Abstract
Adolescence is a period of social, physical, and neurobiological transitions that may leave individuals more vulnerable to the development of internalizing and externalizing symptomatology. Extant research demonstrates that executive functioning (EF) is associated with psychopathology outcomes in adolescence; however, it has yet to be examined how EF and psychopathology develop transactionally over time. Data were collected from 167 adolescents (47% female, 13–14 years old at Time 1) and their primary caregiver over four years. At each time point, adolescents completed three behavioral tasks that capture the underlying dimensions of EF, and both adolescents and their primary caregiver completed measures of adolescent psychopathology. Latent growth curve modeling was used to test the associations between initial levels and trajectories of EF and psychopathology. Results indicated that higher initial levels of internalizing and externalizing symptomatology were associated with lower EF at Time 4 (controlling for Time 1 EF). Initial levels of EF did not predict changes in internalizing and externalizing symptomatology. These findings suggest that early psychopathology may be a risk factor for maladaptive EF development in adolescence.
Keywords: Executive functioning, internalizing symptomatology, externalizing symptomatology, adolescence, growth curve modeling
The developmental period of adolescence marks important social, physical, and neurobiological transitions which can leave individuals vulnerable to a host of psychosocial and adjustment problems (Steinberg, 2005). These transitions are related in part to dramatic changes in structure and function of the brain. Neurodevelopmental models of adolescent brain development emphasize the imbalance in developmental trajectories between subcortical/limbic regions and prefrontal regions, which often manifests in the form of challenges in self-regulation (Casey, Jones, & Hare, 2008). Despite accumulating evidence demonstrating the consequences of these self-regulatory challenges, there lacks a systematic investigation as to how self-regulation and adjustment problems develop transactionally during adolescence. The present study focused on testing whether individual differences in the growth of self-regulation, in the form of executive functioning capacities, may contribute to developmental changes in adolescent psychopathology, and vice versa.
Adolescent Executive Functioning
Broadly, self-regulation is the capacity to flexibly regulate behavior, cognition, and emotion in order to successfully pursue long term goals (Baumeister, Vohs, & Tice, 2007). Self-regulation may encompass a number of processes, including both top-down and bottom-up regulatory processes that control emotion, cognition, and behavior (Nigg, 2017). Effective self-regulation often requires top-down processing of information in order to achieve certain states or goals, and involves effortful, deliberate exertion of control. These top-down aspects of self-regulation are represented by executive functioning (EF). Specifically, EF refers to higher order cognitive abilities that guide goal-directed behaviors and enable self-regulation. According to the theoretical model by Miyake and et al. (2000), these abilities include updating and monitoring of information (working memory), shifting between tasks or mental sets (shifting), and the ability to inhibit prepotent responses (inhibitory control). These three abilities are distinct but correlated and together are thought to reflect the latent construct of EF (Friedman & Miyake, 2017).
EF is not exclusively employed in the service of self-regulation and supports other skills such as solving math problems or planning future tasks. Indeed, EF and related cognitive abilities may affect adolescent adjustment through pathways other than self-regulation (e.g., attributional styles, perspective taking, verbal ability). For example, negative attributional style is a cognitive vulnerability that can exacerbate risk for depression among adolescents (Kim-Spoon, Ollendick, & Seligman, 2012) and trajectories of verbal ability are correlated with trajectories of externalizing symptomatology across childhood and adolescence (Papachristou & Flouri, 2019). However, for the purposes of the current study, we examine EF within the framework of self-regulation, understanding that these top-down cognitive abilities enable self-regulation (Barkley, 2012). Given the overlap in definitions of related constructs in research on self-regulation (see Nigg, 2017), we draw on broader self-regulation literature (e.g., effortful control, cognitive control) to inform our hypotheses regarding the linked development between EF and psychopathology.
Throughout early and middle childhood, EF shows linear growth, and is unidimensional (Lee, Bull, & Ho, 2013). As children transition into adolescence, the protracted development of the prefrontal cortex brings EF toward maturity (Klingberg, Forssberg, & Westerberg, 2002; Kwon, Reiss, & Menon, 2002) and EF begins to differentiate into the three-factor structure involving working memory, shifting, and inhibitory control (Lee et al., 2013). Evidence from human neuroimaging work illustrates these linear increases in EF during adolescence, indexed by lower activation in prefrontal areas during cognitive control tasks (Luna, Padmanabhan, & O’Hearn, 2010; Ordaz, Foran, Velanova, & Luna, 2013). However, there may be substantial variation in the rate of development. That is, some children may develop these cognitive capacities more rapidly than their peers, while others may demonstrate slower rates of growth or stability. In addition to differences in levels of EF, individual variation in change rates may have important implications for adjustment outcomes. For example, Hughes and Ensor (2011) reported that growth rates in EF were predictive of internalizing and externalizing behaviors among children, over and above the effects of initial levels of EF. These findings emphasize the importance of considering developmental change in EF in explaining individual differences in adjustment. However, there is limited research regarding within-person change in EF during adolescence, as well as how this change may be linked to adjustment outcomes.
Adolescent Psychopathology
Deficiencies in EF may contribute to a developmental cascade of risk, with interactions across multiple levels exerting progressive and cumulative effects on adjustment (Masten & Cicchetti, 2010). Indeed, EF has important implications for development across multiple domains of functioning, including academic (Becker, Miao, Duncan, & McClelland, 2014), social (Holmes, Kim-Spoon, & Deater-Deckard, 2016), and psychological (Harden et al., 2019) domains. In adolescence, individuals are particularly vulnerable to problems in psychological domains, as reflected by the notable increase in prevalence of psychological disorders after age 12 (Costello, Mustillo, Erkanli, Keeler, & Angold, 2003; Lee et al., 2014). Specifically, increasing autonomy, novel social influences, and environmental stressors (Steinberg, 2005) expose adolescents to considerable risk for the development of psychopathology, including internalizing symptomatology (e.g., anxiety, depression, withdrawal, and somatic complaints) and externalizing symptomatology (e.g., aggression and rule-breaking behaviors).
Previous work has demonstrated significant individual differences in longitudinal changes in internalizing and externalizing symptomatology in adolescence through age 16 (Hatoum, Rhee, Corley, Hewitt, & Friedman, 2018b). However, findings regarding the direction of these changes during adolescence remain mixed. For example, internalizing symptomatology has shown increases (Leve, Kim, & Pears, 2005), decreases (Hatoum et al., 2018b; Sirin et al., 2015), and no change (Galambos, Barker, & Almeida, 2003) during adolescence. Similarly, externalizing symptomatology has shown both decreases (Bongers, Koot, van der Ende, & Verhulst, 2004; Hatoum et al., 2018b) and increases (Bos et al., 2018; Galambos et al., 2003). The discrepancy in findings regarding the direction of changes in internalizing and externalizing symptomatology may be due in part to the fact that many previous studies have used samples across large age ranges covering portions of both childhood and adolescence. Thus, additional research using repeated measures of psychopathology focusing on adolescence is required to better elucidate the nature of longitudinal changes in internalizing and externalizing symptomatology during this critical development period.
Importantly, not all adolescents suffer from psychological disorders. Since self-regulation is integral to the development of psychopathology (Nigg, 2017), elucidating individual differences in the development of cognitive abilities that facilitate successful self-regulation is imperative to understanding why some adolescents may be particularly vulnerable to developing internalizing and externalizing symptomatology.
Joint Development of Executive Functioning and Internalizing and Externalizing Symptomatology
It is well-established that top-down self-regulatory abilities are related to child and adolescent adjustment outcomes. Deficits in EF have been linked to heightened general psychopathology across development (Martel et al., 2017; White et al., 2017). There is also evidence that these associations differ depending on the domain of psychopathology considered. For example, White et al. (2017) found that EF was associated with internalizing (anxious-misery), but not externalizing, domains of psychopathology in a sample of youths ages 8–24 (N = 9,498). At the same time, there is evidence that externalizing symptomatology is significantly predicted by certain dimensions of EF in middle childhood, pre-adolescence, and adolescence (Huang-Pollock, Shapiro, Galloway-Long, & Weigard, 2017; Martel et al., 2009; Woltering, Lishak, Hodgson, Granic, & Zelazo, 2016). These mixed patterns of results may be due to methodological differences (e.g., measurement, modeling), but also may be due to developmental differences in the EF-psychopathology association. Indeed, a recent cross-sectional study comparing two separate samples (one of children, one of adolescents) found that cognitive control (a common factor based on EF and effortful control) was associated with both internalizing and externalizing symptomatology in children, but only externalizing symptomatology in adolescents (Kim-Spoon, Deater-Deckard, Calkins, King-Casas, & Bell, 2019).
The link between EF and psychopathology may exist because the cognitive abilities encompassed by EF are necessary for successful management of negative emotions and arousal. For example, cognitive control may protect individuals against depression by allowing them to override attention biases and prevent rumination (Gotlib & Joormann, 2010). Further, it has been theorized that deficits in EF contribute to externalizing behaviors (particularly substance use problems) as a result of poor cognitive regulation of behavior (Giancola & Mezzich, 2003). More recent work has identified EF as a transdiagnostic risk factor for psychopathology in late adolescence/young adulthood, proposing that this association may be explained by the effects of EF on dependent stress and rumination (Snyder, Friedman, & Hankin, 2019). Taken together, current theories in developmental psychopathology highlight the critical role of EF in the development of internalizing and externalizing symptomatology.
Prior studies of the EF-psychopathology association have often been limited by self-report or the use of a singular EF task. However, latent models of common EF are increasingly being adopted which capture shared variance across multiple dimensions of EF. Large twin studies (N = 877) adopting this approach have found that higher levels of depression at age 17 are concurrently associated with lower common EF (Friedman, du Pont, Corley, & Hewitt, 2018). Furthermore, common EF at age 17 was associated with levels of parent- and teacher-reported internalizing symptomatology at age 7, but not with the trajectories of symptomatology from ages 7 to 16 (Hatoum, Rhee, Corley, Hewitt, & Friedman, 2018a). However, in this study, data were not available for EF during ages 7 to 16 years and only directionality from psychopathology to EF could be tested.
To date, it remains unclear how EF and psychopathology may develop transactionally over time. That is, not only does EF contribute to psychopathology, but psychopathology may exacerbate EF deficits over time. For example, when internalizing symptoms such as rumination emerge, they tax cognitive resources and make it difficult to perform other cognitive control tasks (Levens, Muhtadie, & Gotlib, 2009). This is consistent with the dual-process model of cognitive vulnerability for depression, which posits that dysphoric mood can deplete cognitive resources, in turn exacerbating cognitive deficits such as processing biases and the inability to engage in reflective processing (Beevers, 2005). Although there is less theoretical support for externalizing symptomatology contributing to EF, Eisenberg et al. (2010) posited that the effect of externalizing symptoms on later self-regulation may be a function of the responses that high externalizing children elicit from their environment. Specifically, the nature of their symptoms may make peers and parents less likely to offer opportunities for them to engage in and practice adaptive self-regulation.
Existing studies examining the relations between self-regulation and psychopathology have typically not utilized designs that would allow for these bidirectional associations to be empirically tested (i.e., cross-sectional in nature or lack of repeated measures of both domains). However, one longitudinal study using a large sample (N = 1,388) tested transactional relations between EF and internalizing and externalizing symptomatology measured at age 5, age 9, and age 13 (LaGasse et al., 2016). The results indicated some evidence of bidirectional associations, such that lower EF at age 9 predicted higher internalizing symptomatology, but not externalizing symptomatology, at age 13. Conversely, higher externalizing symptomatology and lower internalizing symptomatology at age 9 significantly predicted lower EF at age 13. While these findings offer insight in terms of directionality, cross-lagged panel models capture rank-order change from one time to the next, rather than across the entire longitudinal time frame. In order to capture individual differences in within-person change over time, approaches such as latent growth curve modeling must be adopted (see Muthén, 2004 for an overview). To our knowledge, only two studies have examined the association between developmental trajectories of self-regulation and adjustment using latent growth curve modeling. In one study, improvements in EF predicted slower increases in conduct problems among children (Piehler et al., 2014). Similarly, in the second study, both higher initial levels and the change rate of effortful control predicted later levels (but not change rate) of internalizing and externalizing symptomatology (King, Lengua, & Monahan, 2013). However, these prior studies have only tested psychopathology as a consequence, and not a potential risk factor, for self-regulatory development.
Present Study
The purpose of the present study was to determine variation in the development of EF and psychopathology within and between individuals throughout adolescence. Specifically, we sought to examine whether variation in the development of EF (based on inhibitory control, shifting, and working memory) predicted developmental changes in internalizing and externalizing symptomatology. We hypothesized that lower initial levels of EF would predict increases in both internalizing and externalizing symptomatology. Similarly, although we expected to see positive growth in EF across the sample, we expected that those with decreases or slower increases in EF would exhibit increases in internalizing and externalizing symptomatology. To elucidate bidirectional effects between EF and psychopathology, we also tested whether higher initial levels and longitudinal increases in internalizing and externalizing symptomatology would predict changes in EF.
Method
Participants
The current study used four waves of data that were collected as part of an ongoing longitudinal study which began in 2014. The sample includes 167 adolescents (53% males, 47% females) and their primary caregiver (82% biological mothers, 13% biological fathers, 2% grandmothers, 1% foster, 2% other). Adolescents were 13 or 14 years of age at Time 1 (M = 14.13, SD = 0.54), 14 or 15 years of age at Time 2 (M = 15.05, SD = 0.54), 15 or 16 years of age at Time 3 (M = 16.07, SD = .56), and 16 or 17 years of age at Time 4 (M = 17.01, SD = 0.55), with approximately one year between each time point. Adolescents identified as Caucasian (82%), African-American (12%), and other race (6%). Household income ranged from less than $1,000 to greater than $200,000 per year with a median of $35,000 - $49,999 at all time points (consistent with the median for the region; United States Census Bureau, 2010).
At Time 1, 157 families participated. At Time 2, 10 adolescents 14–15 years of age were added for a final sample of 167 parent-adolescent dyads. However, 26 families did not participate at all possible time points for reasons including: declined participation (n = 13), lost contact (n = 10), ineligibility for functional magnetic resonance imaging (fMRI) (n = 2), and extenuating circumstances (n = 1) during the follow-up assessments. These 26 families participated in an average of two time points out of four possible time points. We performed attrition analyses using a general linear model (GLM) univariate procedure to determine whether there were systematic predictors of missing data. Results indicated that rate of participation (indexed by proportion of years participated to years invited to participate) was not significantly predicted by demographic variables (p = .64 for age, p = .60 for income, p = .70 for sex, p = .73 for race, contrasted as White vs non-White).
Procedures
Participants were recruited from the community in the Southeastern United States via flyers, recruitment letters, and e-mail. The analyses reported here include behavioral and self-report data; however, the broader longitudinal study also included a neuroimaging procedure. Thus, individuals were ineligible for the study if they had a history of head injury resulting in loss of consciousness for more than 10 minutes, claustrophobia, orthodontia impairing image acquisition, or other contraindications to fMRI. Data collection occurred at university offices where adolescents agreed to participation via written assent, while parents provided written consent, and were then administered the protocol by trained research assistants. In addition to the data reported here, adolescents and their parents participated in fMRI tasks, as well as other behavioral tasks and questionnaires. These procedures took approximately five hours total. Adolescents and their parents received monetary compensation for their time.
Measures
Internalizing and externalizing symptomatology
Adolescents’ self-reported levels of internalizing and externalizing symptomatology were assessed with the Youth Self-Report (YSR; Achenbach & Rescorla, 2001), a 112-item questionnaire that assesses behavior problems in children ages 11 to 18. Behaviors were rated on a 3-point scale ranging from “0 = Not true” to “2 = Very true”. Raw summed scores from the externalizing symptomatology (aggressive behavior and rule-breaking behavior) and internalizing symptomatology (anxious-depressed, withdrawal-depressed, and somatic complaints) scales were used. The YSR has shown strong psychometric properties for internalizing and externalizing (α = .90; Achenbach & Rescorla, 2001) and demonstrates similar reliability in the current sample for both internalizing symptomatology (α = .85 – .90 across time points) and externalizing symptomatology (α = .84 – .89 across time points).
Parent-report of adolescent internalizing and externalizing symptomatology was assessed with the Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2001), a 118-item questionnaire that assesses behavior problems for children 6–18 years of age. As in the YSR, behaviors are rated on a 3-point scale and we used raw sums for the externalizing and internalizing symptomatology scales. The CBCL has shown strong psychometric properties for internalizing (α = .90) and externalizing (α = .94) symptomatology and demonstrates similar reliability in the current sample for both internalizing symptomatology (α = .87 – .90 across time points) and externalizing symptomatology (α = .90 – .91 across time points). Parent and adolescent reports were moderately correlated for both internalizing (r = .26–.33) and externalizing (r = .28–.35) symptomatology across all time points. Taking advantage of multiple informants’ reports, we created composite scores by averaging parent and adolescent reports for both internalizing and externalizing symptomatology.
Executive functioning
We administered three behavioral tasks that capture the underlying constructs of EF: working memory, shifting, and inhibitory control, which are in line with the theoretical model proposed by Miyake et al. (2000). Working memory was measured using the Stanford-Binet memory for digits (Roid, 2003) in which participants were asked to repeat back a series of numbers read by the experimenter (first forward, then backwards). We used the backwards digits score to index working memory ability. The shifting component of EF was captured using the Wisconsin Card Sorting Test (WCST; Heaton, & Staff, 2003) which requires participants to sort a series of cards based on color, number, and shapes of the patterns on the card under changing schedules of reinforcement. We used the number of perseverative errors as an index of shifting/cognitive flexibility. Finally, inhibitory control was measured using the Multi-Source Interference Task (MSIT; Bush, Shin, Holmes, Rosen, & Vogt, 2003).. In the MSIT, participants are presented with sequences of three digits, two of which are identical. Participants are instructed to indicate the identity (but not the position) of the unique, target digit. In the neutral condition, target digits are congruent with position (e.g., “2” is in the second position in the sequence “121”). In the interference condition, target digits are incongruent with position (e.g. “2” is in the first position in the sequence “211”). To assess task performance, we used intraindividual variability in reaction time, indexed as intraindividual standard deviations (ISDs; MacDonald, Karlsson, Rieckmann, Nyberg, & Bäckman, 2012) for correct responses in the interference condition. Studies examining the role of intraindividual variability (IIV) of reaction time demonstrate the importance of IIV as an indicator of cognitive functioning (e.g., Hultsch, MacDonald, & Dixon, 2002). In our sample, accuracy was negatively correlated with ISD (r = −.26 to −.52 across four waves, ps < .01), suggesting that greater variability in reaction time during the MSIT was associated with worse performance on the task and thus worse inhibitory control. Previous work has also shown that IIV in reaction time changes across development (Williams, Hultsch, Strauss, Hunter, & Tannock, 2005) and may offer information above and beyond mean levels of reaction time. The MSIT was administered while blood-oxygenation-level-dependent (BOLD) responses were recorded using fMRI; however, we used only reaction time data for the current analyses.
Data Analytic Plan
Skewness and kurtosis were examined for all variable distributions with acceptable levels less than 3 and 10, respectively (Kline, 2011) and all variables were normally distributed. Outliers were identified as values ≥ 3 SD from the mean. In these cases, values were winsorized to retain statistical power and attenuate bias resulting from elimination. The hypothesized models were tested via Structural Equation Modeling (SEM) using Mplus statistical software version 8.1 (Muthén & Muthén, 1998–2017). Overall model fit indices were determined by χ2 value, degrees of freedom, corresponding p-value, Root Mean Square Error of Approximation (RMSEA), and Confirmatory Fit Index (CFI). RMSEA values of less than .05 were considered a close fit while values less than .08 were considered an acceptable fit (Browne & Cudeck, 1993). CFI values of greater than .90 were considered an acceptable fit while values greater than .95 were considered an excellent fit (Bentler, 1990). Full information maximum likelihood (FIML) estimation procedure (Arbuckle, 1996) was used for missing data since FIML estimates are superior to those obtained with listwise deletion or other ad hoc methods (Schafer & Graham, 2002).
Univariate latent growth curve modeling (GCM) was used to fit a two-factor growth model across the four time points for EF. Because EF had multiple indicators at each assessment time, a second-order growth model, specifically the curve of factors model (CUFFS; McArdle, 1988) was used. The CUFFS model is an extension of the LCM and characterizes the relation between the multiple indicators and the underlying construct at each time point while estimating the growth trajectory of the construct (Geiser, Keller, & Lockhart, 2013; McArdle, 1988). Within this model, we imposed a series of constraints on the EF factors in order to establish factorial invariance over time. The most parsimonious model with adequate fit was selected as the final model. In the growth model, the first latent factor was the intercept, with all factor loadings fixed to one. The second latent factor was the slope, indicating growth of the function and change over time. To determine the shape of the trajectories, nested model comparisons were used to compare a latent basis growth model to a linear growth model. In the linear growth model, a linear pattern of change was assumed and factor loadings for the slope factor were fixed to 0, 1, 2, and 3. The latent basis growth model allowed the data to estimate the shape of growth by fixing the first and last time points (to 0 and 1, respectively) and freely estimating the second and third. The χ2 difference test was used to compare these nested models, and the most parsimonious model with acceptable fit was chosen as the final model. Next, for psychopathology, univariate GCM was used to fit a two-factor growth model across the four time points. In the same way as the EF GCM, nested model comparisons were used to compare model fits for latent basis and linear growth patterns, separately for internalizing and externalizing symptomatology. Though we used combined parent and adolescent report of psychopathology, we also explored the univariate growth curves for parent and adolescent report separately (see Appendix). Generally, these models demonstrated worse fit than the combined parent and adolescent report.
Results
Correlations and descriptive statistics are presented in Table 1 for EF variables and Table 2 for psychopathology variables.
Table 1.
Descriptive Statistics and Correlations for Executive Functioning Variables
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | M (SD) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Time 1 | ||||||||||||
| 1. Inhibitory control | 0.24 (0.04) | |||||||||||
| 2. Working memory | .20* | 5.56 (1.75) | ||||||||||
| 3. Shifting | .25** | .17* | 7.10 (3.17) | |||||||||
| Time 2 | ||||||||||||
| 4. Inhibitory control | .49** | .27** | .17* | 0.21 (0.04) | ||||||||
| 5. Working memory | .14 | .57** | .02 | .18* | 5.84 (1.90) | |||||||
| 6. Shifting | .28** | .26** | .50** | .23** | .16* | 5.41 (2.16) | ||||||
| Time 3 | ||||||||||||
| 7. Inhibitory control | .45** | .21* | .20* | .59** | .16 | .28** | 0.19 (0.04) | |||||
| 8. Working memory | .16 | .57** | .23** | .28** | .55** | .21* | .18* | 6.11 (2.09) | ||||
| 9. Shifting | .15 | .22** | .11 | .23* | .04 | .10 | .23** | .17* | 4.80 (1.44) | |||
| Time 4 | ||||||||||||
| 10. Inhibitory control | .39** | .13 | .21* | .59** | .18* | .25** | .51** | .12 | .20* | 0.18 (0.04) | ||
| 11. Working memory | .21* | .58** | .18* | .25** | .54** | .17* | .21* | .70** | .18* | .17* | 6.73 (2.31) | |
| 12. Shifting | .15 | .13 | .35** | .13 | –.01 | .26** | .09 | .11 | .11 | .14 | .14 | 4.71 (1.67) |
Note.
p < .05
p < .01
Table 2.
Descriptive Statistics and Correlations for Psychopathology Variables
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | Range | M (SD) |
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Time 1 | |||||||||
| 1. Internalizing symptomatology | 0.50–27.50 | 9.54 (5.45) | |||||||
| 2. Externalizing symptomatology | .49** | 1.00–29.00 | 8.19 (5.14) | ||||||
| Time 2 | |||||||||
| 3. Internalizing symptomatology | .78** | .29** | 0.00–27.50 | 9.41 (5.96) | |||||
| 4. Externalizing symptomatology | .37** | .78** | .36** | 1.00–25.00 | 9.40 (5.00) | ||||
| Time 3 | |||||||||
| 5. Internalizing symptomatology | .70** | .34** | .76** | .31** | 0.00–26.00 | 9.54 (5.79) | |||
| 6. Externalizing symptomatology | .31** | .77** | .22** | .79** | .37** | 0.50–26.00 | 7.94 (5.52) | ||
| Time 4 | |||||||||
| 7. Internalizing symptomatology | .63** | .34** | .64** | .29** | .68** | .28** | 0.00–27.50 | 9.54 (5.74) | |
| 8. Externalizing symptomatology | .28** | .72** | .15 | .68** | .26** | .79** | .37** | 0.50–27.00 | 7.89 (5.34) |
Note.
p < .05
p < .01
Univariate Growth Curve Models
Executive functioning
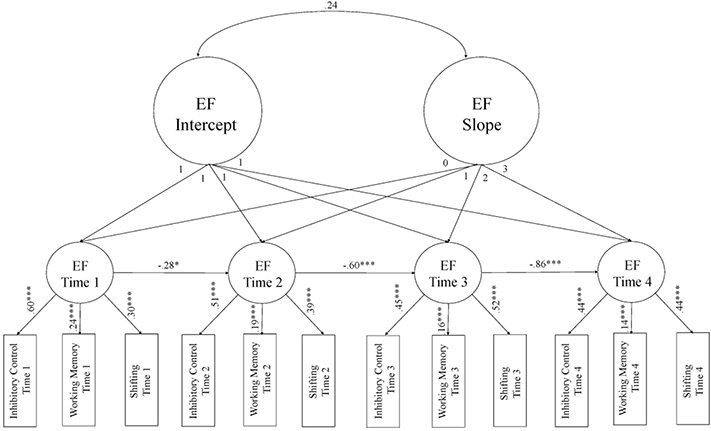
Two alternative models were fit in order to determine the shape of the trajectory of EF. The χ2 difference test indicated that a linear growth model provided the best fit to the data (see Table 3). We then imposed a series of equality constraints to test for configural invariance (invariance of the pattern of fixed and freed loadings across time), weak invariance (invariance of factor loadings across time), and strong invariance (invariance of factor loadings and intercepts across time) (Little, 2013). The model with strong factorial invariance was the most parsimonious version of the model that also demonstrated acceptable model fit (χ2 = 94.24, df = 50, p = .0002, RMSEA = 0.07, CFI = .91). Introducing autoregressive paths between the EF latent factors significantly improved model fit (Δχ2 = 32.03, Δdf = 3, p < .001), and this final model (Figure 1) demonstrated excellent fit (χ2 = 62.21, df = 47, p = .07, RMSEA = 0.04, CFI = .97). Significant variance of the intercept factor (σ2 = 5.55, SE = 1.82, p = .002) indicated individual differences in initial levels of EF. The mean of the latent slope factor was significant (M = 3.33, SE = 0.30, p < .001) indicating overall increases in EF over time. However, the variance of the slope factor was not significant (σ2 = 0.45, SE = 0.35, p = .21). Finally, the association between the EF intercept and slope was not significant (r = .24, SE = 0.47, p = .61).
Table 3.
Fit Indices of Univariate Growth Curve Models for Executive Functioning and Psychopathology Variables
| Model Label | χ2 | df | p | RMSEA | CFI | Δχ2 | Δdf | p(d) |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Executive functioning | ||||||||
| 1. Linear growth model | 62.21 | 47 | .07 | .04 | .97 | |||
| 2. Latent basis growth model+ | 62.33 | 45 | .04 | .05 | .96 | |||
| Externalizing symptomatology | ||||||||
| 3. Linear growth model | 15.26 | 8 | .05 | .07 | .98 | |||
| 4. Latent basis growth model | 9.40 | 6 | .15 | .06 | .99 | 5.86 | 2 | .05 |
| Internalizing symptomatology | ||||||||
| 5. Linear growth model | 13.56 | 8 | .09 | .06 | .99 | |||
| 6. Latent basis growth model+ | 6.27 | 6 | .39 | .02 | 1.00 | |||
Note. Best-fitting univariate model in boldface. CFI = comparative fit index; RMSEA = root mean square error of approximation; Δχ2 = difference in likelihood ratio tests; Δdf = difference in df; p(d) = probability of the difference tests.
Problem with latent variable covariance matrix, model not interpretable
Figure 1.
Unconditional growth curve model for executive functioning (EF). Standardized estimates are presented to demonstrate effect size.
*p < .05, **p < .01, ***p < .001 (based on unstandardized estimates).
Psychopathology
As with the EF models, two separate univariate growth models were fit in order to determine the shape of the trajectories of internalizing and externalizing symptomatology (see Table 3). For externalizing symptomatology, a linear growth model provided marginally better fit to the data and was more parsimonious than the latent basis model. Significant variances of intercept (σ2 = 20.58, SE = 2.79, p < .001) and slope (σ2 = 0.52, SE = 0.23, p = .03) indicated that there were significant individual differences in initial levels as well as change in externalizing symptomatology. The mean of the intercept was significantly different from zero (M = 8.05, SE = 0.39, p < .001), but the mean of the slope was not significant (M = −0.06, SE = 0.11, p = .60), indicating no significant changes in the level of externalizing symptomatology over time. The association between the externalizing symptomatology intercept and slope was not significant (r = −.11, SE = 0.16, p = .49).
For internalizing symptomatology, the linear growth model provided better fit to the data. Significant mean (M = 9.40, SE = 0.43, p < .001) and variance (σ2 = 23.95, SE = 3.37, p < .001) of the intercept indicated that there were significant individual differences in initial levels of internalizing symptomatology. Variance of the slope was significant indicating individual differences in developmental changes (σ2 = 0.81, SE = 0.34, p = .02). However, the mean slope of internalizing symptomatology was not significant (M = 0.05, SE = 0.13, p = .72) indicating no significant change in the level of internalizing symptomatology over time. The association between the internalizing symptomatology intercept and slope was significant (r = −.28, SE = 0.14, p = .05).
Associations Between EF and Psychopathology
Results from the GCM for EF indicated that the slope factor did not have significant variance. For this reason, we did not include the slope factor in the final model and instead included levels EF at Time 4 (controlling for Time 1). Specifically, we used confirmatory factor analysis (CFA) to estimate the latent factor of EF at Times 1 and 4 based on three manifest variables (i.e., inhibitory control, working memory, and shifting). Factor scores were used to promote parsimony and facilitate model convergence. At each time point, the models were fully saturated (i.e., χ2 = 0, df = 0) and all factor loadings were significant (standardized factor loadings ranged from .34 – .55). Factor scores were included as manifest variables in the final model which included the regression paths from psychopathology at Time 1 (intercept) to EF at Time 4, from EF at Time 1 to the slope of psychopathology, and from the psychopathology slope to EF at Time 4. Covariances were estimated between the residuals of the psychopathology intercept and slope factors, and between initial levels of EF and psychopathology. Relevant covariates (income, sex, and age) were tested in each model1.
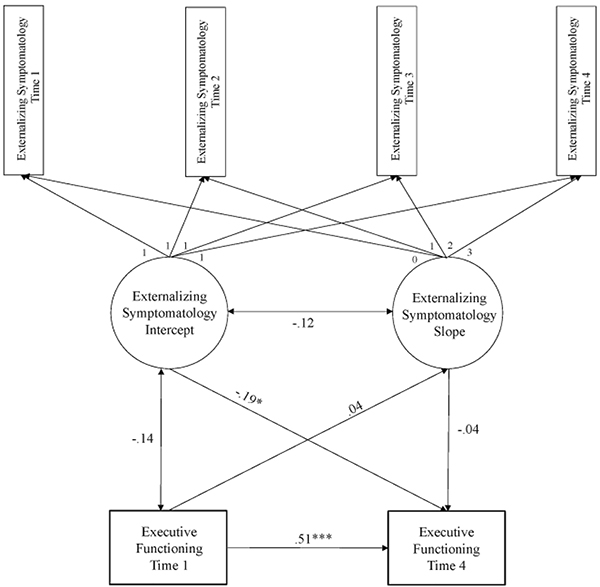
The model examining associations between EF and externalizing symptomatology (Figure 2) demonstrated acceptable fit (χ2 = 20.86, df = 12, p = .05, RMSEA = 0.07, CFI = .98). The intercept of externalizing symptomatology significantly predicted EF at Time 4 (b = −0.05, SE = 0.02, p = .01, β = −.19), suggesting that higher initial levels of externalizing symptomatology were associated with lower EF. EF at Time 1 did not predict the slope of externalizing symptomatology (b = 0.001, SE = 0.003, p = .80, β = .04) and the slope of externalizing symptomatology did not predict EF at Time 4 (b = −0.06, SE = 0.19, p = .75, β = −.04). The association between the externalizing symptomatology intercept and slope residual was not significant (r = −.12, SE = 0.16, p = .46). EF demonstrated moderate stability from Time 1 to Time 4 (b = 0.02, SE = 0.002, p < .001, β = .51).
Figure 2.
Estimates for the associations between executive functioning (EF) and externalizing symptomatology. Standardized estimates are presented to demonstrate effect size. *p < .05, **p < .01, ***p < .001 (based on unstandardized estimates).
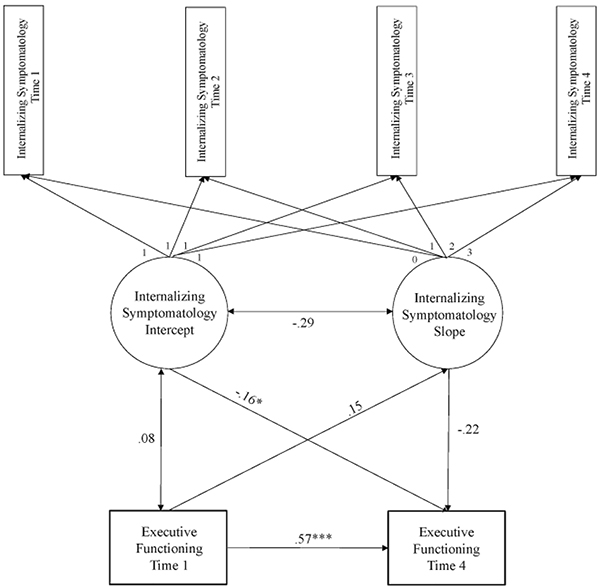
The same model was tested with internalizing symptomatology (Figure 3) and demonstrated acceptable fit (χ2 = 17.66, df = 12, p = .13, RMSEA = 0.05, CFI = .99). The intercept of internalizing symptomatology predicted EF at Time 4 (b = −0.04, SE = 0.02, p = .05, β = −.16), suggesting that higher initial levels of internalizing symptomatology were associated with lower EF. EF at Time 1 did not predict the slope of internalizing symptomatology (b = 0.004, SE = 0.004, p = .30, β = .15) and the slope of internalizing symptomatology did not predict EF at Time 4 (b = −0.28, SE = 0.19, p = .13, β = −.22). The association between the internalizing symptomatology intercept and slope residual was significant (r = −.29, SE = 0.14, p = .04). EF demonstrated moderate stability from Time 1 to Time 4 (b = 0.02, SE = 0.002, p < .001, β = .57).
Figure 3.
Estimates for the associations between executive functioning (EF) and internalizing symptomatology. Standardized estimates are presented to demonstrate effect size. *p < .05, **p < .01, ***p < .001 (based on unstandardized estimates).
Post-hoc Power Analyses
We ran a Monte Carlo study in Mplus according to recommendations from Muthén and Muthén (2002). Using the final estimates from the internalizing and externalizing symptomatology models as starting values, we ran 500 repetitions with a random seed. With n = 167, coverage was sufficient for all estimates (i.e., between .93 and .99) and parameter and SE bias did not exceed 10% for any regression effects, with the exception of three estimates which were greater than the maximum acceptable bias percentage. These were for the effects of the internalizing and externalizing symptomatology slopes on EF and the effect of EF at Time 1 on the externalizing slope. These bias estimates decreased and began to approach acceptable levels at n = 2,000. Thus, greater sample size would be required to detect these particular effects.
Discussion
Recent work has pointed to EF as a transdiagnostic risk factor for psychopathology (Snyder et al., 2019). However, there is a paucity of evidence regarding how EF and psychopathology may develop transactionally over time. We used latent growth curve modeling to examine the joint development of EF with internalizing and externalizing symptomatology across adolescence. We considered both whether EF predicts the development of psychopathology, as well as whether psychopathology predicts the development of EF. We found that while EF increased across adolescence, there were no significant individual differences in the rate of development. When considering levels of EF (rather than rates of change), we found evidence that early psychopathology may interfere with adolescent EF development.
Our results indicate that those with heightened levels of internalizing and externalizing symptomatology in early adolescence were more likely to have lower EF in late adolescence. This finding corroborates previous work with children and adolescents. Hatoum and et al. (2018a) found that EF at age 17 was predicted by the intercept (age 7 levels) of internalizing symptomatology for both males and females, and externalizing symptomatology for males. However, because EF was measured at only one time point, directionality of the associations between EF and psychopathology could not be tested. Our findings clarify that developmental changes in psychopathology were not significantly predicted by earlier levels of EF in adolescence. LaGasse et al. (2016) tested directionality using a cross-lagged panel model, and found that the contributions of psychopathology to EF were more consistent than the contributions of EF to psychopathology. Specifically, both internalizing symptomatology and externalizing symptomatology at age 9 predicted EF at age 13, whereas EF at age 9 predicted only externalizing symptomatology (not internalizing symptomatology) at age 13. Connolly et al. (2014) also demonstrated that higher levels of depressogenic cognitive style (i.e., rumination) predicted decreases in certain aspects of EF (i.e., attentional shifting ability) over one year in a sample of adolescents. In contrast, lower levels of initial EF were not significantly predictive of increased rumination at follow-up. The current findings present the first evidence suggesting that higher levels of both internalizing symptomatology and externalizing symptomatology in early adolescence have detrimental effects on EF development.
Our data demonstrate that adolescents with higher internalizing symptomatology may have lower EF later in adolescence. This finding may be explained in part by the resource allocation hypothesis (Levens et al., 2009), which posits that the maladaptive cognitive patterns associated with depression (e.g., rumination, negative thoughts) may tax available cognitive resources, making it difficult to perform unrelated cognitive tasks (e.g., planning, decision-making). In line with the resource allocation hypothesis, our results suggest that those with lower symptoms likely had greater resources available to manage the new and cognitively taxing situations that arise in adolescence, and thus facilitated adaptive EF development. Different mechanisms may explain how and why early externalizing symptomatology predicted later EF. As speculated by Eisenberg and et al. (2010), aggressive and defiant behaviors may discourage adaptive and positive social engagement from parents and peers, thereby limiting opportunities to engage in adaptive self-regulation strategies (e.g., Farley & Kim-Spoon, 2014). Furthermore, adolescents experiencing these symptoms may not take advantage of opportunities to foster EF abilities when they do arise, thus disrupting their EF development. Additional research will be necessary to further elucidate developmental processes through which internalizing and externalizing symptomatology contribute to EF development over time.
Our longitudinal, second-order latent GCM indicated longitudinal increases in EF over time. This is consistent with theoretical models of adolescent brain development, which highlight linear changes in the prefrontal cortex that continue into early adulthood (Casey et al., 2008; Steinberg, 2008) as well as empirical evidence of prerontal cortex functioning (Ordaz et al., 2013) which supports adaptive EF development during adolescence. However, individual differences in EF growth were not significant, consistent with prior findings showing that EF in adolescence is rank-order stable (e.g., Friedman et al., 2016). For psychopathology, while some previous research has illustrated changes in symptoms across adolescence, we did not observe significant increases or decreases in our sample. This was not entirely unexpected given the relatively high rank-order stability in adolescent psychopathology (Snyder, Young, & Hankin, 2017) and the fact that previous studies using GCM to examine changes in psychopathology during adolescence found mixed results, with increases, decreases, and no change in psychopathology (e.g., Galambos et al., 2003; Hatoum et al., 2018b). These patterns of results may suggest that there are meaningful subgroups of adolescents that demonstrate different patterns of change in psychopathology. That is, some adolescents may increase while others decrease or stay the same, and thus testing mean changes across the entire sample may obscure these differences. Future work may benefit from applying statistical approaches that can capture distinctive subgroups, such as growth mixture modeling, to identify adolescents with different trajectory patterns of psychopathology.
We expected that lower initial levels of EF would predict longitudinal increases in both internalizing and externalizing symptomatology. However, our data did not provide supporting evidence for these hypotheses. Nonetheless, these findings are consistent with prior findings reporting a non-significant association between initial levels of effortful control and change rates of internalizing and externalizing symptomatology in pre-adolescence (King et al., 2013). We note that our sample was relatively small and thus the null findings should be interpreted with caution, and replications with greater sample sizes are warranted.
Limitations and Future Directions
Study limitations point to important directions for future research. First, more recent theoretical models of EF include updating-specific and shifting-specific factors in addition to common EF (Miyake & Friedman, 2012). Though we did not have a sufficient EF task battery to test this updated model, it will be informative for future work to include both the unity (common EF) and diversity (specific ability) components of EF. Second, our limited sample size prevented us from testing effects of factors that have been shown to moderate the associations between self-regulation and psychopathology, such as gender. For example, Hatoum et al. (2018a) found that teacher ratings of externalizing symptomatology were related to common EF, but only in males. Testing individual or environmental level moderators of these associations will be an important step in identifying adolescents who are particularly vulnerable to EF and adjustment problems. Third, although we captured growth in EF and psychopathology across several years of adolescence, a period germane to the development of these constructs, it remains unclear whether these trajectories would extend beyond adolescence. It will be beneficial to clarify whether individuals with higher psychopathology in early adolescence would experience long-term deficits in EF, or if they would eventually “catch up” with their same-age peers. Finally, though we had strong theoretical basis for the EF factors, the use of factor scores in the final model may have introduced bias due to potential issues of factor indeterminacy. Accordingly, replicating the current results using EF latent factors in future studies is warranted.
Despite these limitations, our study illustrates important methodological strengths that facilitate our understanding of EF and psychopathology in adolescence. First, we tested individual differences in within-person developmental trajectories of EF and psychopathology to overcome the limitations of traditional cross-lagged panel designs used often in studies of EF-psychopathology associations, which capture simple rank-order change that is subject to conflation of between- and within-person effects (see Berry & Willoughby, 2017). Furthermore, we used multiple behavioral tasks to index EF. By using multiple measures and CFA to model EF, we were able to extract the common variance and minimize problems related to task impurity (Miyake et al., 2000; Snyder, Miyake, & Hankin, 2015).
Conclusions
Our findings offer novel evidence that adolescents who exhibit higher internalizing and externalizing symptomatology in early adolescence may be more vulnerable to EF deficits later in adolescence. Indeed, improvements in psychopathology in clinical populations are followed by improvements in EF (Biringer et al., 2005), suggesting that addressing early internalizing and externalizing symptomatology may prevent disruptions in EF development. In addition to mitigating psychopathology, prevention efforts during childhood would benefit from proactively strengthening EF abilities and facilitating their development during adolescence. For example, an intervention program effective for increasing growth in EF also demonstrated decreases in conduct problems among children (Piehler et al., 2014). Early interventions such as this may be able to alter trajectories of both psychopathology and EF development during childhood, thereby alleviating the risk for impaired EF development during adolescence. Taken together, our findings highlight the importance of a developmental approach to better understand the nature of EF development in adolescence and identifies emerging psychopathology as a risk factor that may influence EF development.
Acknowledgments
This work was supported by grants from the National Institute of Drug Abuse (R01 DA036017) to J.K-S. and B.K-C. The authors thank the former and current JK Lifespan Development Lab members for help with data collection. We are grateful to the adolescents and parents who participated in this study. The authors declare that they have no competing or potential conflicts of interest.
Appendix
Fit Indices of Univariate Growth Curve Models for Psychopathology Variables, Separated by Parent and Adolescent Report
| Model Label | χ2 | df | p | RMSEA | CFI |
|---|---|---|---|---|---|
|
| |||||
| Externalizing symptomatology- Adolescent report | |||||
| 1. Linear growth model | 25.00 | 8 | .001 | .11 | .95 |
| 2. Latent basis growth model+ | |||||
| Internalizing symptomatology- Adolescent report | |||||
| 3. Linear growth model | 36.31 | 8 | .00 | .15 | .91 |
| 4. Latent basis growth model+ | 7.18 | 6 | .30 | .03 | 1.00 |
| Externalizing symptomatology- Parent report | |||||
| 5. Linear growth tdmodel | 28.71 | 8 | .00 | .12 | .95 |
| 6. Latent basis growth model+ | 25.95 | 6 | .00 | .14 | .95 |
| Internalizing symptomatology- Parent report | |||||
| 7. Linear growth tdmodel | 11.73 | 8 | .16 | .05 | .99 |
| 8. Latent basis growth model+ | 9.25 | 6 | .16 | .06 | .99 |
Note. CFI = comparative fit index; RMSEA = root mean square error of approximation.
Problem with latent variable covariance matrix, model not interpretable
Footnotes
Sex and age were not significantly associated with dependent variables. Income was negatively associated with EF at Time 4. Including income as a covariate did not change the pattern of results. However, it did significantly degrade model fit in the model for externalizing symptomatology (Δχ2 = 13.08, Δdf = 3, p < .01). Thus, income was not included in the final models, but these results are available upon request.
References
- Achenbach TM & Rescorla L (2001). Manual for the ASEBA School-Age Forms and Profiles. Burlington, VT: Department of Psychiatry, University of Vermont. [Google Scholar]
- Arbuckle JL (1996). Full information estimation in the presence of incomplete data. In Marcoulides GA & Schumacker RE (Eds.), Advanced structural equation modeling: Issues and techniques (pp. 243–277). Mahwah, NJ: Erlbaum. [Google Scholar]
- Barkley RA (2012). Executive Functions: What They Are, How They Work, and Why They Evolved. Guilford Press. [Google Scholar]
- Baumeister RF, Vohs KD, & Tice DM (2007). The strength model of self-control. Current Directions in Psychological Science, 16, 351–355. doi: 10.1111/j.1467-8721.2007.00534.x [DOI] [Google Scholar]
- Becker DR, Miao A, Duncan R, & McClelland MM (2014). Behavioral self-regulation and executive function both predict visuomotor skills and early academic achievement. Early Childhood Research Quarterly, 29, 411–424. doi: 10.1016/j.ecresq.2014.04.014 [DOI] [Google Scholar]
- Beevers C (2005). Cognitive vulnerability to depression: A dual process model. Clinical Psychology Review, 25, 975–1002. doi: 10.1016/j.cpr.2005.03.003 [DOI] [PubMed] [Google Scholar]
- Bentler PM (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107, 238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Berry D, & Willoughby MT (2017). On the practical interpretability of cross-lagged panel models: Rethinking a developmental workhorse, 88, 1186–1206. doi: 10.1111/cdev.12660 [DOI] [PubMed] [Google Scholar]
- Biringer E, Lundervold A, Stordal K, Mykletun A, Egeland J, Bottlender R, & Lund A (2005). Executive function improvement upon remission of recurrent unipolar depression. European Archives of Psychiatry and Clinical Neuroscience, 255, 373–380. doi: 10.1007/s00406-005-0577-7 [DOI] [PubMed] [Google Scholar]
- Bongers I, Koot HM, van der Ende J, & Verhulst FC (2004). Developmental trajectories of externalizing behaviors in childhood and adolescence. Child Development, 75, 1523–1537. [DOI] [PubMed] [Google Scholar]
- Bos MGN, Wierenga LM, Blankenstein NE, Schreuders E, Tamnes CK, & Crone EA (2018). Longitudinal structural brain development and externalizing behavior in adolescence. Journal of Child Psychology and Psychiatry, 59, 1061–1072. doi: 10.1111/jcpp.12972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne MW, & Cudeck R (1993). Alternative ways of assessing model fit. In Bollen & Long S (Eds.), Testing structural equation models (pp. 136–162). Beverly Hills: Sage. [Google Scholar]
- Bush G, Shin LM, Holmes J, Rosen BR, & Vogt BA (2003). The Multi-Source Interference Task: Validation study with fMRI in individual subjects. Molecular Psychiatry, 8, 60–70. doi: 10.1038/sj.mp.4001217 [DOI] [PubMed] [Google Scholar]
- Casey B, Jones RM, & Hare TA (2008). The adolescent brain. Annals of the New York Academy of Sciences, 1124, 111–126. doi: 10.1196/annals.1440.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connolly SL, Wagner CA, Shapero BG, Pendergast LL, Abramson LY, & Alloy LB (2014). Rumination prospectively predicts executive functioning impairments in adolescents. Journal of Behavior Therapy and Experimental Psychiatry, 45, 46–56. doi: 10.1016/j.jbtep.2013.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello E, Mustillo S, Erkanli A, Keeler G, & Angold A (2003). Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry, 60, 837–844. doi: 10.1001/archpsyc.60.8.837 [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Spinrad TL, Eggum ND, Silva KM, Reiser M, Hofer C, … Michalik N (2010). Relations among maternal socialization, effortful control, and maladjustment in early childhood. Development and Psychopathology, 22, 507–525. doi: 10.1017/S0954579410000246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farley JP, & Kim-Spoon J (2014). The development of adolescent self-regulation: The role of parent, peer, friend, and romantic relationships. Journal of Adolescence, 37, 433–440. doi: 10.1016/j.adolescence.2014.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman NP, du Pont A, Corley RP, & Hewitt JK (2018). Longitudinal relations between depressive symptoms and executive functions from adolescence to early adulthood. doi: 10.1177/2167702618766360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman NP, & Miyake A (2017). Unity and diversity of executive functions: Individual differences as a window on cognitive structure. Cortex, 1–19. doi: 10.1016/j.cortex.2016.04.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman NP, Miyake A, Altamirano LJ, Corley RP, Young SE, Rhea SA, & Hewitt JK (2016). Stability and change in executive function abilities from late adolescence to early adulthood: A longitudinal twin study. Developmental Psychology, 52, 326–340. doi: 10.1037/dev0000075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galambos NL, Barker ET, & Almeida DM (2003). Parents do matter: Trajectories of change in externalizing and internalizing problems in early adolescence. Child Development, 74, 578–594. doi: 10.1111/1467-8624.7402017 [DOI] [PubMed] [Google Scholar]
- Geiser C, Keller B, Lockhart G (2013). First versus second order latent growth curve models: Some insights from latent state-trait theory. Structural Equation Modeling, 20, 479–503. doi: 10.1080/10705511.2013.797832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giancola PR, & Mezzich AC (2003). Executive functioning, temperament, and drug use involvement in adolescent females with a substance use disorder. Journal of Child Psychology and Psychiatry, 44, 857–866. doi: 10.1111/1469-7610.00170 [DOI] [PubMed] [Google Scholar]
- Gotlib IH, & Joormann J (2010). Cognition and depression: Current status and future directions. Annual Review of Clinical Psychology, 6, 285–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harden KP, Engelhardt LE, Mann FD, Patterson MW, Grotzinger AD, Savicki SL, … Tucker-Drob EM (2019). Genetic associations between executive functions and a general factor of psychopathology. Journal of the American Academy of Child & Adolescent Psychiatry. doi: 10.1016/j.jaac.2019.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatoum AS, Rhee SH, Corley RP, Hewitt JK, & Friedman NP (2018a). Do executive functions explain covariance between internalizing and externalizing behaviors? Development and Psychopathology, 30, 1371–1387. doi: 10.1017/S0954579417001602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatoum AS, Rhee SH, Corley RP, Hewitt JK, & Friedman NP (2018b). Etiology of stability and growth of internalizing and externalizing behavior problems across childhood and adolescence. Behavior Genetics, 48, 298–314. doi: 10.1007/s10519-018-9900-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heaton RK, & Staff PAR (2003). Wisconsin card sorting test: Computer version 4-research edition (WCST: CV4). Lutz, FL: Psychological Assessment Resources. [Google Scholar]
- Holmes CJ, Kim-Spoon J, & Deater-Deckard K (2016). Linking executive function and peer problems from early childhood through middle adolescence. Journal of Abnormal Child Psychology, 44, 31–42. doi: 10.1007/s10802-015-0044-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang-Pollock C, Shapiro Z, Galloway-Long H, & Weigard A (2017). Is poor working memory a transdiagnostic risk factor for psychopathology? Journal of Abnormal Child Psychology, 45, 1477–1490. doi: 10.1007/s10802-016-0219-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes C, & Ensor R (2011). Individual differences in growth in executive function across the transition to school predict externalizing and internalizing behaviors and self-perceived academic success at 6 years of age. Journal of Experimental Child Psychology, 108, 663–676. doi: 10.1016/j.jecp.2010.06.005 [DOI] [PubMed] [Google Scholar]
- Hultsch DF, MacDonald SWS, & Dixon RA (2002). Variability in reaction time performance of younger and older adults. The Journals of Gerontology: Series B, 57, P101–P115. doi: 10.1093/geronb/57.2.P101 [DOI] [PubMed] [Google Scholar]
- Kim-Spoon J, Deater-Deckard K, Calkins S, King-Casas B, & Bell MA (2019). Commonality between executive functioning and effortful control related to adjustment. Journal of Applied Developmental Psychology, 60, 47–55. doi: 10.1016/j.appdev.2018.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim-Spoon J, Ollendick TH, & Seligman LD (2012). Perceived competence and depressive symptoms among adolescents: The moderating role of attributional style. Child Psychiatry & Human Development, 43, 612–630. doi: 10.1007/s10578-012-0287-0 [DOI] [PubMed] [Google Scholar]
- King KM, Lengua LJ, & Monahan KC (2013). Individual differences in the development of self-regulation during pre-adolescence: Connections to context and adjustment. Journal of Abnormal Child Psychology, 41, 57–69. doi: 10.1007/s10802-012-9665-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB (2011). Principles and practice of structural equation modeling (3rd ed.). New York: Guildford Press. [Google Scholar]
- Klingberg T, Forssberg H, & Westerberg H (2002). Increased brain activity in frontal and parietal cortex underlies the development of visuospatial working memory capacity during childhood. Journal of Cognitive Neuroscience, 14, 1–10. [DOI] [PubMed] [Google Scholar]
- Kwon H, Reiss AL, & Menon V (2002). Neural basis of protracted developmental changes in visuo-spatial working memory. Proceedings of the National Academy of Sciences, 99, 13336–13341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaGasse LL, Conradt E, Karalunas SL, Dansereau LM, Butner JE, Shankaran S, … Lester BM (2016). Transactional relations between caregiving stress, executive functioning, and problem behavior from early childhood to early adolescence. Development and Psychopathology, 28, 743–756. doi: 10.1017/S0954579416000286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee K, Bull R, & Ho RMH (2013). Developmental changes in executive functioning. Child Development, 84, 1933–1953. doi: 10.1111/cdev.12096 [DOI] [PubMed] [Google Scholar]
- Lee FS, Heimer H, Giedd JN, Lein ES, Šestan N, Weinberger DR, & Casey BJ (2014). Adolescent mental health—Opportunity and obligation. Science, 346, 547–549. doi: 10.1126/science.1260497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leve LD, Kim HK, & Pears KC (2005). Childhood temperament and family environment as predictors of internalizing and externalizing trajectories from ages 5 to 17. Journal of Abnormal Child Psychology, 33, 505–520. doi: 10.1007/s10802-005-6734-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levens SM, Muhtadie L, & Gotlib IH (2009). Rumination and impaired resource allocation in depression. Journal of Abnormal Psychology, 118, 757–766. doi: 10.1037/a0017206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little TD (2013). Longitudinal structural equation modeling (pp. 141–142). Guilford press. [Google Scholar]
- Luna B, Padmanabhan A, & O’Hearn K (2010). What has fMRI told us about the development of cognitive control through adolescence? Brain and Cognition, 72, 101–113. doi: 10.1016/j.bandc.2009.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDonald SWS, Karlsson S, Rieckmann A, Nyberg L, & Bäckman L (2012). Aging-related increases in behavioral variability: Relations to losses in dopamine D1 receptors. Journal of Neuroscience, 32, 8186–8191. doi: 10.1523/JNEUROSCI.5474-11.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel MM, Pan PM, Hoffmann MS, Gadelha A, do Rosário MC, & Mari JJ, et al. (2017). A general psychopathology factor (P factor) in children: Structural model analysis and external validation through familial risk and child global executive function. Journal of Abnormal Psychology, 126, 137–148. doi: 10.1037/abn0000205 [DOI] [PubMed] [Google Scholar]
- Martel MM, Pierce L, Nigg JT, Jester JM, Adams K, Puttler LI, … Zucker RA (2009). Temperament pathways to childhood disruptive behavior and adolescent substance abuse: testing a cascade model. Journal of Abnormal Child Psychology, 37, 363. doi: 10.1007/s10802-008-9269-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten AS, & Cicchetti D (2010). Developmental cascades. Development and Psychopathology, 22, 491–495. doi: 10.1017/S0954579410000222 [DOI] [PubMed] [Google Scholar]
- McArdle JJ (1988). Dynamic but structural modeling of repeated measures data. In Nesselroade JR, Cattell RB (Eds.), The Handbook of Multivariate Psychology (2nd ed. (pp. 561–614). New York, NY: Springer. [Google Scholar]
- Miyake A, & Friedman NP (2012). The nature and organization of individual differences in executive functions: Four general conclusions. Current Directions in Psychological Science, 21, 8–14. doi: 10.1177/0963721411429458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyake A, Friedman NP, Emerson MJ, Witzki AH, Howerter A, & Wager TD (2000). The unity and diversity of executive functions and their contributions to complex “frontal lobe” tasks: A latent variable analysis. Cognitive Psychology, 41, 49–100. doi: 10.1006/cogp.1999.0734 [DOI] [PubMed] [Google Scholar]
- Muthén B (2004). Latent Variable Analysis: Growth Mixture Modeling and Related Techniques for Longitudinal Data. In Kaplan D, The SAGE Handbook of Quantitative Methodology for the Social Sciences (pp. 346–369). Thousand Oaks California, United States of America: SAGE Publications, Inc. doi: 10.4135/9781412986311.n19 [DOI] [Google Scholar]
- Muthén LK, & Muthén BO (2002). How to use a Monte Carlo study to decide on sample size and determine power. Structural Equation Modeling: A Multidisciplinary Journal, 9, 599–620. doi: 10.1207/S15328007SEM0904_8 [DOI] [Google Scholar]
- Muthén LK, & Muthén BO (1998–2017). Mplus User’s Guide. Seventh Edition. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Nigg JT (2017). Annual Research Review: On the relations among self-regulation, self-control, executive functioning, effortful control, cognitive control, impulsivity, risk-taking, and inhibition for developmental psychopathology. Journal of Child Psychology and Psychiatry, 58, 361–383. doi: 10.1111/jcpp.12675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ordaz SJ, Foran W, Velanova K, & Luna B (2013). Longitudinal growth curves of brain function underlying inhibitory control through adolescence. Journal of Neuroscience, 33, 18109–18124. doi: 10.1523/jneurosci.1741-13.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papachristou E, & Flouri E (2019). The codevelopment of internalizing symptoms, externalizing symptoms, and cognitive ability across childhood and adolescence. Development and Psychopathology, 1–15. doi: 10.1017/S0954579419001330 [DOI] [PubMed] [Google Scholar]
- Piehler TF, Bloomquist ML, August GJ, Gewirtz AH, Lee SS, & Lee WSC (2014). Executive functioning as a mediator of conduct problems prevention in children of homeless families residing in temporary supportive housing: A parallel process latent growth modeling approach. Journal of Abnormal Child Psychology, 42, 681–692. doi: 10.1007/s10802-013-9816-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roid GH (2003). Stanford-Binet Intelligence Scales, Fifth Edition, Itasca, IL: Riverside Publishing. [Google Scholar]
- Schafer JL, & Graham JW (2002). Missing data: Our view of the state of the art. Psychological Methods, 7, 147–177. doi: 10.1037/1082-989X.7.2.147 [DOI] [PubMed] [Google Scholar]
- Sirin SR, Rogers-Sirin L, Cressen J, Gupta T, Ahmed SF, & Novoa AD (2015). Discrimination-related stress effects on the development of internalizing symptoms among latino adolescents. Child Development, 86, 709–725. doi: 10.1111/cdev.12343 [DOI] [PubMed] [Google Scholar]
- Snyder HR, Friedman NP, & Hankin BL (2019). Transdiagnostic mechanisms of psychopathology in youth: Executive functions, dependent stress, and rumination. Cognitive Therapy and Research, 43, 834–851. doi: 10.1007/s10608-019-10016-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR, Miyake A, & Hankin BL (2015). Advancing understanding of executive function impairments and psychopathology: Bridging the gap between clinical and cognitive approaches. Frontiers in Psychology, 6, 1–24. doi: 10.3389/fpsyg.2015.00328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HR, Young JF, & Hankin BL (2017). Strong homotypic continuity in common psychopathology-, internalizing-, and externalizing-specific factors over time in adolescents. Clinical Psychological Science, 5, 98–110. doi: 10.1177/2167702616651076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L (2005). Cognitive and affective development in adolescence. Trends in Cognitive Science, 9, 69–74. [DOI] [PubMed] [Google Scholar]
- Steinberg L (2008). A social neuroscience perspective on adolescent risk-taking. Developmental Review, 28, 78–106. doi: 10.1016/j.dr.2007.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census Bureau. (2010). American community survey. Retrieved from: https://factfinder.census.gov/faces/nav/jsf/pages/searchresults.xhtml?
- White LK, Moore TM, Calkins ME, Wolf DH, Satterthwaite TD, Leibenluft E, … Gur RE (2017). An evaluation of the specificity of executive function impairment in developmental psychopathology. Journal of the American Academy of Child & Adolescent Psychiatry, 56, 975–982.e3. doi: 10.1016/j.jaac.2017.08.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams BR, Hultsch DF, Strauss EH, Hunter MA, & Tannock R (2005). Inconsistency in reaction time across the life span. Neuropsychology, 19, 88. doi: 10.1037/0894-4105.19.1.88 [DOI] [PubMed] [Google Scholar]
- Woltering S, Lishak V, Hodgson N, Granic I, & Zelazo PD (2016). Executive function in children with externalizing and comorbid internalizing behavior problems. Journal of Child Psychology and Psychiatry and Allied Disciplines, 1, 30–38. doi: 10.1111/jcpp.12428 [DOI] [PubMed] [Google Scholar]