Sir,
Follicular mucinosis (FM) is an uncommon disorder, infrequently seen in the pediatric population and defined by a characteristic histological pattern of mucin deposition within the hair follicle and sebaceous glands.[1,2]
Case 1 reports an otherwise healthy 14-year-old boy presenting with a 4-month history of a well-defined, slightly infiltrated and desquamative, erythematous nummular plaque with perifollicular hyperkeratosis on the left zygomatic region [Figure 1a]. The lesion had been treated with a topical antifungal and hydrocortisone 1% cream, without improvement. Case 2 refers to a previously healthy 12-year-old boy presenting with a 3-month history of a well-circumscribed desquamative alopecic plaque on the upper lip, with superimposed erythematous follicular papules [Figure 1b]. The previous treatment with oral terbinafine for 6 weeks with no response.
Figure 1.
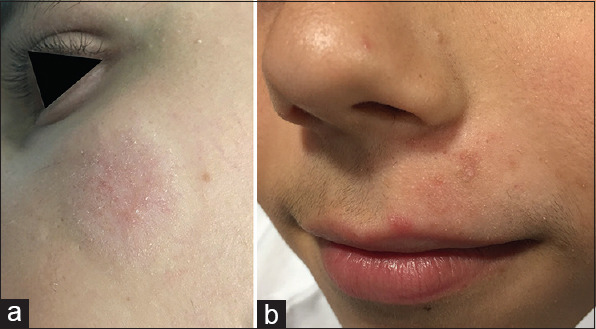
(a) Well-circumscribed, desquamative, erythematous nummular plaque on the left zygomatic region, with perifollicular hyperkeratosis. (b) Desquamative, alopecic plaque on the upper lip, with superimposed erythematous follicular papules
Histological analysis of both skin biopsies disclosed dilated hair follicles with infundibular vacuolar degeneration and a dense perivascular and perifollicular lymphocytic infiltrate [Figure 2a]. Atypical lymphocytes were not observed. Alcian blue staining revealed mucin deposition in and around hair follicles [Figure 2b], compatible with a diagnosis of FM. Routine laboratory studies were within normal range. Both patients were initially treated with fluticasone propionate 0.05% cream, followed by tretinoin 0.05% cream until complete resolution. There was no evidence of recurrence within 18 months of follow-up.
Figure 2.

(a) Histopathological analysis (patient 1) revealed several dilated hair follicles with infundibular vacuolar degeneration and a dense perifollicular and perivascular lymphocytic infiltrate (hematoxylin and eosin, ×100). (b) Alcian blue staining disclosed mucin deposition in and around hair follicles (×100)
Since its first report by Pinkus, two main clinicopathological variants of FM were proposed.[1,2] Primary (idiopathic) FM occurs mostly in children and young adults, following a self-limited course. In contrast, secondary FM mainly manifests in elderly patients, in association with various inflammatory or neoplastic conditions.[3,4] The most common of which is mycosis fungoides (MF), with a prevalence of 15% to 30% of adult patients.[1,5]
Typical FM lesions present as infiltrated, erythematous scaly plaques with grouped follicular papules and nonscarring alopecia in terminal hair-bearing locations.[1] Given the considerable clinicopathological overlap between primary and secondary forms, some authors regard FM as an early folliculotropic variant of MF that follows an indolent clinical course, arguing that both conditions exist along a continuous disease spectrum. While MF is rare in children, a few cases of FM associated with MF or Hodgkin's lymphoma have been reported.[4,6]
In an attempt to distinguish the two forms, a combination of clinical and histopathological criteria is applied [Table 1]. The presence of a single plaque or a limited number of lesions confined to the head and neck is significantly more common in primary FM, whereas multiple, widespread lesions are more likely associated with cutaneous lymphoma.[3,6,7]
Table 1.
Comparison of primary follicular mucinosis and mycosis fungoides(MF)-associated follicular mucinosis
| Primary follicular mucinosis | MF-associated follicular mucinosis | |
|---|---|---|
| Age of patient[3,4] | Children and young adults | Elderly patients |
| Number of lesions[6,7] | Single or a few lesions | Multiple lesions |
| Location of lesions[6,7] | Mainly head and neck | Mostly widespread |
| Histopathology[3,7] | Perifollicular mixed inflammatory infiltrate and mucin deposition within the follicular epithelium and sebaceous glands | Atypical lymphocytes with enlarged, hyperchromatic nuclei and features of epidermotropism or folliculotropism |
| Type of mucin[3] | Dermal-type mucin | Dermal-type mucin |
| Immunohistochemistry[3,6] | CD5+ and CD7+; similar number of CD4+ and CD8+ cells | CD5- and CD7-; CD4+ cells usually outnumber CD8+ cells |
| Disease course and treatment[6,7] | Self-limited; usually resolves within 2 years without treatment | Persistent; may require systemic therapy |
Histopathology is essential to confirm the diagnosis,[3] and to differentiate FM from morphologically similar conditions, such as dermatophytosis, lupus tumidus, or pseudolymphoma. Although skin biopsy is frequently deferred in children, it must be considered in nonresponsive cases, such as ours. Histology reveals a perifollicular mixed inflammatory infiltrate and mucin deposition within the follicular epithelium and sebaceous glands. No difference is found regarding the composition of mucin in primary compared with MF-associated FM.[3] Findings of epidermotropism or atypical lymphocytes, however, are suggestive of a malignant process.[3,6,7] Nevertheless, no histological or immunophenotypical criteria can reliably distinguish between primary and secondary FM or predict disease progression.[2,3,4,5,7] Demonstration of an aberrant T-cell profile is also not indicative of malignancy, as it is commonly found in otherwise benign FM.[3,5]
No standard treatment regimen has been established. An expectant attitude is an option in primary FM, as most cases spontaneously resolve within up to 2 years.[7] Several studies indicate that the condition cannot be unequivocally considered as MF in this age group. Hence, it is recommended to approach it with caution and initial conservative treatment, as to minimize the psychological burden of a diagnosis of malignancy that is unjustifiable in most cases.[1,2,3] However, as the diagnosis of cutaneous lymphoma in its initial phases can be hard to establish, a long-term surveillance of affected individuals is mandatory.[3,5,7]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Zvulunov A, Shkalim V, Ben-Amitai D, Feinmesser M. Clinical and histopathologic spectrum of alopecia mucinosa/follicular mucinosis and its natural history in children. J Am Acad Dermatol. 2012;67:1174–81. doi: 10.1016/j.jaad.2012.04.015. [DOI] [PubMed] [Google Scholar]
- 2.Alikhan A, Griffin J, Nguyen N, Davis D, Gibson L. Pediatric follicular mucinosis: Presentation, histopathology, molecular genetics, treatment, and outcomes over an 11-year period at the Mayo Clinic. Pediatr Dermatol. 2013;30:192–8. doi: 10.1111/pde.12019. [DOI] [PubMed] [Google Scholar]
- 3.Rongioletti F, De Lucchi S, Meyes D, Mora M, Rebora A, Zupo S, et al. Follicular mucinosis: A clinicopathologic, histochemical, immunohistochemical and molecular study comparing the primary benign form and the mycosis fungoides-associated follicular mucinosis. J Cutan Pathol. 2010;37:15–9. doi: 10.1111/j.1600-0560.2009.01338.x. [DOI] [PubMed] [Google Scholar]
- 4.Uysal PI, Bozdogan O, Atilan A, Yalcin B. Juvenile-onset early-stage mycosis fungoides-associated follicular mucinosis: A case report. Am J Dermatopathol. 2018;40:e112–4. doi: 10.1097/DAD.0000000000001114. [DOI] [PubMed] [Google Scholar]
- 5.Brown HA, Gibson LE, Pujol RM, Lust JA, Pittelkow MR. Primary follicular mucinosis: Long-term follow-up of patients younger than 40 years with and without clonal T-cell receptor gene rearrangement. J Am Acad Dermatol. 2002;47:856–62. doi: 10.1067/mjd.2002.124604. [DOI] [PubMed] [Google Scholar]
- 6.Emge DA, Lewis DJ, Aung PP, Duvic M. How to discern folliculotropic mycosis fungoides from follicular mucinosis using a pediatric case. J Cutan Med Surg. 2018;22:336–40. doi: 10.1177/1203475417752366. [DOI] [PubMed] [Google Scholar]
- 7.Rongioletti F. Primary paediatric cutaneous mucinoses. Br J Dermatol. 2020;182:29–38. doi: 10.1111/bjd.18004. [DOI] [PubMed] [Google Scholar]


