Abstract
Background
The social and physical environments in which people live affect the emergence, prevalence, and severity of both infectious and noninfectious diseases. There are limited data on how such social determinants of health, including neighborhood socioeconomic conditions, affect the risk of severe acute respiratory syndrome coronavirus 2 infection and severity of coronavirus disease 2019 during pregnancy.
Objective
Our objective was to determine how social determinants of health are associated with severe acute respiratory syndrome coronavirus 2 infection and the severity of coronavirus disease 2019 illness in hospitalized pregnant patients in New York during the global coronavirus disease 2019 pandemic.
Study Design
This cross-sectional study evaluated all pregnant patients who delivered and had polymerase chain reaction testing for severe acute respiratory syndrome coronavirus 2 between March 15, 2020, and June 15, 2020, at 7 hospitals within Northwell Health, the largest academic health system in New York. During the study period, universal severe acute respiratory syndrome coronavirus 2 testing protocols were implemented at all sites. Polymerase chain reaction testing was performed using nasopharyngeal swabs. Patients were excluded if the following variables were not available: polymerase chain reaction results, race, ethnicity, or zone improvement plan (ZIP) code of residence. Clinical data were obtained from the enterprise electronic health record system. For each patient, ZIP code was used as a proxy for neighborhood. Socioeconomic characteristics were determined by linking to ZIP code data from the United States Census Bureau's American Community Survey and the Internal Revenue Service's Statistics of Income Division. Specific variables of interest included mean persons per household, median household income, percent unemployment, and percent with less than high school education. Medical records were manually reviewed for all subjects with positive polymerase chain reaction test results to correctly identify symptomatic patients and then classify those subjects using the National Institutes of Health severity of illness categories. Classification was based on the highest severity of illness throughout gestation and not necessarily at the time of presentation for delivery.
Results
A total of 4873 patients were included in the study. The polymerase chain reaction test positivity rate was 11% (n=544). Among this group, 359 patients (66%) were asymptomatic or presymptomatic, 115 (21%) had mild or moderate coronavirus disease 2019, and 70 (13%) had severe or critical coronavirus disease 2019. On multiple logistic regression modeling, pregnant patients who had a positive test result for severe acute respiratory syndrome coronavirus 2 were more likely to be younger or of higher parity, belong to minoritized racial and ethnic groups, have public health insurance, have limited English proficiency, and reside in low-income neighborhoods with less educational attainment. On ordinal logit regression modeling, obesity, income and education were associated with coronavirus disease 2019 severity.
Conclusion
Social and physical determinants of health play a role in determining the risk of infection. The severity of coronavirus disease 2019 illness was not associated with race or ethnicity but was associated with maternal obesity and neighborhood level characteristics such as educational attainment and household income.
Key words: COVID-19, health disparities, neighborhood characteristics, SARS-CoV-2, social determinants of health, socioeconomic conditions, ZIP code tabulation areas
AJOG MFM at a Glance.
Why was this study conducted?
There are limited data on how social determinants of health affect the risk of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and severity of coronavirus disease 2019 (COVID-19) in pregnant patients.
Key findings
Pregnant patients with SARS-CoV-2 infection were more likely to be younger, of higher parity, members of minoritized racial and ethnic groups, have public health insurance, limited English proficiency, or reside in low-income neighborhoods with higher unemployment rates, larger households, and less educational attainment. Greater neighborhood socioeconomic deprivation increases the likelihood of infection. The severity of COVID-19 was not associated with race or ethnicity but instead with maternal obesity and neighborhood characteristics such as educational attainment and household income.
What does this add to what is known?
Neighborhood socioeconomic conditions are associated with the risk of SARS-CoV-2 infection and severity of COVID-19 in pregnancy. Racial and ethnic group was associated with likelihood of infection but not severity of COVID-19 illness in pregnancy.
Introduction
Pregnant patients from minoritized racial and ethnic groups have been disproportionately affected by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes coronavirus disease 2019 (COVID-19).1, 2, 3, 4, 5 Reported risk factors for infection during pregnancy include public health insurance, obesity, higher parity, and preexisting pulmonary disease.3 However, individual patient characteristics likely provide an incomplete understanding of the mechanisms contributing to viral transmission and dissemination. The social and physical environments in which people live affect the emergence, prevalence, and severity of both infectious and noninfectious diseases. Collectively, these factors are referred to as social determinants of health (SDH); they affect overall health outcomes and quality of life and have been implicated in health disparities during the COVID-19 pandemic.5, 6, 7, 8, 9, 10
Health disparities are complex and result from numerous additive and synergistic SDH factors. These include, but are not limited to, poverty, lower educational attainment, limited English proficiency, inadequate or unaffordable housing, greater reliance on public transportation, poor insurance coverage, and unequal access to health services. Several studies have investigated how these various factors contribute to inequities in health, and many have emphasized the contributing role of institutional policies and practices.11, 12, 13 Despite evidence that structural and institutional racism can profoundly impact health outcomes, disparities have often been incorrectly attributed to differences in individual behavior and biology.14, 15, 16
Racial and ethnic disparities in maternal morbidity and mortality in the United States are, to some extent, driven by differences in neighborhood and community characteristics.17 Increasingly, structural racism has been recognized as a key driver of these differences.18 It has resulted in imbalances in housing policy, education systems, and labor markets that have contributed to an unequal distribution of disease, psychosocial stressors, and unhealthy behaviors.14 , 19 , 20 Similar policies have affected communities in New York City and Long Island.20 , 21
Persons belonging to socially marginalized groups more frequently reside in economically disadvantaged areas that contribute to poor health. Acute respiratory infections are more prevalent in communities with lower income and less education.22, 23, 24 The risk of viral exposure and transmission is exacerbated by high population density, crowded living conditions, intergenerational multifamily homes, and increased frequency of employment in essential service industries.25 , 26 Early studies of the general population during the COVID-19 pandemic have revealed that individuals belonging to socioeconomically disadvantaged groups bear a disproportionate burden of illness and death.8 , 9 Fewer studies have evaluated the association between SDH and SARS-CoV-2 infection in pregnant patients,3 , 5 and none, based on our review of the literature, have thoroughly evaluated the association between SDH and severity of COVID-19 illness in pregnancy.
In this study, we evaluated the association between SDH and SARS-CoV-2 infection in hospitalized pregnant patients in New York during the global COVID-19 pandemic. Our objective was to determine how patient demographics, medical comorbidities, and neighborhood socioeconomic factors such as household size, income, unemployment, and education level are associated with SARS-CoV-2 infection and the severity of COVID-19 illness in pregnancy.
Materials and Methods
Study population and clinical setting
This cross-sectional study evaluated all pregnant patients who delivered and had polymerase chain reaction (PCR) testing for SARS-CoV-2 between March 15, 2020, and June 15, 2020, at 7 hospitals within Northwell Health, the largest academic health system in New York. These facilities, all located in New York City and Long Island, serve a diverse population; the patients reside in both urban and suburban communities and represent a wide socioeconomic spectrum. Universal SARS-CoV-2 PCR testing protocols, using nasopharyngeal swabs, were implemented at all sites in early April 2020. Study subjects presented to the hospitals primarily for obstetrical indications. Patients were excluded if they were postpartum at presentation or if the following data were not available: PCR results, race, ethnicity, or zone improvement plan (ZIP) code. The Northwell Health Institutional Review Board approved the study as a minimal-risk research using data collected for routine clinical practice and waived the requirement for informed consent. Some patients in this study were included in previous publications characterizing COVID-19 prevalence1 , 27 and severity28, 29, 30 during pregnancy.
Data collection and external data linkage
Clinical data were obtained from the enterprise electronic health record system (Sunrise Clinical Manager, Allscripts Corp, Chicago, IL), including demographics, medical comorbidities, gestational age at presentation, and clinical outcomes. Specific SDH variables retrieved included maternal age, race, ethnicity, preferred language, type of health insurance, and ZIP code of residence. Medical records were manually reviewed for all subjects with positive PCR test results to identify symptomatic patients and then classify those subjects as having mild, moderate, severe, or critical COVID-19 using the National Institutes of Health severity of illness categories.31 Asymptomatic or presymptomatic individuals had a positive test result for SARS-CoV-2 but had no symptoms during their hospitalization. Mild illness was defined as patients who had various signs and symptoms of COVID-19 (eg, fever and cough) but without shortness of breath, dyspnea, or abnormal chest imaging. Individuals who were classified as having moderate illness had evidence of lower respiratory disease and oxygen saturation of ≥94% on room air. Those with severe illness had an oxygen saturation of <94% on room air, ratio of arterial partial pressure of oxygen to fraction of inspired oxygen of <300 mm Hg, respiratory frequency of >30 breaths/min, or lung infiltrates of >50%. Critical illness was defined by respiratory failure, septic shock, or multiple organ dysfunction.. Classification was based on the highest severity of illness throughout gestation and not necessarily at the time of presentation for delivery.
ZIP code was used as a proxy for neighborhood. Socioeconomic characteristics were determined by linking to ZIP code data from the United States Census Bureau's American Community Survey (ACS)32 and the Internal Revenue Service's Statistics of Income Division.33 The ACS data uses ZIP code tabulation areas (ZCTAs) which are areal representations produced by aggregating census blocks to closely approximate United States Postal Service (USPS) ZIP code service areas.34 Specific socioeconomic variables of interest included mean persons per household, median household income, percent unemployment, and percent with less than high school education.
Clinical outcomes and statistical analysis
The primary outcomes evaluated were SARS-CoV-2 PCR test positivity and the severity grouping for COVID-19 (asymptomatic, mild to moderate, or severe to critical). Descriptive statistics were used to characterize the data. Results are presented as mean and standard deviation or median and interquartile range, as appropriate. Comparisons for continuous variables were performed with the Mann-Whitney U test/t test, or 1-way analysis of variance (ANOVA)/Kruskal-Wallis test, as appropriate. Categorical variables were expressed as frequency and percentage. Each categorical outcome was examined using the chi-square test or Fisher exact test, as appropriate. Multiple logistic regression was performed to examine the association between positive SARS-CoV-2 PCR testing and the following potential explanatory variables: maternal age, parity, race, ethnicity, hypertension, diabetes mellitus, asthma, obesity, health insurance, preferred language, and neighborhood socioeconomic variables, as mentioned earlier. Significant predictors were selected using the stepwise bidirectional Akaike information criterion method. Ordinal logit regression modeling was used to determine the relationship between COVID-19 severity (asymptomatic, mild to moderate, or severe to critical) and the same potential explanatory variables. Odds ratios (ORs) and 95% confidence intervals (CIs) are presented. Statistical significance was defined as 2-sided P<.05. Statistical analyses were performed with RStudio 1.1.463 built on R 3.5.1 or SAS Studio 3.8 Enterprise Edition built on SAS 9.04 (SAS Institute Inc, Cary, NC).
Results
Patient characteristics and geographic distribution
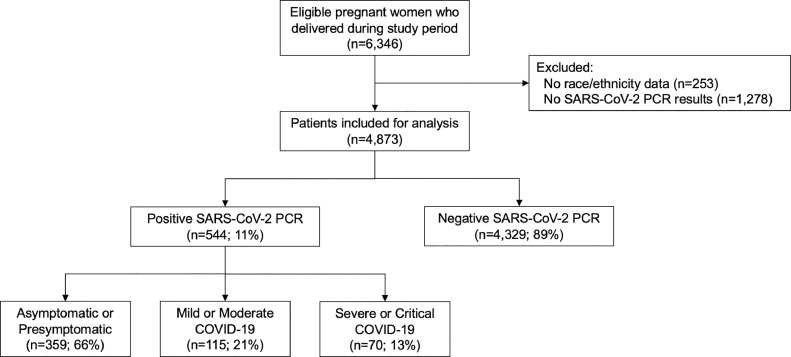
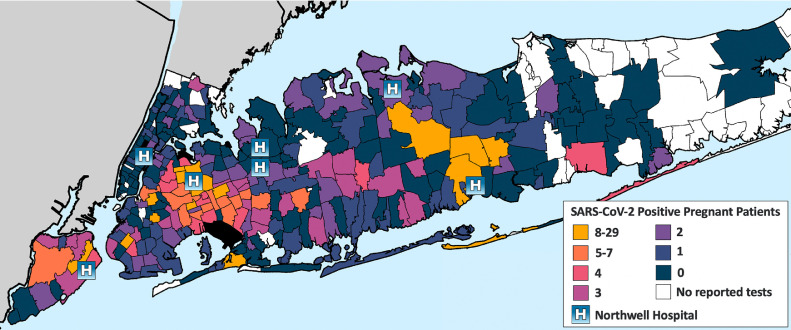
A total of 4873 patients were included in the study (Figure 1 ). Most patients (97%) had SARS-CoV-2 testing after the implementation of universal PCR testing protocols. The overall test positivity rate was 11% (n=544). Among this group, 359 patients (66%) were asymptomatic or presymptomatic, 115 (21%) had mild or moderate COVID-19, and 70 (13%) had severe or critical COVID-19. Patient demographics and clinical characteristics are summarized in Table 1 . Patients with SARS-CoV-2 infection were identified in 162 of 280 ZIP codes represented in the study population; half of the cases (n=274) and one-third of the total study population (n=1565) came from one-tenth (30) of these ZIP codes (Figure 2 ).
Figure 1.
Flowchart of study patients
COVID-19, coronavirus disease 2019; PCR, polymerase chain reaction; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Prasannan. Social determinants of health and coronavirus disease 2019. Am J Obstet Gynecol MFM 2021.
Table 1.
Patient characteristics and severe acute respiratory syndrome coronavirus 2 polymerase chain reaction test positivity
| SARS-CoV-2 PCR result |
|||
|---|---|---|---|
| Characteristic | Negative (n=4329) | Positive (n=544) | P value |
| Demographics | |||
| Maternal age, y | 32.2±5.2 | 30.5±5.8 | <.001 |
| ≥35 | 1486 (34) | 140 (26) | <.001 |
| Race and ethnicity | |||
| Non-Hispanic white | 2048 (47) | 184 (34) | <.001 |
| Non-Hispanic black | 532 (12) | 87 (16) | |
| Hispanic/Latino | 737 (17) | 176 (32) | |
| Asian | 606 (14) | 41 (8) | |
| Multiracial/other | 406 (9) | 56 (10) | |
| Paritya | |||
| 0 | 1867 (45) | 200 (38) | <.001 |
| 1 | 1427 (34) | 157 (30) | |
| 2 | 596 (14) | 86 (16) | |
| ≥3 | 301 (7) | 84 (16) | |
| BMI,b kg/m2 | 30.9±5.9 | 31.4±6.4 | .07 |
| ≥30 | 2034 (50) | 283 (52) | .38 |
| Preferred language | |||
| English | 4051 (94) | 404 (74) | <.001 |
| Non-English | 278 (6) | 140 (26) | |
| Health insurancec | |||
| Public | 1373 (32) | 319 (59) | <.001 |
| Private | 2936 (68) | 222 (41) | |
| Self-pay | 14 (0) | 3 (1) | |
| Comorbidities | |||
| Chronic hypertension | 101 (2) | 15 (3) | .53 |
| Diabetes mellitus | 38 (1) | 10 (2) | .05 |
| Asthma | 74 (2) | 10 (2) | .80 |
| Borough or county of residence | |||
| Bronx | 72 (2) | 14 (3) | <.001 |
| Brooklyn | 401 (9) | 84 (15) | |
| Manhattan | 305 (7) | 11 (2) | |
| Queens | 1471 (34) | 219 (40) | |
| Staten Island | 215 (5) | 36 (7) | |
| Nassau | 990 (23) | 72 (13) | |
| Suffolk | 662 (15) | 99 (18) | |
| Other | 213 (5) | 9 (2) | |
| Neighborhood characteristicsd | |||
| Median household income, $ | 46,410 (34,708–66,028) | 35,427 (30,215–47,381) | <.001 |
| Unemployment rate, % | 4.7 (3.9–6.2) | 5.2 (4.4–6.7) | <.001 |
| Mean persons per household | 2.9 (2.7–3.2) | 3.1 (2.8–3.5) | <.001 |
| Less than high school, % education | 15 (9–21) | 9 (4–17) | <.001 |
Data are median (interquartile range), number (percentage), and mean±standard deviation.
BMI, body mass index; PCR, polymerase chain reaction; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; ZIP, zone improvement plan.
Prasannan. Social determinants of health and coronavirus disease 2019. Am J Obstet Gynecol MFM 2021.
Parity data missing for 138 PCR negative (3%) and 17 PCR positive patients (3%)
BMI data missing for 271 PCR negative (6%) and 1 PCR positive patients (0.2%)
Health insurance missing for 6 PCR negative (0.1%) and 0 PCR positive patients (0%)
Based on ZIP code tabulation areas; 1 or more neighborhood characteristics missing for 113 PCR negative (3%) and 7 PCR positive patients (1%).
Figure 2.
SARS-CoV-2 infection in pregnant patients by ZIP Code.
ZIP, zone improvement plan.
Prasannan. Social determinants of health and coronavirus disease 2019. Am J Obstet Gynecol MFM 2021.
Social determinants of health and severe acute respiratory syndrome coronavirus 2 infection
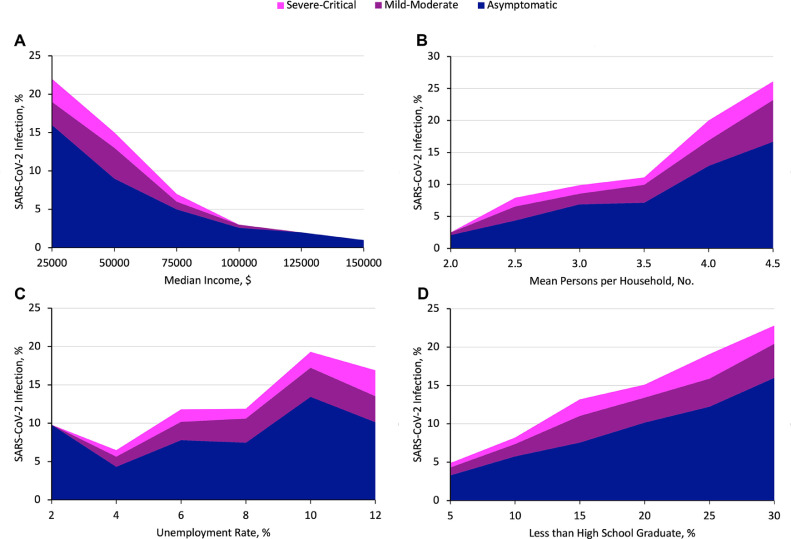
Independent-samples t tests indicated that patients who had a positive test result for SARS-CoV-2 were significantly more likely to reside in neighborhoods where the median annual household income was approximately $11,000 lower, the unemployment rate was 0.5% greater, mean household size was 0.2 persons larger, and the frequency of educational attainment less than high school was 6% higher (all P<.001). Moreover, the frequency of viral infection among study patients was further increased in areas with greater socioeconomic deprivation (Figure 3 , A–D). Chi-square analysis was used for the following comparisons (all P<.001): For neighborhoods in which median household income was less than $35,000, between $35,000 and $60,000, and greater than $60,000, the SARS-CoV-2 test positivity rates for study patients were 19%, 11%, and 5%, respectively. Unemployment rates less than 4%, between 4% and 8%, and greater than 8% were associated with SARS-CoV-2 test positivity rates for study patients of 7%, 12%, and 19%, respectively. Persons per household less than 3.0, between 3.0 and 3.5, and greater than 3.5 were associated with test positivity rates for study patients of 9%, 11%, and 21%, respectively. High school completion rates less than 10%, between 10% and 15%, and greater than 15% were associated with test positivity rates for study patients of 6%, 13%, and 18%, respectively.
Figure 3.
Association of neighborhood characteristics with SARS-CoV-2 infection and COVID-19 severity.
A, Association of neighborhood median annual household income with SARS-CoV-2 infection and COVID-19 severity. B, Association of neighborhood mean persons per household with SARS-CoV-2 infection and COVID-19 severity. C, Association of neighborhood unemployment rate with SARS-CoV-2 infection and COVID-19 severity. D, Association of neighborhood high school graduation rate with SARS-CoV-2 infection and COVID-19 severity.
COVID-19, coronavirus disease 2019; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Prasannan. Social determinants of health and coronavirus disease 2019. Am J Obstet Gynecol MFM 2021.
Despite constituting approximately one-fifth of pregnant patients, Hispanic patients accounted for nearly one-third of SARS-CoV-2 cases, as previously demonstrated by the authors.1 Non-Hispanic black patients represented 13% of the study population and accounted for 16% of SARS-CoV-2 cases. Non-Hispanic white and Asian patients were the least affected groups.
Multiple logistic regression modeling to predict SARS-CoV-2 PCR positivity yielded a number of significant associations (Table 2 ). Compared with those who had a negative test result for the virus, patients who acquired SARS-CoV-2 were more likely to be younger and to have 2 or more previous deliveries, public health insurance, and limited English proficiency. The ORs for most variables, including race and ethnicity, are less than 2, which indicates that individually their effects are relatively small. However, in combination, the results are striking. For example, on chi-square analysis, among patients who were under 35 years of age, with para 2 or greater, of black race or Hispanic ethnicity, with public health insurance, and living in neighborhoods where more than 11.2% (study mean) of the population did not complete high school, the PCR positivity rate was 26% compared with 3% for patients with the converse criteria (OR, 11.7; 95% CI, 6.1–23.0). Furthermore, among patients residing in neighborhoods with income and educational attainment above the median for the study population, racial and ethnic group was not associated with PCR positivity. In these more prosperous areas, PCR positivity was 8% for black and Hispanic patients (n=19 of 252) compared with 5% for non-Hispanic white and Asian (n=74 of 1535; P=.10 on chi-square analysis). This comparison underscores the significant income inequality in our population. Only 16% of black and Hispanic patients (n=252 of 1532) in the study live in neighborhoods with household income and educational attainment above the median compared with 58% of non-Hispanic white and Asian patients (n=1684 of 2879) (P<.001 on chi-square analysis).
Table 2.
Results of multivariable logistic regression model to predict severe acute respiratory syndrome coronavirus 2 PCR test positivity
| Characteristic | OR | 95% CI | P value |
|---|---|---|---|
| Maternal age | 0.957 | 0.937–0.977 | <.001 |
| Parity | 1.275 | 1.175–1.385 | <.001 |
| Race and ethnicitya | |||
| Asian | ref | ref | |
| Hispanic | 1.726 | 1.134–2.677 | <.02 |
| Non-Hispanic black | 1.768 | 1.144–2.776 | <.02 |
| Non-Hispanic white | 1.439 | 0.976–2.175 | .08 |
| Other/multiracial | 1.732 | 1.085–2.789 | <.03 |
| Diabetes mellitus | 2.154 | 0.981–4.345 | <.05 |
| Private vs public health insurance | 0.720 | 0.566–0.917 | <.009 |
| Preferred language, Spanish vs English | 1.670 | 1.144–2.431 | <.009 |
| Neighborhood characteristics | |||
| Median incomeb | 0.887 | 0.796–0.982 | <.03 |
| Percent less than high schoolc | 1.022 | 1.001–1.042 | <.04 |
CI, confidence interval; OR, odds ratio; PCR, polymerase chain reaction; ref, referent.
Prasannan. Social determinants of health and coronavirus disease 2019. Am J Obstet Gynecol MFM 2021.
Asian is referent based on lowest PCR positivity (6%) in the study population
Unit of median income is $10,000; OR can be explained by every unit increase of this amount
Unit of percent less than high school is 1%; OR can be explained by every unit increase of this amount.
Social determinants of health and severity of coronavirus disease 2019 illness
The characteristics associated with SARS-CoV-2 infection differed from those associated with the severity of COVID-19 illness (Table 3 ). Hispanic patients were the largest ethnic or racial group with symptomatic COVID-19 (38%), attributable to the higher infection rate in this population. However, no association was observed between racial or ethnic group and the severity of COVID-19 illness on multiple analysis. Body mass index (BMI), though not associated with PCR positivity, was associated with disease severity. The BMI of patients in the severe to critical COVID-19 group was increased compared with the asymptomatic SARS-CoV-2 positive group (32.7 vs 30.9 kg/m2; P<.04 on t test).
Table 3.
Patient characteristics and severity of coronavirus disease 2019
| Characteristic | Asymptomatic (n=359) | Mild to moderate (n=115) | Severe to critical (n=70) | P value |
|---|---|---|---|---|
| Gestational age at PCR positivity, wk | 38.8±2.3 | 37.7±3.5 | 37.7±3.3 | <.001 |
| Gestational age at delivery, wk | 39.0±2.0 | 38.3±3.0 | 38.0±2.9 | <.008 |
| Demographics | ||||
| Maternal age, y | 30.4±5.7 | 30.8±6.1 | 30.4±5.8 | .82 |
| ≥35 | 93 (26) | 32 (28) | 15 (21) | .62 |
| Race and ethnicity | ||||
| Non-Hispanic white | 140 (39) | 25 (22) | 19 (27) | <.02 |
| Non-Hispanic black | 53 (15) | 20 (17) | 14 (20) | |
| Hispanic/Latino | 106 (30) | 47 (41) | 23 (33) | |
| Asian | 25 (7) | 13 (11) | 3 (4) | |
| Multiracial/other | 35 (10) | 10 (9) | 11 (16) | |
| Paritya | ||||
| 0 | 130 (37) | 46 (42) | 24 (37) | .97 |
| 1 | 108 (31) | 30 (27) | 19 (29) | |
| 2 | 59 (17) | 17 (15) | 10 (15) | |
| ≥3 | 55 (16) | 17 (15) | 12 (18) | |
| BMI,b kg/m2 | 30.9±6 | 32.1±7 | 32.7±6 | <.05 |
| ≥30 | 176 (49) | 64 (56) | 43 (61) | .12 |
| Comorbidities | ||||
| Chronic hypertension | 7 (2) | 6 (5) | 2 (3) | - |
| Diabetes mellitus | 5 (1) | 4 (4) | 1 (1) | - |
| Asthma | 6 (2) | 2 (2) | 2 (3) | - |
| Neighborhood characteristicsc | ||||
| Median household income, $ | 35,012 (29,884–47,381) | 35,475 (30,535–47,839) | 35,451 (30,612–44,669) | .48 |
| Unemployment rate, % | 5.0 (4.3–6.6) | 5.2 (4.4–6.8) | 5.5 (4.4–6.8) | .73 |
| Mean persons per household | 3.0 (2.8–3.5) | 3.1 (2. 8–3.5) | 3.0 (2.8–3.6) | .83 |
| Less than high school, % education | 15.2 (8.8–21.3) | 14.5 (9.0–21.2) | 14.5 (10.1–21.3) | .91 |
Data are median (range), number (percentage), and mean±standard deviation.
BMI, body mass index; PCR, polymerase chain reaction.
Prasannan. Social determinants of health and coronavirus disease 2019. Am J Obstet Gynecol MFM 2021.
Parity data missing for 7 asymptomatic (2%), 5 mild to moderate (4%), and 5 severe to critical patients (7%)
BMI data missing for 1 asymptomatic patient (0%)
Based on ZIP code tabulation areas; 1 or more neighborhood characteristics missing for 6 asymptomatic (2%), 1 mild to moderate (1%), and 0 severe to critical patients (0%).
Neighborhood socioeconomic variables were not associated with COVID-19 severity group on 1-way ANOVA. However, income and education were significant on ordinal logit regression modeling, in which log transformation of those variables was performed to better fit the model (Table 4 ). For each increase of log percent less than high school education, when holding other variables constant, the likelihood of more severe COVID-19 illness group increases by 99% (OR, 1.9). Similarly, for each increase of log median income, when holding other variables constant, the likelihood of more severe COVID-19 illness group increases by 288% (OR, 3.88). Multiple analysis also demonstrated that for each increase of BMI by 1.0 kg/m2, the likelihood of more severe COVID-19 illness group increases by 3% (OR, 1.03). Maternal medical comorbidities were relatively uncommon in this population; therefore, their effect on COVID-19 severity could not be thoroughly evaluated.
Table 4.
Results of ordinal logit regression modeling to predict severity of coronavirus disease 2019
| Characteristic | OR | 95% CI | P value |
|---|---|---|---|
| Gestational age at PCR positivity | 0.901 | 0.846–0.957 | <.002 |
| BMI | 1.031 | 1.003–1.060 | <.04 |
| Neighborhood characteristicsa | |||
| Log of median income | 3.877 | 1.164–12.875 | <.03 |
| Log of percent less than high school | 1.987 | 1.092–3.640 | <.03 |
Under proportional odds assumption, the OR is considered uniform across 2 pairs of ordinal levels: (1) asymptomatic, (2) mild to moderate, and (3) severe to critical.
BMI, body mass index; CI, confidence interval; OR, odds ratio; PCR, polymerase chain reaction.
Prasannan. Social determinants of health and coronavirus disease 2019. Am J Obstet Gynecol MFM 2021.
Log transformation performed to better fit the model.
Comment
Principal findings
Pregnant patients who had a positive test result for SARS-CoV-2 were more likely to be younger or of higher parity, belong to minoritized racial and ethnic groups, have public health insurance, have limited English proficiency, have less educational attainment, and reside in low-income neighborhoods with higher unemployment rates and larger households. Importantly, patients with multiple risk factors and those living in the most socioeconomically deprived areas were even more at risk of infection. On ordinal logit regression modeling, the severity of COVID-19 illness was not associated with race or ethnicity but was associated with maternal obesity and neighborhood level characteristics such as educational attainment and household income.
Results in the context of what is known
Several overlapping and intertwined social, economic, and environmental factors have contributed to health disparities during the COVID-19 pandemic. Our results are similar to studies in the nonpregnant population which have found a disproportionate burden of SARS-CoV-2 infection among minoritized racial and ethnic groups, persons living in poverty, and those with lower educational attainment.7 , 35 A limitation of studies in the general population is that many cases with minimal or absent symptoms go undetected owing to a lack of testing or disproportionate use of testing. Early in the pandemic in New York City, non-Hispanic white residents were more likely to have testing performed even though the highest proportion of positive tests were recorded in predominantly nonwhite neighborhoods of lower socioeconomic status.36 Epidemiologic studies in pregnancy, when aided by universal testing protocols,27 , 37 provide a better understanding of the distribution of infection and disease in the larger population.
The demographic associations with SARS-CoV-2 test positivity that we observed were similar to early reports.3 , 5 We confirm that pregnant patients from minoritized racial and ethnic groups were more affected by the virus. Sakowicz et al3 speculated that an increased number of living children may be a proxy for SDH factors such as overcrowding and inability to socially distance. Indeed, we found that higher parity (≥3) was associated with greater likelihood of infection. However, in contrast to the findings of Sakowicz, we did not detect an independent association between obesity and SARS-CoV-2 test positivity in our larger series of patients. Previous studies have demonstrated an association between BMI, area of residence, and local food environment.38 , 39 In the United States, people who live in socioeconomically deprived areas are more prone to obesity40 but we did not observe a direct correlation between BMI and likelihood of infection with the virus. Furthermore, our findings do not indicate an association between medical comorbidities such as preexisting pulmonary disease and SARS-CoV-2 test positivity, but the overall frequency of such conditions in our study population was low.
Our findings regarding neighborhood characteristics and SARS-CoV-2 test positivity are similar to those of Emeruwa et al.5 In that study, which included a total of 396 pregnant patients of whom 71 were SARS-CoV-2 positive, a multivariable analysis was not included owing to the small sample size and high degree of correlation between variables. The trends that they observed for income, unemployment rate, and household size are similar to our observations. However, the authors did not evaluate the level of educational attainment in affected communities which in our analysis was statistically significantly associated with SARS-CoV-2 test positivity after controlling for other SDH variables. The relationship between specific socioeconomic indicators and health outcomes is complex. It has previously been reported that education may be more predictive than income for the onset of health conditions and that income may be more strongly associated with the progression of illness over time than education.41
Among patients with confirmed SARS-CoV-2 infection, the severity of COVID-19 illness was not as easily predicted from SDH variables. Increased BMI was associated with higher severity group, but in pregnant patients the effect seems to be small. Despite a clear association in nonpregnant populations, medical comorbidities were not associated with disease severity in our study population but, as previously mentioned, the frequency of these conditions was low. Race, ethnicity, maternal age, and parity were also not associated with severity of illness. Our observation that an increase of log median income is associated with more severe COVID-19 illness on ordinal logit regression modeling may be attributable to the higher likelihood of patients living in more affluent areas to report symptoms. This finding was driven by differences between the asymptomatic group and the mild to moderate group; there was no difference between the mild to moderate group and the severe to critical group. Patients from socioeconomically disadvantaged groups may be less likely to report symptoms owing to fear, stigmatization, or more limited and tenuous access to care. Our observation that an increase of log percent less than high school education is associated with increased disease severity in pregnant patients is consistent with early studies evaluating the relationship between educational attainment and COVID-19 complications in the general population.42 Furthermore, similar findings were reported during the H1N1 2009 influenza pandemic, in which infected patients with less than high school education were more likely to be hospitalized than those with higher educational attainment.23
Clinical implications
The populations most affected by the COVID-19 pandemic will likely be the ones most affected by subsequent infectious disease outbreaks barring large-scale public policy changes that address social inequality and health disparities. These policy changes must acknowledge the role of structural racism and focus on reducing and eliminating intergenerational transmission of health disparities. Certainly, the effect of unique sociocultural factors on health (eg, diet, religious and community beliefs, and alternative/traditional medicine) should also be considered when evaluating maternal outcomes. Populations at highest risk of infection can be localized to specific neighborhoods. In these areas, social distancing is hindered by many factors. Adequate SARS-CoV-2 testing resources and access to healthcare must be made available where it is needed most. This localization facilitates culturally and linguistically tailored and targeted health-related communications and interventions. Utilization of community organizations can aid in these efforts.
Research implications
Studies are needed to better understand how maternal and newborn outcomes have been affected by structural inequities during the pandemic. Patients from at risk populations have reduced access to care which may increase maternal morbidity and mortality even among those who are not infected with the virus.43 Public health interventions and community outreach efforts must be rigorously evaluated to determine how effectively they reduce and eliminate health disparities.
Strengths and limitations
This study has limitations, including its retrospective design. Asymptomatic infections went undetected before the implementation of universal testing. It is unknown whether the characteristics of that group differ from those included for analysis. In some cases, the illness may have worsened after discharge from the hospital and patients may have received care outside of our health system. ZCTAs were the area level unit used in our analysis. Spatial mismatch can occur between USPS ZIP codes and ZCTAs such that cases of SARS-CoV-2 are erroneously associated with nearby neighborhoods which may have substantially different socioeconomic indicators.44 In addition, census data may underrepresent undocumented immigrants who are among the most vulnerable populations. Finally, we did not evaluate individual (patient-level) income, employment, household size, or educational attainment. Therefore, we were unable to identify patients with higher household incomes who may electively reside in less affluent neighborhoods to avoid being profiled.
Our study has several strengths. The health system covers a large, diverse geographic region within the New York metropolitan area. A single record system for all hospital sites and shared institutional protocols for all obstetrical units allowed uniformity of data collection. Unlike other large registry studies,45 , 46 which only include suspected or confirmed cases of COVID-19, our study also includes all patients who had a negative test result for the virus under a universal testing protocol. Providing adequate context, with more granular data that are not geographically disaggregated, is essential when evaluating disparities.47 Data in a vacuum can lead to erroneous and dangerous conclusions that reinforce stereotypes.
Conclusions
The COVID-19 pandemic has exposed stark racial, ethnic, and socioeconomic inequities in the United States and revealed the magnitude of resulting health disparities.47, 48, 49 The same inequities that affect the general population also affect pregnant patients. Social and physical determinants of health should be considered when formulating public health strategies to mitigate the spread of SARS-CoV-2 and the disproportionate burden of COVID-19 illness in certain communities.
Acknowledgments
We would like to acknowledge the contributions of the Northwell Health COVID-19 Research Consortium. We also thank Fernando Suarez and Jonathan Amalfitano for the assistance with data retrieval and Mike Rooney for the assistance with map data visualization.
Footnotes
The authors report no conflict of interest.
The authors report no financial support.
Cite this article as: Prasannan L, Rochelson B, Shan W, et al. Social determinants of health and coronavirus disease 2019 in pregnancy. Am J Obstet Gynecol MFM 2021;XX:x.ex–x.ex.
References
- 1.Blitz MJ, Rochelson B, Prasannan L, et al. Racial and ethnic disparity and spatiotemporal trends in severe acute respiratory syndrome coronavirus 2 prevalence on obstetrical units in New York. Am J Obstet Gynecol MFM. 2020;2 doi: 10.1016/j.ajogmf.2020.100212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ellington S, Strid P, Tong VT, et al. Characteristics of women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status - United States, January 22-June 7, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:769–775. doi: 10.15585/mmwr.mm6925a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sakowicz A, Ayala AE, Ukeje CC, Witting CS, Grobman WA, Miller ES. Risk factors for severe acute respiratory syndrome coronavirus 2 infection in pregnant women. Am J Obstet Gynecol MFM. 2020;2 doi: 10.1016/j.ajogmf.2020.100198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Emeruwa UN, Spiegelman J, Ona S, et al. Influence of race and ethnicity on severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection rates and clinical outcomes in pregnancy. Obstet Gynecol. 2020;136:1040–1043. doi: 10.1097/AOG.0000000000004088. [DOI] [PubMed] [Google Scholar]
- 5.Emeruwa UN, Ona S, Shaman JL, et al. Associations Between built environment, neighborhood socioeconomic status, and SARS-CoV-2 infection Among pregnant women in New York City. JAMA. 2020;324:390–392. doi: 10.1001/jama.2020.11370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DiMaggio C, Klein M, Berry C, Frangos S. Black/African American communities are at highest risk of COVID-19: spatial modeling of New York City ZIP code-level testing results. Ann Epidemiol. 2020;51:7–13. doi: 10.1016/j.annepidem.2020.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Figueroa JF, Wadhera RK, Lee D, Yeh RW, Sommers BD. Community-level factors associated With racial and ethnic disparities in COVID-19 rates in Massachusetts. Health Aff (Millwood) 2020;39:1984–1992. doi: 10.1377/hlthaff.2020.01040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maroko AR, Nash D, Pavilonis BT. COVID-19 and inequity: a comparative spatial analysis of New York City and Chicago hot spots. J Urban Health. 2020;97:461–470. doi: 10.1007/s11524-020-00468-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Whittle RS, Diaz-Artiles A. An ecological study of socioeconomic predictors in detection of COVID-19 cases across neighborhoods in New York City. BMC Med. 2020;18:271. doi: 10.1186/s12916-020-01731-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Azar KMJ, Shen Z, Romanelli RJ, et al. Disparities in outcomes Among COVID-19 patients in A large health care system in California. Health Aff (Millwood) 2020;39:1253–1262. doi: 10.1377/hlthaff.2020.00598. [DOI] [PubMed] [Google Scholar]
- 11.Ford CL, Airhihenbuwa CO. The public health critical race methodology: praxis for antiracism research. Soc Sci Med. 2010;71:1390–1398. doi: 10.1016/j.socscimed.2010.07.030. [DOI] [PubMed] [Google Scholar]
- 12.Ford CL, Airhihenbuwa CO. Critical Race Theory, race equity, and public health: toward antiracism praxis. Am J Public Health. 2010;100(Suppl1):S30–S35. doi: 10.2105/AJPH.2009.171058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Griffith DM, Mason M, Yonas M, et al. Dismantling institutional racism: theory and action. Am J Community Psychol. 2007;39:381–392. doi: 10.1007/s10464-007-9117-0. [DOI] [PubMed] [Google Scholar]
- 14.Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health. 2011;32:381–398. doi: 10.1146/annurev-publhealth-031210-101218. [DOI] [PubMed] [Google Scholar]
- 15.Braveman P, Gottlieb L. The social determinants of health: it's time to consider the causes of the causes. Public Health Rep. 2014;129(Suppl2):19–31. doi: 10.1177/00333549141291S206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Petersen EE, Davis NL, Goodman D, et al. Racial/ethnic disparities in pregnancy-related deaths—United States, 2007-2016. MMWR Morb Mortal Wkly Rep. 2019;68:762–765. doi: 10.15585/mmwr.mm6835a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Howell EA. Reducing disparities in severe maternal morbidity and mortality. Clin Obstet Gynecol. 2018;61:387–399. doi: 10.1097/GRF.0000000000000349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Institute for Children's Health Quality website. The impact of institutional racism on maternal and child health. Available at:https://www.nichq.org/insight/impactinstitutional-racism-maternal-and-child-health. Accessed January 20, 2021.
- 19.Chadha N, Lim B, Kane M, Rowland B. What are racial health disparities and why do they exist. Toward the Abolition of biological Race in Medicine. Institute for Healing and Justice. Available at:https://issuu.com/instituteforhealingandjustice/docs/toward_the_abolition_of_biological_race_in_medicin/s/10750471. Accessed January 20, 2021.
- 20.Kucsera J, Orfield G. UCLA: the civil rights project /proyecto Derechos civiles; 2014. New York State's extreme school segregation: inequality, inaction and a damaged future.https://escholarship.org/uc/item/5cx4b8pf Available at: Accessed January 20, 2021. [Google Scholar]
- 21.Mead J. Memories of segregation in Levittown. New York Times. Available at:https://www.nytimes.com/2003/05/11/nyregion/memories-of-segregation-in-levittown.html. Accessed January 27, 2021.
- 22.Balter S, Gupta LS, Lim S, Fu J, Perlman SE, New York City 2009 H1N1 Flu Investigation Team Pandemic (H1N1) 2009 surveillance for severe illness and response, New York, New York, USA, April-July 2009. Emerg Infect Dis. 2010;16:1259–1264. doi: 10.3201/eid1608.091847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lowcock EC, Rosella LC, Foisy J, McGeer A, Crowcroft N. The social determinants of health and pandemic H1N1 2009 influenza severity. Am J Public Health. 2012;102:e51–e58. doi: 10.2105/AJPH.2012.300814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stone AA, Krueger AB, Steptoe A, Harter JK. The socioeconomic gradient in daily colds and influenza, headaches, and pain. Arch Intern Med. 2010;170:570–572. doi: 10.1001/archinternmed.2010.20. [DOI] [PubMed] [Google Scholar]
- 25.Blumenshine P, Reingold A, Egerter S, Mockenhaupt R, Braveman P, Marks J. Pandemic influenza planning in the United States from a health disparities perspective. Emerg Infect Dis. 2008;14:709–715. doi: 10.3201/eid1405.071301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Levy NS, Nguyen TQ, Westheimer E, Layton M. Disparities in the severity of influenza illness: a descriptive study of hospitalized and nonhospitalized novel H1N1 influenza-positive patients in New York City: 2009-2010 influenza season. J Public Health Manag Pract. 2013;19:16–24. doi: 10.1097/PHH.0b013e31824155a2. [DOI] [PubMed] [Google Scholar]
- 27.Blitz MJ, Rochelson B, Rausch AC, et al. Universal testing for coronavirus disease 2019 in pregnant women admitted for delivery: prevalence of peripartum infection and rate of asymptomatic carriers at four New York hospitals within an integrated healthcare system. Am J Obstet Gynecol MFM. 2020;2 doi: 10.1016/j.ajogmf.2020.100169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Blitz MJ, Grünebaum A, Tekbali A, et al. Intensive care unit admissions for pregnant and nonpregnant women with coronavirus disease 2019. Am J Obstet Gynecol. 2020;223:290–291. doi: 10.1016/j.ajog.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Blitz MJ, Rochelson B, Minkoff H, et al. Maternal mortality among women with coronavirus disease 2019 admitted to the intensive care unit. Am J Obstet Gynecol. 2020;223 doi: 10.1016/j.ajog.2020.06.020. 595–599.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pachtman Shetty SL, Meirowitz N, Blitz MJ, Gadomski T, Weinberg CR. Myocardial injury associated with coronavirus disease 2019 in pregnancy. Am J Obstet Gynecol. 2021;224:229–232. doi: 10.1016/j.ajog.2020.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.National Institutes of Health. COVID-19 treatment guidelines panel. Coronavirus Diseases 2019 (COVID-19) treatment guidelines. Available at:https://www.covid19treatmentguidelines.nih.gov/overview/management-of-covid-19/. Accessed May 16, 2020. [PubMed]
- 32.United States Census Bureau. American Community Survey (ACS). Available at:https://www.census.gov/programs-surveys/acs. Accessed August 6, 2020.
- 33.Internal Revenue Service (IRS). SOI Tax Stats—statistics of income. Available at:https://www.irs.gov/statistics/soi-tax-stats-statistics-of-income. Accessed August 6, 2020.
- 34.United States Census Bureau. ZIP code tabulation areas (ZCTAs). Available at:https://www.census.gov/programs-surveys/geography/guidance/geo-areas/zctas.html. Accessed September 22, 2020.
- 35.Wadhera RK, Wadhera P, Gaba P, et al. Variation in COVID-19 hospitalizations and deaths Across New York City boroughs. JAMA. 2020;323:2192–2195. doi: 10.1001/jama.2020.7197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lieberman-Cribbin W, Tuminello S, Flores RM, Taioli E. Disparities in COVID-19 testing and positivity in New York City. Am J Prev Med. 2020;59:326–332. doi: 10.1016/j.amepre.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vintzileos WS, Muscat J, Hoffmann E, et al. Screening all pregnant women admitted to labor and delivery for the virus responsible for coronavirus disease 2019. Am J Obstet Gynecol. 2020;223:284–286. doi: 10.1016/j.ajog.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Booth KM, Pinkston MM, Poston WS. Obesity and the built environment. J Am Diet Assoc. 2005;105(Suppl 1) doi: 10.1016/j.jada.2005.02.045. S110–7. [DOI] [PubMed] [Google Scholar]
- 39.Murphy M, Badland H, Jordan H, Koohsari MJ, Giles-Corti B. Local food environments, suburban development, and BMI: a mixed methods study. Int J Environ Res Public Health. 2018;15 doi: 10.3390/ijerph15071392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Levine JA. Poverty and obesity in the U.S. Diabetes. 2011;60:2667–2668. doi: 10.2337/db11-1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Herd P, Goesling B, House JS. Socioeconomic position and health: the differential effects of education versus income on the onset versus progression of health problems. J Health Soc Behav. 2007;48:223–238. doi: 10.1177/002214650704800302. [DOI] [PubMed] [Google Scholar]
- 42.Wiemers EE, Abrahams S, AlFakhri M, Hotz VJ, Schoeni RF, Seltzer JA. Disparities in vulnerability to complications from COVID-19 arising from disparities in preexisting conditions in the United States. Res Soc Stratif Mobil. 2020;69 doi: 10.1016/j.rssm.2020.100553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Minkoff H. You don't have to be infected to suffer: COVID-19 and racial disparities in severe maternal morbidity and mortality. Am J Perinatol. 2020;37:1052–1054. doi: 10.1055/s-0040-1713852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Grubesic TH, Matisziw TC. On the use of ZIP codes and ZIP code tabulation areas (ZCTAs) for the spatial analysis of epidemiological data. Int J Health Geogr. 2006;5:58. doi: 10.1186/1476-072X-5-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Afshar Y, Gaw SL, Flaherman VJ, et al. Clinical presentation of coronavirus Disease 2019 (COVID-19) in pregnant and recently pregnant people. Obstet Gynecol. 2020;136:1117–1125. doi: 10.1097/AOG.0000000000004178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Delahoy MJ, Whitaker M, O'Halloran A, et al. Characteristics and maternal and birth outcomes of hospitalized pregnant women with laboratory-confirmed COVID-19 - COVID-NET, 13 states, March 1-August 22, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1347–1354. doi: 10.15585/mmwr.mm6938e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chowkwanyun M, Reed AL., Jr Racial health disparities and Covid-19 - caution and context. N Engl J Med. 2020;383:201–203. doi: 10.1056/NEJMp2012910. [DOI] [PubMed] [Google Scholar]
- 48.Berkowitz SA, Cené CW, Chatterjee A. Covid-19 and health equity - time to think big. N Engl J Med. 2020;383:e76. doi: 10.1056/NEJMp2021209. [DOI] [PubMed] [Google Scholar]
- 49.Egede LE, Walker RJ. Structural racism, social risk factors, and Covid-19 - a dangerous convergence for Black Americans. N Engl J Med. 2020;383:e77. doi: 10.1056/NEJMp2023616. [DOI] [PMC free article] [PubMed] [Google Scholar]