Abstract
Cutaneous granulomatous disorders represent diseases with underlying granulomas on histology and are broadly divided into infectious and noninfectious disorders. Although histology is sine qua non in diagnosis of granulomatous disorders, lately dermoscopy has come up as a useful tool assisting in diagnosis of granulomatous disorder. Dermoscopy of granulomatous disorder is characterized by localized or diffuse, structureless yellowish-orange areas, along with vessels. Dermoscopic features of granulomatous disorders can be overlapping among various disorders, but detailed accurate assessment of various findings and their pattern may be useful in differentiating among them. In addition to this, peculiar dermatoscopic findings seen can also prove useful in distinguishing between various disorders. Hereby, we discuss dermatoscopic findings of various granulomatous disorders.
Keywords: Cutaneous granulomatous disorders, dermoscopy, granulomatous disorder
Introduction
Granulomatous disorders of skin incorporate a vast array of disorders which have an underlying collection of histiocytes, giant cells, various inflammatory cells common to all. Broad classification of cutaneous granulomatous disorders depending on the pathogenic aspects divides it into infectious and non-infectious subtypes.[1] Infectious granulomatous disorders include mycobacterial, fungal diseases, syphilis, and leishmaniasis whereas sarcoidosis, necrobiotic disorders, granulomatous rosacea, interstitial granulomatous dermatitis, and foreign body granulomas comprise the non-infectious granulomatous group. Clinically, cutaneous granulomatous disorders (CGD) are characterized by more or less infiltrated lesions. Dermoscopy has evolved over the years to assist in non-invasive diagnosis of several cutaneous granulomatous disorders like sarcoidosis, granuloma annulare, lupus vulgaris, and leishmaniasis to name a few. The dermoscopic appearance of granulomatous disorders is symbolized by presence of structureless orange or orange-yellowish areas (focal or diffuse), along with vessels which can be linear or branching.[2] The distinct yellowish-orange background seen in dermoscopy is reflective of underlying dermal granulomas (mass effect) and their visualization is enhanced by applying slight pressure on the skin which reduces erythema.[3] Other dermoscopic findings noted include milia like cyst, whitish areas, scaling, erythema, follicular plugs, and pigmentation structures.[2,4] Although, orange to orangish-yellow structureless areas are hallmark of granulomatous disorders, it is important to remember that neither their presence is specific nor its absence rules out granulomatous disorders. It must be noted that appearance of such areas might be difficult to appreciate during initial stages when granulomas are less well organized, when granulomas are deep, or their appearance is masked by epidermal changes like hyperkeratosis or ulceration.[3] Apart from CGD, these areas might also be seen in other disorders with dense dermal cellular infiltration like xanthogranuloma, pseudolymphomas, and lymphoma.[3] The arrangement, shape, and color of various dermoscopic findings can help in distinction of CGD.
In the present article, we have described an up-to-date comprehensive review of dermoscopic findings of various infectious and non-infectious disorders. Tables 1 and 2 summarizes the findings of infectious and non-infectious disorders, respectively.
Table 1.
Summary of dermoscopy findings of non-infective granulomatous disorders
| Non-infective disorders | Dermatoscopic findings |
|---|---|
| Sarcoidosis | Orange or yellowish orange (focal or diffuse) structureless areas, well-focussed vessels |
| Others: follicular plugs, scar like depigmentation, scales, pigmentation structures (more common among dark-skinned patients) | |
| Necrobiosis Lipoidica | Diffuse structureless yellowish-orange areas, well-focussed vessels (morphology varying according to stage) |
| Others: ulceration, crusts, scales, whitish structureless areas, and brownish reticular structures | |
| Granuloma annulare | Nonvascular findings: Whitish areas and yellowish-orange (focal or diffuse) structureless areas |
| Vascular findings: Unfocussed vessels over pinkish-red background | |
| Others: pigmented structures, whitish scaling, rosettes, crystalline leaf venations | |
| Annular elastolytic giant cell granuloma | Yellowish-orange structureless areas and scales in periphery; |
| well-focussed reticular vessels over pale pinkish background in the centre | |
| Other: Shiny white lines, pale white areas, pigmentation structures | |
| Rheumatoid nodule | Pink or pink and white mixed homogenous background, dull orange areas (subtle), reticulate pigmentation, vessels (less common) |
| Granulomatous rosacea | Orange-yellow areas (focal or diffuse) with vascular polygons |
| Other: rosettes, linear, and hairpin vessels | |
| Lupus milaris disseminate faciei | Perifollicular structureless yellowish-orange area, keratotic plugs (yellow/white), vessels |
| Granulomatous cheilitis | Yellow-white, white structureless area, and linear (blue arrow) and dotted (red arrow) vessels |
| Others: Erosions and superficial scaling. |
Table 2.
Summary of dermoscopy findings of Infective granulomatous disorders
| Infective granulomatous disorders | Dermatoscopic findings |
|---|---|
| Hansens disease Tuberculoid pole | Yellowish white area in centre, peripheral erythema, and vessels, reduced pigment network, absence of lesional hair and white dots |
| Boderline tuberculoid | White areas, yellowish-orange structureless areas, broken pigmentary network, reduced white dots and hairs, coiled hair, and vessels (facial>extrafacial) |
| Borderline lepromatous | Yellow/yellow white areas, distorted pigment network, widened skin furrows/ chrysalis-like structures, slight diminution of appendageal structures and hairs |
| Lepormatous leprosy | Yellowish-orange areas, diminished hair follicle and eccrine openings but not absent, branching linear vessesls. |
| Type 1 reaction | Yellowish-ornage areas, scaling, keratotic plugs, branching and arborizing vessels |
| Type 2 reaction | Milky-red structureless areas, increased vessels, red dots, white area, patchy brown dots |
| Histoid leprosy | Whitish yellow areas, peripheral pigmentation, shiny white areas, crown vessles, and linear branching vessels |
| Lupus vulgaris | Yellowish-orange structureless areas (focal or diffuse), well-focussed vessels |
| Others: Milia-like cyst, whitish reticular streaks, scales, pigmentation structures, and follicular plugs. | |
| Cutaneous leishmaniasis | Generalised erythema, polymorphic vessles, yellow tears, white starburst pattern |
| Others: Central erosion, ulceration, crusts, scaling, salmon-colored ovoid areas, pustules, white scarring areas, perilesional hypopigmented halo | |
| Chromoblastomycosis | Yellowish-orange areas, pink and white areas, reddish brown to black dots, scales, crusts, and polymorphic vessels |
| Sporotrichosis | Diffuse background erythema, yellowish-orangish areas (early lesion), white fibrotic strands (late stage), and unfocussed vessels |
| Mycetoma | Yellow globules, white structureless areas, structureless blue-white areas, white scales, erosions, and polymorphic vessels |
Non-Infectious Granulomatous Disorders
Sarcoidosis
Dermoscopy of sarcoidosis characteristically displays translucent, orange, or yellowish orange structureless areas which may be focal or diffuse (ranging in prevalence rate from 84.2% to 100.0%) along with well-focused vessels of different morphologies (73.7% to 100%) [Figure 1].[3,5,6,7] Underlying dermal granulomatous inflammation (”mass effect”) is responsible for imparting yellowish-orange hue on dermoscopic examination and is better visualized by applying slight pressure on the skin which decreases erythema. Visualization of structureless areas might be difficult to appreciate in certain situations as during early stage of the disease when granulomas are not well developed, when granulomas are deep, or when surface epidermal changes like hyperkeratosis mask their appearance. Various morphologies of vessels can be seen like linear/linear irregular, branching, dotted, and glomerular with occurrence of the former two commoner than the other vascular patterns. The granulomas push the vessels towards the surface making them appear sharper and well-focused. Follicular plugs, scar like depigmentation, yellowish/white scales, crystalline structures, milia like cysts, and pigmentation structures though seen infrequently are other dermoscopic findings in cutaneous sarcoidosis.[3,5,6,7]
Figure 1.

Dermoscopy of sarcoidosis showing transculent yellowish-orange structureless areas (black star) with well-focussed vessles (blue box). Scar-like depigmentation is also seen (black arrow). [In set: Clinical image]
Necrobiosis lipoidica (NL)
The dermoscopic hallmark findings of NL are diffuse structureless yellowish-orange areas with well-focused vessels, morphology of which varies according to stage of the disease. In early stage or active border of the lesion, dotted, glomerular, comma-shaped, and globular vessels are more prominent with linear, hairpin shaped, and network shaped vessels predominating in well-developed or established lesions of NL. Long standing lesions tend to have sharper, larger, branching-serpentine vessels with a diameter that decreases from center to periphery of the lesion [Figure 2].[3,5,8,9,10,11] The vessels appear sharper and well-focused is due to their dilation and thickening along with marked epidermal atrophy (which is more in advanced stages and center of the lesion). The longer and more branching vessels seen due to the underlying atrophy in NL help differentiate it from other granulomatous disorder like sarcoidosis.[12] Yellowish-orange hue correlates histologically to underlying granulomatous inflammation and at times, to the lipid deposition which imparts a yellower hue in NL compared to other CGD.[3,5,8,9,10,11]
Figure 2.

Well-focused, sharp network shaped, and serpentine vessels over a yellowish-orange background (black star). [In set: Clinical image]
Additional findings less commonly seen in NL include ulceration, white/yellowish crusts, scales, whitish structureless areas (particularly in advanced lesions due to dermal fibrosis), and brownish reticular structures.[3]
Granuloma annulare (GA)
Dermoscopic findings of GA are said to be heterogenous varying greatly depending on the histologic subtype. Unfocused vessels of varied morphologies (dotted, linear irregular, branching) over a pinkish-red background are said to be constant findings with vascular structures having a prevalence rate of 88.0%.[3,5] The most common non-vascular findings are whitish areas (regular, globular, or both), and yellowish-orange (focal or diffuse) structureless areas [Figure 3]. It is common to find pale-white/yellowish-white structureless areas in dermoscopy of GA in patients with skin of colour (authors personal observation). The appearance of vascular structures is quite subtle compared to other granulomatous disorders and earlier studies have documented a lower prevalence rate of vessels which may depend on technique used (better visualization with polarized mode) and amount of pressure used during examination as disappearance of vascular structures is possible even with slight pressure.[9,11,13] The whitish area and yellowish orange structureless areas represents underlying collagen degeneration/mucin deposition/dermal fibrosis and dermal granulomas respectively on histology. Yellowish orange structureless areas (particularly when diffuse) are seen to be more commonly associated with palisading histological pattern and are absent in lesions with interstitial pattern or when granulomas are located deep.[3,13]
Figure 3.

Dermoscopy of granuloma annulare showing pale-white structureless areas all along the annulus (black stars). [In set: Clinical image]
Other less commonly noted findings are pigmented structures, whitish scaling, rosettes, crystalline leaf venations which are whitish, parallel striae emerging from a central vein.[13]
Annular elastolytic giant cell granuloma (AEGCG)
Dermoscopy of AEGCG is not well described with only one case reported hitherto. In a recent report by Errichetti et al., yellowish-orange structureless areas (optical effect secondary to underlying dermal granulomas) and whitish-grayish scaling (due to hyperkeratosis) were seen at the periphery and well-focused reticular vessels over pale pinkish background in the center [Figure 4].[14] Although whitish-gray scales are non-specific findings, appearance of well-focused vessels is a useful clue when suspecting AEGCG as owing to central epidermal atrophy, superficial dilated dermal vessels are present closer to the surface and in turn, more evident.[5,14] In addition to the above-mentioned findings, pigmentation structures (commoner in skin of color), pale white areas and shiny white lines (correspond to loss of elastic fibers in dermis histopathologically) can also be found in dermoscopy of AEGCG (authors’ personal observation) [Figure 4].
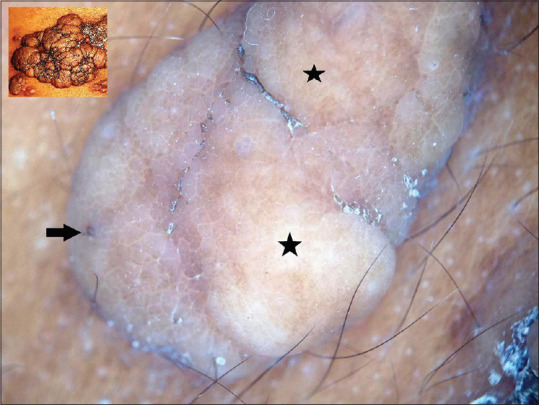
Figure 4.

Dermoscopy of annular elastolytic giant cell granuloma showing diffuse yellowish orange structureless areas (black star) in the periphery with vessels over a pinkish background more prominent in the center. Pigmentation structures and shiny white lines (black arrow) also appreciated. [In set: Clinical image]
Rheumatoid nodule (RN)
The usual dermoscopic finding in RN is pink or pinkish-white mixed homogenous background. Less commonly, presence of arborizing or short linear vessels may be noted.[15]
The structureless orange or yellowish orange appearance characteristically seen in CGD is either absent in rheumatoid nodule or if present, is quite subtle appearing dull orange owing to the deep localization of granulomas [Figure 5].[3,5]
Figure 5.

Dermoscopy of rheumatoid nodule displaying a subtle, diffuse dull orange structureless area. [In set: Clinical image]
Other non-infective granulomatous disorders
Granulomatous rosacea (GR)
Dermoscopy of GR illustrates focal or diffuse orange-yellow areas (represent dermal granulomas) along with vascular polygons (linear reddish or purple vessels arranged in a polygonal network) are found in dermoscopy of GR [Figure 6]. Though findings of orange-yellow areas are similar to other CGD, vascular polygons are said to be a highly specific finding of rosacea.[3,5,16,17] Other findings like rosettes, linear, and hairpin vessels are less frequent findings.[3]
Figure 6.

Vascular polygons (black arrow) over a yellowish-orange background (black star) seen in dermoscopy of granulomatous rosacea. [In set: Clinical image]
Lupus milaris disseminata faciei (LMDF)
Dermoscopy of LMDF shows discrete, structureless yellowish-orange area arranged focally around follicles, along with whitish or yellow keratotic plugs, perifollicular scales, and vessels [Figure 7]. Discrete yellowish-orange areas mirror the perifollicular localization of granulomas in LMDF with keratotic plugs secondary to follicular hyperkeratosis and lateral pressure on follicles by granulomas.[3,18,19]
Figure 7.

Dermoscopy of lupus milaris disseminates faciei shows perifollicular structureless yellowish-orange areas (black star), with follicular keratotic plugs (black boxes), perifollicular scales, and vessels (black arrow). [In set: Clinical image]
Granulomatous cheilitis
Granulomatous cheilitis is a chronic granulomatous inflammatory disorder characterized by persistent, usually asymptomatic swelling of lips (upper, lower, or both) that is histologically characterized by presence of non-caseating granulomas in the dermis. It is considered as a manifestation of orofacial granulomatosis, a clinical description of orofacial swelling caused by non-caseating granulomatous inflammation not associated with systemic disease. In one of the authors’ (KAA) personal observation, yellow-orange structureless areas, yellow white globules, gray-white structureless areas and vessels (dotted and linear) along with erosions and superficial scaling were the predominant dermoscopic features noted [Figure 8]. These features, although may not be helpful in differentiating from other granulomatous inflammatory conditions causing chronic lip swelling (e.g., sarcoidosis, tuberculosis, and foreign body reactions), they may be of value in differentiating from other disorders causing chronic lip swelling such as amyloidosis, contact cheilitis, and hereditary angioedema.[20]
Figure 8.

Dermoscopy of granulomatous cheilitis showing yellow-white structureless areas (black star), white structureless area (red star), and linear (blue arrow) and dotted (red arrow) vessels. [In set: Clinical image]
Infectious Granulomatous Disorders
Hansen's disease
Leprosy is a chronic granulomatous disorder with varied clinical manifestations making it a close mimicker of various other infective and non-infective granulomatous disorders. Dermoscopy of Hansen's disease has been described recently in several studies with each subtype having a distinct appearance. Dermoscopy of leprosy can be studied by evaluating certain important criteria namely (1) scales and atrophic areas (2) the arrangement or morphology of vessels, (3) variations of colors (4) follicular, sweat gland, and appendageal abnormalities, and (5) specific features (clues).[21] In a recent study by K. Vinay et al., dermoscopic features of entire spectrum of Hansen's disease was described.[22] Yellowish-orange structures areas, vascular structures, broken/reduced pigment network and paucity of appendageal structures findings common to all subtypes. Dermoscopy of borderline tuberculoid (BT) hansens is best studied among all subtypes with diminished pigment network, white areas, decreased appendageal structures (reduced hairs and white dots), yellowish-orange structureless areas, branching and anastomosing vessels being the predominant dermoscopic findings [Figure 9].[3,22,23] White structureless areas correspond to decreased number of melanocytes and yellowish-orange globules represent underlying dermal granulomas. Reduced white dots are secondary to destruction of appendageal structures by granulomatous inflammation.
Figure 9.

Dermoscopy of borderline tuberculoid leprosy showing yellow-white structureless areas (black stars). Note the conspicuous scarcity of eccrine openings and empty hair follicles (black arrow). [In set: Clinical image]
While findings of yellowish-orange globules and vascular structures in leprosy is similar to those found in other granulomatous disorders, presence of white areas, diminished pigment network, and reduced white dots are findings unique to dermoscopy of leprosy. Some of the above-mentioned findings in BT hansens are seen to differ according to the site lesion (facial vs extrafacial). Facial lesions tend to have prominent vascular structures, yellow areas, and coiled hairs owing to richer vascularity, thin epidermis, and involvement of hair shaft of vellus hairs in facial area respectively.[3,22,23] In BT lesions with type 1 reaction, in addition to the above findings of yellowish orange areas and branching and arborizing vessels, greyish white scales (represent hyperkeratosis) and keratinous plugs are seen.[22]
Tuberculoid leprosy (TT) lesion show central yellowish white area with peripheral erythema and vessels (representing dilated dermal vasculature) along with broken pigmentary network and lesional loss of hair follicles and white dots (representing eccrine gland openings).[22] Lesions of borderline lepromatous (BL) leprosy show distorted pigment network, widened skin furrows (seen as white chrysalis-like structures), only slight reduction of appendageal structures and hairs, and yellow areas. In patients of skin of color yellow-white areas are a common finding (authors personal observation) [Figure 10]. Lesions of lepromatous leprosy display yellowish-orange areas with branching vessels. Hair follicles and eccrine openings are diminished but not absent. Dermoscopic findings in Erythema nodosum leprosum (ENL) are not specific and show milky-red structureless areas, increased vessels, red dots (representing increased and dilated vessels on histology by immune complex vasculitis), white areas (reflecting underlying fibrosis), and patchy brown dots (due to dermal melanin).[5,22]
Figure 10.

Dermoscopy of borderline lepromatous leprosy showing yellow-white structureless areas (black stars), widened skin furrows (blue arrow), and distorted pigment network (black arrow). [In set: Clinical image]
Histoid leprosy (HL) shows whitish yellow areas along with linear branching vessels, crown vessels, and peripheral pigmentation on dermoscopy.[22,24] Prominence of linear branching vessels is attributed to upward displacement of vessels due to underlying dermal granulomas. Crown vessels which are a variant of linear branching vessels that originate from periphery of the lesion and do not cross the midline are also described in dermoscopy of molluscum contagiosum and sebaceous hyperplasia apart from HL.[22,25] The central whitish-yellow structureless area and peripheral pigmented rim is attributed to whorled arrangement of spindle-shaped histiocytes in the granuloma and color of the hyperpigmented skin type, respectively.[3,24,25] In a recent study by Acharya et al., shiny white structures (SWS) which represent dermal fibrosis were described with shiny white areas, crystalline lines, and rosettes as its morphological findings.[25]
Treated lesions of lepromatous leprosy show persistent yellowish areas with increased pigmentary change (secondary to increase in lesional basal pigmentation post treatment).
Lupus vulgaris (LV)
Dermoscopic appearance of LV is characterized by the presence of focal or diffuse, yellowish-orange structureless areas on a pinkish background, and well-focussed vessels with a prevalence rate of 93.8%–100.0% [Figure 11].[3] Other findings are whitish reticular streaks, scales, pigmentation structures, and follicular plugs. Milia-like cysts can also be seen which possibly reflect the foci of caseating necrosis histologically.[3,26] Although, it is difficult to distinguish between LV and sarcoidosis when depending solely on dermoscopic appearance, some authors believe that caseous necrosis (which makes the granuloma less compact) or lipid deposition within multinucleate Langhans giant cells can impart a more yellowish hue to the former, whereas granulomas of sarcoidosis appear dull orange when compared with those of LV.[3]
Figure 11.

Dermoscopy of lupus vulgaris showing yellow-orange structureless areas (black stars), white structureless areas (blue stars) and white scales (red arrow) on a pink structureless background. [In set: Clinical image]
Fish tank granuloma
Dermoscopy of fish tank granuloma has recently been reported to show orange structureless areas and dotted/glomerular vessels.[27] Orange structureless areas are seen secondary to underlying dermal granulomas and inflammatory granulomatous infiltrate presenting as dotted and glomerular vessels upon dermoscopy.[27] Other findings reported are white scales (corresponds to epidermal orthokeratosis), crusts and erosions.
Cutaneous leishmaniasis (CL)
The most common dermoscopic findings of CL are generalised erythema and vessels with prevalence rate of 81.9%–100.0% and 86.9%–100.0% respectively, appearing secondary to underlying dilated vessels [Figure 12].[3,28] More often than not vascular structures found in CL are polymorphic (two or more types of vessels) with varying combinations of irregular linear, arborizing, hairpin, comma shaped, tree like, glomerulus-like, corckscew, and dotted patterns.[3,28,29,30,31] Other notable findings are yellowish tears (39.1%–59.0% of cases) and white starburst pattern (8.6% to 60.4% of cases). Yellowish tears are yellow-white, oval to round, teardrop shaped structures which occur secondary to lateral compression of follicular ostium from tumoral growth causing follicular keratin plugging. White starburst pattern is peculiar radiating striae or peripheral white halo which represent underlying hyperkeratosis. Contrary to other CGDs, surface or epidermal changes like central erosion, ulceration, crusts, yellow or white scaling, and hyperkeratosis are frequently encountered in CL especially in later stages of the disease. Other findings described are salmon-colored ovoid areas, perilesional hypopigmented halo, thrombotic vessels, yellowish hue, white scarring areas, milia-like cysts, and pustules.[3,28,29,30,31]
Figure 12.

Dermoscopy of cutaneous leishmaniasis showing generalized erythema, polymorphic vessels (black arrows), and yellow to white tear drops (black circle). Erosions, crusts, and scaling can also be appreciated. [In set: Clinical image]
Two main types of dermoscopic patterns of CL have been described depending on the evolution of disease: initial papular lesions showing yellow tears with vascular structures and more advanced tumoral lesions showing hyperkeratosis, erosion/ulceration along with white starburst-like pattern and vascular structures at the periphery[28]
Chromoblastomycosis
Dermoscopic findings of chromoblastomycosis is reported in a handful of reports with yellowish-orange areas, pink and white areas, multiple scattered reddish brown to black dots and globules, scales, crusts, and polymorphic vessels [Figure 13].[32,33,34] The yellowish-orange areas represent the mycotic granuloma, while the white areas are reflective of hyperkeratosis and pseudoepitheliomatous hyperplasia. The reddish brown to black dots and globules are found to be characteristic of chromoblastomycosis and represent the transepidermal elimination of muriform cells, inflammatory cells, thrombotic vessels, and haemorrhage.[32,33,34]
Figure 13.

Dermoscopy of chromoblastomycosis showing yellow-orange globules (black arrows), reddish-black dots (black circles) over pink and white areas, and yellowish white scales. [In set: Clinical image]
Sporotrichosis
Dermoscopic features of sporotrichosis are not well described in literature. In a recent series describing dermoscopic findings of cutaneous sporotrichosis, evolving lesions of cutaneous sporotrichosis showed diffuse background erythema, yellowish-orangish areas, whereas late lesions show white fibrotic strands, and unfocussed telangiectatic vessels were seen in both stages.[35] Other findings reported are ulceration, hemorrhagic crusting, and yellow tears. Yellow tears are also seen in cutaneous leishmaniasis as described earlier and represent follicular plugs that become prominent due to lateral compression from the dermal inflammation and granuloma. They are probably more prominent in facial lesions owing to abundant pilosebaceous follicles over face [Figure 14].
Figure 14.

Dermoscopy of sporotrichosis showing diffuse erythema, yellowish-orangish areas (blue stars), yellow tears (black circle), white fibrotic areas (black star), scales, and unfocussed vessels (black arrow). [In set: Clinical image]
Mycetoma
Mycetoma is a chronic infection that presents with triad of soft tissue swelling, sinuses and grains. Grains are considered hallmark of the disease but at times they do not manifest upon clinical examination. In mycetoma, dermoscopy shows yellow globules and structureless areas, white structureless areas, white scales, erosions, and polymorphic vessels [Figure 15].[36,37] Dermoscopic examination can also help in visualizing small grains with structureless blue-white areas surrounded by a white halo and polymorphic vessels evident when grains are absent.[38] From dermoscopic-pathological correlation point of view, yellow globules, white structureless areas, structureless blue-white areas represent dermal granulomas admixed with neutrophils, dermal fibrosis, and compact masses of pigmented fungi with associated subcutaneous pigmentation, respectively.
Figure 15.

Dermoscopy of mycetoma showing a central serosanguineous crust (yellow star) surrounded by white halo (blue arrow) indicative a discharging sinus, yellow-orange structureless areas (black stars) on a pinkish background. [In set: Clinical image]
Dermoscopic differential diagnoses for yellow-orange and yellow-white structures
Certain non-granulomatous disorders can exhibit yellow-orange and yellow-white structures on dermoscopy, in patterns similar to granulomatous disorders discussed above. Hence, it is imperative to interpret these findings in conjunction with other dermoscopic features and in the context of clinical aspects of the disease for appropriate diagnosis.
Yellow-orange structureless areas are observed in colloid milia, solitary mastocytoma (secondary to dense dermal mast cell population), and xanthogranuloma (reflect dermal aggregates of xanthomatized histiocytes) [Figure 16].[37,38,39,40,41] Yellow-white globules and structureless areas can be seen in nevus lipomatosus, [Figure 17], nevus sebaceous [Figure 18] and sebaceous tumors [Figure 19].[42,43,44]
Figure 16.

Dermoscopy of xanthogranuloma showing yellow-orange and yellow-white structureless areas (black stars) with linear marginal vessels extending towards but without crossing the center (blue arrows). [In set: Clinical image]
Figure 17.
Dermoscopy of nevus lipomatosus cutaneous superficialis showing a global lobulated aspect of the lesion with cerebriform surface, yellow-white structureless areas (black stars) and comedo-like structures (black arrow). [In set: Clinical image]
Figure 18.

Dermoscopy of nevus sebaceous (verrucous plaque lesion) showing bright yellow-white structureless areas and papillary excrescences (blue arrow) indicative of overlying epidermal hyperplasia. [In set: Clinical image]
Figure 19.

Dermoscopy of benign sebaceous hyperplasia showing multiple yellow-white globules with central umbilications (black arrows) and linear and branching vessels (red arrows). [In set: Clinical image]
Conclusion
Dermoscopy is a useful non-invasive, bedside tool which can aid in reaching the diagnosis of granulomatous disorders with presence of orangish-yellow structureless areas and vessels being the hallmark finding, common all across the spectrum of CGD. Presence of the characteristic orange-yellow areas should raise suspicion of an underlying granulomatous pathology and should in turn be followed by thorough evaluation of other dermoscopy features (shape, color, arrangement, additional clues) as presence of certain features can be distinctive of a particular granulomatous disorder. Though, dermoscopy alone is not diagnostic it can act as a valuable and easy to perform procedure in addition to histopathology and microbiological studies.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Tronnier M, Mitteldorf C. Histologic features of granulomatous skin diseases. Part 1: Non-infectious granulomatous disorders. J Dtsch Dermatol Ges. 2015;13:211–6. doi: 10.1111/ddg.12610. [DOI] [PubMed] [Google Scholar]
- 2.Errichetti E, Stinco G. Dermoscopy in general dermatology: A practical overview. Dermatol Ther (Heidelb) 2016;6:471–507. doi: 10.1007/s13555-016-0141-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Errichetti E, Stinco G. Dermatoscopy of Granulomatous Disorders. Dermatol Clin. 2018;36:369–75. doi: 10.1016/j.det.2018.05.004. [DOI] [PubMed] [Google Scholar]
- 4.Errichetti E, Stinco G. The practical usefulness of dermoscopy in general dermatology. G Ital Dermatol Venereol. 2015;150:533–46. [PubMed] [Google Scholar]
- 5.Lallas A, Errichetti E, Ioannides D. Dermoscopy in General Dermatology. Boca Raton: CRC Press; 2019. [Last Accessed on 2020 Jul 09]. Available from: https://doi.org/10.1201/9781315201733 . [Google Scholar]
- 6.Pellicano R, Tiodorovic-Zivkovic D, Gourhant JY, Catricala C, Ferrara G, Caldarola G, et al. Dermoscopy of cutaneous sarcoidosis. Dermatology. 2010;221:51–4. doi: 10.1159/000284584. [DOI] [PubMed] [Google Scholar]
- 7.Chauhan P, Meena D, Hazarika N. Dermoscopy of sarcoidosis: A useful clue to diagnosis. Indian Dermatol Online J. 2018;9:80–1. doi: 10.4103/idoj.IDOJ_84_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lallas A, Zaballos P, Zalaudek I, Apalla Z, Gourhant JY, Longo C, et al. Dermoscopic patterns of granuloma annulare and necrobiosis lipoidica. Clin Exp Dermatol. 2013;38:425–7. doi: 10.1111/ced.12126. [DOI] [PubMed] [Google Scholar]
- 9.Ramadan S, Hossam D, Saleh MA. Dermoscopy could be useful in differentiating sarcoidosis from necrobiotic granulomas even after treatment with systemic steroids. Dermatol Pract Concept. 2016;6:17–22. doi: 10.5826/dpc.0603a05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Conde-Montero E, Avile×s-Izquierdo JA, Mendoza-Cembranos MD, Parra-Blanco V. Dermoscopy of necrobiosis lipoidica. Actas Dermosifiliogr. 2013;104:534–7. doi: 10.1016/j.ad.2012.07.017. [DOI] [PubMed] [Google Scholar]
- 11.Pellicano R, Caldarola G, Filabozzi P, Zalaudek I. Dermoscopy of necrobiosis lipoidica and granuloma annulare. Dermatology. 2013;226:319–23. doi: 10.1159/000350573. [DOI] [PubMed] [Google Scholar]
- 12.Balestri R, La Placa M, Bardazzi F, Rech G. Dermoscopic subpatterns of granulomatous skin diseases. J Am Acad Dermatol. 2013;69:e217–8. doi: 10.1016/j.jaad.2013.03.030. [DOI] [PubMed] [Google Scholar]
- 13.Errichetti E, Lallas A, Apalla Z, Di Stefani A, Stinco G. Dermoscopy of granuloma annulare: A clinical and histological correlation study. Dermatology. 2017;233:74–9. doi: 10.1159/000454857. [DOI] [PubMed] [Google Scholar]
- 14.Errichetti E, Cataldi P, Stinco G. Dermoscopy in annular elastolytic giant cell granuloma. J Dermatol. 2019;46:e66–7. doi: 10.1111/1346-8138.14539. [DOI] [PubMed] [Google Scholar]
- 15.Ramadan S, Hossam D, Saleh MA. Dermoscopy could be useful in differentiating sarcoidosis from necrobiotic granulomas even after treatment with systemic steroids. Dermatol Pract Concept. 2016;6:17–22. doi: 10.5826/dpc.0603a05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lallas A, Argenziano G, Apalla Z, Gourhant JY, Zaballos P, Di Lernia V, et al. Dermoscopic patterns of common facial inflammatory skin diseases. J Eur Acad Dermatol Venereol. 2014;28:609–14. doi: 10.1111/jdv.12146. [DOI] [PubMed] [Google Scholar]
- 17.Lalla A, Argenziano G, Longo C, Moscarella E, Apalla Z, Koteli C, et al. Polygonal vessels of rosacea are highlighted by dermoscopy. Int J Dermatol. 2014;53:e325–7. doi: 10.1111/ijd.12270. [DOI] [PubMed] [Google Scholar]
- 18.Ayhan E, Alabalik U, Avci Y. Dermoscopic evaluation of two patients with lupus miliaris disseminatus faciei. Clin Exp Dermatol. 2014;39:500–2. doi: 10.1111/ced.12331. [DOI] [PubMed] [Google Scholar]
- 19.Chauhan P, Jindal R, Shirazi N. Dermoscopy of lupus milaris disseminatus faciei: A step closer to diagnosis. Dermatol Pract Concept. 2020;10:e2020055. doi: 10.5826/dpc.1003a55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Critchlow WA, Chang D. Cheilitis granulomatosa: A review. Head Neck Pathol. 2014;8:209–13. doi: 10.1007/s12105-013-0488-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chopra A, Mitra D, Agarwal R, Saraswat N, Talukdar K, Solanki A. Correlation of dermoscopic and histopathologic patterns in leprosy - A pilot study. Indian Dermatol Online J. 2019;10:663–8. doi: 10.4103/idoj.IDOJ_297_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vinay K, Kamat D, Chatterjee D, Narang T, Dogra S. Dermatoscopy in leprosy and its correlation with clinical spectrum and histopathology: A prospective observational study. J Eur Acad Dermatol Venereol. 2019;33:1947–51. doi: 10.1111/jdv.15635. [DOI] [PubMed] [Google Scholar]
- 23.Ankad BS, Sakhare PS. Dermoscopy of borderline tuberculoid leprosy. Int J Dermatol. 2018;57:74–6. doi: 10.1111/ijd.13731. [DOI] [PubMed] [Google Scholar]
- 24.Ankad B, Sakhare P. Dermoscopy of histoid leprosy: A case report. Dermatol Pract Concept. 2017;7:63–5. doi: 10.5826/dpc.0702a14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Acharya P, Mathur MC. Clinicodermoscopic study of histoid leprosy: A case series. Int J Dermatol. 2020;59:365–8. doi: 10.1111/ijd.14731. [DOI] [PubMed] [Google Scholar]
- 26.Brasiello M, Zalaudek I, Ferrara G, Gourhant JY, Capoluongo P, Roma P, et al. Lupus vulgaris: A new look at an old symptom—The lupoma observed with dermoscopy. Dermatology. 2009;218:172–4. doi: 10.1159/000182255. [DOI] [PubMed] [Google Scholar]
- 27.Lobato-Berezo A, Martín-Ezquerra G, Vidal-Navarro A, Pujol RM. Red and orange colors as dermoscopic clues for fish-tank granuloma. Dermatol Pract Concept. 2019;9:162–4. doi: 10.5826/dpc.0902a18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Llambrich A, Zaballos P, Terrasa F, Torne I, Puig S, Malvehy J. Dermoscopy of cutaneous leishmaniasis. Br J Dermatol. 2009;160:756–61. doi: 10.1111/j.1365-2133.2008.08986.x. [DOI] [PubMed] [Google Scholar]
- 29.Yücel A, Günasti S, Denli Y, Uzun S. Cutaneous leishmaniasis: New dermoscopic findings. Int J Dermatol. 2013;52:831–7. doi: 10.1111/j.1365-4632.2012.05815.x. [DOI] [PubMed] [Google Scholar]
- 30.Taheri AR, Pishgooei N, Maleki M, Goyonlo VM, Kiafar B, Banihashemi M, et al. Dermoscopic features of cutaneous leishmaniasis. Int J Dermatol. 2013;52:1361–6. doi: 10.1111/ijd.12114. [DOI] [PubMed] [Google Scholar]
- 31.Ayhan E, Ucmak D, Baykara SN, Akkurt ZM, Arica M. Clinical and dermoscopic evaluation of cutaneous leishmaniasis. Int J Dermatol. 2015;54:193–201. doi: 10.1111/ijd.12686. [DOI] [PubMed] [Google Scholar]
- 32.Subhadarshani S, Yadav D. Dermoscopy of chromoblastomycosis. Dermatol Pract Concept. 2017;7:23–4. doi: 10.5826/dpc.0704a06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chauhan P, Jindal R, Shirazi N. Dermoscopy of chromoblastomycosis. Indian Dermatol Online J. 2019;10:759–60. doi: 10.4103/idoj.IDOJ_213_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang CS, Chen CB, Lee YY, Yang CH, Chang YC, Chung WH, et al. Chromoblastomycosis in Taiwan: A report of 30 cases and a review of the literature. Med Mycol. 2018;56:395–405. doi: 10.1093/mmy/myx075. [DOI] [PubMed] [Google Scholar]
- 35.Vinay K, Bhattacharjee R, Bishnoi A, Chatterjee D, Rudramurthy S, Dogra S. Dermatoscopic features of cutaneous sporotrichosis? J Eur Acad Dermatol Venereol. 2020 doi: 10.1111/jdv.16539. doi: 10.1111/jdv.16539. [DOI] [PubMed] [Google Scholar]
- 36.Ankad BS, Manjula R, Tejasvi T, Nikam BP. Dermoscopy of eumycotic mycetoma: A case report. Dermatol Pract Concept. 2019;9:297–9. doi: 10.5826/dpc.0904a10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ankad BS, Beergoudar SL, Nikam BP. Dermatoscopy in actinomycetoma: An observation. Indian Dermatol Online J. 2019;10:330–1. doi: 10.4103/idoj.IDOJ_268_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Litaiem N, Midassi O, Zeglaoui F. Detecting subclinical mycetoma's black grains using dermoscopy. Int J Dermatol. 2019;58:231–2. doi: 10.1111/ijd.14187. [DOI] [PubMed] [Google Scholar]
- 39.Amezcua Gudiño S, López López AM, Soria Orozco M, Figueroa Martínez AY, Ramírez Padilla M. Severe colloid milium presenting as papillomatosis cutis associated with vitiligo. Int J Dermatol. 2017;56:878–80. doi: 10.1111/ijd.13681. [DOI] [PubMed] [Google Scholar]
- 40.Vano-Galvan S, Alvarez-Twose I, De las Heras E, Morgado JM, Matito A, Sánchez-Muñoz L, et al. Dermoscopic features of skin lesions in patients with mastocytosis. Arch Dermatol. 2011;147:932–40. doi: 10.1001/archdermatol.2011.190. [DOI] [PubMed] [Google Scholar]
- 41.Oliveira TE, Tarlé RG, Mesquita LAF. Dermoscopy in the diagnosis of juvenile xanthogranuloma. An Bras Dermatol. 2018;93:138–40. doi: 10.1590/abd1806-4841.20186849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vinay K, Sawatkar GU, Saikia UN, Kumaran MS. Dermatoscopic evaluation of three cases of nevus lipomatosus cutaneous superficialis. Indian J Dermatol Venereol Leprol. 2017;83:383–6. doi: 10.4103/ijdvl.IJDVL_677_16. [DOI] [PubMed] [Google Scholar]
- 43.Kelati A, Baybay H, Gallouj S, Mernissi FZ. Dermoscopic Analysis of nevus sebaceus of Jadassohn: A study of 13 cases. Skin Appendage Disord. 2017;3:83–91. doi: 10.1159/000460258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cheng CY, Su HJ, Kuo TT. Dermoscopic features and differential diagnosis of sebaceous carcinoma. J Dermatol. 2020;47:755–62. doi: 10.1111/1346-8138.15384. [DOI] [PubMed] [Google Scholar]


