Abstract
Pericardial effusion may be the tipping point to unravel hypothyroidism. Large effusions may not correlate with severity of cardiovascular compromise. Medical therapy over surgical intervention is appropriate if no evidence of cardiac tamponade.
Keywords: hypothyroidism, myxedema, pericardial disease, pericardial effusion
Pericardial effusion may be the tipping point to unravel hypothyroidism. Large effusions may not correlate with severity of cardiovascular compromise. Medical therapy over surgical intervention is appropriate if no evidence of cardiac tamponade.
1. CASE HISTORY
Primary hypothyroidism has been associated with many undue adverse effects. Its cardiovascular manifestations include reductions in heart rate and contractility with the development of hypertension, angina, heart failure, and pericardial effusion consistent with hypothyroid heart. Early recognition and treatment can help mitigate these advanced features.[1]
Question: What are the cardiac implications of untreated hypothyroidism?
Answer: We present a case of pericardial effusion from primary hypothyroidism.
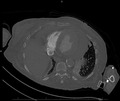
A 70‐year‐old woman with a history of chronic obstructive pulmonary disease (COPD), chronic arthritis with no documented hypothyroidism presented to the emergency department with dyspnea evolving over the last month, generalized weakness, and arthritic pain. Initial vitals were notable for bradycardia and hypoxia, with an oxygen saturation of 80% necessitating supplemental oxygen. She was awake, was appeared frail, and was not in acute distress. The examination revealed muffled heart sounds, jugular venous distention, and features consistent generalized myxedema (Figure 1). Initial workup revealed pancytopenia with macrocytosis and revealed an unremarkable chemistry panel with a brain natriuretic peptide (BNP) of 133.4 PG/ML. Imaging revealed cardiomegaly and pulmonary congestion on chest radiography (Figure 2), while computerized tomography (CT) chest with contrast revealed a moderate to large pericardial effusion (Figure 3). Thyroid‐stimulating hormone (TSH) was 102.94 UIU/ML (normal range 0.30‐5.50 UIU/ML) with a free T4 less than 0.1 NG/DL (normal range 0.9‐1.8 NG/DL). A transthoracic echocardiogram confirmed a large circumferential pericardial effusion without tamponade physiology and severe concentric left ventricular hypertrophy (Figure 4). She was initially treated with a single dose of intravenous levothyroxine 300 mcg, followed by 100 mcg daily. Also received hydrocortisone 50 mg every 8 hours. Following clinical improvement was transitioned to oral levothyroxine 100 mcg daily, and hydrocortisone was slowly discontinued. Repeat echocardiogram prior to discharge revealed significant improvement, showing only moderate effusion adjacent to the left ventricle. She was discharged on an oral course of levothyroxine with close follow‐up with a cardiologist.
FIGURE 1.

Myxedema demonstrating features of hypothyroidism
FIGURE 2.
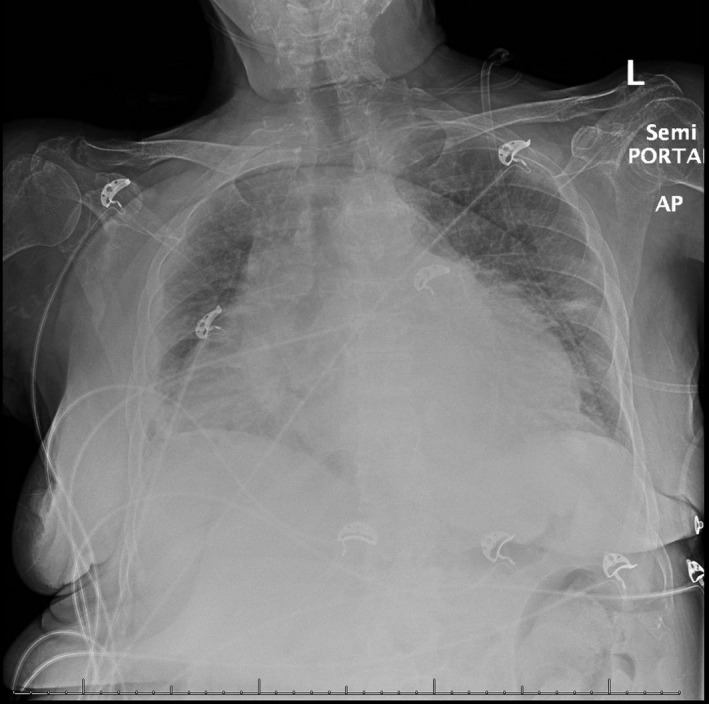
Chest radiograph demonstrating enlarged cardiac silhouette
FIGURE 3.

Computerized Tomography (CT) demonstrating large pericardial effusion
FIGURE 4.
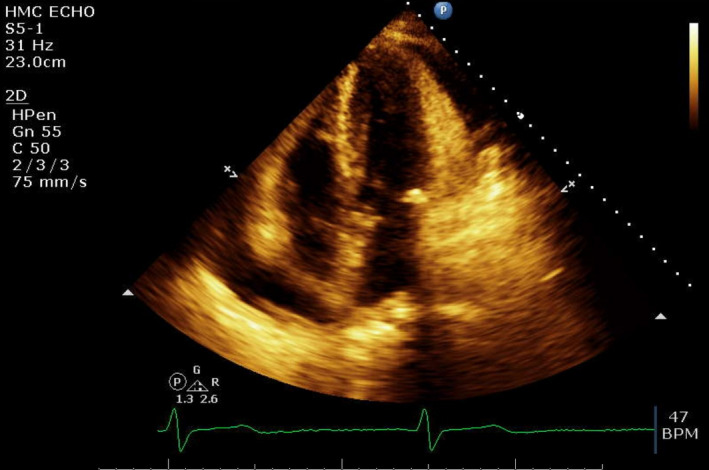
Transthoracic echocardiogram with four‐chamber view showing pericardial effusion
CONFLICT OF INTEREST
None to declare.
AUTHOR CONTRIBUTIONS
Anoosha Ponnapalli: designed the manuscript, collected the data, and reviewed the manuscript. Smit S. Deliwala: collected the data, prepared the manuscript, and reviewed the manuscript. Yazan Zayed: reviewed the manuscript. Ghassan Bachuwa: reviewed the manuscript.
ETHICAL STATEMENT
Informed consent was obtained from the patient for the publication of this case report.
ACKNOWLEDGMENTS
Published with written consent of the patient.
Ponnapalli A, Deliwala SS, Zayed Y, Bachuwa G. Pericardial effusion uncovering underlying hypothyroidism. Clin Case Rep. 2021;9:1816–1818. 10.1002/ccr3.3857
DATA AVAILABILITY STATEMENT
Data sharing was not applicable as no datasets were generated or analyzed for this article.
REFERENCES
- 1. Chahine J, Ala CK, Gentry JL, Pantalone KM, Klein AL. Pericardial diseases in patients with hypothyroidism. Heart. 2019;105(13):1027‐1033.. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing was not applicable as no datasets were generated or analyzed for this article.


