ABSTRACT
Introduction
Tinnitus is prevalent among Service members and Veterans and is often comorbid with mental health disorders. Associations between the severity of individuals’ tinnitus and mental health symptoms are not well described.
Materials and Methods
We conducted a population-based survey of a stratified random sample of 1,800 Veterans diagnosed with tinnitus. We used the Tinnitus Functional Index to measure tinnitus severity and the Primary Care-Posttraumatic Stress Disorder (PTSD) screen and the Hospital Anxiety and Depression Scale to assess PTSD, depression, and anxiety. Descriptive statistics and bivariable and multivariable regression models were used to estimate associations between Veterans’ tinnitus severity and mental health symptoms. Inverse probability weights were used to account for sample stratification and survey non-response. Multivariable odds ratios (ORs) and 95% confidence intervals (CIs) controlled for Veterans’ demographics, military history, and health diagnoses.
Results
A total of 891 Veterans completed surveys (adjusted response rate = 53%). Large proportions rated their tinnitus as severe (29.4%; 95% CI: 27.2-31.6) or very severe (18.7%; 95% CI: 16.8-20.5). In multivariable regression models, and compared with Veterans with none/mild tinnitus, the likelihood of screening positive for PTSD was increased for those who reported moderate (OR = 4.0; 95% CI: 1.6-10.3), severe (OR = 7.5; 95% CI: 3.1-18.5), or very severe (OR = 17.5; 95% CI: 4.4-70.0) tinnitus. Similarly, Veterans’ likelihood of positive depression screens were elevated for those with moderate (OR = 2.6; 95% CI: 1.1-5.9), severe (OR = 3.0; 95% CI: 1.4-6.5), or very severe (OR = 15.5; 95% CI: 4.3-55.5) tinnitus, as was the likelihood of positive anxiety screens for those with severe (OR = 2.6; 95% CI: 1.1-6.3) or very severe (OR = 13.4; 95% CI: 4.0-44.3) tinnitus.
Conclusions
Mental health symptoms are strongly associated with Veterans’ tinnitus severity. A better understanding of the interplay between these conditions may help improve the provision of interdisciplinary (Audiology and Mental Health) care for Service members and Veterans.
INTRODUCTION
Tinnitus, the sensation of ringing or other sounds in the ear or head in the absence of acoustic stimuli, is the most prevalent disability among U.S. Veterans.1,2 In 2018, nearly 160,000 Veterans began receiving Department of Veterans Affairs (VA) disability compensation for tinnitus, bringing the total number of Veterans that are service-connected for tinnitus to approximately 2.0 million.2 Many Veterans seek help for their tinnitus from healthcare providers.3–5 Among the 7.1 million who used VA healthcare between 2011 and 2016, more than 13% were diagnosed with tinnitus.5 Tinnitus is similarly prevalent among active duty Service members, with large numbers also seeking help from military healthcare providers.6–8 It has been estimated that those with past military service are about twice as likely to experience tinnitus than their non-military civilian counterparts.9,10
Many individuals who experience tinnitus are not adversely affected by it; however, a substantial proportion reports it to be bothersome and intrusive. Tinnitus can cause concentration difficulties, inability to sleep, agitation, and emotional distress.4 It is often associated with mental health disorders, a phenomenon that may be physiological as well as psychological in etiology.11 Indeed, Veterans diagnosed with tinnitus by VA healthcare providers are twice as likely than those without tinnitus to be diagnosed with mental health or behavioral disorders, including posttraumatic stress disorder (PTSD), depression, anxiety, and substance use disorders.5 It is notable that cognitive behavioral therapy is recognized as an evidence-based treatment for both tinnitus and mental health disorders.12 This suggests a role for collaborative Audiology and Mental Health services that can address the co-occurrence of these conditions, a recommendation that has been previously described.13
Although research has identified robust assoc- iations between tinnitus and mental health diagnoses, the co-occurrence of active symptoms and the role of tinnitus severity on mental health disorders are not as well established. A better understanding of the interplay between tinnitus severity and mental health symptoms could inform the provision of interdisciplinary care for Service members or Veterans who are identified with one or more of these disorders. The objective of this study was to examine associations between self-reported tinnitus severity and symptoms of PTSD, depression, and anxiety among Veterans who use VA healthcare and have sought care for tinnitus.
METHODS
Overview
This was a population-based survey of Veterans who used VA healthcare and were diagnosed with tinnitus. Veterans were asked to complete a mailed or internet survey that asked them to report the impact of tinnitus on their daily functioning and symptoms of mental health disorders. A $20 incentive was paid to those who completed the survey. The conduct of this study was approved by the VA Portland Health Care System Institutional Review Board (IRB) and Research and Development Committees.
Sampling Frame
The sampling strategy for this study is presented in Fig. 1. Using data from the VA Corporate Data Warehouse, which contains healthcare records of all Veterans receiving VA services, we identified over 7.9 million unique Veterans who used VA health services nationally for the 5-year period between October 1, 2011 and September 30, 2016. From this population, we selected a random sample of 715,400. Veterans were excluded if they were deceased, enrolled in hospice or palliative care, or had not received VA outpatient care during the study period (e.g., had only received inpatient care). Of those remaining, 13.4% had been diagnosed with tinnitus (identified using International Classification of Diseases [ICD] diagnosis codes) one or more times as either an inpatient or outpatient, and 3.8% had been diagnosed one or more times as an inpatient or two or more times as an outpatient.5 Using the group that met this more stringent definition of tinnitus diagnosis, we identified Veterans who had non-missing ages, were < 90 years of age, had complete addresses, and were not institutionalized. We then restricted our sample to those who had used the VA between October 1, 2015 and September 30, 2016 in order to ensure the most up-to-date mailing addresses. This left a final sampling frame of 19,867 Veterans.
FIGURE 1.
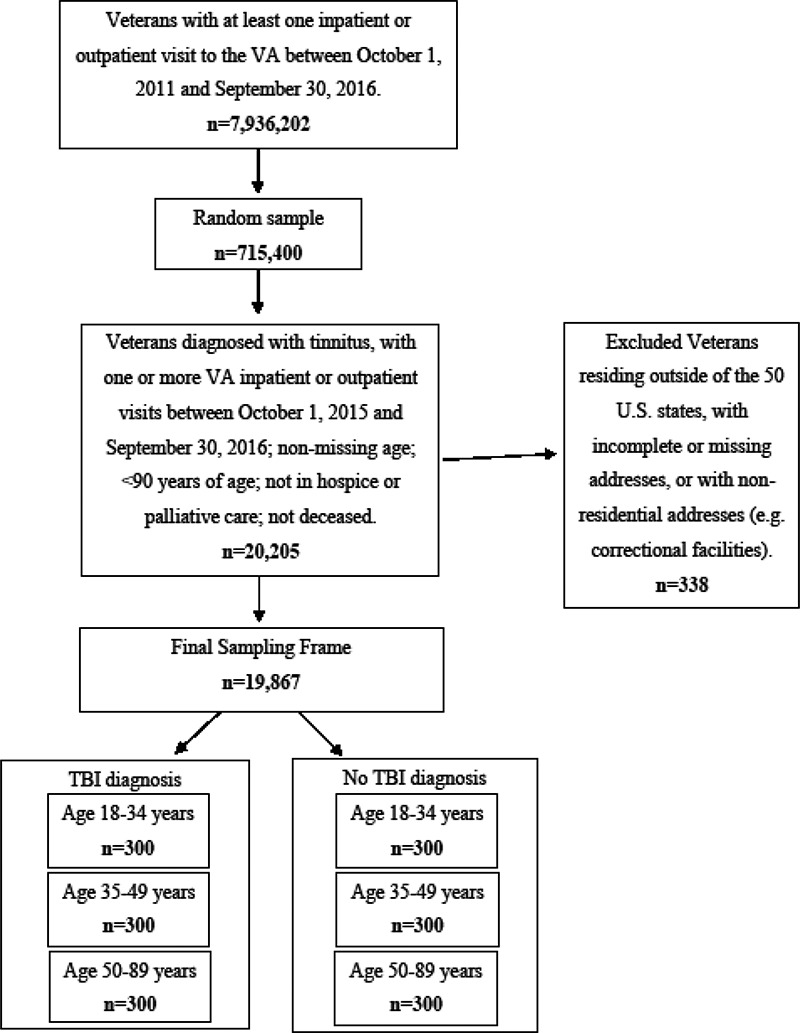
Development of final sampling frame and selection of stratified random sample of n = 1,800 Veterans diagnosed with tinnitus by Department of Veterans Affairs (VA) healthcare providers. TBI, traumatic brain injury.
From this sampling frame, we randomly sampled 1,800 Veterans, stratified by comorbid traumatic brain injury (TBI) diagnosis status (yes/no) and categories of age (18-34; 35-49; 50-89 years) to increase precision and ensure sufficient responses for analyses relative to these variables (n = 300 were sampled from each of the six strata). Age and TBI diagnosis (based on ICD codes, as used previously, and ascertained for the entire 5-year period from October 1, 2011 to September 30, 2016) were collected from Veterans’ healthcare records in the Corporate Data Warehouse.14 TBI was used as a stratification variable because of its prevalence among recent Service members and Veterans, its role in Veterans’ receipt of VA healthcare, and its strong association with both tinnitus and mental health disorders; thus, oversampling Veterans with TBI diagnoses helped ensure sufficient numbers of participants with TBI for analyses.5,6,15,16 Sampled Veterans were invited by mail to participate in the survey.
Procedures
To the extent allowed by the IRB, we used Dillman’s Tailored Design Method to recruit Veterans into the study and to maximize survey response rates.17 First, using addresses obtained from VA data, sampled Veterans received via U.S. Postal Service an introductory letter explaining the study’s purpose, a scannable paper survey booklet, instructions that included elements of informed consent, and a return envelope. The letters included language describing an alternative option to complete the survey online, which was hosted on our university affiliate’s server using Research Electronic Data Capture (REDCap) tools. Survey questions consisted of true/false, multiple choice, Likert-type scales, and open-ended response items. The paper survey booklet and online survey contained the same questions, with the exception of open-ended response items, which were excluded from the online survey because of IRB internet security requirements.
Measures
Veterans’ demographic and military history characteristics were identified using VA administrative data and survey items. Demographic characteristics included age at the time the sample was drawn (categorized as 18-34, 35-49, and 50-89 years), sex (male versus female), marital status (married versus not married), race (white versus all other races), education (high school or less, vocational/Associate’s degree, and college degree or more), annual household income (<$50,000 versus ≥$50,000), region of residence (West, Midwest, South, and Northeast), length of military service (<5 years versus ≥ 5 years), military branch (Army, Air Force, Navy, Marine Corps), military status (separated versus guard/reserves/active duty), and VA service connection status, an indicator of disability related to Veterans’ military service (not service connected, service connected < 50%, and service connected ≥ 50%).18
Tinnitus severity was measured using the Tinnitus Functional Index, a validated instrument that was developed to measure the effects of tinnitus on daily functioning.19 Responses were categorized as none or mild, moderate, severe, and very severe using recommended cut points of 0-31, 32-53, 54-72, and 73-100, respectively.20 Diagnoses of pain, PTSD, depression, and anxiety were identified using diagnosis codes identified in Veterans’ health records from the VA Corporate Data Warehouse. We used ICD—ninth revision—Clinical Modification (ICD-9-CM) codes to identify diagnoses through September 30, 2015 and ICD-10-CM codes to identify those assigned between October 1, 2015 and September 30, 2016; equivalent diagnoses between the two systems were identified using a mapping table published by the Centers for Medicare & Medicaid Services. We coded Veterans as having a diagnosis if the relevant ICD codes were assigned during two or more outpatient visits or one or more inpatient stay for the 5-year period between October 1, 2011 and September 30, 2016.
Veterans’ current mental health symptoms, assessed at the time of the survey, included PTSD, depression, and anxiety. PTSD was evaluated using the Primary Care-PTSD Screen, a validated, four-item measure used by the VA to screen Veterans for PTSD in primary care and other medical settings.21 We defined a positive PTSD screen as answering ‘yes’ to at least three out of the four screening questions.21 Depression and anxiety were assessed using the Hospital Anxiety and Depression Scale, a brief, validated self-assessment to screen for anxiety and depression symptoms in non-psychiatric hospital settings.22 Depression was defined as a total score of eight or higher on the seven depression screening questions. Similarly, anxiety was defined as a total score of eight or higher on the seven anxiety screening questions.
Data Analysis
Using descriptive analyses, we examined frequencies of all demographics, military history variables, clinical characteristics, and survey responses for the participants. We then estimated population proportions and their 95% confidence intervals (CIs) for each variable. Inverse probability weights were used to account for our stratified sampling design as well as survey non-response.23 Data were cross-tabulated to examine associations between the independent (tinnitus severity levels) and dependent (positive screens for PTSD, depression, and anxiety) variables of interest. Bivariable logistic regression models were used to compute odds ratios (ORs) and 95% CIs, estimating the strength of the associations between variables. Multivariable logistic regression modeling was used to estimate associations while controlling for potentially confounding variables; we employed a model specification strategy based on causal modeling and directed acyclic graphing techniques.24 Covariates for each model included age, sex, race (used as an indicator of experience with discrimination or structural racism), education level, marital status, region of residence, military branch, military status, time in military, service-connection status, and past diagnoses (October 1, 2011 through September 30, 2016) of TBI, pain, PTSD, depression, and anxiety. Analyses were performed using SAS/STAT software Version 9.4.
RESULTS
Of the 1,800 mailed surveys, 110 (6.1%) were returned as undeliverable, and 10 (0.5%) were returned with an indication that the Veteran was now deceased. A total of 891 Veterans returned completed surveys (adjusted response rate = 53% of those not undeliverable), including 692 by U.S. mail and 199 online using REDCap. Response rates were nearly the same for Veterans diagnosed with TBI (n = 446) and those without TBI diagnoses (n = 445).
Population Characteristics
Population characteristics (i.e., based on weighted data representing the entire sampling frame) are presented in Table I. Most of the population was male (95.6%; 95% CI: 94.7-96.6), white (73.9%; 95% CI: 71.8-76.0), had a vocational or Associate’s degree (51.7%; 95% CI: 49.3-54.1), and had spent < 5 years in the military (59.3%; 95% CI: 57.0-61.7). Many (46.6%; 95% CI: 44.2-49.0) had a VA service-connected disability rating ≥ 50%. Large proportions had been diagnosed by their VA healthcare providers with pain (75.4%; 95% CI: 73.3-77.6), PTSD (29.5%; 95% CI: 27.4-31.5), depression (32.3%; 95% CI: 30.1-34.6), and anxiety (16.8%; 95% CI: 15.1-18.5) during the 5-year period between October 1, 2011 and September 30, 2016. Only 5.6% (95% CI: 5.6-5.7) had been diagnosed with TBI.
TABLE I.
Sociodemographic, Military, and Clinical Characteristics of Veterans Diagnosed With Tinnitus, by Tinnitus Severity; N = 891
| None/Mild (n = 171) (26.5%; 24.3-28.7) |
Moderate (n = 223) (25.4%; 23.3-27.5) |
Severe (n = 253) (29.4%; 27.2-31.6) |
Very severe (n = 244) (18.7%; 16.8-20.5) |
||
|---|---|---|---|---|---|
| Characteristic | n | Weighted proportion % (95% CI) |
Weighted proportion % (95% CI) |
Weighted proportion % (95% CI) |
Weighted proportion % (95% CI) |
| Demographic and Military Service Characteristics | |||||
| Age | |||||
| 18-34 | 75 | 33.5 (28.2-38.9) | 35.2 (30.0-40.5) | 26.7 (21.7-31.6) | 4.6 (3.1-6.0) |
| 35-49 | 225 | 20.0 (17.1-22.8) | 22.4 (19.5-25.2) | 34.5 (31.2-37.8) | 23.1 (20.3-26.0) |
| 50-89 | 591 | 26.8 (24.4-29.2) | 25.4 (23.1-27.7) | 29.1 (26.6-31.5) | 18.7 (16.7-20.8) |
| Sex | |||||
| Male | 836 | 27.4 (25.1-29.7) | 24.7 (22.5-26.8) | 29.0 (26.7-31.3) | 18.9 (16.9-20.8) |
| Female | 55 | 6.1 (3.7-8.4) | 41.5 (30.6-52.3) | 37.6 (26.7-48.4) | 14.9 (10.5-19.3 |
| Marital Status | |||||
| Married | 612 | 23.7 (21.2-26.2) | 27.2 (24.7-29.8) | 30.5 (27.9-33.2) | 18.6 (16.4-20.7) |
| Not married | 279 | 34.0 (29.4-38.7) | 20.6 (16.9-24.2) | 26.4 (22.4-30.4) | 19.0 (15.3-22.6) |
| Race | |||||
| White | 595 | 30.1 (27.4-32.9) | 25.4 (22.9-27.9) | 30.0 (27.4-32.6) | 14.4 (12.5-16.3) |
| All other races | 296 | 16.2 (12.9-19.6) | 25.3 (21.4-29.3) | 27.6 (23.6-31.7) | 30.8 (26.5-35.1) |
| Education | |||||
| High school or less | 151 | 20.1 (15.7-24.6) | 23.8 (19.2-28.4) | 33.0 (27.9-38.0) | 23.1 (18.6-27.6) |
| Vocational/Associates | 478 | 25.1 (22.1-28.1) | 27.7 (24.7-30.7) | 29.6 (26.6-32.7) | 17.6 (15.1-20.1) |
| College or more | 262 | 34.6 (30.0-39.2) | 22.3 (18.5-26.1) | 25.9 (21.8-30.1) | 17.2 (13.9-20.5) |
| Annual Household Income | |||||
| <$50,000 | 496 | 25.3 (22.2-28.3) | 21.5 (18.8-24.2) | 33.3 (30.2-36.5) | 19.9 (17.4-22.5) |
| ≥$50,000 | 395 | 28.0 (24.8-31.3) | 30.2 (26.9-33.5) | 24.6 (21.5-27.7) | 17.2 (14.5-19.9) |
| Region of Residence | |||||
| West | 225 | 30.7 (26.1-35.2) | 23.8 (19.8-27.9) | 34.0 (29.5-38.6) | 11.4 (8.7-14.2) |
| Midwest | 199 | 30.8 (26.3-35.3) | 24.2 (20.1-28.3) | 30.4 (26.0-34.8) | 14.6 (11.4-17.9) |
| South | 370 | 17.4 (14.4-20.4) | 30.0 (26.4-33.5) | 27.0 (23.5-30.5) | 25.7 (22.3-29.0) |
| Northeast | 97 | 39.3 (31.8-46.9) | 16.4 (11.1-21.7) | 27.5 (20.9-34.1) | 16.8 (11.3-22.2) |
| Time Served in Military | |||||
| < 5 years | 379 | 30.1 (27.0-33.2) | 22.8 (20.0-25.5) | 27.4 (24.5-30.3) | 19.8 (17.2-22.4) |
| ≥ 5 years | 512 | 21.3 (18.4-24.3) | 29.3 (26.0-32.6) | 32.3 (28.9-35.7) | 17.1 (14.5-19.6) |
| Military Branch | |||||
| Air Force | 97 | 24.2 (18.5-29.9) | 21.7 (16.5-26.9) | 44.4 (37.9-50.9) | 9.7 (5.8-13.6) |
| Army | 531 | 23.8 (20.9-26.6) | 25.8 (23.0-28.6) | 28.5 (25.7-31.4) | 21.9 (19.2-24.5) |
| Navy | 137 | 41.6 (35.5-47.6) | 31.4 (25.6-37.1) | 19.0 (14.4-23.6) | 8.1 (5.5-10.7) |
| Marine Corps | 126 | 23.4 (17.7-29.2) | 20.4 (14.7-26.1) | 27.5 (21.4-33.6) | 28.6 (22.4-34.8) |
| Military Status | |||||
| Separated | 858 | 26.6 (24.4-28.9) | 24.9 (22.7-27.0) | 29.6 (27.4-31.9) | 18.9 (17.0-20.8) |
| Active or Guard/Reserves | 33 | 19.9 (12.4-27.5) | 58.0 (45.4-70.7) | 14.3 (5.0-23.7) | 7.7 (4.3-11.0) |
| Service Connection | |||||
| None | 136 | 29.3 (24.6-34.0) | 24.9 (20.5-29.3) | 39.6 (34.7-44.6) | 6.2 (4.0-8.4) |
| < 50% | 195 | 42.0 (37.2-46.7) | 27.0 (22.8-31.2) | 21.2 (17.4-24.9) | 9.9 (7.3-12.5) |
| ≥ 50% | 560 | 15.9 (13.4-18.4) | 24.8 (21.8-27.7) | 28.5 (25.4-31.6) | 30.9 (27.7-34.1) |
| Previous VA Diagnoses (in the 5-year period between October 1, 2011 and September 30, 2016) | |||||
| TBI Diagnosis | |||||
| Yes | 446 | 14.5 (13.0-16.1) | 24.5 (22.7-26.4) | 26.9 (25.0-28.7) | 34.1 (32.1-36.0) |
| No | 445 | 27.2 (24.9-29.6) | 25.5 (23.2-27.7) | 29.5 (27.2-31.9) | 17.8 (15.8-19.7) |
| Pain Diagnosis | |||||
| Yes | 767 | 23.5 (12.1-25.9) | 23.5 (21.2-25.9) | 29.0 (26.5-31.5) | 24.0 (21.7-26.3) |
| No | 124 | 35.9 (30.8-40.9) | 31.2 (26.6-35.9) | 30.5 (25.8-35.2) | 2.4 (1.3-3.5) |
| PTSD Diagnosis | |||||
| Yes | 473 | 16.5 (13.4-19.5) | 19.5 (16.4-22.6) | 27.8 (24.2-31.4) | 36.2 (32.2-40.2) |
| No | 418 | 30.7 (27.9-33.5) | 27.9 (25.2-30.6) | 30.0 (27.3-32.8) | 11.4 (9.5-13.2) |
| Depression Diagnosis | |||||
| Yes | 433 | 18.2 (15.0-21.4) | 19.5 (16.4-22.7) | 32.1 (28.2-35.9) | 30.2 (26.4-34.0) |
| No | 458 | 30.5 (27.6-33.3) | 28.2 (25.5-30.9) | 28.1 (25.4-30.8) | 13.2 (11.2-15.2) |
| Anxiety Diagnosis | |||||
| Yes | 233 | 14.0 (10.4-17.7) | 18.2 (14.1-22.3) | 39.2 (33.7-44.6) | 28.6 (23.8-33.4) |
| No | 658 | 29.0 (26.5-31.6) | 26.9 (24.5-29.3) | 27.4 (25.0-29.8) | 16.7 (14.7-18.7) |
Tinnitus Severity
Large proportions of survey respondents reported severe or very severe tinnitus, corresponding to weighted population proportions of 26.5% (24.3-28.7) with none or mild tinnitus, 25.4% (23.3-27.5) with moderate tinnitus, 29.4% (27.2-31.6) with severe tinnitus, and 18.7% (16.8-20.5) with very severe tinnitus. Tinnitus severity varied by Veterans’ demographic and military history characteristics and VA diagnoses. Compared with the youngest group of Veterans, a higher proportion of those 35 to 49 years of age reported severe (34.5%; 95% CI: 31.2-37.8) or very severe tinnitus (23.1%; 95% CI: 20.3-26.0). Similarly, a higher proportion of Veterans who reported a race other than white had very severe tinnitus compared with white Veterans (30.8%; 95% CI: 26.5-35.1 and 14.4%; 95% CI: 12.5-16.3, respectively). Compared with Veterans with higher education, larger proportions of Veterans with a high school degree or less reported severe (33.0%; 95% CI: 27.9-38.0) or very severe tinnitus (23.1%; 95% CI: 18.6-27.6).
Larger proportions of Veterans who served in the Army or Marine Corps had very severe tinnitus (21.9%; 95% CI: 19.2-24.5 and 28.6%; 95% CI: 22.4-34.8, respectively). However, Veterans who served in the Air Force had the highest proportion who reported severe tinnitus (44.4%; 95% CI: 37.9-50.9). A substantially higher proportion of Veterans service connected at ≥ 50% reported very severe tinnitus (30.9%; 95% CI: 27.7-34.1) compared with Veterans with < 50% or no service connection (9.9%; 95% CI: 7.3-12.5 and 6.2%; 95% CI: 4.0-8.4, respectively). Similarly, higher proportions of Veterans that had previous (5-year) diagnoses of TBI, pain, PTSD, depression, or anxiety from their VA healthcare providers reported very severe tinnitus than those without these respective diagnoses.
Mental Health Symptoms
There were 587 Veterans who screened positive for PTSD, 629 who screened positive for depression, and 659 who screened positive for anxiety, corresponding to population proportions of 39.5% (37.3-41.8), 58.8% (56.4-61.2) and 52.5% (50.1-55.0), respectively (Table II). The proportions of Veterans that screened positive for PTSD increased substantially as Veterans’ tinnitus severity increased from none/mild (15.0%; 95% CI: 12.1-17.9) to moderate (30.4%; 95% CI: 26.3-34.6), severe (46.6%; 95% CI: 42.1-51.0), and very severe (75.8%; 95% CI: 70.8-80.7). This pattern was also observed for those screening positive for depression (34.0%; 95% CI: 29.3-38.7 to 93.2%; 95% CI: 90.4-96.0) and for anxiety (29.8%; 95% CI: 25.5-34.2 to 87.5%; 95% CI: 83.7-91.3).
TABLE II.
Positive Posttraumatic Stress Disorder, Depression, and Anxiety Screening Results Among Veterans Diagnosed With Tinnitus, by Self-reported Tinnitus Severity
| n | Weighted proportion % (95% CI) |
Bivariable OR (95% CI) |
Multivariable OR (95% CI)a |
|
|---|---|---|---|---|
| Tinnitus Severity | Positive Screen for PTSD (n = 587; 39.5% [37.3-41.8]) | |||
| None/Mild | 71 | 15.0 (12.1-17.9) | Reference | Reference |
| Moderate | 132 | 30.4 (26.3-34.6) | 2.5 (1.2-5.1) | 4.0 (1.6-10.3) |
| Severe | 178 | 46.6 (42.1-51.0) | 4.9 (2.5-9.8) | 7.5 (3.1-18.5) |
| Very Severe | 206 | 75.8 (70.8-80.7) | 17.9 (7.0-45.6) | 17.5 (4.4-70.0) |
| Positive Screen for Depression (n = 629; 58.8% [56.4-61.2]) | ||||
| None/Mild | 76 | 34.0 (29.3-38.7) | Reference | Reference |
| Moderate | 136 | 55.1 (50.3-59.9) | 2.4 (1.2-4.9) | 2.6 (1.1-5.9) |
| Severe | 188 | 62.5 (58.2-66.9) | 3.2 (1.6-6.5) | 3.0 (1.4-6.5) |
| Very Severe | 229 | 93.2 (90.4-96.0) | 27.1 (8.4-87.5) | 15.5 (4.3-55.5) |
| Positive Screen for Anxiety (n = 659; 52.5% [50.1-55.0]) | ||||
| None/Mild | 82 | 29.8 (25.5-34.2) | Reference | Reference |
| Moderate | 151 | 45.0 (40.3-49.7) | 1.9 (1.0-3.7) | 2.0 (0.8-5.0) |
| Severe | 200 | 57.3 (52.9-61.8) | 3.2 (1.7-6.0) | 2.6 (1.1-6.3) |
| Very Severe | 226 | 87.5 (83.7-91.3) | 16.6 (5.9-46.8) | 13.4 (4.0-44.3) |
Multivariable models included age, sex, race, education level, marital status, region of residence, military branch, military status, time in military, service-connection status, and previous diagnoses (between October 1, 2011 and September 30, 2016) of traumatic brain injury, pain, PTSD, depression, and anxiety.
PTSD, posttraumatic stress disorder.
Associations Between Tinnitus Severity and Mental Health Symptoms
The results of logistic regression modeling suggested strong associations between increasing tinnitus severity and positive screens for PTSD, depression, and anxiety (Table II). Results were similar in both bivariable regression models and multivariable models controlling for Veterans’ demographics, military history characteristics, and 5-year diagnoses from VA healthcare providers. In multivariable models, compared with Veterans with none/mild tinnitus, the likelihood of screening positive for PTSD was increased for those who reported moderate (OR = 4.0; 95% CI: 1.6-10.3), severe (OR = 7.5; 95% CI: 3.1-18.5), or very severe (OR = 17.5; 95% CI: 4.4-70.0) tinnitus. Similarly, Veterans’ likelihood of positive depression screens tended to increase as their tinnitus severity increased from none/mild to moderate, severe, and very severe (OR = 2.6; 95% CI: 1.1-5.9; OR = 3.0; 95% CI: 1.4-6.5; and OR = 15.5; 95% CI: 4.3-55.5, respectively), as did their likelihood of positive anxiety screens for severe and very severe tinnitus (OR = 2.6; 95% CI: 1.1-6.3 and OR = 13.4; 95% CI: 4.0-44.3, respectively).
DISCUSSION
Using validated measures and a population-based sampling frame, this study examined the self-reported severity of tinnitus among Veteran VA users that had been diagnosed with tinnitus and estimated associations between levels of Veterans’ tinnitus severity and their symptoms of PTSD, depression, and anxiety. To our knowledge, our study is unique in its examination of tinnitus and mental health associations using such granular measures of tinnitus severity. The results of this work suggest that, even while controlling for a large number of potential confounders including past diagnoses of mental health disorders, associations between active symptoms of tinnitus and mental health are robust. Additionally, we found that the more severely Veterans’ tinnitus was ranked as affecting their daily functioning, the more likely they were to screen positive for mental health disorders. These findings suggest a need for greater awareness of the acute associations between tinnitus and mental health symptoms and enhanced coordination of Audiology and Mental Health services for individuals with tinnitus, particularly those with more severe cases.
Our study adds to a body of research that has identified associations between tinnitus and mental health diagnoses among treatment-seeking Service members, Veterans, and non-Veteran civilians.3,5–8,10,25–28 Across studies, greater proportions of individuals that are diagnosed with tinnitus have comorbid mental health diagnoses, including PTSD, depression, and anxiety. For example, up to one-third of Veterans seeking help for tinnitus have also been diagnosed with PTSD, a prevalence approximately three times greater than among those not seeking care for tinnitus.5,25 Although the potential for shared neurophysiological pathways exists, in which the same regions of the brain are involved in both emotional reactions to tinnitus and mood regulation, it is likely that one condition does not cause another.27,28 However, the experience of tinnitus may exacerbate mental health symptoms or, contrarily, mental health disorders may reduce the ability for individuals to cope with tinnitus. Regardless of the causal direction, those who experience both would potentially benefit from therapies that address both the physiological and psychological basis of these conditions.
A combined Audiology and Mental Health therapy for tinnitus, called Progressive Tinnitus Management (PTM), has been developed in the VA and implemented in a number of VA Audiology clinics.29,30 PTM incorporates sound therapy with components of cognitive behavioral therapy (CBT); randomized controlled trials show this program to reduce distress caused by tinnitus and to improve functioning, as represented by clinically significant reductions in TFI scores.31,32 In addition, PTM—as well as CBT alone—has been shown to reduce symptoms of both depression and anxiety among tinnitus sufferers.12,32 Military healthcare providers have adapted PTM for delivery to active duty Service members. There have been calls to improve access to this interdisciplinary program for the large number of Veterans who seek VA healthcare for tinnitus.13 However, with large numbers of Veterans in need of mental health services, it proves to be a challenge to incorporate mental healthcare into audiologic services for tinnitus.33 Ongoing research is examining methods to improve the implementation of PTM in the VA and across other settings.
PTM follows a stepped model of care, and it is important to note that the great majority of participants do not need more intensive services at the highest levels.31,32 Briefly, PTM Level 1 comprises referral guidelines for any healthcare provider to make appropriate referrals for a patient reporting tinnitus. Level 2 involves a standard audiologic evaluation, including a hearing exam and hearing aid evaluation when warranted, in addition to a brief assessment of the functional effects of tinnitus. Levels 1 and 2 can be implemented in hearing healthcare settings with minimal impact on clinical function. Because a number of patients attribute hearing difficulties to tinnitus, many who are assessed for hearing loss at Level 2 will not need to continue on to PTM Level 3.34 If further services are deemed appropriate for a patient, then Audiology and Mental Health collaboratively provide Level 3 skills education using audiologic and psychologic therapies (sound therapy and CBT, respectively).31,32 Most Veterans who progress to PTM Level 3 have their tinnitus-specific needs met at this level. Those requiring more intensive help may progress to Level 4, involving an in-depth interdisciplinary evaluation by an audiologist and a psychologist to determine if one-on-one assistance is warranted. Level 5 involves individualized support from Audiology and/or Mental Health, based on the outcome of the Level 4 evaluation. Although developed and evaluated in the VA setting, PTM is readily adaptable to other healthcare systems (particularly if Audiology and Mental Healthcare are already integrated) and to non-military or non-Veteran civilian patients.
Previous estimates have suggested that about 20% of civilian adults with tinnitus require clinical intervention in order to experience relief from symptoms.1,35 Assuming similar proportions of Veterans are affected, then at least 342,000 Veterans would benefit from access to evidence-based treatment. It was notable in this study that, among Veterans who had been diagnosed with tinnitus within the VA, such large proportions reported TFI scores indicating severe or very severe impacts of tinnitus on their daily functioning. Clearly, symptom management and minimizing distress for individuals with bothersome tinnitus should be a high priority among providers who encounter patients seeking help with tinnitus. Similar to our findings involving a VA sample, recent research involving a population-based civilian sample found that Veterans as well as non-Veteran civilians with tinnitus were more likely to report symptoms of both depression and anxiety; there were no differences in the strength of the observed associations between Veterans and non-Veterans.10 Thus, it stands to reason that, like the VA and Military Health System, civilian healthcare systems would also best support their patients with bothersome tinnitus by offering integrated Audiology and Mental Health services.
Another noteworthy finding from this study was the proportion of Veterans with tinnitus and comorbid TBI diagnoses who reported very severe tinnitus (34.1%) relative to those without comorbid TBI diagnoses (17.8%). This is not surprising given the growing body of research showing that Veterans with a history of TBI are more likely to report auditory problems—namely hearing difficulties and tinnitus—than those without TBI.3,5–7,26 The etiology of auditory dysfunction among individuals with a history of TBI is not well understood, particularly when experienced by those with audiometrically normal hearing.36 TBI-related auditory disorders are likely to vary by factors such as the source of TBI (e.g., blast/bomb versus blunt force), severity of TBI, physical location of injury, time since injury, and concomitant exposures. Research is needed to better understand the interplay between hearing impairment, tinnitus, and mental health disorders among individuals with TBI. In the present study, we observed associations between tinnitus severity and mental health symptoms even after controlling for TBI, suggesting that these patterns are at least consistent in Veterans both with, and without, TBI. Notably, a modified version of a tinnitus management program (PTM Level 3 Audiology and Mental Health skills training) has been developed and shown to be efficacious for Veterans with potential limitations because of TBI (e.g., attentional deficits).32
Limitations
Limitations of this work include the potential for lack of generalizability of trends observed among Veteran VA users to Veterans who seek healthcare outside the VA, Service members, or even civilians, who also commonly experience tinnitus.35 However, ours was a population-based survey that was designed to be representative of Veterans who have been diagnosed with tinnitus in the VA and our results are similar to recent population-based research involving civilians.10 Thus, it is likely that results reflect, at least to some extent, the experiences of other cohorts that suffer from tinnitus. Additionally, uncertainty about data accuracy may be a limitation of this work. For example, the ICD diagnosis codes used to identify Veterans’ clinical characteristics may not accurately represent Veterans’ health status, given potential miscoding, and the fact that these codes represent treatment receipt rather than Veterans’ actual disease states. Our approach of coding a Veteran with a diagnosis if they had one or more respective inpatient, or two or more outpatient, ICD codes assigned at any time during the 5-year period between October 1, 2011 and September 30, 2016 may make this possibility less of a concern. Finally, the wide CIs associated with the ORs estimating associations between tinnitus severity and mental health symptom variables suggest instability of these weighted estimates. It is possible that there is broad variance in Veterans’ mental health symptoms across tinnitus severity levels. However, the trends of increasing ORs as levels of tinnitus severity increase suggest a dose-response type pattern, which was consistent for all three mental health screens. Our ongoing work will continue to examine the complex interplay between tinnitus severity and Veterans’ mental health symptoms and disorders.
CONCLUSION
Mental health symptoms appear to be strongly associated with Veterans’ tinnitus severity. A better understanding of the relationships between these conditions may help improve the provision of interdisciplinary (Audiology and Mental Health) care for Service members and Veterans. Continued research in this area could help improve daily functioning and quality of life among Service members and Veterans who experience these disorders.
ACKNOWLEDGMENTS
We thank the participants for their help with this research and for their service to the U.S. military.
Contributor Information
Austin Prewitt, VA Health Services Research & Development Service Center of Innovation, Center to Improve Veteran Involvement in Care, VA Portland Health Care System (R&D 66), Portland, OR 97239, USA; Oregon Health and Science University – Portland State University School of Public Health, 3181 SW Sam Jackson Park Road (GH230), Oregon Health and Science University, Portland, OR 97239, USA.
Graham Harker, VA Health Services Research & Development Service Center of Innovation, Center to Improve Veteran Involvement in Care, VA Portland Health Care System (R&D 66), Portland, OR 97239, USA; Oregon Health and Science University – Portland State University School of Public Health, 3181 SW Sam Jackson Park Road (GH230), Oregon Health and Science University, Portland, OR 97239, USA.
Tess A Gilbert, VA Health Services Research & Development Service Center of Innovation, Center to Improve Veteran Involvement in Care, VA Portland Health Care System (R&D 66), Portland, OR 97239, USA.
Elizabeth Hooker, VA Health Services Research & Development Service Center of Innovation, Center to Improve Veteran Involvement in Care, VA Portland Health Care System (R&D 66), Portland, OR 97239, USA.
Maya E O’Neil, VA Health Services Research & Development Service Center of Innovation, Center to Improve Veteran Involvement in Care, VA Portland Health Care System (R&D 66), Portland, OR 97239, USA; VA Rehabilitation Research & Development Service, National Center for Rehabilitative Auditory Research, VA Portland Health Care System (P5-NCRAR),Portland, OR 97239, USA; Department of Psychiatry, School of Medicine, 3181 SW Sam Jackson Park Road (GH230), Oregon Health and Science University, Portland, OR 97239, USA; Department of Medical Informatics and Clinical Epidemiology, School of Medicine, 3181 SW Sam Jackson Park Road (BICC), Oregon Health & Science University, Portland, OR 97239, USA.
Kelly M Reavis, Oregon Health and Science University – Portland State University School of Public Health, 3181 SW Sam Jackson Park Road (GH230), Oregon Health and Science University, Portland, OR 97239, USA; VA Rehabilitation Research & Development Service, National Center for Rehabilitative Auditory Research, VA Portland Health Care System (P5-NCRAR),Portland, OR 97239, USA.
James A Henry, VA Rehabilitation Research & Development Service, National Center for Rehabilitative Auditory Research, VA Portland Health Care System (P5-NCRAR),Portland, OR 97239, USA; Department of Otolaryngology – Head & Neck Surgery, School of Medicine, 3181 SW Sam Jackson Park Road (PV01), Oregon Health & Science University, Portland, OR 97239, USA.
Kathleen F Carlson, VA Health Services Research & Development Service Center of Innovation, Center to Improve Veteran Involvement in Care, VA Portland Health Care System (R&D 66), Portland, OR 97239, USA; Oregon Health and Science University – Portland State University School of Public Health, 3181 SW Sam Jackson Park Road (GH230), Oregon Health and Science University, Portland, OR 97239, USA; VA Rehabilitation Research & Development Service, National Center for Rehabilitative Auditory Research, VA Portland Health Care System (P5-NCRAR),Portland, OR 97239, USA.
FUNDING
This research was supported by grants from the Veterans Health Administration, Office of Research and Development, Rehabilitation Research and Development Service (SPiRE 121 RX002216-01 to K.F.C.; C9427S to J.A.H.; and C9230C to M.P.F.). Support for this work was also received from the Oregon Clinical and Translational Research Institute at Oregon Health and Science University (1 UL1 RR024140 01).
REFERENCES
- 1. Jastreboff PJ: Phantom auditory perception (tinnitus): mechanisms of generation and perception. Neurosci Res 1990; 8(4): 221-54. [DOI] [PubMed] [Google Scholar]
- 2. Veterans Benefits Administration: VBA Annual Benefits Report Fiscal Year 2018 : U.S. Department of Veterans Affairs, 2018. Available at https://www.benefits.va.gov/REPORTS/abr/docs/2018-abr.pdf; accessed July 11, 2020.
- 3. Swan AA, Nelson JT, Swiger B, et al. : Prevalence of hearing loss and tinnitus in Iraq and Afghanistan veterans: a Chronic Effects of Neurotrauma Consortium study. Hear Res 2017; 349: 4-12. [DOI] [PubMed] [Google Scholar]
- 4. Henry JA, Griest SE, Blankenship C, et al. : Impact of tinnitus on military service members. Mil Med 2019; 184(1S): 604-14. [DOI] [PubMed] [Google Scholar]
- 5. Carlson KF, Gilbert TA, O’Neil ME, et al. : Health care utilization and mental health diagnoses among Veterans with tinnitus. Am J Audiol 2019; 28(1S): 181-90. [DOI] [PubMed] [Google Scholar]
- 6. Theodoroff SM, Lewis MS, Folmer RL, et al. : Hearing impairment and tinnitus: prevalence, risk factors, and outcomes in US Service members and Veterans deployed to the Iraq and Afghanistan wars. Epidemiol Rev 2015; 37: 71-85. [DOI] [PubMed] [Google Scholar]
- 7. Clifford RE, Baker D, Risbrough VB, Huang M, Yurgil KA: Impact of TBI, PTSD, and hearing loss on tinnitus progression in a US Marine cohort. Mil Med 2019; 184: 839-46. [DOI] [PubMed] [Google Scholar]
- 8. Helfer TM, Jordan NN, Lee RB, et al. : Noise-induced hearing injury and comorbidities among post deployment U.S. Army Soldiers: April 2003-June 2009. Am J Audiol 2011; 20(1): 33-41. [DOI] [PubMed] [Google Scholar]
- 9. Folmer RL, McMillan GP, Austin DF, Henry JA: Audiometric thresholds and prevalence of tinnitus among male Veterans in the United States: data from the national health and nutrition examination survey, 1999-2006. J Rehabil Res Dev 2011; 48(5): 503-16. [DOI] [PubMed] [Google Scholar]
- 10. Reavis KM, Henry JA, Marshall LM, Carlson KF: Prevalence of self-reported depression symptoms and perceived anxiety among community-dwelling U.S. Adults reporting tinnitus. Perspectives of the ASHA Special Interest Groups 2020; in press.
- 11. Trevis KJ, McLachlan NM, Wilson SJ: A systematic review and meta-analysis of psychological functioning in chronic tinnitus. Clin Psychol Rev 2018; 60: 62-86. [DOI] [PubMed] [Google Scholar]
- 12. Martinez-Devesa P, Perera R, Theodoulou M, et al. : Cognitive behavioral therapy for tinnitus. Cochrane Database Syst Rev 2010; 9: CD005233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Schmidt CJ, Kaelin C, Henselman L, et al. : Need for mental health providers in Progressive Tinnitus Management: a gap in clinical care. Fed Pract 2017; 34(5): 6-9. [PMC free article] [PubMed] [Google Scholar]
- 14. Carlson KF, Gilbert TA, Morasco BJ, et al. : Linkage of VA and state prescription drug monitoring program data to examine concurrent opioid and sedative-hypnotic prescriptions among Veterans. Health Serv Res 2018; 53(S3): 5285-308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Okie S: Traumatic brain injury in the war zone. N Eng J Med 2005; 352(20): 2043-7. [DOI] [PubMed] [Google Scholar]
- 16. Taylor BC, Hagel EM, Carlson KF, et al. : Prevalence and costs of co-occurring traumatic brain injury with and without psychiatric disturbance and pain among Afghanistan and Iraq War Veteran VA users. Med Care 2012; 50(4): 342-46. [DOI] [PubMed] [Google Scholar]
- 17. Dillman D: Mail and Internet Surveys: The Tailored Design Method. New York, NY, John Wiley and Sons, 2000. [Google Scholar]
- 18. U.S. Department of Veterans Affairs : A disability compensation website. Available at https://www.va.gov/disability/about-disability-ratings/; accessed July 11, 2020.
- 19. Meikle MB, Henry JA, Griest SE, et al. : The tinnitus functional index: development of a new clinical measure for chronic, intrusive tinnitus. Ear Hear 2012; 33(2): 153-76. [DOI] [PubMed] [Google Scholar]
- 20. Henry JA, Griest SE, Thielman E, McMillan G, Kaelin C, Carlson KF: Tinnitus functional index: development, validation, outcomes research, and clinical application. Hear Res 2016; 334: 58-64. [DOI] [PubMed] [Google Scholar]
- 21. Prins A, Ouimette P, Kimerling R, et al. : The primary care PTSD screen (PC-PTSD): development and operating characteristics. Primary Care Psychiatry 2003; 9(1): 9-14. [Google Scholar]
- 22. Zigmond AS, Snaith RP: The hospital anxiety and depression scale. Acta Psychiatr Scand 1983; 67(6): 361-70. [DOI] [PubMed] [Google Scholar]
- 23. Little R: Survey nonresponse adjustments for estimates of means. Int Stat Rev 1986; 54: 139e57. [Google Scholar]
- 24. Greenland S, Pearl J, Robins JM: Causal diagrams for epidemiologic research. Epidemiology 1999; 10(1): 37-48. [PubMed] [Google Scholar]
- 25. Fagelson MA: The association between tinnitus and posttraumatic stress disorder. Am J Audiol 2007; 16(2): 107-17. [DOI] [PubMed] [Google Scholar]
- 26. Moring JC, Peterson AL, Kanzler KE: Tinnitus, traumatic brain injury, and posttraumatic stress disorder in the military. Int J Behav Med 2018; 25(3): 312-21. [DOI] [PubMed] [Google Scholar]
- 27. Langguth B, Landgrebe M, Kleinjung T, et al. : Tinnitus and depression. World J Biol Psychiatry 2011; 12(7): 489-500. [DOI] [PubMed] [Google Scholar]
- 28. Pattyn T, Van Den Eede F, Vanneste S, et al. : Tinnitus and anxiety disorders: a review. Hear Res 2016; 333: 255-65. [DOI] [PubMed] [Google Scholar]
- 29. Edmonds CM, Ribbe C, Thielman EJ, Henry JA: Progressive tinnitus management level 3 skills education: a 5-year clinical retrospective. Am J Audiol 2017; 26(3): 242-50. [DOI] [PubMed] [Google Scholar]
- 30. Beck JE, Zaugg TL, Egge JL, Lima EN, Thielman EJ: Progressive tinnitus management at two Veterans Affairs medical centers: clinical implementation with modified protocols. Am J Audiol 2019; 28(1S): 162-73. [DOI] [PubMed] [Google Scholar]
- 31. Henry JA, Thielman EJ, Zaugg TL, et al. : Randomized controlled trial in clinical settings to evaluation effectiveness of coping skills education used with progressive tinnitus management. J Speech Lang Hear Res 2017; 60(5): 1378-97. [DOI] [PubMed] [Google Scholar]
- 32. Henry JA, Thielman EJ, Zaugg TL, et al. : Telephone-based progressive tinnitus management for persons with and without traumatic brain injury: a randomized controlled trial. Ear Hear 2019; 40(2): 227-42. [DOI] [PubMed] [Google Scholar]
- 33. Tuepker A, Elnitsky C, Newell S, Zaugg T, Henry JA: A qualitative study of implementation and adaptations to Progressive Tinnitus Management (PTM) delivery. PLoS One 2018; 13(5): e0196105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Henry JA, Zaugg TL, Myers PJ, Schechter MA: The role of audiologic evaluation in progressive audiologic tinnitus management. Trends Amplif 2008; 12(3): 170-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bhatt JM, Lin HW, Bhattacharyya N: Prevalence, severity, exposures, and treatment patterns of tinnitus in the United States. JAMA Otolaryngol Head Neck Surg 2016; 142(10): 959-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hoover EC, Souza PE, Gallun FJ: Competing views on abnormal auditory results after mild traumatic brain injury. SIG-6 Perspect Hear Hear Dis Res Diagn 2015; 19(1): 12-21. [Google Scholar]


