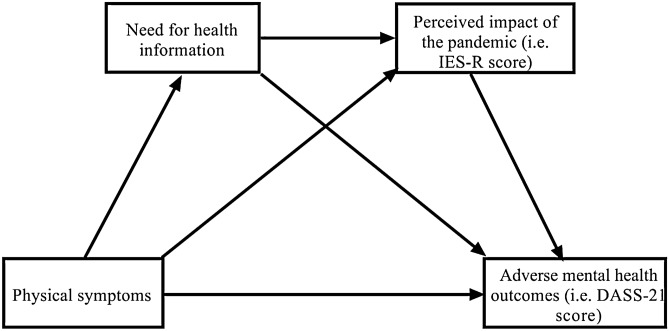
To address the above research gaps, this study aimed to compare the mental health outcomes in the general population of 8 countries (China, Pakistan, Philippines, Iran, Poland, Spain, the US, Vietnam) during the COVID-19 pandemic. Based on existing theoretical perspectives, we constructed a chain mediation model to test the following hypothesis (see Fig. 1): (a) the physical symptoms resembling COVID-19 infection would be positively associated with adverse mental health outcomes (i.e., depression, anxiety and stress); (b) the need for health information would mediate the association between physical symptoms and adverse mental health outcomes; (c) the perceived impact of COVID-19 pandemic would mediate the association between physical symptoms and adverse mental health outcomes; (d) the need for health information and perceived impact of the pandemic would be sequential mediators in the association between physical symptoms and adverse mental health outcomes.
Figure 1.
Proposed chain mediation model to explain the association between physical symptoms resembling COVID-19 infection and adverse mental health outcomes (i.e., anxiety, depression and stress).
Results
Demographics of participants
There were 4612 participants from 8 countries (866 from China, 982 from Poland, 619 from the Philippines, 651 from Spain, 571 from the US, 391 from Iran, 419 from Pakistan, and 113 from Vietnam) who took part in the Global Mental Health Survey during the COVID-19 pandemic. Supplementary Table 1 compares the demographics of 8 countries. More than half of the participants were women in all countries (United States: 52.9% to 79.0% in Spain) except Pakistan. More than half of Chinese participants were below the age of 31 years. More than half of the Spanish participants were above the age of 41 years. The majority of Chinese, Iranian, Vietnamese and Polish respondents were married, while most Filipino respondents were single. More than 70% of participants have a university degree.
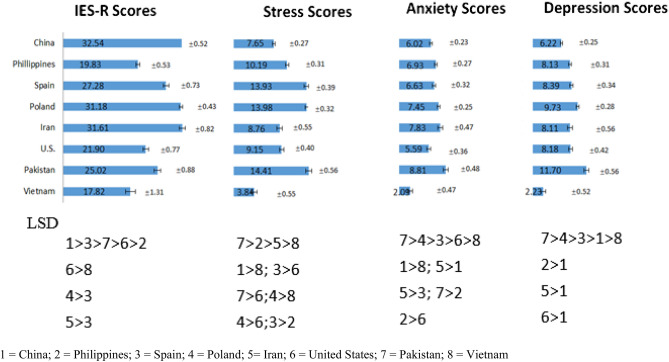
Comparison of mental health outcomes among 8 countries
Figure 2 compares the IES-R and DASS-21 scores among all countries. China (mean = 32.54, SD = 0.52), Iran (mean = 31.61, SD = 0.82) and Poland (mean = 31.18, SD = 0.43) were the three countries with highest IES-R scores. There were significant differences in IES-R scores among 8 countries ( F(7, 4604) = 61.79, η2 = 0.086, p < 0.001). Pakistan (mean = 14.41, SD = 0.56), Poland (mean = 13.98, SD = 0.32) and Spain (mean = 13.93, SD = 0.39) were the three countries with highest DASS-21 stress scores. There were significant differences in DASS-21 stress scores among 8 countries (F(7, 4599) = 62.41, η2 = 0.087, p < 0.001). Pakistan (mean = 8.81, SD = 0.48), Iran (mean = 7.83, SD = 0.47) and Poland (mean = 7.45, SD = 0.25) were the three countries with highest DASS-21 anxiety scores. There were significant differences in DASS-21 anxiety scores among 8 countries (F(7, 4603 ) = 14.71, η2 = 0.022, p < 0.001). Pakistan (mean = 11.70, SD = 0.56), Poland (mean = 9.73, SD = 0.28) and Spain (mean = 8.39, SD = 0.34) were the three countries with highest DASS-21 depression scores. There were significant differences in DASS-21 depression scores among 8 countries (F(7, 4604) = 26.00, η2 = 0.038, p < 0.001). Vietnam has the lowest IES-R (mean = 17.82, SD = 1.31), stress (mean = 3.24, SD = 0.55), anxiety (mean = 2.09, SD = 0.47) and depression (mean = 2.23, SD = 0.52) scores. The LSD analysis showed that the scores of Vietnam were significantly lower than each of the other countries (p < 0.05).
Figure 2.
Comparison of Impact of Event Scale (Revised) IES-R and Depression, Anxiety and Stress Scale-21 (DASS-21) scores among 8 countries based on the least significant difference (LSD) analysis. 1 = China; 2 = Philippines; 3 = Spain; 4 = Poland; 5 = Iran; 6 = United States; 7 = Pakistan; 8 = Vietnam.
Physical symptoms resembling COVID-19 and need for health information
Supplementary Table 2 shows the frequency of physical symptoms that resemble COVID-19 infection. During the COVID-19 pandemic, the most common physical symptoms reported by the participants in 8 countries were headache (28.62%), cough (20.73%) and sore throat (19.7%). The least frequent physical symptoms were breathing difficulties (11.56%), rigors or chills (11.27%) and fever (10.99%). The prevalence of other physical symptoms was coryza (19.32%), myalgia (16.37%), dizziness (15.26%) and gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea) (16.97%). Supplementary Table 3 shows the health information needs of participants from 8 countries. The top three information needs include understanding the effectiveness of drugs and vaccines available (70.22%), need for advice regarding treatment methods (64.36%) and information about local outbreaks (62.3%). Chinese participants reported the highest percentage for health information needs (> 90%).
Correlation of subscales
The mean average score per item for each subscale and correlations of sub-scales are displayed in Table 1. All the subscales were significantly correlated (p < 0.01) except for the need for health information with DASS-21 stress and depression subscales (p > 0.05). Physical symptoms resembling COVID-19 infection were positively and significantly associated with the perceived psychological impact of the pandemic as well as DASS-21 stress, anxiety and depression scores (p < 0.01). The need for health information was positively and significantly associated with the perceived psychological impact of the pandemic, DASS-21 anxiety score and physical symptoms (p < 0.01).
Table 1.
Descriptive statistics and correlations of mean average score per item among subscales for all participants in 8 countries (N = 4612).
| Sub-scales | M ± SD | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|---|
| 1.Perceived psychological impact of COVID-19 | 2.24 ± 1.27 | 1 | |||||
| 2.DASS-21 Stress | 1.75 ± 1.03 | .539** | 1 | ||||
| 3.DASS-21 Anxiety | 1.90 ± 1.36 | .539** | .735** | 1 | |||
| 4.DASS-21 Depression | 1.78 ± 1.21 | .485** | .767** | .723** | 1 | ||
| 5.Physical symptoms resembling COVID-19 infection | 1.06 ± 1.43 | .157** | .198** | .231** | .172** | 1 | |
| 6.The need for health information | 7.58 ± 3.42 | .172** | -0.003 | .055** | -0.001 | .096** | 1 |
†M refers to the mean average score per subscale. Mean average score = total score of subscale/number of items of a subscale.
*p < 0.05, **p < 0.01.
The chain mediation model
Table 2 presents the results from the mediation of the need for health information and the perceived impact of the pandemic in the relationship between physical symptoms resembling COVID-19 infection and adverse mental health outcomes. In the first step, physical symptoms were found to have a significant and positive association with the need for health information (p < 0.001). In the second step, both physical symptoms and the need for health information were observed to show a significant and positive association with the perceived impact of the pandemic (p < 0.001). In the third step, mediation analysis was performed to assess the association between physical symptoms, the need for health information, the perceived impact of the pandemic and mental health outcomes. For anxiety, physical symptoms, the need for health information and the perceived impact of the pandemic were significantly and positively associated with anxiety (p < 0.001). For depression, physical symptoms, the need for health information and the perceived impact of the pandemic were significantly and positively associated with depression (p < 0.001). For stress, physical symptoms, the need for health information and the perceived impact of the pandemic were significantly and positively associated with stress (p < 0.001).
Table 2.
Results of mediation analysis.
| Independent variables | Fit index | B | SE | T | 95% CI | |||
|---|---|---|---|---|---|---|---|---|
| R | R2 | F | LLCI | ULCI | ||||
| Dependent variable: need for health information | ||||||||
| Constant | 0.48 | 0.23 | 115.90*** | 9.70 | 0.12 | 80.88*** | 9.46 | 9.93 |
| Physical symptoms | 0.20 | 0.04 | 4.43*** | 0.11 | 0.28 | |||
| Dependent variable: perceived impact of the COVID-19 pandemic | ||||||||
| Constant | 0.34 | 0.12 | 47.36*** | 2.27 | 0.07 | 30.44*** | 2.12 | 2.41 |
| Need for health information | 0.03 | 0.01 | 5.62*** | 0.02 | 0.04 | |||
| Physical symptoms | 0.18 | 0.02 | 9.99*** | 0.14 | 0.21 | |||
| Dependent variable: DASS-21 anxiety score | ||||||||
| Constant | 0.60 | 0.36 | 180.77*** | − 0.12 | 0.07 | − 1.55 | − 0.26 | 0.03 |
| Need for health information | 0.01 | 0.01 | 1.18 | − 0.004 | 0.02 | |||
| Perceived impact of the pandemic | 0.59 | 0.01 | 44.22*** | 0.57 | 0.62 | |||
| Physical symptoms | 0.19 | 0.02 | 11.87*** | 0.16 | 0.22 | |||
| Dependent variable: DASS-21 depression score | ||||||||
| Constant | 0.55 | 0.31 | 144.37*** | 0.18 | 0.07 | 2.59** | 0.04 | 0.31 |
| Need for health information | -0.004 | 0.01 | -0.80 | -0.01 | 0.01 | |||
| Perceived impact of the pandemic | 0.49 | 0.01 | 39.11*** | 0.46 | 0.51 | |||
| Physical symptoms | 0.11 | 0.02 | 7.66*** | 0.09 | 0.14 | |||
| Dependent variable: DASS-21 stress score | ||||||||
| Constant | 0.62 | 0.39 | 209.76*** | 0.18 | 0.06 | 3.20** | 0.07 | 0.28 |
| Need for health information | -0.01 | 0.004 | -1.31 | -0.01 | 0.003 | |||
| Perceived impact of the pandemic | 0.46 | 0.01 | 45.89*** | 0.44 | 0.48 | |||
| Physical symptoms | 0.10 | 0.01 | 8.07*** | 0.07 | 0.12 | |||
B = unstandardized coefficient.
*** Significant at level p < 0.001.
Table 3 shows the chain mediating effect of the need for health information and the perceived impact of the COVID-19 pandemic between physical symptoms and various mental health outcomes. For anxiety, the chain mediating effect of the need for health information and perceived impact of the COVID-19 pandemic between physical symptoms and anxiety was significant (effect = 0.004, 95% CI = 0.002–0.007). For depression, the chain mediating effect of the need for health information and perceived impact of the pandemic between physical symptoms and depression was significant (effect = 0.003, 95% CI = 0.001–0.006). For stress, the chain mediating effect of the need for health information and perceived impact of the pandemic between physical symptoms and depression was significant (effect = 0.003, 95% CI = 0.001–0.005).
Table 3.
Results of the chain mediating effect based on Bootstrapping Test.
| 95% CI | ||||||||
|---|---|---|---|---|---|---|---|---|
| Effect | SE | LLCI | ULCI | |||||
| Dependent variable: DASS-21 Anxiety scores | ||||||||
| Physical symptoms → Need for health information → Anxiety | ||||||||
| 0.001 | 0.001 | -0.001 | 0.004 | |||||
| Physical symptoms → Need for health information → Perceived impact of the pandemic → Anxiety | ||||||||
| 0.004 | 0.001 | 0.002 | 0.007 | |||||
| Physical symptoms → Perceived impact of the pandemic → Anxiety | ||||||||
| 0.105 | 0.01 | 0.08 | 0.13 | |||||
| Dependent variable: DASS-21 Depression scores | ||||||||
| Physical symptoms → Need for health information → Depression | ||||||||
| -0.001 | 0.001 | -0.003 | 0.001 | |||||
| Physical symptoms → Need for health information → perceived impact of the pandemic → Depression | ||||||||
| 0.003 | 0.001 | 0.001 | 0.006 | |||||
| Physical symptoms → Perceived impact of the pandemic → Depression | ||||||||
| 0.086 | 0.009 | 0.068 | 0.104 | |||||
| Dependent variable: DASS-21 Stress scores | ||||||||
| Physical symptoms → Need for health information → Stress | ||||||||
| -0.001 | 0.001 | -0.003 | 0.0003 | |||||
| Physical symptoms → Need for health information → Perceived impact of events → Stress | ||||||||
| 0.003 | 0.001 | 0.001 | 0.005 | |||||
| Physical health → Perceived impact of events → Stress | ||||||||
| 0.08 | 0.01 | 0.06 | 0.10 | |||||
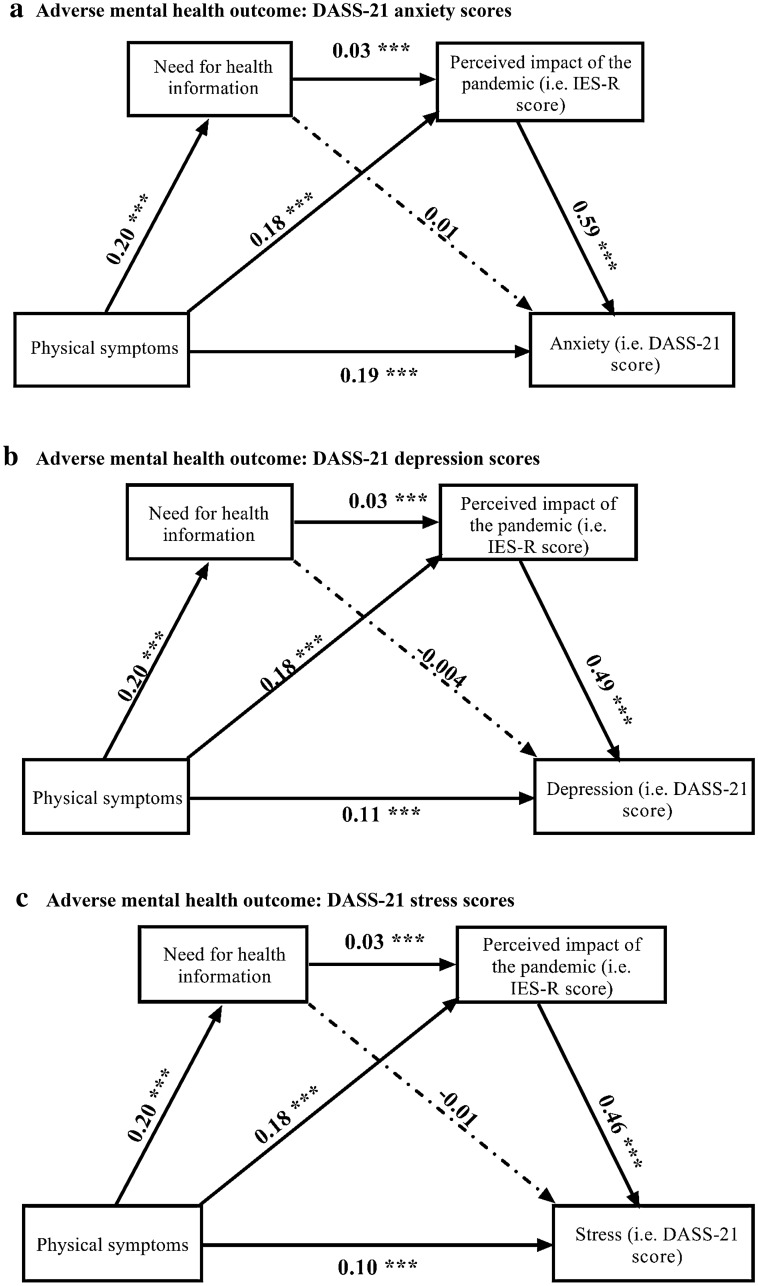
Figure 3a showed the chain mediating effect of the need for health information, and the sequential chain mediating effect for the need for health information and the perceived impact of the COVID pandemic in the association between physical symptoms and anxiety. All the paths in this model were significant (p < 0.001) except that the association between the need for health information and anxiety (B = 0.01, p > 0.05). Figure 3b showed the chain mediating effect of the need for health information, and the sequential chain mediating effect for the need for health information and the perceived impact of the COVID pandemic in the association between physical symptoms and depression. All the paths in this model were significant (p < 0.001) except that the association between the need for health information and depression (B = − 0.004, p > 0.05). Figure 3c showed the chain mediating effect of the need for health information, and the sequential chain mediating effect for the need for health information and the perceived impact of the COVID pandemic in the association between physical symptoms and stress. All the paths in this model were significant (p < 0.001) except that the association between the need for health information and stress (B = − 0.01, p > 0.05). For the three adverse mental health outcomes, the need for health information, when considered alone, did not act as a mediator.
Figure 3.
Tests of chain mediation model showed the indirect effect of need for health information, and the sequential indirect effects of the need for health information and perceived impact of the pandemic, in the association between physical symptoms resembling COVID-19 infection and adverse mental health outcomes. (a) Adverse mental health outcome: DASS-21 anxiety scores. *** Significant at level p < 0.001. (b) Adverse mental health outcome: DASS-21 depression scores. *** Significant at level p < 0.001. (c) Adverse mental health outcome: DASS-21 stress scores. *** Significant at level p < 0.001.
Discussion
The objective of this study was to compare the levels of DASS-21 scores and to rest the association between physical symptoms resembling COVID-19 infection and adverse mental health outcomes, as well as the mechanisms accountable for this association in multi-national populations across Asia, Europe and North America. The key findings were summarized as follows: (a) Poland and Pakistan were two countries with high levels of anxiety, depression and stress; (b) Vietnam had the lowest mean scores in anxiety, depression and stress; (c) Physical symptoms resembling COVID-19 infection was a risk factor for adverse mental health outcomes. Test of mediation showed that the need for health information explained partly of this mediation process. Although the need for health information did not act as a mediator when considered alone, there was a sequential mediating effect in which physical symptoms was associated with the need for health information, which in turn associated with higher perceived impact of the pandemic, which in turn associated with adverse mental health outcomes (i.e., anxiety, depression and stress).
Based on research conducted before the pandemic, the normative data for DASS-21 are as follows: the mean depression score was 3.87, the mean anxiety score was 2.95, and the mean stress score was 4.8724. In this study, the mean DASS-21 scores of all countries were higher than normative data except Vietnam. For IES-R, the means IES-R scores reported by healthy citizens after witnessing cardiopulmonary resuscitation (CPR) was 20.17.25. In this study, the mean IES-R scores of Chinese, Spanish, Polish, Iranian, American and Pakistani respondents were higher than healthy citizens witnessing CPR except for Filipino and Vietnamese. We observed that Pakistan and Poland were the two countries with the highest DASS-21 subscale scores. Before the COVID-19 pandemic, the World Happiness Report ranked the countries that had the greatest improvement of happiness from 2005–2008 to 2016–2018 as follows: Philippines (+ 0.860), Pakistan (+ 0.703), Poland (+ 0.445) and China (+ 0.426)26. In contrast, United States (− 0.446), Iran (− 0.713) and Spain (− 0.793) showed reduction in happiness scores from 2005–2008 to 2016–201826. The COVID-19 pandemic might reverse the increase in happiness scores in Poland and Pakistan. Each country faced unique challenges during the pandemic. Respondents from Poland reported high DASS-21 stress, anxiety and depression scores. A recent Polish study found that loneliness was correlated with psychiatric symptoms and emotional response to physical health threat during the COVID-19 pandemic27. Furthermore, increased worry about the social isolation and concerns for financial problems was observed in lonelier Poles27. Additionally, the Polish media frequently reported that the healthcare system in Poland was not prepared to fight the pandemic, having to deal with staff shortages, deficit in medicine supplies and personal protective equipment (PPE) for health personnel or hospital closures, which may have had an impact on the mental health of the Poles28. Pakistani respondents reported high levels of DASS-21 stress, anxiety and depression scores, which may be related to perceptions of an incomplete response to COVID-19 due to poor sanitation, lack of basic preventive measures, lack of proper testing and medical facilities28. Pakistani health professionals started protesting and threatened to quit work due to a lack of PPE28. The unpreparedness and contradictory policies resulted in an alarmingly high COVID-19 spread and worsening mental health of Pakistani people, although data collected on mental health was during the peak time of the COVID-19 spread in the country. Chinese respondents reported the highest IES-R scores. China was the first country to report COVID-19, but the Chinese people were also accused of not being transparent about the COVID-19 and spreading the virus across the world29. The editor-in-chief of The Lancet, Richard Horton expressed concern about discrimination or revenge actions toward China and Chinese30. Iran ranked second in terms of high IES-R and DASS-21 anxiety scores. The economic sanctions that prevented medical supplies, equipment and drugs from arriving in Iran31 could lead to anxiety among Iranians during the pandemic.
In this study, Vietnamese respondents were found to have the lowest DASS-21 and IES-R scores. Coincidentally, news reports identified Vietnam as one of the best countries in adopting multiples effective measures that have been key to fighting the COVID-19 pandemic to date32. Effective measures include dissemination of health information33, engagement of grassroots healthcare system34 and village health collaborators34, as well as safeguarding the health of workforce35 to ensure minimal impact on the economy.
The current study is the first to demonstrate the mediation mechanism underlying the association between physical symptoms resembling COVID-19 infection and mental health outcomes. Based on the chain mediation model, physical symptoms were positively associated with higher anxiety, depression and stress. This result adds to previous studies that have suggested that real or perceived infection threats could lead to negative psychological reactions36, and people's anxieties were closely related to physical symptoms37. Experiencing physical symptoms that resemble COVID-19 infection could trigger hypochondriasis38, and a higher number of physical symptoms experienced could lead to strong disease conviction39. As a result, rapid diagnostic test development and implementation are crucial to alleviating adverse mental health outcomes when a person experiences physical symptoms similar to COVID-19 infection40. The uncertainty of potential threat during the early stage of the COVID-19 pandemic could trigger anxieties, depression and stress much more than fear38. The current study also identified the role of health information as a mediator in the link between physical symptoms and the perceived impact of the pandemic. During the strict lockdown, people were refrained from social interaction41 and spent more time at home and searching for health information online. Consistent with the protection motivation theory19, the need to search for more health information is triggered by activity in survival circuits that detects imminent threats of COVID-19. Nevertheless, the need for health information was not associated with adverse mental health outcomes, which might partially support the information-buffer hypothesis. The need for health information formed a sequential mediation path with the perceived impact of the pandemic on mental health outcomes. This finding is consistent with previous research about information-induced behavioral changes during the COVID-19 lockdowns42. Excessive health information might heighten the perceived impact of the pandemic through cyberchondria that is defined as the unfounded escalation of concerns about COVID-19 symptoms based on a review of search results and literature online43. According to the nocebo phenomenon21, conflicting health information (e.g., confused face mask policy)22, unproven conspiracy theories44 and rumors45 also enhanced the negative impact of the pandemic. In contrast, people who were likely to less frequently accessed health information were less anxious, depressed and stressed, and worried about the pandemic46. Our findings confirmed the second path of the indirect effect: that physical symptoms resembling COVID-19 infection was associated with a higher level perceived impact of the pandemic and led to adverse mental health outcomes. This finding is consistent with previous research that symptoms of emerging infectious diseases might lead to stigma and adverse mental health outcomes47. In summary, the current study provided evidence that the perceived impact of the COVID-19 pandemic was associated with the need for health information which was rooted in the physical symptoms resembling COVID-19 infection. Physical symptoms were associated with adverse mental health outcomes with sequential mediation by the need for health information and perceived impact of the pandemic.
The findings of this first multi-national study have several implications on public mental health strategies. Firstly, Kaslow et al. (2020) proposed that community mental health strategies include providing support groups, participating in health education outreach and disseminating mental wellness guides48. Furthermore, mental health professionals should offer online psychological interventions such as cognitive behavior therapy (CBT) and mindfulness-based therapy to improve the general population's mental health49. The COVID-19 pandemic provides an opportunity to introduce and promote telepsychiatry that overcomes the quarantine measures and geographical distance for mental health assistance50. Second, as physical symptoms resembling COVID-19 infection (e.g., headache, chills, breathing difficulty, dizziness, coryza) were associated with adverse mental health outcomes, the lack of testing for coronavirus could worsen mental health. There is an urgent need to develop accurate, rapid diagnostic tests in general practitioners' clinics, community and rural settings51. For low income countries, coronavirus testing should be easily accessible and free. A negative COVID-19 test result for members of the general population who present with physical symptoms may alleviate anxiety, depression and stress. Third, based on our findings, the WHO, governments and health authorities should provide regular updates on health information including effectiveness of prevention strategies, therapeutics, and vaccines and treatment methods. The study results could contribute reference information to various countries that need to monitor public mental health status and provide accurate and consistent health information during the pandemic37.
Limitations
This study has several limitations. The first limitation was that the study population had different sociodemographic characteristics as compared to the world population. The respondent sampling method also compromised the representativeness of samples. The study population was female predominant (proportion of female in the study population: 68.55%; world population: 49.58%)52 and a high proportion of the study population possessed a university degree (proportion of degree holders in the study population: 70%; world population: 7%)53. The second limitation was sampling and selection bias because we could not reach out to potential respondents without Internet access in both countries. There was an uneven number of participants among 8 countries because 1938 Vietnamese participants were excluded due to incomplete questionnaires, and a smaller number of Iranian participants were recruited due to lack of Internet access in some areas of Iran. The third limitation was the cross-sectional nature of this study. Although the chain mediation model contributes to our understanding of the mediational factors that might influence the association between physical symptoms and adverse mental health outcomes, it cannot verify the temporal relationship. A longitudinal study is required to verify the direction of the paths further. The fourth limitation was that we did not record demographic data regarding the pre-existing mental illness of the study participants. The fifth limitation was that self-reported psychological impact levels, anxiety, depression and stress may not always be aligned with objective assessment by mental health professionals. Nevertheless, the perceived impact, anxiety, depression and stress are based on personal feelings, and self-reporting was paramount during the COVID-19 pandemic. The sixth limitation was that we could not confirm whether participants were seropositive to COVID-19 at the time of the survey because it was an online questionnaire-based study. Another possible limitation was the different recruitment periods of participants for each country and we planned to study the impact of COVID-19 during the peak periods that varied from country to country. Lastly, we were unable to calculate the response rate. For potential respondents who were not keen to participate in the online survey, no response was recorded, and we could not collect any information from them.
In conclusion, this multi-national study across three continents results provides empirical evidence that COVID-19 affected mental health worldwide. We found that Poland and Pakistan were two countries with the highest mean scores in IES-R and DASS-21 anxiety, depression and stress scales. In contrast, Vietnam had the lowest mean scores in IES-R and DASS-21 anxiety, depression and stress scales. The chain mediation model shows that the need for health information and the perceived impact of the pandemic exert sequential mediating effects on mental health outcomes in people who experience physical symptoms that resemble COVID-19 infection. It is hoped that these results will be public health values in formulating mental health strategies for the pandemic.
Materials and methods
Participants and questionnaires
The recruitment period for each country is listed as follows: China (February 28 to March 1, 2020), Philippines (March 28 to April 7, 2020), Spain (April 14 to 18, 2020), Iran (March 24 to 26, 2020), United States (April 21 to April 29, 2020), Pakistan (April 21 to July 6, 2020), Vietnam (April 7 to 14 2020) and Poland (March 22 to March 26, 2020). This study was approved by the institutional review boards of Complutense University of Madrid (Spain) (Protocol Number: IRB (Pr_2019_20_027), East Carolina University (The US) (Protocol Number: UMCIRB 20-000838), Hanoi Medical University (Vietnam) (Protocol Number: QD 75/QD-YHDP&YHDP), Huaibei Normal University (China) (Protocol Number: HBU-IRB-2020-002), Islamic Azad University (Iran) (Protocol Number: IRB-2020-001), University of Karachi (Pakistan) (Protocol Number: ICP-1 (101) 2698), the University of Philippines Manila (Protocol Number: UPMREB 2020-198-01) and the SWPS University of Social Sciences and Humanities (Poland) (Protocol Number: WKEB62/04/2020). This study was performed according to the Declaration of Helsinki, and the ethical principles in the Belmont Report. All participants were above the age of 18 years and provided informed consent prior to participation of this study.
This study used a theory-based questionnaire, the National University of Singapore (NUS) COVID-19 questionnaire, designed to examine the relationship between physical symptoms resembling COVID-19, health information required, the psychological impact of COVID-19 and mental health parameters. Its psychometric properties were established in the initial phase and peak of the COVID-19 epidemic54,55. The NUS COVID-19 questionnaire consisted of 3 subscales: (1) demographic data; (2) physical symptoms related to COVID-19 in the past 14 days, and (3) health information required for the COVID-19 pandemic. Demographic data about age, gender, education, household size, marital status, parental status and residential city in the past 14 days were collected. Physical symptoms related to COVID-19 included cough, fever, gastrointestinal and other symptoms. Respondents also rated their physical health status and stated their history of chronic medical illness. The health information required for the COVID-19 pandemic includes symptoms related to COVID-19, prevention and treatment advice, need for a regular update, knowledge in local transmission, the effectiveness of drugs and vaccines, travel advice, transmission methods and other countries' responses. The internal consistency of subscales on physical symptoms and the need for health information was examined using Cronbach alpha coefficients. Cronbach's alpha > 0.6 was considered acceptable reliability based on a previous theory-based questionnaire56. The Cronbach's alpha for physical symptoms and the need for health information subscales were 0.63 and 0.95, respectively.
The psychological impact of COVID-19 was measured using the Impact of Event Scale-Revised (IES-R). The IES-R is a self-administered questionnaire that has been well-validated in the American, European and Asian populations for determining the extent of psychological impact after exposure to a traumatic event (i.e., the COVID-19 pandemic) within one week of exposure57–60. This 22-item questionnaire is composed of three subscales, aiming to measure the mean avoidance, intrusion and hyperarousal61. The total IES-R score is divided into 0–23 (normal), 24 – 32 (mild psychological impact), 33–36 (moderate psychological impact) and > 37 (severe psychological impact)62. For the regression analysis, the cut-off score for high and low psychological impact was 24. In this study, the Cronbach's alpha for the different versions of IES-R are as follows: China: 0.949, Iran: 0.912, Pakistan: 0.95, Poland: 0.883, Philippines: 0.912, Spain: 0.948, the US: 0.959 and Vietnam: 0.92.
The mental health status of respondents was measured using the Depression, Anxiety and Stress Scale (DASS-21) and calculation of scores was based on a previous study63. DASS-21 has been used to assess mental health in American64, Asian65,66 and European67 populations. The internal consistency of DASS-21 stress, anxiety and depression scales was measured by the Cronbach's alpha. In this study, the Cronbach's alpha for different versions of DASS-21 is as follows: China: stress: 0.888, anxiety: 0.845, depression: 0.878; Iran: stress: 0.934, anxiety: 0.891, depression: 0.94; Pakistan: stress: 0.923, anxiety: 0.914, depression: 0.923; Philippines: stress: 0.839, anxiety: 0.784, depression: 0.889; Poland: stress: 0.890, anxiety: 0.854, depression: 0.886; Spain: stress: 0.895, anxiety: 0.876, depression: 0.89; The US: stress: 0.921, anxiety: 0.914, depression: 0.938 and Vietnam: stress: 0.864, anxiety: 0.866, depression: 0.904. For the regression analysis, the cut-off score for high stress score group was ≥ 35; the low stress score group was ≤ 10; high anxiety group was ≥ 20; low anxiety group was ≤ 6; high depression group was ≥ 28 and low depression group was ≤ 9. IES-R and DASS-21 were previously used in research related to the COVID-19 epidemic54,58,68,69..
Statistical analysis
Descriptive statistics were calculated to compare demographic characteristics, physical symptoms and health service utilization, contact history, knowledge and concern, precautionary measure and additional health information variables among 8 countries. One-Way analysis of variance (ANOVA) compared the mean IES-R and DASS-21 scores between 8 countries to determine whether the associated population mean IES-R or DASS-21 scores were significantly different. If there were significant differences among 8 countries, the Least Significant Difference (LSD) would calculate the smallest significance between mean scores of two countries with different combinations. Any difference larger than the LSD is considered a significant result. We used Pearson's correlation to calculate the correlation coefficients between physical symptoms, the need for health information, and the perceived impact of COVID-19 pandemic and adverse mental health outcomes. Then we followed a stepwise method to construct the best fitting model for the mediated effects of the need for health information and the perceived impact of the pandemic. Mediation analyses were conducted by a regression-based macro for SPSS version 21.070. In addition, a bootstrapping procedure with 2000 replications was run to test the chain mediation model. The significance levels of direct and indirect effects among the four factors (i.e., physical symptoms, health information requirement, the psychological impact of events and mental health parameters) and chain mediating effect would be determined. All tests were two-tailed, with a significance level of p < 0.05. Statistical analysis was performed on SPSS Statistic 21.0.
Disclaimer
The findings and conclusions in this manuscript are those of the authors, and do not necessarily represent an official position of the affiliated institutions.
Transparency declaration
The authors affirm that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Patient and Public Involvement statement
Patients or the public WERE NOT involved in the design, or conduct, or reporting, or dissemination plans of our research.
Dissemination declaration
Dissemination to these groups is not possible/applicable.
Supplementary Information
Author contributions
C.W., A.C.C., M.T., M.I.L.N., C.T., M.A.F., H.A.H., B.X.T., V.K., R.H., S.F.S. led the conception, design of the survey and coordinated research in each country. A.C.C., K.A., M.E.A.G., D.G., S.H., M.T.H., M.H., X.T.L., W.M., P.R., M.S., C.T., L.X., Z.X., G.T.V., D.Z. supported the training and supervision of data collection teams in each country and led the data analysis in each country. C.W., W.M., L.X., Z.X., D.Z. checked the quality of data and conducted the comparative analysis of all countries. N.A.C. translated results into English, prepared tables and integrated comments from all authors. C.W., A.C.C., M.T., M.I.L.N., C.T., M.A.F., H.A.H., B.X.T., V.K., R.M., C.H., R.H., S.F.S., K.A. contributed to writing and performed critical review of the manuscript. All co-authors substantially contributed to the interpretation of the results and to the preparation and writing of the manuscript.
Funding
This study has the following funding sources: Huaibei Normal University, China, Ministry of Science and Higher Education in Poland under the 2019–2022 program, Regional Initiative of Excellence", project number 012 / RID / 2018/19, National University of Singapore iHeathtech Other Operating Expenses (R-722-000-004-731) and Vingroup Innovation Foundation (VINIF) COVID research grant (VINIF.2020.Covid19.DA07) in Vietnam.
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-85943-7.
References
- 1.Worldmeters. COVID-19 Coronavirus Pandemic. (2020). https://www.worldometers.info/coronavirus/. Accessed 4 Dec 2020.
- 2.Li J, et al. Anxiety and depression among general population in China at the peak of the COVID-19 epidemic. World Psychiatry. 2020;19(2):249–250. doi: 10.1002/wps.20758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chirico F, Magnavita N. COVID-19 infection in Italy: An occupational injury. S. Afr. Med. J. 2020;110(6):12944. [PubMed] [Google Scholar]
- 4.Adhanom Ghebreyesus T. Addressing mental health needs: An integral part of COVID-19 response. World Psychiatry. 2020;19(2):129–130. doi: 10.1002/wps.20768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chirico, F.N.G. Tribute to healthcare operators threatened by COVID-19 pandemic. J. Health Soc. Sci.5(2), 65–168 (2020).
- 6.Tran, B.X., et al. Studies of novel coronavirus disease 19 (COVID-19) pandemic: A global analysis of literature. Int. J. Environ. Res. Public Health 17(11) (2020). [DOI] [PMC free article] [PubMed]
- 7.Wang, Y., et al. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol. Health Med. 1–10 (202). [DOI] [PubMed]
- 8.Ahorsu, D.K., et al. The fear of COVID-19 scale: Development and initial validation.Int. J. Ment. Health Addict. 1–9 (2020). [DOI] [PMC free article] [PubMed]
- 9.Hashmi, A.M., Saleem, H.A. New horizons: COVID-19 and the burden of neuropsychiatric illness in Pakistan.Pak. J. Med. Sci.36(Covid19-s4), S95–S98 (2020). [DOI] [PMC free article] [PubMed]
- 10.Chirico F, Magnavita N. The crucial role of occupational health surveillance for health-care workers during the COVID-19 pandemic. Workplace Health Saf. 2021;69(1):5–6. doi: 10.1177/2165079920950161. [DOI] [PubMed] [Google Scholar]
- 11.Chirico F, Nucera G, Magnavita N. Protecting the mental health of healthcare workers during the COVID-19 emergency. BJPsych. Int. 2021;18(1):E1. doi: 10.1192/bji.2020.39. [DOI] [Google Scholar]
- 12.Ozamiz-Etxebarria N, et al. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad Saude Publ. 2020;36(4):e00054020. doi: 10.1590/0102-311x00054020. [DOI] [PubMed] [Google Scholar]
- 13.Liu, C.H. et al. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Res. 290, 113172 (2020). [DOI] [PMC free article] [PubMed]
- 14.Guo Y, et al. Mental health disorders and associated risk factors in quarantined adults during the COVID-19 outbreak in China: Cross-sectional study. J. Med. Internet Res. 2020;22(8):e20328. doi: 10.2196/20328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mazza, C. et al. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: Immediate psychological responses and associated factors. Int. J. Environ. Res. Public Health17(9) (2020). [DOI] [PMC free article] [PubMed]
- 16.Qian M, et al. Anxiety levels, precautionary behaviours and public perceptions during the early phase of the COVID-19 outbreak in China: A population-based cross-sectional survey. BMJ Open. 2020;10(10):e040910. doi: 10.1136/bmjopen-2020-040910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moccia L, et al. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: An early report on the Italian general population. Brain Behav. Immun. 2020;87:75–79. doi: 10.1016/j.bbi.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.French MT, Mortensen K, Timming AR. Psychological distress and coronavirus fears during the initial phase of the COVID-19 pandemic in the United States. J. Ment. Health Policy Econ. 2020;23(3):93–100. [PubMed] [Google Scholar]
- 19.Rogers RW. A protection motivation theory of fear appeals and attitude change1. J. Psychol. 1975;91(1):93–114. doi: 10.1080/00223980.1975.9915803. [DOI] [PubMed] [Google Scholar]
- 20.Van der Velde FW, Van der Pligt J. AIDS-related health behavior: Coping, protection motivation, and previous behavior. J. Behav. Med. 1991;14(5):429–451. doi: 10.1007/BF00845103. [DOI] [PubMed] [Google Scholar]
- 21.Amanzio M, et al. How do nocebo phenomena provide a theoretical framework for the COVID-19 pandemic? Front. Psychol. 2020;11:589884. doi: 10.3389/fpsyg.2020.589884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kolstoe SE. Covid-19: Public messaging on vaccination must heed warnings from confused face mask messaging. BMJ. 2020;370:m3775. doi: 10.1136/bmj.m3775. [DOI] [PubMed] [Google Scholar]
- 23.Wells RE, Kaptchuk TJ. To tell the truth, the whole truth, may do patients harm: The problem of the nocebo effect for informed consent. Am. J. Bioeth. 2012;12(3):22–29. doi: 10.1080/15265161.2011.652798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Henry JD, Crawford JR. The short-form version of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. Br. J. Clin. Psychol. 2005;44(Pt 2):227–239. doi: 10.1348/014466505X29657. [DOI] [PubMed] [Google Scholar]
- 25.Zilberg NJ, Weiss DS, Horowitz MJ. Impact of Event Scale: A cross-validation study and some empirical evidence supporting a conceptual model of stress response syndromes. J. Consult. Clin. Psychol. 1982;50(3):407–414. doi: 10.1037/0022-006X.50.3.407. [DOI] [PubMed] [Google Scholar]
- 26.WHR. World Happiness Report: Change World Happiness. https://worldhappiness.report/ed/2019/changing-world-happiness/. Accessed 16 July 2020.
- 27.Okruszek, Ł., Aniszewska-Stańczuk, A., Piejka, A., Wiśniewska, M., Żurek, K. Safe But Lonely? Loneliness, Mental Health Symptoms and COVID-19. 2020: Poland. [DOI] [PMC free article] [PubMed]
- 28.Salman, M., et al. How prepared was Pakistan for the COVID-19 outbreak? Disaster Med. Public Health Prep. 1–5 (2020). [DOI] [PMC free article] [PubMed]
- 29.PTI. Trump Accuses China of Not Being Transparent About COVID-19; Says Beijing ‘Chose’ Not to Stop Coronavirus From Spreading. 2020. https://www.financialexpress.com/world-news/trump-accuses-china-of-not-being-transparent-about-covid-19-says-beijing-chose-not-to-stop-coronavirus-from-spreading/2030588/. Accessed 25 July 2020.
- 30.Catherine, W. It’s Unfair to Blame China for Coronavirus Pandemic, Lancet Editor Tells State Media. 2020. https://www.scmp.com/news/china/science/article/3082606/its-unfair-blame-china-coronavirus-pandemic-lancet-editor-tells. Accessed 8 May 2020.
- 31.Motevalli, G. Iran Says U.S. Sanctions Blocked Delivery of U.K.-Made Masks. 2020. https://www.bloomberg.com/news/articles/2020-03-21/iran-says-u-s-sanctions-blocked-delivery-of-u-k-made-masks. Accessed 12 Apr 2020.
- 32.Dao TL, Nguyen TD, Hoang VT. Controlling the COVID-19 pandemic: Useful lessons from Vietnam. Travel Med. Infect. Dis. 2020;37:101822. doi: 10.1016/j.tmaid.2020.101822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Le, H.T. et al. Demand for health information on COVID-19 among Vietnamese.Int. J. Environ. Res. Public Health17(12) (2020). [DOI] [PMC free article] [PubMed]
- 34.Tran BX, et al. The operational readiness capacities of the grassroots health system in responses to epidemics: Implications for COVID-19 control in Vietnam. J. Glob. Health. 2020;10(1):011006. doi: 10.7189/jogh.10.011006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tran BX, et al. Characterize health and economic vulnerabilities of workers to control the emergence of COVID-19 in an industrial zone in Vietnam. Saf. Sci. 2020;129:104811. doi: 10.1016/j.ssci.2020.104811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schweda A, et al. Phenotyping mental health: Age, community size, and depression differently modulate COVID-19-related fear and generalized anxiety. Compr. Psychiatry. 2020;104:152218. doi: 10.1016/j.comppsych.2020.152218. [DOI] [PubMed] [Google Scholar]
- 37.Jo W, et al. Online information exchange and anxiety spread in the early stage of the novel coronavirus (COVID-19) outbreak in South Korea: Structural topic model and network analysis. J. Med. Internet Res. 2020;22(6):e19455. doi: 10.2196/19455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Coelho CM, et al. On the nature of fear and anxiety triggered by COVID-19. Front. Psychol. 2020;11:581314. doi: 10.3389/fpsyg.2020.581314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pardue CM, White KS, Gervino EV. The role of disease conviction: Exploring its effects on chest pain and anxiety-related models of non-cardiac chest pain. J. Clin. Psychol. Med. Settings. 2019;26(2):131–141. doi: 10.1007/s10880-018-9572-9. [DOI] [PubMed] [Google Scholar]
- 40.Mitchell, S.L. et al. Understanding, verifying, and implementing emergency use authorization molecular diagnostics for the detection of SARS-CoV-2 RNA.J. Clin. Microbiol.58(8) (2020). [DOI] [PMC free article] [PubMed]
- 41.Jacques-Aviñó C, et al. Gender-based approach on the social impact and mental health in Spain during COVID-19 lockdown: A cross-sectional study. BMJ Open. 2020;10(11):e044617. doi: 10.1136/bmjopen-2020-044617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Buonomo, B., Della Marca, R.: Effects of information-induced behavioural changes during the COVID-19 lockdowns: The case of Italy.R. Soc. Open Sci.7(10), 201635 (2020). [DOI] [PMC free article] [PubMed]
- 43.Seyed Hashemi SG, et al. The mediating effect of the cyberchondria and anxiety sensitivity in the association between problematic internet use, metacognition beliefs, and fear of COVID-19 among Iranian online population. Heliyon. 2020;6(10):e05135. doi: 10.1016/j.heliyon.2020.e05135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shahsavari, S., et al. Conspiracy in the time of corona: Automatic detection of emerging COVID-19 conspiracy theories in social media and the news.J. Comput. Soc. Sci. 1–39 (2020). [DOI] [PMC free article] [PubMed]
- 45.Dong W, et al. Public emotions and rumors spread during the COVID-19 epidemic in China: Web-based correlation study. J. Med. Internet Res. 2020;22(11):e21933. doi: 10.2196/21933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shiina A, et al. Relationship between perception and anxiety about COVID-19 infection and risk behaviors for spreading infection: A national survey in Japan. Brain Behav. Immun. Health. 2020;6:100101. doi: 10.1016/j.bbih.2020.100101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Park HY, et al. Posttraumatic stress disorder and depression of survivors 12 months after the outbreak of Middle East respiratory syndrome in South Korea. BMC Public Health. 2020;20(1):605. doi: 10.1186/s12889-020-08726-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kaslow NJ, et al. Flattening the emotional distress curve: A behavioral health pandemic response strategy for COVID-19. Am. Psychol. 2020;75(7):875–886. doi: 10.1037/amp0000694. [DOI] [PubMed] [Google Scholar]
- 49.Ho CS, Chee CY, Ho RC. Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann. Acad. Med. Singap. 2020;49(1):1–3. doi: 10.47102/annals-acadmedsg.2019252. [DOI] [PubMed] [Google Scholar]
- 50.Di Carlo, F., et al. Telepsychiatry and other cutting-edge technologies in COVID-19 pandemic: Bridging the distance in mental health assistance.Int. J. Clin. Pract. (2020). [DOI] [PMC free article] [PubMed]
- 51.Tran BX, et al. Reaching further by Village Health Collaborators: The informal health taskforce of Vietnam for COVID-19 responses. J. Glob. Health. 2020;10(1):010354. doi: 10.7189/jogh.10.010354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Worldbank. Population, Female (% of Total Population). https://data.worldbank.org/indicator/SP.POP.TOTL.FE.ZS. Accessed 21 July 2020.
- 53.Bank, A.D. Statistics from Economic Research and Regional Cooperation Department. 2018. https://www.adb.org/mobile/basic-statistics-2018/. Accessed 2 Dec 2020.
- 54.Wang C, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17(5):E1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wang, C., et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China.Brain Behav. Immunity (2020). [DOI] [PMC free article] [PubMed]
- 56.Ma R, Castellanos DC, Bachman J. Identifying factors associated with fast food consumption among adolescents in Beijing China using a theory-based approach. Public Health. 2016;136:87–93. doi: 10.1016/j.puhe.2016.03.019. [DOI] [PubMed] [Google Scholar]
- 57.Zhang MW, et al. Usage of social media and smartphone application in assessment of physical and psychological well-being of individuals in times of a major air pollution crisis. JMIR mHealth uHealth. 2014;2(1):e16–e16. doi: 10.2196/mhealth.2827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chew, N.W.S., et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak.Brain Behav Immun. (2020). [DOI] [PMC free article] [PubMed]
- 59.Papadakaki M, et al. Physical, psychological and economic burden of two-wheel users after a road traffic injury: Evidence from intensive care units of three EU countries. J. Saf. Res. 2018;67:155–163. doi: 10.1016/j.jsr.2018.10.005. [DOI] [PubMed] [Google Scholar]
- 60.Hosey MM, et al. The IES-R remains a core outcome measure for PTSD in critical illness survivorship research. Crit. Care. 2019;23(1):362. doi: 10.1186/s13054-019-2630-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhang MWB, et al. Methodology of developing a smartphone application for crisis research and its clinical application. Technol. Health Care. 2014;22(4):547–559. doi: 10.3233/THC-140819. [DOI] [PubMed] [Google Scholar]
- 62.Creamer M, Bell R, Failla S. Psychometric properties of the impact of event scale - Revised. Behav. Res. Ther. 2003;41(12):1489–1496. doi: 10.1016/j.brat.2003.07.010. [DOI] [PubMed] [Google Scholar]
- 63.Le TA, et al. Multi-level predictors of psychological problems among methadone maintenance treatment patients in difference types of settings in Vietnam. Substance Abuse Treat. Prevent. Policy. 2019;14(1):39–39. doi: 10.1186/s13011-019-0223-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Norton PJ. Depression anxiety and stress scales (DASS-21): Psychometric analysis across four racial groups. Anxiety Stress Coping. 2007;20(3):253–265. doi: 10.1080/10615800701309279. [DOI] [PubMed] [Google Scholar]
- 65.Ho CSH, et al. Relationship of anxiety and depression with respiratory symptoms: Comparison between depressed and non-depressed smokers in Singapore. Int. J. Environ. Res. Public Health. 2019;16(1):163. doi: 10.3390/ijerph16010163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Quek TC, et al. Misophonia in Singaporean psychiatric patients: A cross-sectional study. Int. J. Environ. Res. Public Health. 2018;15(7):1410. doi: 10.3390/ijerph15071410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.González-Cabrera, J., et al. Cyberbullying in gifted students: Prevalence and psychological well-being in a Spanish sample. Int. J. Environ. Res. Public Health16(12) (2019). [DOI] [PMC free article] [PubMed]
- 68.Hao F, T.W., Jang, L., Zhang, L., Jiang, X., McIntyre, R.S., Zhang, Z., Sun, J., Ho, R., Ho, C., Tam, W. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav. Immun. (2020). [DOI] [PMC free article] [PubMed]
- 69.Tan, B.Y.Q., et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore.Ann. Intern. Med. (2020). [DOI] [PMC free article] [PubMed]
- 70.AF, H. Introduction to Mediation, Moderation and Conditional Process Analysis: A Regression-Based Approach. (Guildford Press, 2013).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.