Introduction
Tracheal cartilaginous sleeve (TCS), a tube of tracheal cartilage formed by vertical fusion of tracheal rings, is associated with syndromic forms of craniosynostosis.1,2 These syndromes have significant morbidity and mortality alone, and TCS incurs a 90% mortality risk by two years of age without tracheostomy from restricted growth of the fused tracheal rings compared to the child resulting in a stenotic airway.2 We report the case of a patient with severe Apert syndrome with class IV3 TCS extending from the thyroid cartilage to the distal bronchi with long-segment stenosis treated with cervicothoracic slide tracheoplasty. This report was exempt from internal review board analysis and written parental consent was obtained prior to publication.
Case Report
A two-month-old female with Apert syndrome (FGFR2 c.755C>G, p.Ser252Trp) presented to clinic for multi-suture craniosynostosis, cleft palate, and midnasal stenosis. Over the next four months she had multiple admissions for viral-associated respiratory distress prompting nasal stenosis repair and grade 3 subglottic stenosis (SGS) was identified.
Following this, she remained intubated for two weeks with a viral infection before undergoing elective tracheostomy. TCS was identified from the thyroid cartilage extending inferiorly beyond the surgical field. Tracheotomy location was approximated at the 2nd to 3rd tracheal rings using transillumination from a flexible endoscope inside the endotracheal tube. The abnormally thick cartilage was addressed with a stellate tracheotomy. After tracheostomy, she had difficulty ventilating and flexible laryngoscopy found the tube within a posterolateral midtracheal diverticulum prompting exchange for a shorter tube.
Over six months she had intermittent occlusions and multiple decannulations. She developed posterior tracheal ulcers and recurrent Pseudomonas-associated tracheitis and returned to the operating room six times for tracheostomy exchanges and subglottic dilation. Her SGS progressed to grade 4, and the TCS was found extending into the bilateral bronchi.
Seven months after tracheostomy, revision tracheostomy was performed to move her stoma superiorly. This resolved the recurrent occlusions, yet she remained in critical condition with chronic CO2 retention. Four-dimensional CT identified right main bronchus adynamic narrowing and severe kyphosis with C2-T12 spinal fusion. Slide tracheoplasty was discussed along with the significant mortality risk given the TCS severity, multi-level airway obstruction, and chronic tracheitis. Despite the risks, the family elected to pursue open reconstruction.
The otolaryngology and cardiothoracic surgery teams planned the procedure using 3D-printed models of the patient’s trachea. Model tracheas allowed for optimal incision planning for airway expansion and provided an opportunity to practice suturing anastomoses (Supplemental Video).
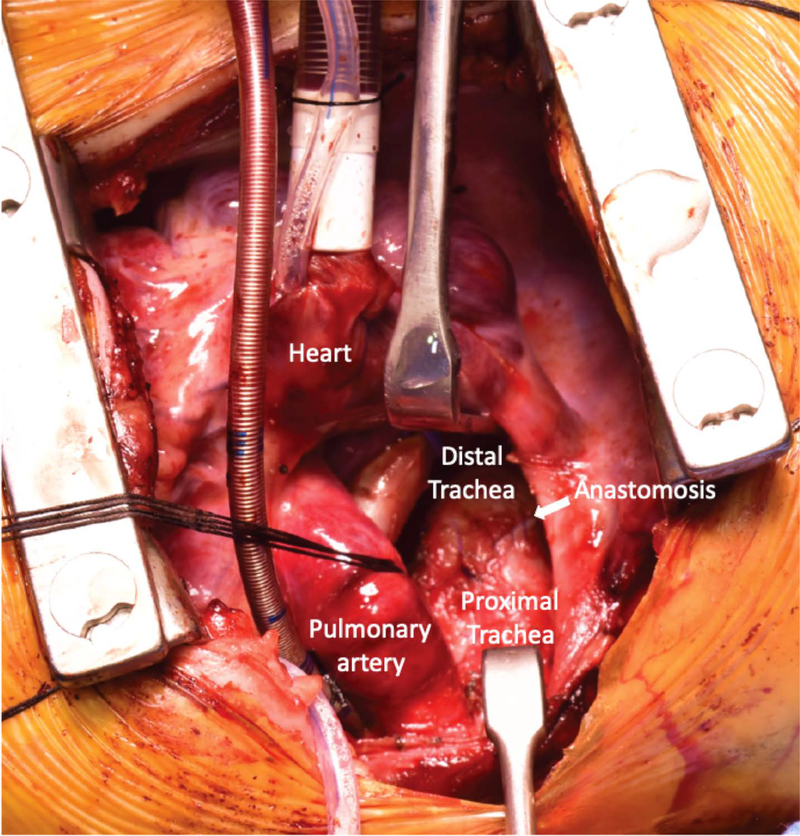
Surgery was performed at age 21-months. Following direct laryngoscopy and bronchoscopy with subglottic balloon dilation, she was nasotracheally intubated and the tracheostomy closed. The thoracic surgery team performed a sternotomy and mediastinal dissection to expose the cervical trachea to the mainstem bronchi and cardiopulmonary bypass initiated. The distal trachea was divided transversely and incised longitudinally along the left lateral proximal trachea segment and the right lateral right main bronchus to facilitate a side-to-side slide tracheoplasty. Cartilage contouring was required to approximate the abnormally thick cartilaginous segments into a tight closure. The anastomosis was closed with running 5–0 PDS and fibrin sealant (Fig. 1). Endotracheal tube position was endoscopically confirmed, the patient was removed from bypass, and the chest closed (Supplemental Video).
Figure 1:
Intraoperative photo of completed anastomosis following cervicothoracic side-to-side slide tracheoplasty for stenotic class IV tracheal cartilaginous sleeve.
Following reconstruction, she remained intubated and paralyzed for one week with humidification, inhaled tobramycin, and piperacillin/tazobactam. Her tracheostomy tube was replaced one week postoperatively to accommodate ventilation requirements and bypass the SGS, and the anastomosis was intact. She developed Pseudomonas tracheitis and restarted broad-spectrum antibiotics. One month postoperatively, bronchoscopy revealed anterior tracheal anastomosis dehiscence (Fig. 2). This healed into a fibrotic plaque over four months without surgical intervention. She transferred out of the ICU but requires ventilator support for restrictive lung disease due to spinal fusions with persistent tracheal ulcerations despite multiple custom tubes. Ultimately, she’s done well, recently undergoing syndactyly release and awaits spine surgery.
Figure 2:
Endoscopic photo of anterior tracheal anastomosis dehiscence into the anterior mediastinum found on routine endoscopy one-month postoperatively.
Discussion
Recent reports estimate the prevalence of TCS in craniosynostosis syndromes at 22–29%, and for patients requiring operative airway evaluation prevalence increases to 60–80%.1,4 Diagnosis is difficult with endoscopy alone and often not fully appreciated until tracheostomy.
TCS survivability improves with tracheostomy, however subsequent airway interventions are not outlined.2,5 Tracheostomy for TCS is fraught with complications including challenging placement, granulation tissue, recurrent obstruction, and rarely death.2 Airway reconstruction via cervicothoracic slide tracheoplasty presents a potential option for patients with severe TCS, although we expect significantly increased mortality risk due to the complex patient population and comorbidities.
Supplementary Material
Acknowledgements
The authors would like to acknowledge S. Friedman, Ph.D., for his assistance in 3D planning and printing for this case, E. R. Gallagher, M.D., M.P.H., J. Roberts, M.D., and A. Striegl, M.D. for their expertise in Apert syndrome and care of this patient, S. Parikh, M.D., and J.P. Dahl, M.D., Ph.D., M.B.A., for their insight into complex airway management and helpful discussions, and V. Masco for assistance in figure and video preparation. K.Z. was supported by F32 HL147398-01 from the National Heart, Lung, and Blood Institute during preparation of this manuscript.
Footnotes
Presentations: This case has not previously been presented.
References
- 1.Wenger TL, Dahl J, Bhoj EJ, et al. Tracheal cartilaginous sleeves in children with syndromic craniosynostosis. Genetics in medicine : official journal of the American College of Medical Genetics. 2017;19(1):62–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lertsburapa K, Schroeder JW, Jr.,., Sullivan C. Tracheal cartilaginous sleeve in patients with craniosynostosis syndromes: a meta-analysis. Journal of pediatric surgery. 2010;45(7):1438–1444. [DOI] [PubMed] [Google Scholar]
- 3.Noorily MR, Farmer DL, Belenky WM, Philippart AI. Congenital tracheal anomalies in the craniosynostosis syndromes. Journal of pediatric surgery. 1999;34(6):1036–1039. [DOI] [PubMed] [Google Scholar]
- 4.Pickrell BB, Meaike JD, Canadas KT, Chandy BM, Buchanan EP. Tracheal Cartilaginous Sleeve in Syndromic Craniosynostosis: An Underrecognized Source of Significant Morbidity and Mortality. The Journal of craniofacial surgery. 2017;28(3):696–699. [DOI] [PubMed] [Google Scholar]
- 5.Hamilton J, Clement WA, Kubba H. Management of congenital cartilaginous sleeve trachea in children. Int J Pediatr Otorhinolaryngol. 2014;78(11):2011–2014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.