Abstract
Background:
We present two cases of scalp arteriovenous fistula (sAVF) treated by transarterial embolization with the aid of a temporary balloon occlusion (TBO) to detect precise vasculature.
Case Description:
Case 1: A 59-year-old woman noticed a sudden onset of pulsating bruits. sAVF was fed by the right superficial temporal artery (STA) and drained to the right superficial temporal vein. We performed feeder occlusion using coils after the recognition of a single feeder and a single fistula using TBO. Case 2: A 42-year-old woman noticed a pulsating subcutaneous mass. sAVF was fed by the right occipital artery (OA) and drained to the right occipital vein (OV). We could detect another feeder of the right STA after the TBO of the OA. We performed transarterial feeder occlusion for STA and OA using coil and N-butyl-2-cyanoacrylat including OV and shunt point, because this case was a single fistula with multiple feeders.
Conclusion:
sAVFs are a relatively rare disease with a complex vascular structure. For the adequate transarterial approach, TBO was useful for detecting the precise vasculature of sAVF.
Keywords: Scalp arteriovenous fistula, Temporary balloon occlusion, Transarterial embolization

INTRODUCTION
Scalp arteriovenous fistulas (sAVFs) are rare abnormal connections between subcutaneous arteries and veins without an intervening capillary bed. They are also referred to as cirsoid aneurysm, aneurysma serpentinum, aneurysm racemosum, or plexiform angioma.[3] Symptoms include pulsatile mass, headache, bruits, tinnitus, and hemorrhage.[8]
Treatment includes surgical excision, endovascular embolization, or a combination of these treatments.[2-10] Embolization has become more common, and transarterial or transvenous approach is selected. To treat appropriately, an understanding of the vascular structure is essential. However, it is sometimes difficult to detect the precise vasculature because sAVFs have a large variety of complex connection between subcutaneous feeding arteries and draining veins even when several modalities are used including digital subtraction angiography (DSA), three-dimensional DSA, computed tomography angiography, and magnetic resonance imaging scan. It leads to the misdiagnosis and failure of treatment. Here, we report successful transarterial treatment for two cases of sAVFs with the aid of a temporary balloon occlusion (TBO).
CASE REPORT
Case 1
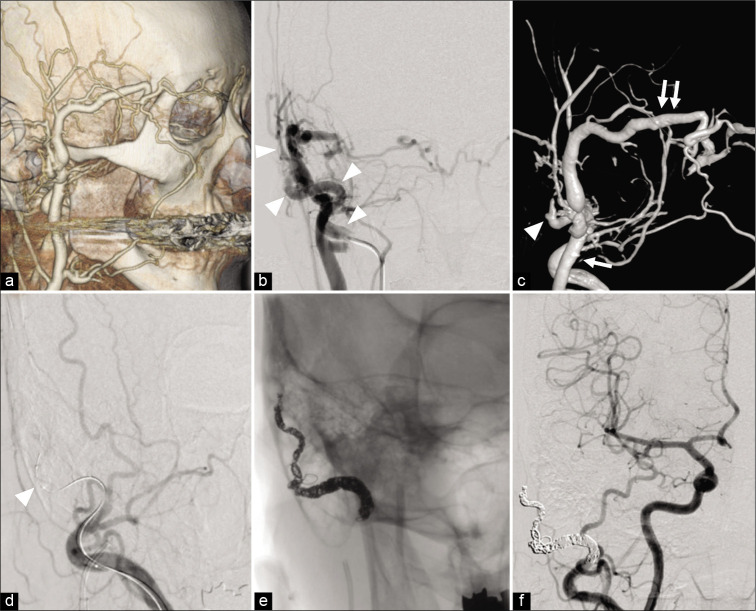
The patient was a 53-year-old woman with a history of hyperlipidemia but no past episode of trauma. The patient noticed a sudden onset of pulsating bruits in the right preauricular region. The symptoms did not improve over 2 years. Therefore, the patient underwent MRI at another hospital and was referred to our hospital for suspected sAVF. On admission, no neurological abnormalities were noted. We noticed pulsating bruits, thrill at the right preauricular region. CT angiography (CTA) [Figure 1a] and DSA [Figure 1b and c] revealed sAVF with a fistula in the right preauricular region fed by the right superficial temporal artery (STA) and drained to the right superficial temporal vein to the lower external jugular vein and to the superior ophthalmic vein through the angular vein. Endovascular treatment was initiated under local anesthesia. After the placement of a 6 Fr sheath in the right femoral artery, a 6Fr Launcher guiding catheter (Medtronic, Minneapolis, MN, USA) was placed at the right external carotid artery. When Hyperform 4 mm × 7 mm (Medtronic, Minneapolis, MN, USA) was placed in the STA just proximal to the fistulous point, shunt flow disappeared [Figure 1d]. We recognized that this sAVF had the structure of a single feeder and a single fistula. After the removal of the HyperForm and the placement of the SL10 microcatheter (Stryker, Kalamazoo, MI, USA) at distal the STA, transarterial embolization (TAE) for STA using platinum coils was performed [Figure 1e]. We achieved a complete occlusion of the arteriovenous shunt [Figure 1f]. After embolization, the pulsating bruits disappeared. There were no complications including necrosis of the scalp and irritating mass of the coil. One year after TAE, no recanalization occurred.
Figure 1:
(a) CT angiography showing the dilated subcutaneous vein suspected the existence of an arteriovenous shunt in the right preauricular region. (b) DSA showing scalp arteriovenous fistula with a fistula at the right preauricular region fed by the right STA (arrowhead). (c) 3D-DSA showing the fistulous point (arrowhead) is located in the preauricular region fed by the right STA and drained to the right STV to lower the external jugular vein (arrow) and to the superior ophthalmic vein through the angular vein (double arrow). (d). TBO using Hyperform 4 mm × 7 mm (Medtronic, Minneapolis, MN, USA) placed in the STA just proximal to the fistulous point (arrowhead) reveals that no additional feeder exists. (e) Transarterial embolization for STA was performed using platinum coils. (f) The disappearance of the arteriovenous shunt is confirmed. sAVF: Scalp arteriovenous fistula, TBO: temporary balloon occlusion, ST: Superficial temporal artery, OA: Occipital artery, OV: Occipital vein, NBCA: N-butyl-2-cyanoacrylat, DSA: Digital subtraction angiography, CTA: CT angiography.
Case 2
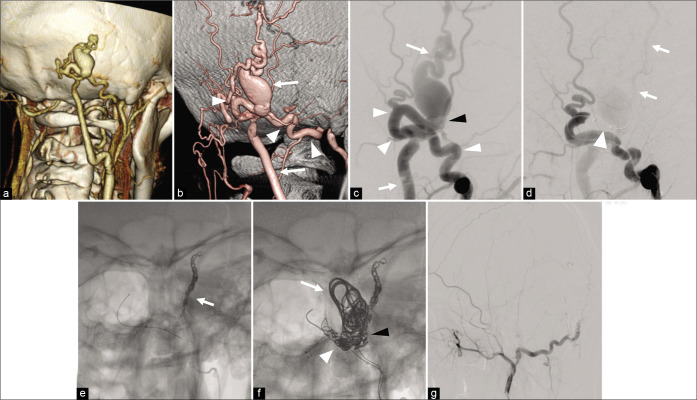
The patient was a 42-year-old woman with no history of traumatic episodes. She noticed a pulsating subcutaneous mass in the right occipital head. The patient underwent CTA at a local plastic surgery hospital and for suspected sAVF and was referred to our hospital. On admission, no neurological abnormalities were noted. We noticed a pulsating mass and bruit of the right back of the head. CTA [Figure 2a] and DSA [Figure 2b and c] revealed sAVF with a fistula at the right back of the head fed by the right occipital artery (OA) and drained into the right occipital vein (OV). Endovascular treatment was initiated under local anesthesia. After the placement of a 6 Fr sheath in the right femoral artery, a 6Fr Roadmaster guiding catheter (Goodman, Aichi, Japan) was placed at the right OA. When SHORYU HR 4 mm × 7 mm (Kaneka Medix Corp, Osaka, Japan) was placed in the OA just proximal to the fistulous point, another feeder of the right STA that had a retrograde flow to the same fistulous point was revealed [Figure 2d]. We recognized that this sAVF had the structure of a single fistula with multiple feeders. After the removal of the SHORYU and the placement of the SL-10 microcatheter (Stryker, Kalamazoo, MI, USA) at the right STA from OA through the shunt point, we performed TAE of the STA using coils and 33% N-butyl-2-cyanoacrylate (NBCA) at first [Figure 2e]. Second, we performed occlusion of dilated OV including the shunt point, and finally OA using coil and 33% NBCA [Figure 2f]. We achieved a complete occlusion of the arteriovenous shunt [Figure 2g]. After embolization, the pulsating mass disappeared. There were no complications including necrosis of the scalp and irritating mass of coil. One year after TAE, no recanalization occurred.
Figure 2:
(a) CT angiography showing the dilated subcutaneous vein suspected the existence of an arteriovenous shunt in the right occipital head. (b) 3D-DSA showing scalp arteriovenous fistula with a fistula at the right occipital head fed by the right OA (arrowhead) and drained to the right OV (arrow). (c) DSA showing the OA and OV has a direct connection at the fistulous point (black arrowhead). (d) TBO using SHORYU HR 4 mm × 7 mm (Kaneka Medix Corp, Osaka, Japan) (arrowhead) placed in the OA just proximal to the fistulous point (arrowhead) reveals that an additional feeder from the STA (arrow) with retrograde flow exists. (e) TAE for STA was performed using coils and NBCA. (f) TAE for dilated OV (arrow) including shunt point (black arrowhead), and OA (arrowhead) using coil and NBCA. (g) The disappearance of the arteriovenous shunt is confirmed. sAVF: Scalp arteriovenous fistula, TBO: temporary balloon occlusion, ST: Superficial temporal artery, OA: Occipital artery, OV: Occipital vein, NBCA: N-butyl-2-cyanoacrylat, DSA: Digital subtraction angiography, CTA: CT angiography.
DISCUSSION
sAVFs are rare subcutaneous diseases with abnormal connections between subcutaneous arteries and veins without an intervening capillary bed. In a recent systematic review of the literature, Sofela et al. reported that the etiology of sAVF was that 60.2% were spontaneous, 32.3% trauma, and 7.5% iatrogenic in total 74 patients.[8] sAVFs were more common in men than in women. The most common symptoms were a pulsatile mass (94.4%), headaches (25.3%), and tinnitus (20.2%). Hemorrhage could also be present.
They can be managed by surgical excision only, endovascular embolization only, or a combination of both.[2-10] To treat appropriately, the understanding of vascular structure is essential. For the diagnosis, conventional DSA, three-dimensional DSA, CTA, and MRI are performed.[2,5] However, it is sometimes difficult to detect the structure because of their heterogeneous angioarchitecture and non-uniform structure. A high-flow shunt also makes it difficult. It leads to misdiagnosis and failure of treatment. Yokouchi et al. classified sAVFs to three types in the way of treatment.[10] Type A scalp AVFs as having a single fistula fed by a single proximal feeding artery, type B AVFs as having a single fistula fed by multiple arterial feeders, and type C AVFs as having multiple fistulas with plexiform feeding arteries and a main dilated draining vein. The recommendation of treatment was that type A was initiated by TAE, type B by TVE, and type C by a combination of surgical excision and endovascular embolization. In our case, the fistula was type A in case1 and type B in case2.
The transarterial approach is easier compared with the transvenous approach especially when the target vessel is dilated and less tortuous.[1,8] Shunt occlusion is also possible by penetrating the embolic material as a coil and liquid embolic material through the feeder. However, inappropriate feeder occlusion results in the fails catheter access to the fistula site. Furthermore, TAE is rarely curative, and recurrence may occur.[2] In Case 1, TAE using coils was performed because TBO revealed a single fistula fed by a single feeder. This simple vascular structure is a good indication for TAE. In Case 2, TBO revealed two feeders of dilated OA and normal caliber of the STA. By the temporary occlusion of the major feeder, the complex structure of sAVF becomes easier to understand in detail, and therapeutic strategies would be considered precisely. Indeed, our cases experienced no recurrence. Therefore, TBO was useful for understanding the precise vasculature of sAVF for TAE. TVE is needed when sAVF has a complicated structure of multiple feeders as previously reported.[2,6] One of the disadvantages of the transvenous approach is catheter access because the subcutaneous vein has a large variety of vasculature. Hence, TVE with direct puncture sometimes required.[4] TVE also carries the risk of migration of the embolic materials into the draining vein and pulmonary embolization.[5,6] Surgical removal has historically been the most common treatment for sAVF.[3,7] However, it has several risks, such as massive blood loss and skin necrosis requiring scalp reconstruction. Attention should be taken to decide the treatment strategy. As for the embolic materials, NBCA or Onyx has been widely used for sAVFs. However, a wide range of TAE using NBCA or Onyx leads to the skin necrosis because of skin inflammation and the lack of blood supply to the normal skin.[1] Onyx use is also countered by tantalum-induced black skin discoloration; therefore, attention should be paid to the region uncovered by hair.[2] When using a coil, an irritating mass may be a disadvantage. However, scalp necrosis is not hard to occur and to handle coils is easy. Hence, TAEs using coils were also effective in our cases.
CONCLUSION
sAVFs are rare diseases with complex vasculature. For the safe and effective endovascular transarterial approach for sAVF, TBO is useful for understanding the precise vasculature.
Acknowledgments
We acknowledge the assistance of editorial services that provided language.
Footnotes
How to cite this article: Kawano D, Fukuda K, Fukumoto H, Horio Y, Takahara M, Abe H, et al. The usefulness of temporary balloon occlusion during transarterial embolization for scalp arteriovenous fistula. Surg Neurol Int 2021;12:89.
Contributor Information
Dai Kawano, Email: kawanojohn@gmail.com.
Kenji Fukuda, Email: kenji.fukuda.0315@me.com.
Hironori Fukumoto, Email: infinite19@hotmail.co.jp.
Yoshinobu Horio, Email: yoshinobu.horio.1986@gmail.com.
Masaki Takahara, Email: crazy.bozu@gmail.com.
Hiroshi Abe, Email: neuroabe1972@gmail.com.
Toshio Higashi, Email: toshio.higashi@gmail.com.
Tooru Inoue, Email: toinoue@adm.fukuoka-u.ac.jp.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Arat A, Cil BE, Vargel I, Turkbey B, Canyigit M, Peynircioglu B, et al. Embolization of high-flow craniofacial vascular malformations with onyx. AJNR Am J Neuroradiol. 2007;28:1409–14. doi: 10.3174/ajnr.A0547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dalyai RT, Schirmer CM, Malek AM. Transvenous balloon-protected embolization of a scalp arteriovenous fistula using onyx liquid embolic. Acta Neurochir (Wien) 2011;153:1285–90. doi: 10.1007/s00701-011-0998-1. [DOI] [PubMed] [Google Scholar]
- 3.Fisher-Jeffes ND, Domingo Z, Madden M, de Villiers JC. Arteriovenous malformations of the scalp. Neurosurgery. 1995;36:656–60. doi: 10.1227/00006123-199504000-00003. discussion 660. [DOI] [PubMed] [Google Scholar]
- 4.Komiyama M, Nishikawa M, Kitano S, Sakamoto H, Imai K, Tsujiguchi K, et al. Non-traumatic arteriovenous fistulas of the scalp treated by a combination of embolization and surgical removal. Neurol Med Chir (Tokyo) 1996;36:162–5. doi: 10.2176/nmc.36.162. [DOI] [PubMed] [Google Scholar]
- 5.Li D, Heiferman DM, Rothstein BD, Syed HR, Shaibani A, Tomita T. Scalp arteriovenous malformation (cirsoid aneurysm) in adolescence: Report of 2 cases and review of the literature. World Neurosurg. 2018;116:e1042–6. doi: 10.1016/j.wneu.2018.05.161. [DOI] [PubMed] [Google Scholar]
- 6.Ni W, Tian Y, Gu Y, Mao Y. Transvenous endovascular treatment for scalp arteriovenous fistulas: Results with combined use of onyx and coils. World Neurosurg. 2017;107:692–7. doi: 10.1016/j.wneu.2017.08.056. [DOI] [PubMed] [Google Scholar]
- 7.Senoglu M, Yasim A, Gokce M, Senoglu N. Nontraumatic scalp arteriovenous fistula in an adult: Technical report on an illustrative case. Surg Neurol. 2008;70:194–7. doi: 10.1016/j.surneu.2007.04.018. [DOI] [PubMed] [Google Scholar]
- 8.Sofela A, Osunronbi T, Hettige S. Scalp cirsoid aneurysms: Case illustration and systematic review of literature. Neurosurgery. 2020;86:E98–107. doi: 10.1093/neuros/nyz303. [DOI] [PubMed] [Google Scholar]
- 9.Sousa LH, Gatto LA, Junior Z, Koppe GL. Scalp cirsoid aneurysm: An updated systematic literature review and an illustrative case report. World Neurosurg. 2018;119:416–27. doi: 10.1016/j.wneu.2018.08.098. [DOI] [PubMed] [Google Scholar]
- 10.Yokouchi T, Iwabuchi S, Tomiyama A, Samejima H, Ogata N, Goto K. Embolization of scalp AVF. Interv Neuroradiol. 1999;5(Suppl 1):121–6. doi: 10.1177/15910199990050S122. [DOI] [PubMed] [Google Scholar]