During a 4-week quit attempt, Asian American smokers were more successful in avoiding smoking when they received a reminder of their own intention just before a self-identified risky situation on a familiar device and when they followed through with specified plans
Keywords: Just-in-time intervention, Implementation intention, Cessation, Asian American young adults, Within-person randomization
Abstract
Identifying vulnerable windows for a given problematic behavior and providing timely and appropriate support are critical for building an effective just-in-time (JIT) intervention for behavioral change. We developed and evaluated an implementation intention (II) based, JIT cessation intervention prototype to support Asian American young adult smokers to prevent lapses in their cessation attempts in real-time. We examined how a JIT II reminder may prevent lapses during self-identified high-risk smoking situation (HRSS) as a microtemporal process. We also tested whether the effect of JIT reminder changes over the course of study and differed between those who used their own versus project loan phones. Asian American young adult smokers (N = 57) who were interested in quitting or reducing smoking participated in a 4 week, mobile-based, cessation study (MyQuit USC, MQU). MQU is a JIT mobile app that deploys a user-specified II reminder at user-specified HRSS and assesses momentary lapse status. Generalized mixed linear models were conducted to assess the effect of the JIT intervention on lapse prevention. We found a significant interaction effect (p = .03) such that receiving JIT reminder reduced the likelihood of lapses for participants using their own phones but not for the loaners. The results also showed that when participants enacted the suggested II, they were less likely to lapse (p < .001). The JIT effect did not change over time in study (p = .21). This study provides evidence that receiving a reminder of a smoker’s own plan just before a self-identified risky situation on a familiar device and successfully executing specified plans can be helpful in preventing lapses. Our results highlighted factors to consider when designing and refining a JIT intervention.
Implications.
Practice: Receiving a reminder of a smoker’s own intention just before a self-identified risky situation can be helpful in preventing lapses among Asian American young adult smokers.
Policy: Policymakers working on decreasing combustible cigarette use among minority young adults are recommended to incorporate large-scale, just-in-time (JIT), tailored interventions to existing cessation aid services.
Research: Future research should continue to investigate microtemporal contextual moderators for behavioral change that can be used to optimize the effectiveness of the JIT interventions.
INTRODUCTION
With advancement in technology, just-in-time (JIT) personalized interventions have been suggested as effective methods that could promote changes in a wide variety of health behaviors [1–5]. A JIT intervention is operationalized as a timely, relevant type of support, that is delivered only when it is required and appropriate in order to facilitate desired behavioral changes [3,6]. Despite its potential role in supporting behavior change, researchers have noted a disconnect between current technological capacity and existing behavioral theories to guide the development of JIT interventions [3,7].
A pragmatic behavioral framework is needed that identifies specific moments preceding risky behaviors (i.e., behavioral antecedents) unique to a person, such as time of the day or location. It has been suggested that such a framework be couched in individualized ecological contexts, such as presence or absence of social support or levels of exposure to cues associated with a certain behavior, that may be static or dynamic over time [7]. These moments can be prioritized as vulnerable windows for problematic behavior and timely opportunities (when a person is receptive) for potential intervention. The timeliness (i.e., when) and content (i.e., construct to target in order to encourage behavioral change) of effective interventions for a given behavior is an area of active research. The current study exemplifies this research effort in developing and evaluating a JIT intervention prototype to support Asian American young adult smokers to prevent early lapses in their cessation attempts in real time.
Deciding when to intervene: identifying windows of vulnerability for a target behavior
Identifying the temporal and contextual windows associated with a given problematic health behavior is an empirical task because, often, guidance found in the literature on such windows is scant [7]. Moreover, timepoints dependent on socioecological constructs specific to a broad population may not generalize to understudied populations, such as Asian Americans. Similarly, available theories may be too general because the time “windows” would depend on how one thinks about timescales (defined as “the size of temporal intervals used to develop or test a theory”) for a given behavior [7, p. 1212]. Accurate prediction of the exact time when a smoker is about to light up a cigarette (in minutes or seconds) may be necessary to deploy appropriate JIT cessation support in real time. To identify these windows of vulnerability, researchers have employed various strategies that trigger JIT cessation support prompted either by users, programmed schedules or algorithms, or combination of both. Some mobile cessation apps have relied on smokers themselves to request JIT support when they experience craving although such user-triggered methods typically lead to low use [8–10]. Others have employed automated methods where support is sent out on fixed or variable schedules [11,12] or sensor-assisted, context-sensitive systems [13–15]. One of the few similar studies used machine-learning methods to identify windows of vulnerability using a real-time self-reported sampling strategy known as ecological momentary assessment (EMA) in tandem with GPS-assisted virtual boundaries (i.e., geofencing) [2]. These devices and methods, however, have been mostly tested in highly controlled settings and offer insufficient accuracy for identifying windows of vulnerability to justify user burden. Problems with feasibility and sustainability of wearing or carrying devices during a cessation attempt are also of concern [2].
Young adult Asian American smokers as a high-risk/priority population
Although overall cigarette smoking rates among Asian Americans appear to be lower than the national average [16], this group show substantial subgroup variation in the prevalence of cigarette smoking, ranging from 7.6% (Chinese and Indians) to 20% (Koreans; CDC) [17]. Recent research also highlights the need for culturally tailored tobacco-control surveillance efforts, such as including non-English-speaking participants and community-participatory research methods when collecting survey data [18] to capture more accurate prevalence rates of tobacco use among younger segments of these ethnic groups. Young adult smokers are also more likely to be “light” or “intermittent” smokers, which may be associated with unique barriers during cessation attempts despite low levels of nicotine addiction [19–21]. Furthermore, these individuals are often immersed in environments where smoking is culturally encouraged and socially functional [22]. The existing research has examined the effectiveness of more conventional approaches, such as telephone quitlines [23], culturally tailored face-to-face [24] or telephone or video [25] individual counseling, family-based telephone counseling [26], nicotine replacement therapy (NRT) [27], NRT combined with motivational interviewing [28], and web-based intervention [29]. To date, the current study represents one of the first attempts to pilot test an implementation intention (II) based, JIT cessation intervention, specifically targeting young Asian American adult smokers.
From our previous formative research involving both quantitative and qualitative data obtained from Asian American young adult smokers [30], we learned that these smokers were typically aware of the times and/or the contexts in which they would light up a cigarette within a day. These smokers often describe that smoking is “culturally functional” in enhancing or maintaining social bonding [31,32] and emphasize its close cultural tie with food and drinking [22]. These young adults also visit places (e.g., restaurants and bars in ethnic enclaves) that could trigger smoking urge as cigarette use is highly prevalent and deemed as a cultural norm [33]. Although we had initially considered incorporating real-time locational data, we reasoned that battery drainage issues and detection inaccuracy associated with location-based technology would add burden to participants. Thus, the current study expanded upon our formative research and employed a feasible and scalable approach to automate personalized JIT support for prerecorded, user-specified windows of vulnerability for lapse or high-risk smoking situations (HRSSs). Specifically, the JIT architecture in this study requested smokers to identify and record HRSS windows (defined by hours on a given day) in the form of a calendar-based system prior to starting their quit attempt. This information was used to deploy automated and personalized JIT support for each HRSS window per smokers’ individual daily schedules.
Deciding on what JIT support to deploy: role of relevant II reminders
Forming IIs [34] to perform a behavior has been theorized to assist people in making various behavioral changes [35–37], including smoking cessation [38–40]. IIs refer to plans specifying where and when to initiate a particular action by creating specific behavioral responses (e.g., I will leave my cigarettes in my trunk) to specific cues (e.g., when I drive) [34,37] and have been shown to be effective in pursuing a chronic or complex goal (e.g., remain abstinent) [41,42]. Compared to goal intentions, IIs represent more automated goal-striving strategies that require less cognitive effort to initiate and perform the intended behavior. Over time, successfully executing these plans would promote self-regulation and facilitate goal intentions during specific times or contexts [34]. Gollwitzer and Sheeran [37] contended that IIs facilitate forming new habits via establishment and automation of an “if-then” behavioral chain (e.g., when I “wake up in the morning” and I will “brush my teeth” instead of “smoking”). As these concrete II plans become a habit to encourage or substitute a given behavior over time, IIs are also believed to help one recognize relevant cues and contexts in an enhanced manner.
Because IIs are concrete, specific plans tied to highly personalized contexts, they may be particularly effective when delivered in a JIT fashion, such as a reminder. However, it is noteworthy that a large volume of the existing literature on II interventions has primarily focused on assessing their effectiveness on cessation outcomes either at nonintensive time intervals (e.g., between-group pre–post design [39,43] or in between-group longitudinal designs with monthly measures [44]) and/or in laboratory settings [45,46]. Thus, additional work is needed to determine whether IIs, when delivered JIT during HRSS in the form of II reminders, are effective when assessed in more detailed microtemporal timescales, such as hours within a day.
The current study
In this current study, we investigated the effect of JIT II reminders on reducing momentary lapses during a mobile-supported smoking cessation attempt among Asian American young adults by assessing the lapse outcome in near real time. Further, our study design allowed us to assess whether the user-specified II was indeed executed in an effort of avoiding momentary lapses. Therefore, we examined how an II reminder and subsequent enactment may prevent lapse during HRSS as a microtemporal process and hypothesized the following a priori:
H1: On average, participants would be less likely to lapse when receiving an II reminder during a personalized HRSS than when not receiving the reminder.
H2: Successfully enacting prespecified IIs would decrease the likelihood of momentary lapses.
Furthermore, as our JIT intervention, MyQuit USC (MQU), is compatible only with the Android platform and only about a third of the sample (n = 16, 28%) interacted with MQU on their own phones, we include the phone type (loan vs. own phone) as a person-level moderator. In addition, exit interviews informed us that how far along a smoker is within the 4 week cessation period is another important moderator to consider when assessing JIT II effectiveness. Participants mentioned that the second and third weeks of the quit attempt were notable time points. During these weeks, some participants reported that they became more motivated to follow their II reminders and enact their IIs, while others lost interest in engaging with MQU features altogether or found the quit process too difficult. As we were interested in studying the habit-formation process during cessation attempts, we consider the passage of time since the beginning of quit attempt as a highly relevant contextual factor for JIT effectiveness and, therefore, examined whether the JIT effect is consistent throughout the cessation period. Thus, we formally tested the following exploratory hypotheses:
H3: The effect of JIT reminder on lapse avoidance would be stronger for those participants who interacted with MQU on their own Android phones.
H4: For H1 and H2, the effect of JIT reminder would decrease over the cessation period, as we postulated that HRSS recognition and II enactment would become increasingly more habitual for participants.
METHODS
Participants
Participants were Asian American, English-speaking, young adult daily smokers (18–25 years of age; self-identified Asian Americans; and combustible cigarette users who smoked 5+ days/week) who wanted to reduce or quit smoking. For recruitment, we targeted social media sites of community organizations and local college campuses in Southern California. Study flyers were also distributed at special events or places where these adults tend to congregate (e.g., popular restaurants and bars). Out of 153 participants who had been recruited and/or had initially contacted us, 52 could not be reached after several attempts, 9 were no longer interested, and 28 were ineligible. Sixty-four individuals were enrolled, 7 of whom either voluntarily dropped out or we ended their participation before completion due to persistently poor (<50%) compliance with the study protocols. Therefore, the final person-level sample size was 57 Asian American young adult smokers. Power calculations for Level-2 sample size were not conducted a priori given the pilot nature of the current study.
MQU protocols
The University of Southern California Institutional Review Board approved all research procedures of the study. The full details on the MQU app development via formative research have been published elsewhere [30]. To briefly summarize the protocol details relevant for the current study, MQU is a JIT mobile phone cessation app that deploys a user-specified II reminder in a JIT manner (i.e., 10 min prior to a user-specified HRSS hour) for 4 weeks.
To assess whether receiving an II reminder reduces the likelihood of momentary lapse, we randomized whether or not the system sent out the personalized II reminder at each HRSS window, at a 75% rate (i.e., within-person randomization). In other words, each participant was prompted with a push notification containing their own personalized II reminders corresponding to each HRSS, only 75% of the time. Borrowing the JIT framework terminology, each HRSS for an individual participant was a decision point [7]. Subsequently, the momentary lapse outcome was assessed via a brief EMA survey at 45 min after the beginning of every user-specified HRSS hour window (e.g., 9:45 am in an HRSS-specified window as 9:00–10:00 am). MQU has additional features where participants can record non-HRSS lapses (“Oops I smoked!”) and where they can prompt II reminders on demand (“I’m craving a cigarette!”). Participants also responded to a brief end-of-the-day survey each night at a specified time. The system also logged interaction data (e.g., whether a participant viewed the JIT prompt and the frequency of landing on MQU home page). The current study focuses on the momentary lapse data as the outcome.
Procedures
The data were collected from February 2016 to June 2018. During the initial meeting with trained research assistants, participants provided informed consent and completed a 20 min baseline survey on demographic characteristics and smoking-related history, including nicotine dependence assessed with Fagerstrom Test of Nicotine Dependence (FTND) [47]. After completing the survey, research assistants helped participants set up an account on MQU.
Given MQU’s compatibility only with the Android platform, we distributed a loan phone if the participant owned an iPhone (n = 41, 72% of the sample). If participants owned an Android, we helped them download the MQU app on their own phones. Once logged in, participants were asked to select their desired quit date within the following 10 days and input the quit date in the system. Afterward, participants were asked to compile their personalized HRSS on the customized MQU calendar along with corresponding II reminders. Participants were encouraged to specify their own unique HRSSs and IIs; the MQU app also presented prepopulated suggestions for HRSSs and IIs from which participants could select. Participants were required to compile at least five HRSSs each day (up to maximum 24 HRSSs). Therefore, each time block entry a participant selected within a day was linked to a specific context (i.e., situation) and/or time window associated with personalized HRSS and was targeted in the intervention. To streamline the input process, participants could opt to copy daily schedules for weekdays and separately for weekends. This initial meeting took approximately 30–60 min.
To minimize missing data, trained researchers monitored participants’ EMA and end-of-day survey data daily and contacted participants via their personal phones to encourage their participation when compliance rates fell below 80%. Upon completion of the 4 week quit attempt with MQU, we conducted approximately 1 h semistructured exit interviews focusing on user experience/engagement and their quit processes. The exit interviews were audio-taped and transcribed verbatim by research assistants. Participants received up to $200 (~$7/day for completed surveys) for their participation.
Measures
Independent variable
The within-person, JIT II reminder randomization sent out 10 min prior to a user-specified HRSS was the main predictor (when II reminder sent = 1; when II reminder not sent = 0).
Dependent variable
After every HRSS, upon which MQU reminded participants what the scheduled HRSS was, participants were asked whether they smoked (yes = 1, no = 0) during the given HRSS. This momentary lapse status was the primary dependent variable for this study.
Covariates
At each post-HRSS EMA, participants were also asked to indicate whether they followed through with their specified II plan for a given HRSS (yes/no). The MQU system also logged whether a participant viewed the II reminder when the notification arrived by opening the notification and clicking “Okay” (hereafter “acknowledged”). This prompt-level interaction was aggregated to calculate person-level averages; we use this variable as a proxy for each participant’s level of exposure to the II reminders.
Contextual moderators
As our participants informed us of the significance of time passage during their quit process, we considered weeks in study as an important, within-person contextual moderator. The phone type (loan = 1 vs. own phone = 0), a person-level, study design-related moderator, was also included as an effect modifier.
Statistical analyses
A set of four generalized mixed linear models were conducted to predict the likelihood of momentary lapse, using SAS 9.4. For Model 1, the main predictor was the JIT II reminder status (H1; 1= II reminder sent, 0 = II reminder not sent). Subsequently, we tested the effect of enacting the II on momentary lapses (H2), controlling for the person-level exposure proxy variable, study week, and phone type (Model 2). In Model 3, we tested the II effect moderation by phone type (H3) by including an interaction term between II reminder and phone type. In Model 4, we included additional interaction terms by time in study (H4).
RESULTS
Descriptive statistics for person- and prompt-level characteristics are provided in Table 1.
Table 1.
Descriptive statistics
| Person level (N = 57) | M (SD)/n(%) |
|---|---|
| Age | 21.72 (2.14) |
| Female | 13 (22.8%) |
| Ethnicity | |
| Korean American | 48 (84.2%) |
| Chinese American | 6 (10.5%) |
| Japanese American | 1 (1.7%) |
| Vietnamese American | 1 (1.7%) |
| Indian American | 1 (1.7%) |
| FTND total score | 2.56 (2.03) |
| Number of days smoked last week | 6.23 (0.91) |
| Number of cigarettes per day last week | 4.58 (0.78) |
| Began smoking before 15 years | 33 (57.9%) |
| Have tried to quit in the past | 44 (77.19%) |
| Vaped for ≥1 days during MQU | 20 (35.09%) |
| Used own Android phone | 16 (28.07%) |
| II randomization rate | 74.50 (4.03) |
| Post-HRSS EMA compliance rate | 58.70 (21.82) |
| II reminder acknowledgment rate | 52.68 (22.27) |
| Momentary lapse rate | 16.44 (18.15) |
| Total number of days lapsed | 8.91 (7.98) |
| Prompt-level (N = 7,682) | M (SD)/n (%) |
| II reminders deployed | 5,734 (74.64%) |
| Interacted with MQU to acknowledge II reminders that were deployed | 2,992 (52.18%) |
| Post-HRSS EMA complied | 4,488 (58.42%) |
| Momentary lapse | 776 (17.29%) |
| Carried out suggested II | 2,557 (56.97%) |
EMA ecological momentary assessment; FTND Fagerstrom Test of Nicotine Dependence; HRSS high-risk smoking situation; II implementation intention.
Person-level descriptive statistics
The participants were Asian American young adults who were current daily smokers (N = 57, Mage = 21.7, 22.8% female, 84.2% Korean American). The mean FTND score was 2.56 (standard deviation [SD] = 2.03). About half of the participants (47.4%, n=27) reported smoking fewer than five cigarettes per day; 52.6% of the sample (n = 30) reported smoking six or more cigarettes per day. A majority of the participants (57.9%, n = 33) began smoking before they turned 15 and the remaining participants (42.1%, n = 24) started smoking at 15 and older. Twenty participants (35.1%) reported some form of e-cig use at least 1 day out of the 4 week period. Participants specified 5.18 HRSSs per day on average (SD = 1.45, max = 9). The average rate of acknowledging the II reminder when it was sent was 52.68% (range: 3.70%–70.07%). On average, participants reported lapses 17.29% of the time and on 8.91 days of the 4 week period.
Prompt-level descriptive statistics
As detailed in Table 1, there were a total 8,262 lines of HRSS prompt-level data generated by the system, 7,682 of which MQU successfully logged the randomization condition at decision points (i.e., the baseline Level-1 sample size). The log data showed that planned randomization was successfully deployed; the JIT II reminders were sent out at an average rate of 74.6% (n = 5,734) of the HRSS (ranging from 65.7% to 81.5% across participants). On average, participants acknowledged receiving the II reminder 52.68% of the time (person-level rate), which equates to approximately half (n = 2,992; 52.18%) of the JIT II reminders sent out.
Out of 7,682 possible randomization-initiated HRSS prompts, participants responded to 4,333 of the post-HRSS EMA (56.40%), which serves as the effective sample for the current study. The missed EMA surveys were not related to gender (p = .38), FTND score (p = .42), use of vaping (p = .08), weeks in study (p = .79), or time of the day (p = .45). As expected, however, participants were more likely to fail to respond to EMA surveys on weekends than weekdays (p = .007); those who had loan (vs. own) phones were also more likely to miss EMA surveys (p = .003). Momentary lapses were reported in 776 prompts (17.29%). Participants reported enacting the suggested II at 2,557 prompts, about half of the specified HRSSs (56.97%).
Effects of JIT reminders on momentary lapse averaged across the study period
Main effects of JIT reminders: H1
As seen in Model 1 of Table 2, in the unadjusted model, we found that, on average, participants were not less likely to lapse when they received JIT reminders relative to when they did not receive them (Model 1: b = −0.14, OR = 0.87, p = .16). Therefore, H1 was not supported. The JIT reminder effects remained nonsignificant (Model 2: b = −0.11, OR = 0.90, p = .30) when controlling for time in study, the main effect of phone type, the between-person engagement proxy variable, and whether the II given plan was enacted.
Table 2.
The effect of II reminder on momentary lapses by phone type
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Intercept | −2.19 (0.25)*** | −1.02 (0.58) | −1.13 (0.58) | −1.18 (0.60) |
| II reminder (vs. no reminder) | −0.14 (0.10) | −0.11 (0.10) | 0.05 (0.13) | 0.22 (0.19) |
| Study week | −0.07 (0.04) | −0.07 (0.04) | −0.05 (0.09) | |
| Own (vs. loan) phone | 0.19 (0.53) | 0.53 (0.55) | 0.26 (0.57) | |
| II reminder × Own phone | −0.47 (0.22)* | −0.47 (0.22)* | ||
| Study week × Own phone | 0.19 (0.09)* | |||
| II reminder × Study week | −0.12 (0.09) | |||
| Enacted II | −1.07 (0.10)*** | −1.09 (0.10)*** | −1.09 (0.10)*** | |
| Person-level % II reminder acknowledged | −1.58 (1.43) | −1.55 (1.44) | −1.55 (1.44) |
Study week is centered at Week 1. Model 1 reports the unadjusted main effect of receiving (vs. not receiving) II reminder on momentary lapse. Model 2 reports the adjusted main effect of receiving II reminder, adjusting for study week, phone type, study week, whether they enacted the specified II at a given prompt, and person-level overall engagement level variable. Model 3 reports the results of the interaction of II reminder and phone type. Model 4 reports the results of two additional interaction terms. Log odds and standard errors are reported.
II implementation intention.
*p < .05; **p < .01; ***p < .001.
Effects of II enactment: H2
We found that when participants reported enacting the given II (vs. failing to enact), the likelihood of momentary lapse was significantly reduced (Model 2: b = −1.07, OR = 0.34, p < .001), providing support for H2. The main effects of time in study (b = −0.07, OR = 0.93, p = .09), using participants’ own Android vs. loan phone (b = 0.19, OR = 1.21, p = .72) and “acknowledging” the II reminder prompts more frequently versus less so (b = −1.58, OR = 0.21, p = .27) were not significantly related to the likelihood of lapses.
Phone type and time in study as JIT effect modifiers: H3 and H4
To test H3, we examined whether the JIT effect on momentary lapses differed between those who used their own versus loan phones (see Table 2; Model 3). Averaged across all study weeks, the JIT effect for loaner participants was not significant (b = 0.05, OR = 1.19, p = .70). The significant interaction (b = −0.47, p = .03) signaled that, for those who used their own phone, the likelihood of lapse was significantly reduced when they received JIT II (b = −0.42, OR = 0.84, p = .018) relative to that for the loaner participants, providing support for H3.
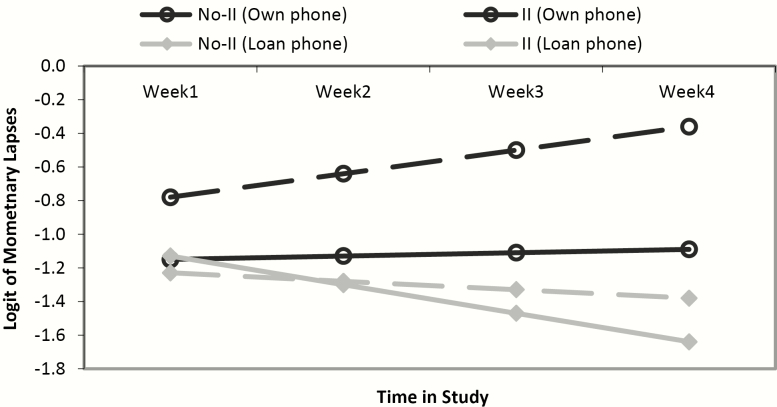
To test H4, we examined whether the JIT effect changed over study period (Table 2; Model 4). The effect of JIT II reminder on lapse, regardless of phone type, did not vary across time in study (b = −0.12, OR = 0.89, p = .21), failing to provide support for H4. A significant interaction between study week and phone type (b = 0.19, OR = 1.21, p = .036) indicated that the likelihood of lapses increased at a steeper rate for those who used own phones, relative to the loaner participants. Furthermore, the results showed that the interaction between JIT effect and phone type remained significant (b = −0.47, p = .03) after the inclusion of additional interaction terms (Model 4). As seen in Fig. 1, the JIT effect in reducing lapses was more pronounced for the participants who used their own phones relative to the loaner participants. This pattern was consistently observed across the study weeks. We also tested the three-way interaction among II status, phone type, and time in study and found it to be not significant (p = .24, not shown in Table 2), indicating that the JIT effects over time did not differ across phone types.
Fig 1.
Log odds of momentary lapses: the JIT effects over time by phone type.
DISCUSSION
The current study evaluated feasibility and initial effectiveness of a mobile-based cessation pilot intervention that delivered automated and personalized JIT support tailored to Asian American smokers’ individual daily schedules. Our findings show that, on average, receiving an implementation intention reminder during personalized high-risk smoking situations in JIT manner did not reduce the likelihood of momentary lapse.
Further analyses revealed that the effect of JIT reminders on smoking lapse prevention may vary as a function of the medium through which they interacted with our JIT cessation app, MQU. Contrary to our hypothesis that the initial effect of JIT reminders would dissipate over time, we found that the JIT effect on lapses did not significantly change over time in study. However, our findings show that those who interacted with MQU on their own phones were able to avoid lapses more effectively when they received JIT reminders (vs. when not receiving), averaged across study period. This was not observed for the loaner participants. Our tests for moderation revealed that the diminished JIT effect was mostly driven by loaner participants, whose II effect on momentary lapses was substantially dampened (i.e., the likelihood of lapses did not differ between II vs. no II conditions). Sensitivity analyses showed that these main findings were not affected by light versus heavy smoking. The main effect of cigarettes per day at baseline (CPD) on momentary lapses was not significant (p = .68); CPD was also not a JIT effect modifier on momentary lapses (p = .56).
In addition, our findings emphasize the importance of enacting the planned actions in the moment leading up to potential HRSS to avoid lapses. In other words, whether the given II was enacted consistently predicted a lower likelihood of lapse, regardless of JIT reminder. The robust effect of carrying out the preplanned II on lapse avoidance found in our study corroborates the existing literature on the importance of forming and executing specific automated strategies leading up to goal attainment on behavioral change [38–40] but on a more microtemporal scale.
It is also noteworthy that the effect of JIT reminders for those who used their own phones remained significant even after controlling for the effect of a planned action being carried out (vs. not) for a given HRSS. Specifically, this finding suggests that JIT II reminders may provide support beyond cueing II enactment via other cognitive routes, such as making salient one’s motivation to quit or cueing ad hoc lapse avoidance strategies to aid individuals to avoid momentary lapse. In fact, our participants reported that they had executed their preplanned IIs during less than 60% of the corresponding HRSS. Furthermore, supplemental analyses revealed that self-developed IIs (62%) were more frequently used than prepopulated IIs (38%). However, the main effect of self-developed versus prepopulated II on momentary lapses was not significant; it was also not a JIT effect modifier on momentary lapses (p = .93, p = .84, respectively). These findings highlight the need for future microtemporal study designs that investigate how to encourage II enactment or other cognitive processes helpful for cessation at a momentary level.
Overall, our findings substantiate the habit-forming (i.e., if–then link) process of behavioral intention [48–50] over time in the context of cessation. While there was a possibility of participants experiencing saturation from repeated exposure to II reminders over time, which could potentially dampen the effectiveness of the reminders, we believe that the personalized JIT element of our study design potentially maintained the relevance and effectiveness of these reminders over the 4 week study period. The nonsignificant effect of JIT reminders during the beginning weeks might indicate that some length of initiation period may be essential for users to acclimate to planned actions and other cessation protocols. This interpretation is also supported by several exit interviews, where participants described that viewing II reminders and other MQU push notifications repeatedly over time increased their motivation to enact lapse avoidance strategies as their quit attempt progressed and as the cessation trial period was coming to an end. Accordingly, a future version of MQU might incorporate features that encourage participants’ motivation to quit at the start of a quit attempt, particularly among those with little experience with prior attempts to quit. Alternatively, the II reminders initially specified at the start of the quit attempt may not actually have been ideal or feasible for some participants in a given HRSS. As participants became better aware of specific plans they were willing to enact as they continued to experience their HRSS during the quit process, the mitigating effect of JIT II reminders on lapse may have been more pronounced in the latter weeks as they discovered which lapse avoidance strategies, whether planned at baseline or ad hoc strategies, worked best. In fact, in the exit interviews, almost three quarters of participants (72.7%) described instances where they employed ad hoc lapse avoidance strategies that were not their originally specified IIs.
Next, a substantive amount of missing values from the EMA surveys deserves a further discussion as found in other mHealth intervention studies [51]. The missed prompts may represent the times and contexts in which the participant’s receptivity is low due to a variety of reasons for a given moment (i.e., dynamic state of receptivity to intervention support [7]). In other words, II reminders that were not logged as “acknowledged” and/or missing values for lapse status might represent unavailability, thus, inappropriate windows to intervene. Unfortunately, this information could not be directly obtained in the current study (i.e., we did not ask the reasons why they missed a previous prompt, if missing). We should note that the failure to comply with EMA prompts was more prevalent among those who used loan phones. Although we cannot assume whether the missingness and the lapse status are systematically associated for the loaner participants, the null JIT effect for loaner participants could be attributable to the observed missing patterns. We observed that missingness in momentary prompts was not related to time in study, implying that the compliance did not systematically decrease over time. Future investigation similar to the current study will continue to provide an improved foundation for better detecting such windows and refine JIT interventions. Automated algorithms that take missingness patterns up until a given timepoint into account when deciding whether to deploy JIT support at a subsequent decision point might be one such method.
We did assess the effect of “acknowledging” the II reminder, construed as a between-person, proxy variable for overall engagement with the MQU system and included it in the model as a covariate. However, researchers have argued that greater levels of interaction or engagement with the intended intervention do not necessarily represent “effective engagement” that leads to desired behavioral change outcomes [52]. In the same vein, we note that engaging with research protocols, such as acknowledging II reminders, does not equate to engaging with quit behavior.
Limitations with the current study deserve attention, as we did not restrict participation from smokers who use e-cigarette (e.g., JUUL) and a few participants indeed used “I will vape instead” as one of their IIs. Those who vaped at least once during the quit attempt (n = 20) reported vaping at least once a day on 13.9 days of the 4 week period—JUUL products started gaining notable popularity during the summer of 2017 [45]. This tobacco product trend may have dampened the internal validity in assessing the JIT effects on the outcome as nicotine intake would have been satisfied by vaping. Further, we did not assess momentary lapses via objective measures and instead relied on self-reports recorded by the MQU. It should be noted, however, that study compensation did not depend on the success of quit attempts. In fact, we conveyed to the participants of the importance of honest reports of incidences and the integrity of data.
Furthermore, MQU was available only on the Android platform as a cross-platform version was not achievable given limited study resources. We explicitly tested moderation by phone type and, even with limited statistical power (person-level N = 16), we were able to detect the effect of JIT II reminders for those who used their own phones. The results from our exit interview data suggest that interacting with loan phones might have been suboptimal for delivering JIT reminders as participants were less familiar with Android phones and more frequently experienced technical glitches, forgot to charge phones or bring loan charger, and/or missed EMA prompts due to inaccessibility of the loan phone (e.g., in one’s bag). Certain social situations (e.g., going out with friends) may have further reduced the likelihood of loaners interacting with MQU. For example, some participants mentioned leaving loan phones at home to avoid losing them while out drinking or reported reduced loan phone use on weekends. These results offer important implications for other mobile health studies in which project loan phones are provided to participants for behavior change.
Despite these limitations, the current study is the first of its kind to evaluate the effects of automated and personalized JIT reminders tailored for Asian American young adult smokers, a group who exhibits high risk for nicotine addiction but tends to underutilize available resources to quit smoking. To our knowledge, the current study is one of the first studies that assesses follow-through of the planned IIs in near real time and the effects on momentary lapse in the context of smoking cessation. Our findings provide detailed accounts of the contextual moderators within a cessation period in which JIT reminders of personalized IIs may be more or less effective in helping smokers to avoid momentary lapses among Asian American young adult smokers. Our findings demonstrated potential effectiveness of JIT approach for cessation research for this population.
Acknowledgements
This work was supported by American Cancer Society (124758-MRSG-13-155-01-CPPB).
Compliance with Ethical Standards
Conflicts of Interest: All authors declare that they have no conflicts of interest.
Authors’ Contributions JH conceived and executed the project, collected and analyzed the data, and wrote the manuscript. CJC collected data, assisted in data analysis and manuscript writing. ED built the MQU system, MQU data server, assisted in data analysis and manuscript writing. DS-M contributed to manuscript writing and editing with expertise in mobile health and JIT intervention. GFD contributed to manuscript writing and editing with expertise in mobile health, EMA and JIT intervention. AML contributed to manuscript writing and editing with expertise in nicotine addiction, health disparity and substance use among young adults.
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Informed consents were obtained from all individual participants included in this study.
References
- 1. Hermens H, op den Akker H, Tabak M, Wijsman J, Vollenbroek M. Personalized coaching systems to support healthy behavior in people with chronic conditions. J Electromyogr Kinesiol. 2014;24(6):815–826. [DOI] [PubMed] [Google Scholar]
- 2. Naughton F, Hopewell S, Lathia N, et al. A context-sensing mobile phone app (Q sense) for smoking cessation: A mixed-methods study. JMIR Mhealth Uhealth. 2016;4(3):e106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Riley WT, Rivera DE, Atienza AA, Nilsen W, Allison SM, Mermelstein R. Health behavior models in the age of mobile interventions: Are our theories up to the task? Transl Behav Med. 2011;1(1):53–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Spring B, Pellegrini C, McFadden HG, et al. Multicomponent mHealth intervention for large, sustained change in multiple diet and activity risk behaviors: The make better choices 2 randomized controlled trial. J Med Internet Res. 2018;20(6):e10528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Thomas JG, Bond DS. Behavioral response to a just-in-time adaptive intervention (JITAI) to reduce sedentary behavior in obese adults: Implications for JITAI optimization. Health Psychol. 2015;34S:1261–1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Intille SS, Kukla C, Farzanfar R, Bakr W. Just-in-time technology to encourage incremental, dietary behavior change. In: AMIA Annual Symposium Proceedings. American Medical Informatics Association; 2003;874. [PMC free article] [PubMed]
- 7. Nahum-Shani I, Hekler EB, Spruijt-Metz D. Building health behavior models to guide the development of just-in-time adaptive interventions: A pragmatic framework. Health Psychol. 2015;34S:1209–1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Brendryen H, Kraft P. Happy ending: a randomized controlled trial of a digital multi-media smoking cessation intervention. Addiction. 2008;103(3):478–484; discussion 485. [DOI] [PubMed] [Google Scholar]
- 9. Naughton F, Jamison J, Boase S, et al. Randomized controlled trial to assess the short-term effectiveness of tailored web- and text-based facilitation of smoking cessation in primary care (iQuit in practice). Addiction. 2014;109(7):1184–1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ubhi HK, Michie S, Kotz D, Wong WC, West R. A mobile app to aid smoking cessation: Preliminary evaluation of SmokeFree28. J Med Internet Res. 2015;17(1):e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Free C, Knight R, Robertson S, et al. Smoking cessation support delivered via mobile phone text messaging (txt2stop): A single-blind, randomised trial. Lancet. 2011;378(9785):49–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Heron KE, Smyth JM. Ecological momentary interventions: incorporating mobile technology into psychosocial and health behaviour treatments. Br J Health Psychol. 2010;15(Pt 1):1–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ali AA, et al. mPuff: Automated detection of cigarette smoking puffs from respiration measurements. In: Proceedings of the 11th International Conference on Information Processing in Sensor Networks. ACM; 2012;269–280. [Google Scholar]
- 14. Parate A, et al. Risq: Recognizing smoking gestures with inertial sensors on a wristband. In: Proceedings of the 12th Annual International Conference on Mobile Systems, Applications, and Services.ACM; 2014;149–161. [DOI] [PMC free article] [PubMed]
- 15. Shoaib M, Bosch S, Incel OD, Scholten H, Havinga PJ. Complex human activity recognition using smartphone and wrist-worn motion sensors. Sensors (Basel). 2016;16(4):426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Torre LA, Sauer AM, ChenMS, Jr, Kagawa-Singer M, Jemal A, Siegel RL. Cancer statistics for Asian Americans, Native Hawaiians, and Pacific Islanders, 2016: Converging incidence in males and females. CA Cancer J Clin. 2016;66(3):182–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wong MM, Klingle RS, Price RK. Alcohol, tobacco, and other drug use among Asian American and Pacific Islander Adolescents in California and Hawaii. Addict Behav. 2004;29(1):127–141. [DOI] [PubMed] [Google Scholar]
- 18. Tanjasiri SP, Lew R, Mouttapa M, et al. Environmental influences on tobacco use among Asian American and Pacific Islander youth. Health Promot Pract. 2013;14(5 Suppl):40S–47S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Brook DW, Brook JS, Zhang C, Whiteman M, Cohen P, Finch SJ. Developmental trajectories of cigarette smoking from adolescence to the early thirties: Personality and behavioral risk factors. Nicotine Tob Res. 2008;10(8):1283–1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. McDermott L, Dobson A, Owen N. Occasional tobacco use among young adult women: A longitudinal analysis of smoking transitions. Tob Control. 2007;16(4):248–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. White HR, Bray BC, Fleming CB, Catalano RF. Transitions into and out of light and intermittent smoking during emerging adulthood. Nicotine Tob Res. 2009;11(2):211–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Huh J, Sami M, Abramova ZS, Spruijt-Metz D, Pentz MA. Cigarettes, culture, and Korean American emerging adults: An exploratory qualitative study. West J Nurs Res. 2013;35(9):1205–1221. [DOI] [PubMed] [Google Scholar]
- 23. Zhu SH, Cummins SE, Wong S, Gamst AC, Tedeschi GJ, Reyes-Nocon J. The effects of a multilingual telephone quitline for Asian smokers: A randomized controlled trial. J Natl Cancer Inst. 2012;104(4):299–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kim SS, Kim SH, Fang H, Kwon S, Shelley D, Ziedonis D. A culturally adapted smoking cessation intervention for Korean Americans: A mediating effect of perceived family norm toward quitting. J Immigr Minor Health. 2015;17(4):1120–1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kim SS, Sitthisongkram S, Bernstein K, Fang H, Choi WS, Ziedonis D. A randomized controlled trial of a videoconferencing smoking cessation intervention for Korean American women: preliminary findings. Int J Womens Health. 2016;8:453–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Tsoh JY, Burke NJ, Gildengorin G, et al. A social network family-focused intervention to promote smoking cessation in Chinese and Vietnamese American male smokers: A feasibility study. Nicotine Tob Res. 2015;17(8):1029–1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Fang CY, Ma GX, Miller SM, Tan Y, Su X, Shive S. A brief smoking cessation intervention for Chinese and Korean American smokers. Prev Med. 2006;43(4):321–324. [DOI] [PubMed] [Google Scholar]
- 28. Wu D, Ma GX, Zhou K, Zhou D, Liu A, Poon AN. The effect of a culturally tailored smoking cessation for Chinese American smokers. Nicotine Tob Res. 2009;11(12):1448–1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. McDonnell DD, Kazinets G, Lee HJ, Moskowitz JM. An internet-based smoking cessation program for Korean Americans: Results from a randomized controlled trial. Nicotine Tob Res. 2011;13(5):336–343. [DOI] [PubMed] [Google Scholar]
- 30. Cerrada CJ, Dzubur E, Blackman KCA, Mays V, Shoptaw S, Huh J. Development of a just-in-time adaptive intervention for smoking cessation among Korean American emerging adults. Int J Behav Med. 2017;24(5):665–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Huh J, Cerrada CJ, Kirkpatrick MG, Dunton G, Leventhal AM. Social contexts of momentary craving to smoke among Korean American emerging adults. Addict Behav. 2016;56:23–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Huh J, Shin H, Leventhal AM, et al. Momentary negative moods and being with friends precede cigarette use among Korean American emerging adults. Nicotine Tob Res. 2014;16(9):1248–1254. [DOI] [PubMed] [Google Scholar]
- 33. Huh J, Paul Thing J, Abramova ZS, Sami M, Beth Unger J. Place matters in perceived tobacco exposure among Korean American young adults: Mixed methods approach. Subst Use Misuse. 2014;49(8):1054–1063. [DOI] [PubMed] [Google Scholar]
- 34. Gollwitzer PM. Implementation intentions: strong effects of simple plans. Am Psychologist. 1999;54(7):493–503. [Google Scholar]
- 35. Adriaanse MA, Vinkers CD, De Ridder DT, Hox JJ, De Wit JB. Do implementation intentions help to eat a healthy diet? A systematic review and meta-analysis of the empirical evidence. Appetite. 2011;56(1):183–193. [DOI] [PubMed] [Google Scholar]
- 36. Bélanger-Gravel A, Godin G, Amireault S. A meta-analytic review of the effect of implementation intentions on physical activity. Health Psychol Rev. 2013;7(1):23–54. [Google Scholar]
- 37. Gollwitzer PM, Sheeran P. Implementation intentions and goal achievement: A meta‐analysis of effects and processes. Adv Exp Soc Psychol. 2006;38:69–119. [Google Scholar]
- 38. Armitage CJ. Efficacy of a brief worksite intervention to reduce smoking: The roles of behavioral and implementation intentions. J Occup Health Psychol. 2007;12(4):376–390. [DOI] [PubMed] [Google Scholar]
- 39. Armitage CJ. A volitional help sheet to encourage smoking cessation: A randomized exploratory trial. Health Psychol. 2008;27(5):557–566. [DOI] [PubMed] [Google Scholar]
- 40. van Osch L, Lechner L, Reubsaet A, Wigger S, de Vries H. Relapse prevention in a national smoking cessation contest: Effects of coping planning. Br J Health Psychol. 2008;13(Pt 3):525–535. [DOI] [PubMed] [Google Scholar]
- 41. Orbell S, Hodgkins S, Sheeran P. Implementation intentions and the theory of planned behavior. Pers Soc Psychol Bull. 1997;23(9):945–954. [DOI] [PubMed] [Google Scholar]
- 42. Orbell S Sheeran P. Motivational and volitional processes in action initiation: A field study of the role of implementation intentions 1. J Appl Soc Psychol. 2000;30(4):780–797. [Google Scholar]
- 43. Chapman J, Armitage CJ, Norman P. Comparing implementation intention interventions in relation to young adults’ intake of fruit and vegetables. Psychol Health. 2009;24(3):317–332. [DOI] [PubMed] [Google Scholar]
- 44. Conner M, Higgins AR. Long-term effects of implementation intentions on prevention of smoking uptake among adolescents: A cluster randomized controlled trial. Health Psychol. 2010;29(5):529–538. [DOI] [PubMed] [Google Scholar]
- 45. Brandstätter V, Lengfelder A, Gollwitzer PM. Implementation intentions and efficient action initiation. J Pers Soc Psychol. 2001;81(5):946–960. [DOI] [PubMed] [Google Scholar]
- 46. Webb TL, Sheeran P. Mechanisms of implementation intention effects: The role of goal intentions, self-efficacy, and accessibility of plan components. Br J Soc Psychol. 2008;47(Pt 3):373–395. [DOI] [PubMed] [Google Scholar]
- 47. Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström Test for Nicotine Dependence: A revision of the Fagerström Tolerance Questionnaire. Br J Addict. 1991;86(9):1119–1127. [DOI] [PubMed] [Google Scholar]
- 48. Mancha RM, Yoder CY. Cultural antecedents of green behavioral intent: An environmental theory of planned behavior. J Environ Psychol. 2015;43:145–154. [Google Scholar]
- 49. Orbell S, Verplanken B. The automatic component of habit in health behavior: habit as cue-contingent automaticity. Health Psychol. 2010;29(4):374–383. [DOI] [PubMed] [Google Scholar]
- 50. Verplanken B, Faes S. Good intentions, bad habits, and effects of forming implementation intentions on healthy eating. Eur J Soc Psychol. 1999;29(5‐6): 591–604. [Google Scholar]
- 51. Scherer EA, Ben-Zeev D, Li Z, Kane JM. Analyzing mHealth engagement: Joint models for intensively collected user engagement data. JMIR Mhealth Uhealth. 2017;5(1):e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Yardley L, Spring BJ, Riper H, et al. Understanding and promoting effective engagement with digital behavior change interventions. Am J Prev Med. 2016;51(5):833–842. [DOI] [PubMed] [Google Scholar]