Abstract
Background
As SARS-CoV-2 continues to spread, a thorough characterisation of healthcare needs and patient outcomes, and how they have changed over time, is essential to inform planning.
Methods
We developed a probabilistic framework to analyse detailed patient trajectories from 198,846 hospitalisations in France during the first nine months of the pandemic. Our model accounts for the varying age- and sex- distribution of patients, and explore changes in outcome probabilities as well as length of stay.
Findings
We found that there were marked changes in the age and sex of hospitalisations over the study period. In particular, the proportion of hospitalised individuals that were >80y varied between 27% and 48% over the course of the epidemic, and was lowest during the inter-peak period. The probability of hospitalised patients entering ICU dropped from 0·25 (0·24–0·26) to 0·13 (0·12–0·14) over the four first months as case numbers fell, before rising to 0·19 (0·19–0·20) during the second wave. The probability of death followed a similar trajectory, falling from 0·25 (0·24–0·26) to 0·10 (0·09–0·11) after the first wave before increasing again during the second wave to 0·19 (0·18–0·19). Overall, we find both the probability of death and the probability of entering ICU were significantly correlated with COVID-19 ICU occupancy.
Interpretation
There are large scale trends in patients outcomes by age, sex and over time. These need to be considered in ongoing healthcare planning efforts.
Funding
INCEPTION.
Research in context.
Evidence before this study
As the SARS-CoV-2 epidemic continues to resurge in many places, we need a detailed understanding of healthcare needs and patient outcomes to inform planning. However, it remains difficult to build a coherent picture of hospital patient pathways given the huge diversity seen in these pathways in a situation when both COVID-19 epidemiology and clinical care evolved very quickly. We searched PubMed, medRxiv and GoogleScholar for studies that were investigating hospital patient outcomes over time, published between 1 January and 1 December. We found three studies that shown a drop in-hospital mortality over the course of the pandemic, but analysed retrospectively relatively limited or specific datasets (e.g. only ICU patients), and did not provide age- and sex- specific estimates. None looked at the evolution of mortality over several epidemic waves.
Added value of this study
Here we analysed detailed individual patient trajectories from 198,846 hospitalisations from March to November 2020 in France. Our framework is able to monitor in-hospital mortality in real-time, accounting for delays and censoring. We identify shifting age and sex profiles of hospitalised patients as well as large scale fluctuations in patient mortality across all age groups as the endemic has progressed.
Implications of all the available evidence
These findings shed new light on the evolution of outcomes over multiple epidemic waves, as well as the possible underlying causes. It also provides an evidence base for understanding current and future healthcare needs.
Alt-text: Unlabelled box
1. Introduction
The rapid nature of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spread placed unprecedented strain on healthcare facilities around the world. Many countries enforced restrictions to avoid their healthcare system from being overwhelmed [1,2]. Accurate projections of healthcare needs can help plan the pressure on the healthcare system, try to prevent them from reaching capacity and ensure they are well equipped to deal with increasing demand [3], [4], [5]. We thus need a robust understanding of pathways patients take at hospital, including the duration of hospital stays and need for intensive care treatment, and how this changed over the course of the pandemic. The mass of patient data gathered in countries that have experienced large pandemic waves can provide invaluable insight on these parameters. This is the case of France, which has experienced two large epidemic peaks in the nine-month period since the virus was first detected in the country.
It remains difficult to build a coherent picture of hospital patient pathways given the huge diversity seen in these pathways in a situation when both COVID-19 epidemiology and clinical care evolved very quickly. First, outcomes of hospitalisation for SARS-CoV-2 infection range from limited symptoms allowing immediate discharge, death within a few hours to weeks spent in ICU and can vary substantially with the age and sex of the patient [6,7]. Second, the age, sex and severity profile of hospitalised patients may have changed during the course of the pandemic along with the intensity of control measures and the multiple parameters influencing healthcare seeking patterns and decisions to admit them to hospital. Finally, improvements in clinical care may also have modified outcomes as clinicians progressively learned to manage COVID-19 patients, including through new treatment strategies [8].
Early studies describing hospital outcomes and trajectories have considered short periods of the pandemic, considered outcomes as constant over time, not considered age- and sex- specific differences in both outcomes and length of stay or ignored the fact that many currently hospitalized individuals are yet to have their outcome [9], [10], [11], [12], [13], [14], [15], [16], [17], [18]. More recently, studies have shown substantial improvement in hospital mortality over the first epidemic wave in the UK and in the US [11], [12], [13]. Those changes were not fully explained by clinical and demographic factors. Hypothesis for these drops include changing patient severity, increasing clinical experience, decreasing hospital volume, use of new treatments, nonpharmacologic treatments, earlier intervention, and community awareness. Thus, it remained unclear whether patient outcome did really improve, or if the drop seen was an artefact due to less severe patients entering hospitals.
Here, we aim to shed a new light on the evolution of in-hospital mortality through the analysis of 9 months of data, which include the first and second 2020 epidemic wave in France. Our goal consists in two key points: (i) assessing changes in patient outcomes over the course of the pandemic in France, and (ii) providing detailed age- and sex- specific estimates of those outcomes, to help inform health-care planning. Using data from a dedicated COVID-19 surveillance system that was rapidly integrated into all French hospitals, we characterise the complex hospital pathways of COVID-19 patients . We reconstruct full patient trajectories from first admission to eventual discharge or death with details on the attended wards (conventional or ICU) and develop a modelling framework that explicitly accounts for the heterogeneous nature of the changing profile of patients being admitted into hospitals and censoring. Through our approach, we can disentangle the relative contributions of patient characteristics (e.g. age and sex) in assessing whether improvements have occurred in outcome over the course of the epidemic. The study also provides a detailed account of the way the French healthcare system coped with an unprecedented wave of hospitalisations during this unique crisis in French history.
2. Methods
2.1. Data
We used a linelist of hospitalised patients from the SI-VIC database who started their hospitalisation between 13 March and 30 November 2020 (Fig. 1). It includes 198,846 patients, from 1763 different healthcare structures, across metropolitan France. This database is designed to be exhaustive for hospitalisations in general ward and ICU: any healthcare structure (public and private) in charge of a SARS-CoV-2 positive patient must declare the patient in SI-VIC. No medical data is recorded in SI-VIC, with the exception of information on the type of medical care structure (ward). The system thus contains administrative information on the patient's journey through the health system (date of hospitalisation, details on the attended wards, outcome (discharge or death) and region) and minimal information on the patient (age, sex and place of residence). The deployment of SI-VIC was authorized by an Institutional Board (CNIL, Commission Nationale Informatique et Libertés). No consent of the patients is required, and the patients must be informed of their right to access, modify, rectify and delete any data concerning them. We worked on an anonymized version of the dataset, with each patient having only an ID number. Further details about the administrative nature of the dataset can be found in the SI appendix.
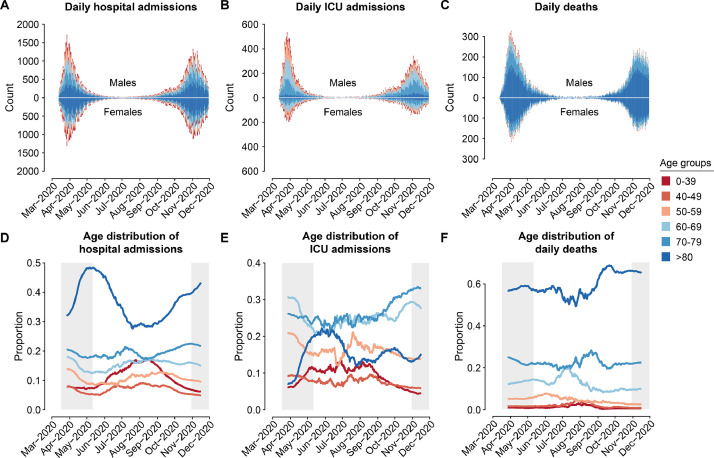
Fig. 1.
Hospitalisation, ICU and death data.
A. Daily number of hospital admissions, as a function of time. B. Daily number of ICU admissions, as a function of time. C. Daily number of deaths, as a function of time. In each panel, males counts are shown at the top, females counts are shown at the bottom. D. Age distribution of hospital admissions, as a function of time. E. Age distribution of ICU admissions, as a function of time. F. Age distribution of deaths, as a function of time. Distributions are computed on rolling 28-day windows. Colours represent the age group. Shaded areas on the bottom represent the lockdown periods in France (17 March - 11 May and 30 October - 15 December).
2.2. Modelling delays and probabilities of ICU admission, death and discharge
We consider that all patients are initially admitted to hospital. Patients can then be admitted into ICU, die without entering ICU, or be discharged (Fig. S1). Patients who are admitted to ICU can subsequently either die or be discharged. We let the probabilities of ICU admission, death within ICU, death outside ICU, discharge from ICU and discharge without entry into ICU vary by age (0–39, 40–49, 50–59, 60–69, 70–79, 80+) and sex. Given the small number of patients in younger age groups, we let the delays between admission and outcome vary by age, on a restricted number of age groups (0–59, 60–69, 70–79, 80+) and by sex. In initial analyses, we found that the delays from hospitalisation to ICU admission or death did not differ substantially by age and sex, and so we used a single delay distribution from hospitalisation to ICU, and one delay distribution from hospitalisation to death across all individuals (irrespective of age or sex).
We modelled the delay from hospitalisation to ICU using a zero-inflated exponential distribution (Fig. S2A). For the delay from hospitalisation to death (hospital discharge, respectively) we used a mixture distribution composed of an exponential distribution for those that die (are discharged from hospital, respectively) within a short delay and a lognormal distribution for those that die (are discharged from hospital, respectively) after longer delays (Fig. S2B) [19]. The delays from ICU to death and hospital discharge were modelled using a lognormal distribution [10,20]. We also considered a gamma distribution as a sensitivity analysis. To model more realistically the delays, we truncated all the distributions to 120 days [9,20], which affected 762 patients (out of 198,846). Further details can be found in the SI appendix.
3. Parameter estimation
We used a probabilistic framework based on competing risk models with cause-specific relative hazards [21], [22], [23]. We specifically accounted for censoring by incorporating into the likelihood not only patients with outcomes (i.e. ICU admission, death, discharge) but also patients without any known outcome by the end of the dataset (30th November). We make use of individual data to jointly estimate the different probabilities and delays, which let us account for the varying age and sex profiles of patients.
Briefly, we write the likelihood , given each event that can occur to each patient after hospital admission, of the event probability and the delay distribution (Fig. S1). Each individual can go through multiple events, the contribution of each individual to the likelihood is then the product of the likelihood of each event . The total likelihood then becomes:
where denotes the set of parameters (outcome probabilities and delays). Further details on the framework can be found in the SI appendix.
We use the Rstan package [24] to fit the parameters. We use 2·5 and 97·5 quantiles from the resulting posterior distributions for 95% credible intervals of the parameters. The presented probabilities are an average of the age- and sex- specific estimates, weighted by the proportion of the population that are of that age and sex.
4. Estimation of changes over time
To investigate changes in outcome probabilities during the course of the epidemic, we partitioned the epidemic into ten time periods: T1: 13 March - 1 April; T2: 2 April - 21 April; T3: 22 April - 11 May; T4: 12 May - 31 May; T5: 1 June - 30 June, T6: 1 July - 31 July, T7: 1 August - 31 August, T8: 1 September - 30 September, T9: 1 October - 31 October, T10: 1 November - 30 November. The first four periods lasted 20 days (first epidemic wave) and the following ones lasted 1 month (30 to 31 days). This approach allowed us to track changes over the course of the epidemic where parameter estimates are independent across time periods. It also allowed us to explore specific changes from the beginning of the first wave up to the second wave, including during the two lockdown periods (13 March - 11 May 2020 and 30 October-15 December 2020).
We used the percentage of ICU occupancy by COVID-19 patients as a proxy to monitor the pressure on the healthcare system. This percentage is computed as the number of COVID-19 patients in ICU, divided by the initial total number of ICU beds available in France (5664 beds, source: DGOS). Correlation was computed using Pearson's correlation test.
4.1. Simulation study
To evaluate the capacity of our inferential framework to correctly estimate parameters, we developed a simulation framework where both the delays and the probabilities of outcomes were known. We assessed the performance of the model on both a fixed and a varying risk over time, as well as a fixed and a varying delay from admission to death. Further details of the simulation study can be found in the SI appendix.
4.2. Role of the funding source
The funders had no role in the data analysis, interpretation, writing of the report, or in the decision to submit the paper for publication.
5. Results
Over the first nine months of the epidemic (13 March - 30 November 2020), there were 198,846 hospitalisations (mean age 69), of which 35,818 were admitted to ICU (mean age 64) and 33,269 died (mean age 80) (Fig. 1). Only 25% of deaths were in individuals that entered ICU (Fig. S3). Seventy three percent of the deaths among patients that did not enter ICU were aged >80y, whereas only 24% of deaths among those admitted to ICU were in the oldest age group (Fig. S4).
The age and sex profiles of hospitalised patients changed over the course of the pandemic wave. In particular, the proportion of hospitalised individuals that were >80y varied between 27% during the summer 2020 and 48% at the peak of the first wave. There were also large fluctuations in the proportion of the patient population that was <40y, going from 8% at the start of the epidemic to 17% during the summer, and decreasing again to 6% at the end of November (Fig. 1D). The proportion of hospitalised cases that were female increased from 45% to 53% during the spring before returning to 48% by the end of November (Fig. S5). The age and sex distribution of those entering ICU also changed, contrasting with those that died, which remained approximately stable (Figs. 1E,F and S2B-C).
5.1. Probabilities of different outcomes over the course of the pandemic
Using our model and adjusting by age and sex, we found that overall 18·2% (18·0–18·4) of patients entered ICU (Fig. 2A, Table S1) and 19·7% (19·5–20·0) died (Fig. 2D, Table S1). Of patients who do not enter ICU, 14·9% (14·6–15·1) died, ranging from 0·4% (0·2–0·6) in females under 40 years old to 36·3% (35·5–37·1) in males older than 80 years old (Fig. 2B, Table S2). Among patients admitted to ICU, on average 31·2% (30·4–32·2) died, ranging from 7·8% (6·4–9·4) in patients under 40 years old to 46·8% (44·6–49·1) in patients over 80 years old, with limited difference by sex (relative risk: 1·0 [0·8–1·4]) (Fig. 2C, Table S2).
Fig. 2.
Probabilities of ICU admission and death.
A. Probability of ICU admission given hospitalisation, as a function of age. B. Probability of death given hospitalisation and no ICU admission, as a function of age. C. Probability of death given ICU admission, as a function of age. D. Overall probability of death given hospitalisation, irrespective of ICU admission, as a function of age. Probabilities are computed as a weighted average on the period from March to November 2020. Females are shown in red, males in blue. The horizontal lines and shaded areas represent the overall mean across all ages and sexes. The boxplots represent the 2.5, 25, 50, 75, and 97.5 percentiles of the posterior distributions. .
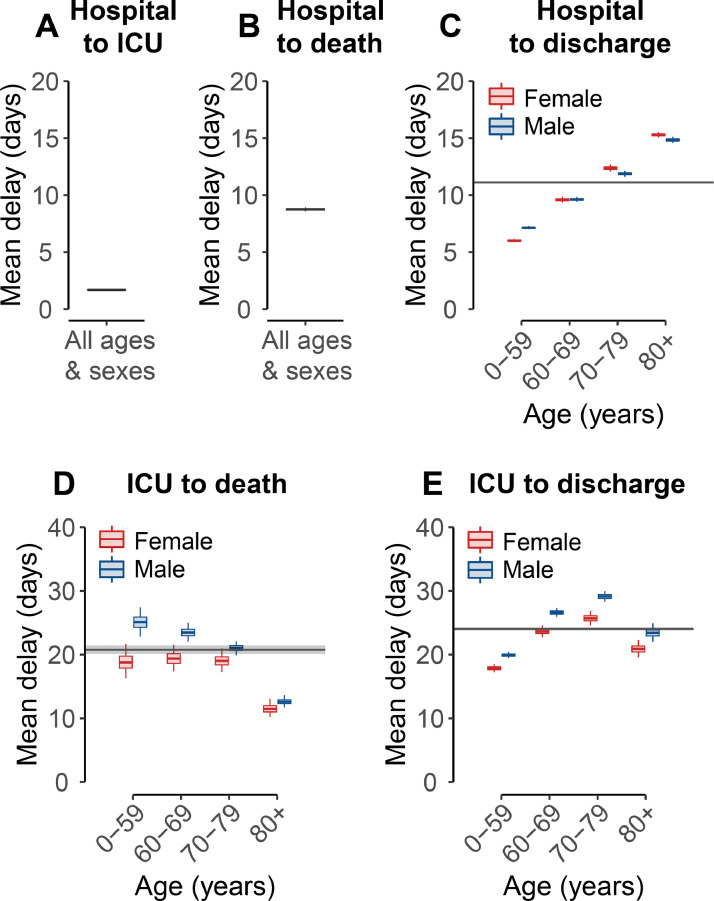
We characterised how delays between hospitalisation and outcomes varied according to the age and sex of patients, as well as the outcome considered. The delay from hospitalisation to ICU admission was short, with a mean delay of 1·7 days (1·6–1·7) (Fig. 3A, Table S3) [19], and was stable across age and sex (Fig. S6). For patients that did not enter ICU, the delay between hospitalisation and death also did not vary by age or sex (mean: 10·6 days [10·4–10·8], Fig. 3B-S6), whereas the delay from hospitalisation to discharge did (Fig. 3C). The delay between ICU admission and death was longer for males and shorter for older patients, ranging from 25·1 days (22·8–27·4) in males <60 years old to 11·5 days (10·2–13·1) in females >80 years old (Fig. 3D, Table S4). Further, the delay from ICU admission to outcome depended on whether the patient died (mean: 20·8 days [20·1–21·5]) or was discharged (mean: 24·0 days [23·8–24·4]) (Fig. 3D-E, Table S4–5).
Fig. 3.
Mean delays to ICU admission, death and hospital discharge.
A. Mean delay from hospitalisation to ICU admission B. Mean delay from hospitalisation to death, given that the patient was not admitted in ICU. C. Mean delay from hospitalisation to hospital discharge, given that the patient was not admitted in ICU, as a function of age. D. Mean delay from ICU admission to death, as a function of age. E. Mean delay from ICU admission to hospital discharge, as a function of age and sex. Means are computed as a weighted average on the period from March to November 2020. Parameters characterising delay distributions are given in Tables S3–5. The horizontal lines and shaded areas represent the overall mean across all ages and sexes. Females are shown in red, males in blue. The boxplots represent the 2.5, 25, 50, 75, and 97.5 percentiles of the posterior distributions.
We found that many individuals had their outcomes within a day of hospitalisation. We estimated that 5·7% (5·6–5·8) of all hospitalised deaths occurred within a day of admittance. Similarly 8·3% (7·9–8·6) of all discharges, and 61·3% (60·8–61·8) of all ICU admittances occurred within the first day of hospitalisation (Fig. S7). The proportion of hospitalised deaths that occurred quickly changed substantially during the study period, with a large drop at the end of the summer (Fig. S8, Table S6).
5.2. Changes in outcomes over the course of the epidemic
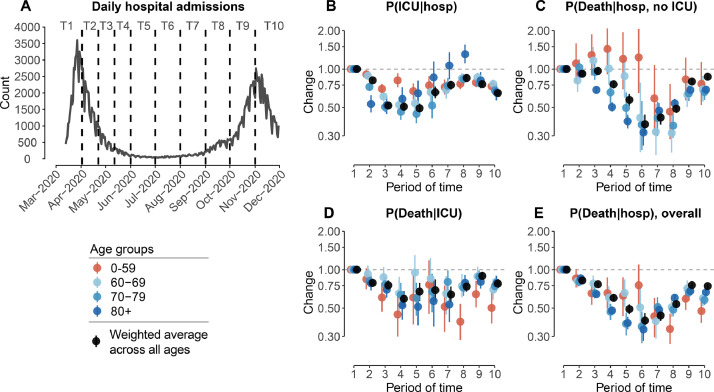
We found that the probability of entering ICU fell at the beginning of April across all age groups, but especially in those >60y in age (Fig. 4B, Table S7). At the beginning of the summer, the probability of entering ICU was 0·49 (0·45–0·54) times that at the start of the epidemic (25·4% [24·4–26·4] at the start compared to 12·6% [11·6–13·6] in June 2020). However, we observed that the probability of entering ICU rose again from July 2020, especially in those aged >80 years. By the end of November 2020, it was 0·65 (0·62–0·68) times that at the start of the epidemic.
Fig. 4.
Changes in probabilities of ICU admission and death.
A. Daily number of hospital admissions as a function of time, from 13th March to 30th June 2020. Dashed lines denote the different windows of time (named T1-T5) used to estimate the changes in probabilities. B. Changes in probability of ICU admission given hospitalization, as a function of time. C. Changes in probability of death given hospitalization and no ICU admission, as a function of time. D. Changes in probability of death given ICU admission, as a function of time. E. Changes in overall probability of death given hospitalization, as a function of time. We divide the epidemic into different periods of time: T1: 13 March - 1 April; T2: 2 April - 21 April; T3: 22 April - 11 May; T4: 12 May - 31 May; T5: 1 June - 30 June, T6: 1 July - 31 July, T7: 1 August - 31 August, T8: 1 September - 30 September, T9: 1 October - 31 October, T10: 1 November - 30 November. All changes are weighted by the proportion of patients that are of each sex. Changes are computed relatively to T1 (reference), estimates are presented in Tables S7–10. The dots and lines represent 2.5, 50 and 97.5 percentiles of the posterior distributions.
There was also a significant decrease in the probability of death during the first wave [11], [12], [13]. Among those that were not admitted into ICU, the overall probability of death fell from 16·4% (15·6–17·1) in the earliest time window to 6·1% (5·1–7·1) by the end of the first wave (Fig. 4C, Table S8). However, we observed that since the summer, the probability of death rose again to 14·2% (13·9–14·6). Among those that were admitted into ICU, the overall probability of death fell, down from 34·1% (32·0–36·2) in the earliest time window to 23·4% (19·1–28·1) by the end of the first wave (Fig. 4D, Table S9), before increasing again during the second wave to 30·1% (28·9–31·3). Among all deaths, the proportion occurring in ICU also varied over the two pandemic waves. We estimated that this proportion was low during the peaks of the waves (1st peak: 22·5% [19·5–25·9], 2nd peak: 22·3% [21·3–23·3]), and higher during the summer (38·4% [37·2–41·5] in August 2020) (Table S10).
Overall, the probability of death among hospitalised patients (combining those that entered ICU with those that did not) fell steadily throughout the first wave and across all age groups (Fig. 4E, Table S11). In July 2020, the overall probability of death was 0·40 (0·35–0·46) times that of the first time period (24·9% [24·0–25·9] vs 10·0% [8·7–11·3]). However, the probability of death rose during the second wave of the epidemic, across all age groups except in patients <60 years of age. In November, the overall probability of death was 0·74 times (0·71–0·78) that of the beginning of the pandemic (24·9% [24·0–25·9] vs 18·6% [18·1,19·0]). These trends in patient outcomes were of the same magnitude in males and females (Fig. S9).
5.3. Changes in the delay distributions over the course of the pandemic
We investigated how the delay between hospital admission and outcomes has varied over the epidemic (Fig. S10, Table S12). The delay from hospitalisation to ICU admission remained stable over the 9 months. For patients not admitted in ICU, the delay from hospitalisation to death decreased over the first epidemic wave from 10·2 days (9·6–10·9) to 9·1 days (8·8–9·5), but then increased to 13·4 days (12·6–14·3) by September 2020. The delay from hospital admission to discharge remained stable for patients <60 years in age, but fluctuated for older patients. It first decreased over the first epidemic wave from 14·4 days (13·9–15·2) to 13·1 days (12·7,13·6), and then increased again to return near the original delay. We observed similar trends for patients admitted in ICU.
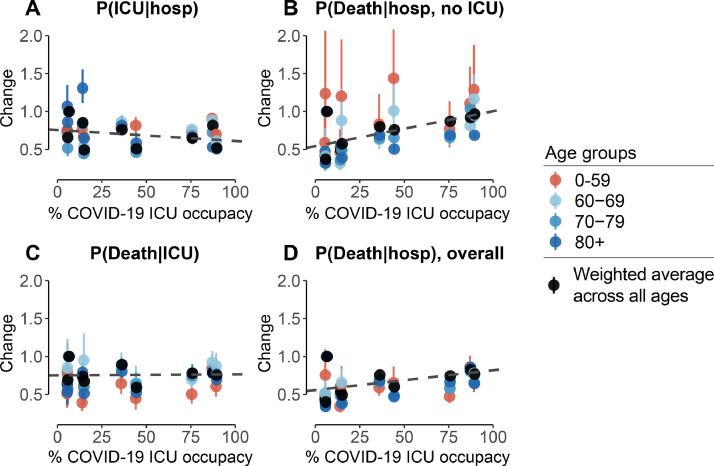
5.4. Correlation between changes and hospital occupancy
We used the percentage of ICU occupancy by COVID-19 patients as a proxy to monitor the pressure on the healthcare system. We observed a significant negative correlation between COVID-19 ICU occupancy and the probability of being admitted to ICU (Correlation[Cor]: −0·32 [−0·57,−0·01]), as well as a significant positive correlation with the mortality outside ICU (Cor: 0·39 [0·09,0·62]) (Fig. 5A and B). We found no significant correlation between COVID-19 ICU occupancy and mortality within ICU (Cor: 0·02 [−0·29,0·33]) or with overall mortality (Cor: 0·24 [−0·07,0·52]) (Fig. 5C and D).
Fig. 5.
Correlation between changes in outcome probabilities and COVID-19 ICU occupancy.
A. Changes in probability of ICU admission given hospitalization, as a function of COVID-19 ICU occupancy. B. Changes in probability of death given hospitalization and no ICU admission, as a function of COVID-19 ICU occupancy. C. Changes in probability of death given ICU admission, as a function of COVID-19 ICU occupancy. D. Changes in overall probability of death given hospitalization, as a function of ICU occupancy. The COVID-19 ICU occupancy corresponds to the mean occupancy of ICU by COVID-19 patients on each time period. All changes are weighted by the proportion that are of each sex. The dashed line represents the average trend (linear fit). .
5.5. Pathways to recovery or death
Of individuals that enter ICU that ultimately die, only 8·4% exited ICU back to general hospital wards before dying. In contrast, among ICU patients that are ultimately discharged, 72·0% went back to general hospital wards. On average, discharged ICU patients spent 15·4 days (15·2–15·6) in ICU, representing 64% of their total time after being admitted into ICU and 8·6 days (8·5–8·7) in post-ICU general wards. Patients that ultimately died spent on average 19·1 days (92%, 95%CI: 18·4–19·7) in ICU and 1·7 days (95%CI: 1·7–1·8) in post-ICU general wards (Table S13). Finally, while in this study we considered that exiting general wards constitutes a hospital discharge, 18·5% of ICU patients (but only 2·1% of all patients) needed long-term care and rehabilitation care.
5.6. Model performance
In a simulation study, we demonstrated that our modelling framework was able to correctly identify known delays and outcome probabilities in real-time, accounting for censoring (Figs. S11–14).
6. Discussion
We have used a large detailed dataset of hospitalised COVID-19 cases to track patient trajectories over the course of two 2020 pandemic waves in France. Our framework provides a robust approach to incorporate evolving profiles of patients over the course of the epidemic and capture changes in their outcome. We observe that while there was a large reduction in both the probability of entering ICU and the probability of dying among hospitalised individuals, these improvements were partly reversed as case numbers began to rise again. These effects were observed across age groups and could not be explained by the variations in age- and sex- profiles of patients over the course of the epidemic.
There are likely to be multiple underlying reasons for the substantial changes in outcomes among hospitalised individuals as the epidemic has progressed. First, increasing clinical experience is likely to have played an important part as clinicians quickly shared knowledge and experience. Second, improved care might have played a role as the pathophysiology of COVID-19 started to become better understood. For example, improved understanding of the key role of inflammation [25] resulted in increasing use of immunomodulatory drugs, and in particular corticosteroids (e.g. dexamethasone [8]). However, observed improvements in patients outcomes partly reversed as case numbers rose during the second wave. This suggests a substantial part of the initial improvements was due to the hospitalisation of less severe cases during the inter-peak period or reduced strains on the healthcare system. Other efforts in the US and the UK that have identified improvements in patient outcomes have so far only considered the first wave (Fig. S15) [11], [12], [13]. We expect that these improvements will be partly reversed once the growth in cases during the second peak is considered. Nonetheless we show that, despite the new rise, overall hospital mortality is still lower than at the start of the epidemic.
We found that only a minority of deaths occur in ICU. This suggests that many of the patients that are at highest risk of death are never transferred to ICU. Consistent with this observation we found that the proportion of patients that enter ICU is very low among those older than 70 years of age. This reflects the fact that older patients may not be transferred to ICU when they are too fragile to undergo such treatments [26]. Moreover we found that the proportion of death occurring in ICU greatly varied during the pandemic, with this proportion being at its lowest at the peaks of the waves, pointing to large variations in healthcare practices across the epidemic waves.
Overall, we find substantial heterogeneity exists in the time between hospitalisation and death. There has been a growing realisation that the disease can manifest in different ways, even between ultimately fatal cases [7,27]. The reasons for this remain unclear, although a role for host immune response, comorbidities, alongside age and sex differences appear key [29]. We note that the proportion of deaths that occurred within a day of hospitalisation dropped over the summer. It remains unclear if this drop is due to a changing profile of patients, or changes in hospital reporting practices. In a sensitivity analysis, we excluded all individuals that had an outcome (discharge or death) within a day of hospitalisation, with largely unchanged probabilities of the different outcomes (Fig. S16).
Among those that survive infection, the pathways individuals take to recovery can be long and complex. While we only considered the time to death or hospital discharge once entering ICU, the proportion of time actually spent in ICU can vary substantially and depends on their outcome. In particular we note that nearly a quarter of discharged ICU patients needed longer-term care following their exit from the ICU wards. This is worth further investigation as this is a critical link in the continuum of care, helping move patients from ICU to eventual discharge to the community [28]. Among those that died, the shorter stay in ICU is potentially a consequence of stopping support for a patient who is not responding to therapy, and who is deemed unlikely to survive.
The observed evolution in outcomes will be a result of a complex interplay of different factors which we could not account for. In particular, we do not know the underlying severity of cases entering hospital, including specific comorbidities, and how this has changed over time [15]. We also do not know the specific treatment regimens given to patients. Furthermore, regional differences in infection burden, local hospital capacity and decision-making by physicians is likely to have resulted in variability in outcomes across hospitals or communities. Our data was insufficiently granular to explore these local trends. More detailed data on comorbidities and treatment regimens could help disentangle the potential causes for our observed changes in health outcomes over the course of the epidemic. Despite these limitations, this comprehensive dataset that covers all COVID-19 hospitalisations in France throughout a long time period has allowed us to uncover important overall trends in the outcomes of patients over the pandemic, while accounting for the varying sex and age profile of cases. We have also been able to capture the durations patients spend within hospital and how this differs by age and their ultimate outcome. These estimates provide a much needed evidence base to help characterise future demands on the healthcare sector from the pandemic.
Author Contributions
N.L., H.S., and S.C. conceived of the study, developed the methods, performed analyses, and co-wrote the paper. J.P., N.H., N.C. Y.Y., L.B., P.-Y.B. and F.C. contributed to data collection and analysis. All authors contributed to paper revisions.
Ethical considerations
The study was based on a secondary use of a database/pseudonymised data collected from health professionals. According to French law such studies are not required to receive ethics committee approval. In addition, the study was carried out as a contribution to the legal missions of health surveillance and alert of Santé Publique France, and therefore benefited from the legal prerogatives vested in Santé Publique France to carry out these missions. Santé Publique France can access all information, which is necessary for the accomplishment of its missions and has authorization from the French data protection authority to process personal health data in order to prevent, manage or assess the consequences of an epidemic.
Availability of data and materials
Code is available at https://github.com/noemielefrancq/Evolution-Outcomes-COVID19-France.
Declaration of Interests
N.L, J.P., N.H., N.C., L.B., P.-Y.B., Y.Y., F.C. and S.C. have nothing to disclose. YY has been a board member receiving consultancy fees from ABBVIE, BMS, Gilead, MSD, J&J, Pfizer, and ViiV Healthcare, however, all these activities have been stopped in the 3 past years. H.S. reports personal fees from AstraZeneca Data Safety Monitoring Board, outside the submitted work.
Acknowledgement
We acknowledge financial support from the INCEPTION project (PIA/ANR-16-CONV-0005), the Investissement d'Avenir program, the Laboratoire d'Excellence Integrative Biology of Emerging Infectious Diseases program (grant ANR-10-LABX-62-IBEID), Santé Publique France, the European Union's Horizon 2020 research and innovation program under grants 101003589 (RECOVER), AXA and Groupama. H.S. and N.L. acknowledge support from the European Research Council (grant 804744) and the EPSRC Impact Acceleration Grant (RG90413).
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.lanepe.2021.100087.
Contributor Information
Henrik Salje, Email: hs743@cam.ac.uk.
Simon Cauchemez, Email: simon.cauchemez@pasteur.fr.
Appendix. Supplementary materials
References
- 1.Flaxman S., Mishra S., Gandy A., Unwin H.J.T., Mellan T.A., Coupland H. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020;584(7820):257–261. doi: 10.1038/s41586-020-2405-7. [DOI] [PubMed] [Google Scholar]
- 2.Brauner J.M., Mindermann S., Sharma M., Johnston D., Salvatier J., Gavenčiak T. Inferring the effectiveness of government interventions against COVID-19. Science. 2020 doi: 10.1126/science.abd9338. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moghadas S.M., Shoukat A., Fitzpatrick M.C., Wells C.R., Sah P., Pandey A. Projecting hospital utilization during the COVID-19 outbreaks in the United States. Proc Natl Acad Sci USA. 2020;117(16):9122–9126. doi: 10.1073/pnas.2004064117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Massonnaud C., Roux J., Crépey P. COVID-19: forecasting short term hospital needs in France. medRxiv. 2020 https://www.medrxiv.org/content/10.1101/2020.03.16.20036939v1.abstract Available from: [Google Scholar]
- 5.Andronico A., Kiem C.T., Paireau J., Succo T., Bosetti P., Lefrancq N. Evaluating the impact of curfews and other measures on SARS-CoV-2 transmission in French Guiana. medRxiv. 2020 doi: 10.1038/s41467-021-21944-4. https://www.medrxiv.org/content/10.1101/2020.10.07.20208314v1.abstract Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singhal T. A review of coronavirus disease-2019 (COVID-19) Indian J Pediatr. 2020;87(4):281–286. doi: 10.1007/s12098-020-03263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cascella M., Rajnik M., Cuomo A., Dulebohn S.C., Di Napoli R. StatPearls. StatPearls Publishing; Treasure Island (FL): 2020. Features, evaluation, and treatment of coronavirus. [PubMed] [Google Scholar]
- 8.RECOVERY Collaborative Group. Horby P., Lim W.S., Emberson J.R., Mafham M., Bell J.L. Dexamethasone in hospitalized patients with Covid-19 - preliminary report. N Engl J Med. 2020 doi: 10.1056/NEJMoa2021436. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Verity R., Okell L.C., Dorigatti I., Winskill P., Whittaker C., Imai N. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis. 2020;20(6):669–677. doi: 10.1016/S1473-3099(20)30243-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Faes C., Abrams S., Van Beckhoven D., Meyfroidt G., Vlieghe E., Hens N. Time between symptom onset, hospitalisation and recovery or death: statistical analysis of Belgian COVID-19 patients. Int J Environ Res Public Health. 2020;17(20) doi: 10.3390/ijerph17207560. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dennis J.M., McGovern A.P., Vollmer S.J., Mateen B.A. Improving survival of critical care patients with coronavirus disease 2019 in England: a national cohort study, March to June 2020. Crit Care Med. 2020 doi: 10.1097/CCM.0000000000004747. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Doidge J.C., Gould D.W., Ferrando-Vivas P., Mouncey P.R., Thomas K., Shankar-Hari M. Trends in intensive care for patients with COVID-19 in England, Wales and Northern Ireland. Am J Respir Crit Care Med. 2020 doi: 10.1164/rccm.202008-3212OC. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Horwitz L., Jones S.A., Cerfolio R.J., Francois F., Greco J., Rudy B. Trends in COVID-19 Risk-Adjusted Mortality Rates. J Hosp Med. 2020 doi: 10.12788/jhm.3552. https://www.journalofhospitalmedicine.com/jhospmed/article/230561/hospital-medicine/trends-covid-19-risk-adjusted-mortality-rates Available from: [DOI] [PubMed] [Google Scholar]
- 14.Richardson S., Hirsch J.S., Narasimhan M., Crawford J.M., McGinn T., Davidson K.W. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized With COVID-19 in the New York City Area. JAMA. 2020 doi: 10.1001/jama.2020.6775. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lewnard J.A., Liu V.X., Jackson M.L., Schmidt M.A., Jewell B.L., Flores J.P. Incidence, clinical outcomes, and transmission dynamics of severe coronavirus disease 2019 in California and Washington: prospective cohort study. BMJ. 2020;369:m1923. doi: 10.1136/bmj.m1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Petrilli C.M., Jones S.A., Yang J., Rajagopalan H., O'Donnell L., Chernyak Y. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020;369:m1966. doi: 10.1136/bmj.m1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Karagiannidis C., Mostert C., Hentschker C., Voshaar T., Malzahn J., Schillinger G. Case characteristics, resource use, and outcomes of 10 021 patients with COVID-19 admitted to 920 German hospitals: an observational study. Lancet Respir Med. 2020;8(9):853–862. doi: 10.1016/S2213-2600(20)30316-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Perez-Guzman P.N., Daunt A., Mukherjee S., Crook P., Forlano R., Kont M.D. Clinical characteristics and predictors of outcomes of hospitalized patients with COVID-19 in a multi-ethnic London NHS Trust: a retrospective cohort study. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa1091. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Salje H., Tran Kiem C., Lefrancq N., Courtejoie N., Bosetti P., Paireau J. Estimating the burden of SARS-CoV-2 in France. Science. 2020;369(6500):208–211. doi: 10.1126/science.abc3517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Linton N.M., Kobayashi T., Yang Y., Hayashi K., Akhmetzhanov A.R., Jung S.-.M. Incubation period and other epidemiological characteristics of 2019 novel coronavirus infections with right truncation: a statistical analysis of publicly available case data. J Clin Med Res. 2020;9(2) doi: 10.3390/jcm9020538. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cox D.R. Regression models and life-tables. J R Stat Soc Series B Stat Methodol. 1972;34(2):187–202. [Google Scholar]
- 22.Lunn M., McNeil D. Applying Cox regression to competing risks. Biometrics. 1995;51(2):524–532. [PubMed] [Google Scholar]
- 23.Lau B., Cole S.R., Gange S.J. Competing risk regression models for epidemiologic data. Am J Epidemiol. 2009;170(2):244–256. doi: 10.1093/aje/kwp107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stan Development Team. RStan: the R Interface to Stan. 2020. Available from: http://mc-stan.org/
- 25.Moore J.B., June C.H. Cytokine release syndrome in severe COVID-19. Science. 2020;368(6490):473–474. doi: 10.1126/science.abb8925. [DOI] [PubMed] [Google Scholar]
- 26.Joebges S., Biller-Andorno N. Ethics guidelines on COVID-19 triage-an emerging international consensus. Crit Care. 2020;24(1):201. doi: 10.1186/s13054-020-02927-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang Y., Wang Y., Chen Y., Qin Q. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J Med Virol. 2020;92(6):568–576. doi: 10.1002/jmv.25748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Simpson R., Robinson L. Rehabilitation after critical illness in people with COVID-19 infection. Am J Phys Med Rehabil. 2020;99(6):470–474. doi: 10.1097/PHM.0000000000001443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mesas A.E., Cavero-Redondo I., Álvarez-Bueno C., Sarriá Cabrera M.A., Maffei de Andrade S., Sequí-Dominguez I. Predictors of in-hospital COVID-19 mortality: a comprehensive systematic review and meta-analysis exploring differences by age, sex and health conditions. PLoS ONE. 2020;15(11) doi: 10.1371/journal.pone.0241742. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Code is available at https://github.com/noemielefrancq/Evolution-Outcomes-COVID19-France.